Rehabilitation Outcome Measures in Patients with Spinal Stenosis: A Literary Review
Abstract
:1. Introduction
- Congenital LSS, due to postnatal disorders which cause pathological stricture of the central spinal canal. This form is quite rare (only 4–5% of all LSS) [3].
- Acquired LSS due to aging and subsequent degenerative changes of spinal structures, particularly facet joints, intervertebral discs (with associated bulging), and the ligamentum flavum.
- Combined LSS deriving from both of the precedent conditions [4].
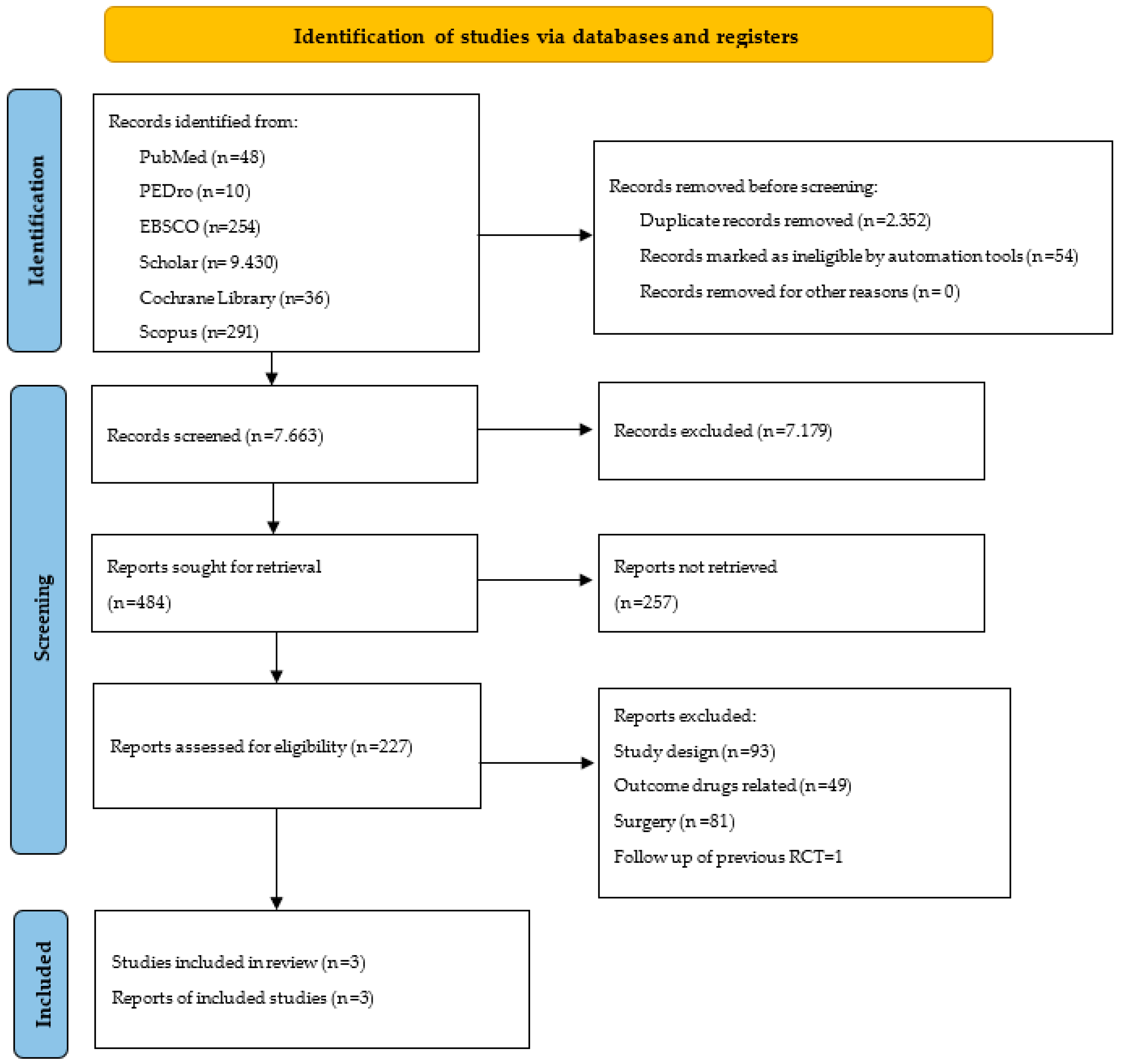
2. Methods
- RQ1: Which are the main outcome domains to be evaluated in the rehabilitation of the patient with lumbar stenosis?
