Effect of Ice Slurry Ingestion on Post-Exercise Physiological Responses in Rugby Union Players
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