- RQ2: Does the literature only suggest self-reported outcome measures (questionnaires) or does the literature include objective scores?
- -
- P: Patients with a diagnosis of lumbar spinal stenosis, with an indication to undergo an intensive physiotherapy treatment period. No difference was defined depending on stenosis location (central canal, lateral recess, foramen).
- -
- I: Physiotherapy modalities (therapeutic exercises, manual therapy, strength exercises, stretching protocols, aerobic exercises), even in multidisciplinary rehabilitation plans.
- -
- C: Inactive control groups or usual care prosecution.
- -
- O: Physiotherapy-related tools, both patient-centred (questionnaires) and objective ones (evaluation scales performed by physiotherapists, clinical/instrumental tests). Patient satisfaction was not considered. The main hypothesised domains of outcome: functionality, quality of life, pain, symptom control, and fear of movement.
Search Strategy
3. Results
3.1. Critical Appraisal
3.2. Study Results
3.3. Self-Reported Disability
- -
- The study of pain and its location in the back/leg (with a deep focus on pain influence in everyday life for the French-Swiss questionnaire)
- -
- Investigation of activities of daily living, such as washing, eating, walking different distances, sleeping, weightlifting, and sexual activity (deepened in the ODI index)
- -
- General mobility, in a home setting and on trips
- -
- Balance (French-Swiss questionnaire and Zurich in depth).
3.4. Clinical Tests
3.5. Pain
- -
- Reconstruction of pain during the day and at night
- -
- Requiring assistance from a caregiver
- -
- Endurance and pain during gait and stairs
- -
- Emotional concerns and depression
3.6. Mental Wellbeing and Kynesiophobia
- -
- Fear of (re)injury and avoiding exertion to not worsen pain
- -
- Somatic tract (such as consideration of proper condition by others)
3.7. Quality of Life
4. Discussion
- Disability (ODI, Zurich questionnaire, French-Swiss questionnaire) [32,33,34] tended to change at any given study time, with a trend of maintaining stable benefits in patients treated with complex rehabilitation plans (involving stretching/strengthening exercises, isotonic/isometric reinforcement, and manual therapy).
- In general lower extremity ability tests, the SPWT walked distance test seemed to be more sensitive to physiotherapy, showing significant changes. SPPB had no significant changes between groups. Instead, the functional test registered changes only for sit-to-stand repetitions. Muscle testing and active flexion ROM recognised minimal improvements at 6 weeks, while significance was reached only after surgery [34].
- Mental wellbeing and kynesiophobia declined in our included papers [32,33,34]: depression (HADS, CES-D, Beck Index), catastrophizing behaviours (PCS), fear of movement (TSK), anxiety (PASS-20), and falls (FES). These represented the less sensitive domains in LSS patients, with a general trend of remaining stable or minimally improving without significance.
- Finally, quality of life was measured through SF-36 [32,33] and Euroqol-5D [34]. Only SF-36 showed changes in treated patients, and only in a few sub-scales (pain, physical function, and mental health) in the long term. This was in accord with the assumption that all mental/social/wellbeing domains are not sensitive to pre/post measures, deserving a long follow-up time to demonstrate treatment efficacy.
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Watters, W.C., III; Baisden, J.; Gilbert, T.J.; Kreiner, S.; Resnick, D.K.; Bono, C.M.; Ghiselli, G.; Heggeness, M.H.; Mazanec, D.J.; O’Neill, C.; et al. Degenerative lumbar spinal stenosis: An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J. 2008, 8, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.; Gray, D.; Kreuter, W.; Mirza, S.; Martin, B. United States trends in lumbar fusion surgery for degenerative conditions. Spine 2005, 30, 1441–1445. [Google Scholar] [CrossRef]
- Schneider, M.J.; Ammendolia, C.; Murphy, D.R.; Glick, R.M.; Hile, E.; Tudorascu, D.L.; Morton, S.C.; Smith, C.; Patterson, C.G.; Piva, S.R. Comparative Clinical Effectiveness of Nonsurgical Treatment Methods in Patients with Lumbar Spinal Stenosis: A Randomized Clinical Trial. JAMA Netw. Open 2019, 2, e186828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chad, D.A. Lumbar spinal stenosis. Neurol. Clin. 2007, 25, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Hallinan, J.T.P.D.; Zhu, L.; Yang, K.; Makmur, A.; Algazwi, D.A.R.; Thian, Y.L.; Lau, S.; Choo, Y.S.; Eide, S.E.; Yap, Q.V.; et al. Deep Learning Model for Automated Detection and Classification of Central Canal, Lateral Recess, and Neural Foraminal Stenosis at Lumbar Spine MRI. Radiology 2021, 300, 130–138. [Google Scholar] [CrossRef]
- Özer, A.F.; Akyoldaş, G.; Çevik, O.M.; Aydın, A.L.; Hekimoğlu, M.; Sasani, M.; Öktenoğlu, T.; Çerezci, Ö.; Süzer, T. Lumbar Foraminal Stenosis Classification That Guides Surgical Treatment. Int. J. Spine Surg. 2022, 16, 666–673. [Google Scholar] [CrossRef]
- Machado, G.C.; Ferreira, P.H.; Harris, I.A.; Pinheiro, M.B.; Koes, B.W.; Van Tulder, M.; Rzewuska, M.; Maher, C.G.; Ferreira, M.L. Effectiveness of Surgery for Lumbar Spinal Stenosis: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0122800. [Google Scholar] [CrossRef] [Green Version]
- Porter, R.W. Spinal stenosis and neurogenic claudication. Spine 1996, 21, 2046–2052. [Google Scholar] [CrossRef]
- Lurie, J.; Tomkins-Lane, C. Management of lumbar spinal stenosis. BMJ 2016, 352, h6234. [Google Scholar] [CrossRef]
- Conway, J.; Tomkins, C.; Haig, A. Walking assessment in people with lumbar spinal stenosis: Capacity, performance, and self-report measures. Spine J. 2011, 11, 816–823. [Google Scholar] [CrossRef] [Green Version]
- Katz, J.N.; Dalgas, M.; Stucki, G.; Katz, N.P.; Bayley, J.; Fossel, A.H.; Chang, L.C.; Lipson, S.J. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995, 38, 1236–1241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomkins-Lane, C.C.; Conway, J.; Hepler, C.; Haig, A. Changes in objectively measured physical activity [performance] after epidural steroid injection for lumbar spinal stenosis. Arch. Phys. Med. Rehabil. 2012, 93, 2008–2014. [Google Scholar] [CrossRef]
- Whitehurst, M.; Brown, L.E.; Eidelson, S.G.; D’Angelo, A. Functional mobility performance in an elderly population with lumbar spinal stenosis. Arch. Phys. Med. Rehabil. 2001, 82, 464–467. [Google Scholar] [CrossRef]
- Tomkins-Lane, C.C.; Holz, S.C.; Yamakawa, K.S.; Phalke, V.V.; Quint, D.J.; Miner, J.; Haig, A.J. Predictors of walking performance and walking capacity in people with lumbar spinal stenosis, low back pain, and asymptomatic controls. Arch. Phys. Med. Rehabil. 2012, 93, 647–653. [Google Scholar] [CrossRef] [Green Version]
- Ammendolia, C.; Stuber, K.J.; Rok, E.; Rampersaud, R.; Kennedy, C.A.; Pennick, V.; Steenstra, I.A.; de Bruin, L.K.; Furlan, A.D.; Cochrane Back and Neck Group. Nonoperative treatment for lumbar spinal stenosis with neurogenic claudication. Cochrane Database Syst. Rev. 2013, 30, CD010712. [Google Scholar] [CrossRef] [PubMed]
- Haig, A.J.; Tomkins, C.C. Diagnosis and management of lumbar spinal stenosis. J. Am. Med. Assoc. 2010, 303, 71–72. [Google Scholar] [CrossRef] [PubMed]
- Tomkins, C.C.; Dimoff, K.H.; Forman, H.S.; Gordon, E.S.; McPhail, J.; Wong, J.R.; Battié, M.C. Physical therapy treatment options for lumbar spinal stenosis. J. Back Musculoskelet. Rehabil. 2010, 23, 31–37. [Google Scholar] [CrossRef]
- Macedo, L.G.; Hum, A.; Kuleba, L.; Mo, J.; Truong, L.; Yeung, M.; Battié, M.C. Physical therapy interventions for degenerative lumbar spinal stenosis: A systematic review. Phys. Ther. 2013, 93, 1646–1660. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, A.; Nakamura, H. Microendoscopic Lumbar Posterior Decompression Surgery for Lumbar Spinal Stenosis: Literature Review. Medicina 2022, 58, 384. [Google Scholar] [CrossRef]
- Sengupta, D.K.; Herkowitz, H.N. Lumbar spinal stenosis. Treatment strategies and indications for surgery. Orthop. Clin. N. Am. 2003, 34, 281–295. [Google Scholar] [CrossRef]
- McGregor, A.H.; Probyn, K.; Cro, S.; Doré, C.J.; Burton, A.K.; Balagué, F.; Pincus, T.; Fairbank, J. Rehabilitation following surgery for lumbar spinal stenosis. Cochrane Database Syst. Rev. 2013, 2, CD009644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaina, F.; Tomkins-Lane, C.; Carragee, E.; Negrini, S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst. Rev. 2016, 29, CD010264. [Google Scholar] [CrossRef]
- Otani, K.; Kikuchi, S.; Yabuki, S.; Igarashi, T.; Nikaido, T.; Watanabe, K.; Konno, S. Lumbar spinal stenosis has a negative impact on quality of life compared with other comorbidities: An epidemiological cross-sectional Study of 1862 community-dwelling individuals. Sci. World J. 2013, 23, 590652. [Google Scholar] [CrossRef] [Green Version]
- Oka, H.; Matsudaira, K.; Takano, Y.; Kasuya, D.; Niiya, M.; Tonosu, J.; Fukushima, M.; Oshima, Y.; Fujii, T.; Tanaka, S.; et al. A comparative study of three conservative treatments in patients with lumbar spinal stenosis: Lumbar spinal stenosis with acupuncture and physical therapy study (LAP study). BMC Complement. Altern. Med. 2018, 18, 19. [Google Scholar] [CrossRef] [Green Version]
- de Luca, K.; Anderson, D.; Dutt, A.; Magennis, L.; Parrello, T.; Ferreira, M.L.; Chiarotto, A. Outcome Domain and Measurement Instrument Reporting in Randomized Controlled Trials of Interventions for Lumbar Spinal Stenosis: A Systematic Review. J. Orthop. Sports Phys. Ther 2022, 52, 446-A2. [Google Scholar] [CrossRef] [PubMed]
- Bagley, C.; MacAllister, M.; Dosselman, L.; Moreno, J.; Aoun, S.G.; El Ahmadieh, T.Y. Current concepts and recent advances in understanding and managing lumbar spine stenosis. F1000Research 2019, 8, F1000 Faculty Rev-137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Br. Med. J. 2021, 372, n71. [Google Scholar] [CrossRef]
- Richardson, W.S.; Wilson, M.C.; Nishikawa, J.; Hayward, R.S. The well-built clinical question: A key to evidence-based decisions. ACP J. Club 1995, 123, A12–A13. [Google Scholar] [CrossRef]
- Huang, X.; Lin, J.; Demner-Fushman, D. Evaluation of PICO as a knowledge representation for clinical questions. AMIA Annu. Symp. Proc. 2006, 2006, 359–363. [Google Scholar]
- Verhagen, A.P.; De Vet, H.C.; De Bie, R.A.; Kessels, A.G.; Boers, M.; Bouter, L.M.; Knipschild, P.G. The Delphi list: A consensus list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J. Clin. Epid. 1998, 51, 1235–1241. [Google Scholar] [CrossRef] [Green Version]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.M.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ammendolia, C.; Côté, P.; Southerst, D.; Schneider, M.; Budgell, B.; Bombardier, C.; Hawker, G.; Rampersaud, Y.R. Comprehensive Nonsurgical Treatment Versus Self-directed Care to Improve Walking Ability in Lumbar Spinal Stenosis: A Randomized Trial. Arch. Phys. Med. Rehabil. 2018, 99, 2408–2419. [Google Scholar] [CrossRef]
- Minetama, M.; Kawakami, M.; Teraguchi, M.; Kagotani, R.; Mera, Y.; Sumiya, T.; Nakagawa, M.; Yamamoto, Y.; Matsuo, S.; Koike, Y.; et al. Supervised physical therapy vs. home exercise for patients with lumbar spinal stenosis: A randomized controlled trial. Spine J. 2019, 19, 1310–1318. [Google Scholar] [CrossRef] [PubMed]
- Marchand, A.A.; Houle, M.; O’Shaughnessy, J.; Châtillon, C.E.; Cantin, V.; Descarreaux, M. Effectiveness of an exercise-based prehabilitation program for patients awaiting surgery for lumbar spinal stenosis: A randomized clinical trial. Sci. Rep. 2021, 11, 11080. [Google Scholar] [CrossRef] [PubMed]
- Stucki, G.; Daltroy, L.; Liang, M.H.; Lipson, S.J.; Fossel, A.H.; Katz, J.N. Measurement properties of a self-administered outcome measure in lumbar spinal stenosis. Spine 1996, 21, 796–803. [Google Scholar] [CrossRef] [Green Version]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2952. [Google Scholar] [CrossRef] [PubMed]
- Marchand, A.A.; Tetreau, C.; O’Shaughnessy, J.; Descarreaux, M. French-Canadian adaptation and validation of the Swiss spinal stenosis questionnaire for patients with lumbar spinal stenosis. Spine 2019, 44, E487–E493. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill Pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res. 2011, 63 (Suppl. S11), S240–S252. [Google Scholar]
- Fukui, M.; Chiba, K.; Kawakami, M.; Kikuchi, S.I.; Konno, S.I.; Miyamoto, M.; Seichi, A.; Shimamura, T.; Shirado, O.; Taguchi, T.; et al. Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ). Part 3. Validity study and establishment of the measurement scale. J. Orthop. Sci. 2008, 13, 173–179. [Google Scholar] [CrossRef] [Green Version]
- Woby, S.R.; Roach, N.K.; Urmston, M.; Watson, P.J. Psychometric properties of the TSK-11: A shortened version of the Tampa Scale for Kinesiophobia. Pain 2005, 117, 137–144. [Google Scholar] [CrossRef]
- Sullivan, M.J.; Bishop, S.R.; Pivik, J. The pain catastrophizing scale: Development and validation. Psychol. Assess. 1995, 7, 524–532. [Google Scholar] [CrossRef]
- Roelofs, J.; McCracken, L.; Peters, M.L.; Crombez, G.; van Breukelen, G.; Vlaeyen, J.W. Psychometric evaluation of the Pain Anxiety Symptoms Scale (PASS) in chronic pain patients. J. Behav. Med. 2004, 27, 167–183. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Radloff, L.S. The CES-D scale. A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Jackson-Koku, G. Beck Depression Inventory. Occup. Med. 2016, 66, 174–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tinetti, M.E.; Richman, D.; Powell, L. Falls efficacy as a measure of fear of falling. J. Gerontol. 1990, 45, P239–P243. [Google Scholar] [CrossRef]
- Balestroni, G.; Bertolotti, G. EuroQol-5D (EQ-5D): An instrument for measuring quality of life. Monaldi Arch. Chest Dis. 2012, 78, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Pua, Y.H.; Cai, C.C.; Lim, K.C. Treadmill walking with body weight support is no more effective than cycling when added to an exercise program for lumbar spinal stenosis: A randomised controlled trial. Aust. J. Physiother. 2007, 53, 83–89. [Google Scholar] [CrossRef]
- Sahin, F.; Yilmaz, F.; Kotevoglu, N.; Kuran, B. The efficacy of physical therapy and physical therapy plus calcitonin in the treatment of lumbar spinal stenosis. Yonsei Med. J. 2009, 50, 683–688. [Google Scholar] [CrossRef] [Green Version]
- Goren, A.; Yildiz, N.; Topuz, O.; Findikoglu, G.; Ardic, F. Efficacy of exercise and ultrasound in patients with lumbar spinal stenosis: A prospective randomized controlled trial. Clin. Rehabil. 2010, 24, 623–631. [Google Scholar] [CrossRef]
- Hammerich, A.; Whitman, J.; Mintken, P.; Denninger, T.; Akuthota, V.; Sawyer, E.E.; Hofmann, M.; Childs, J.D.; Cleland, J. Effectiveness of Physical Therapy Combined with Epidural Steroid Injection for Individuals with Lumbar Spinal Stenosis: A Randomized Parallel-Group Trial. Arch. Phys. Med. Rehabil. 2019, 100, 797–810. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, J.N.; Tosteson, T.D.; Lurie, J.D.; Tosteson, A.N.; Blood, E.; Hanscom, B.; Herkowitz, H.; Cammisa, F.; Albert, T.; Boden, S.D.; et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N. Engl. J. Med. 2008, 358, 794–810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sampath Dakshina Murthy, A.; Karthikeyan, T.; Vinoth Kanna, R. Gait-based person fall prediction using deep learning approach. Soft Comput. 2021, 26, 12933–12941. [Google Scholar] [CrossRef]
- Sampath Dakshina Murthy, A.; Karthikeyan, T.; Vinoth Kanna, T. Wearable sensor based acoustic gait analysis using phase transition-based optimization algorithm on IoT. Int. J. Speech Technol. 2021, 1–11. [Google Scholar] [CrossRef]
- Delitto, A.; Piva, S.R.; Moore, C.G.; Welch, W.C. Surgery versus Nonsurgical Treatment of Lumbar Spinal Stenosis. Ann. Intern. Med. 2015, 163, 397–398. [Google Scholar] [CrossRef]
- Fritz, J.M.; Lurie, J.D.; Zhao, W.; Whitman, J.M.; Delitto, A.; Brennan, G.P.; Weinstein, J.N. Associations between physical therapy and long-term outcomes for individuals with lumbar spinal stenosis in the SPORT study. Spine J. 2014, 14, 1611–1621. [Google Scholar] [CrossRef] [Green Version]
- Whitman, J.M.; Flynn, T.W.; Childs, J.D.; Wainner, R.S.; Gill, H.E.; Ryder, M.G.; Garber, M.B.; Bennett, A.C.; Fritz, J.M. A Comparison between Two Physical Therapy Treatment Programs for Patients with Lumbar Spinal Stenosis. Spine 2006, 31, 2541–2549. [Google Scholar] [CrossRef] [PubMed]
| Database | Search String |
|---|---|
| Pubmed | [[lumbarised OR lumbarization OR lumbars OR lumbosacral region OR lumbosacral region [mesh]]] AND [[spinal stenosis [mesh] OR spinal stenosis]] AND [[physical therapy modalities [mesh] OR rehabilitation [mesh] OR strenght exercise OR manual therapy OR stretching exercise OR multidisciplinary treatment]] AND [outcome assessment]; filters: from 2017 to 2022 |
| Cochrane | [[“lumbarised” OR “lumbarization” OR “lumbars” OR “lumbosacral region” OR [“lumbosacral” AND “region”] OR “lumbosacral region”]] AND [[“spinal stenosis” OR [“spinal” AND “stenosis”] OR “spinal stenosis”]] AND [[“physical therapy modalities” OR “rehabilitation”]] AND [“outcome assessment”] in All Text; filters: from 2017 to 2022 |
| Scholar | [[lumbarized OR lumbarization OR lumbar OR lumbosacral region]] AND [[spinal stenosis]] AND [[physical therapy modalities OR rehabilitation OR strength exercise OR manual therapy OR stretching exercise OR multidisciplinary treatment]] AND [outcome assessment]; filters: from 2017 to 2022 |
| Scopus | [lumbar OR lumbosacral AND region OR lumbarization] AND [spinal AND stenosis] [physiotherapy OR rehabilitation OR manual AND therapy OR strength AND exercise OR stretching OR multidisciplinary AND rehabilitation] in All fields; filters: from 2017 to 2022 |
| Pedro | Simple search: lumbar spinal stenosis physiotherapy |
| EBSCO | [[lumbarised OR lumbarization OR lumbars OR lumbosacral region]] AND [[spinal stenosis]] AND [[physical therapy modalities OR rehabilitation OR strength exercise OR manual therapy OR stretching exercise OR multidisciplinary treatment]] AND [outcome]; filters: from 2017 to 2022 |
| Author | Year | Country | Sample | Intervention | Outcome and Tools | Critical Appraisal Score |
|---|---|---|---|---|---|---|
| Ammendolia C et al. [29] | 2018 | USA | 104 patients with LSS, randomly divided in experimental [n = 51] or control arm [n = 53]. | Exp: 6-week comprehensive physiotherapy protocol (which involved education, active exercises, manual therapy, stretching exercises) Cont: 6-weeks autonomous rehabilitation programme with standard activities Follow up at 8 weeks and 3/6/12 months | Walking ability: SPWT test General movement ability: SPPB Disability LSS related: ODI/Zurich questionnaire Pain: NRS for back, legs and numbness Depression: CES-D Fear of Falls: FES | Pedro score 8/10 Jadad Score 4/5 |
| Minetama M et al. [30] | 2019 | Japan | 86 patients with LSS assigned to experimental [n = 43] or control arm [n = 43]. | Exp: supervised 6-weeks physiotherapy programme (manual therapy, stretching and strengthening exercises, cycling, body weight supported treadmill sessions) Cont: standard lumbar flexion exercise protocol Follow up at 6 weeks | Walking ability; SPWT test and n. of daily steps Disability LSS related: Zurich questionnaire and its sub-areas Pain: NRS scale for back, legs and numbness; JOABPEQ questionnaire Depression: HADS scale Mental wellbeing: PCS, PASS-20 Kynesiophobia: Tampa scale Quality of Life: SF-36 Pedometer (only control group) | Pedro score 9/10 Jadad Score 4/5 |
| Marchand AA et al. [32] | 2021 | Canada | 68 patients with LSS awaiting for spinal surgery. Thy were randomly assigned to experimental [n = 35] or control group [n = 33] | Exp: supervised physiotherapy 6-weeks treatment [mainly based on isometric/isotonic reinforcement exercise with increasing difficulty and treadmill training] Cont: Standard usual care protocol [written instructions given to the patient] Follow up at post intervention, post-surgery, 3/6 months | Disability LSS related: ODI; French-Swiss spinal stenosis questionnaire Clinical improvements: Isometric endurance strength of trunk flexor/extensor and knee extensor muscles; active lumbar ROM; get up and go test and sit to stand test repetition Pain: NRS for back, legs, Numbness Depression: Beck Index Kynesiophobia: Tampa scale Quality of life: Euroqol-5D Perception of treatment: 7 points scale for global impression of Change | Pedro score 9/10 Jadad Score 4/5 |
| Test | Objective | Action Required |
|---|---|---|
| Self-placed walk test (SPWT) | Evaluate the longest distance the patient is able to walk in a maximum time of 30 min | Walk on a flat surface until LSS symptom hinder the activity |
| Short physical performance battery (SPPB) | Evaluate general lower extremity function | The test is composed by different tasks: (1) Ability to stand for 10 s with feet in 3 different positions (together side-by-side, semi-tandem, and tandem) (2) Two timed trials of a 3-m or 4-m walk (fastest recorded) (3) Time to rise from a chair five times |
| Isometric measurements | Evaluate isometric contraction of back flexors/extensor muscles and knee extensors | Perform modified Sorensen test (back extensor), maximum trunk flexion maintenance, knee active extension maintenance |
| Active Range of motion Testing (AROM) | Quantifying active lumbar movement | Perform all pain free movements with low back (flexion, extension, lateral inclination, rotation) |
| Get up and go test | Identify fall risk | From a sitting position, stand without using arms to support. Walk 10 feet, turn, and return to the chair Sit back in the chair without using arms for support |
| Sit to stand test | Test leg strength and endurance | From a sitting position go stand and then return (5 times) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciardi, G.; Lamberti, G.; Casati, V.; Paris, E. Rehabilitation Outcome Measures in Patients with Spinal Stenosis: A Literary Review. Physiologia 2023, 3, 421-432. https://doi.org/10.3390/physiologia3030029
Ciardi G, Lamberti G, Casati V, Paris E. Rehabilitation Outcome Measures in Patients with Spinal Stenosis: A Literary Review. Physiologia. 2023; 3(3):421-432. https://doi.org/10.3390/physiologia3030029
Chicago/Turabian StyleCiardi, Gianluca, Gianfranco Lamberti, Vittorio Casati, and Elena Paris. 2023. "Rehabilitation Outcome Measures in Patients with Spinal Stenosis: A Literary Review" Physiologia 3, no. 3: 421-432. https://doi.org/10.3390/physiologia3030029
APA StyleCiardi, G., Lamberti, G., Casati, V., & Paris, E. (2023). Rehabilitation Outcome Measures in Patients with Spinal Stenosis: A Literary Review. Physiologia, 3(3), 421-432. https://doi.org/10.3390/physiologia3030029






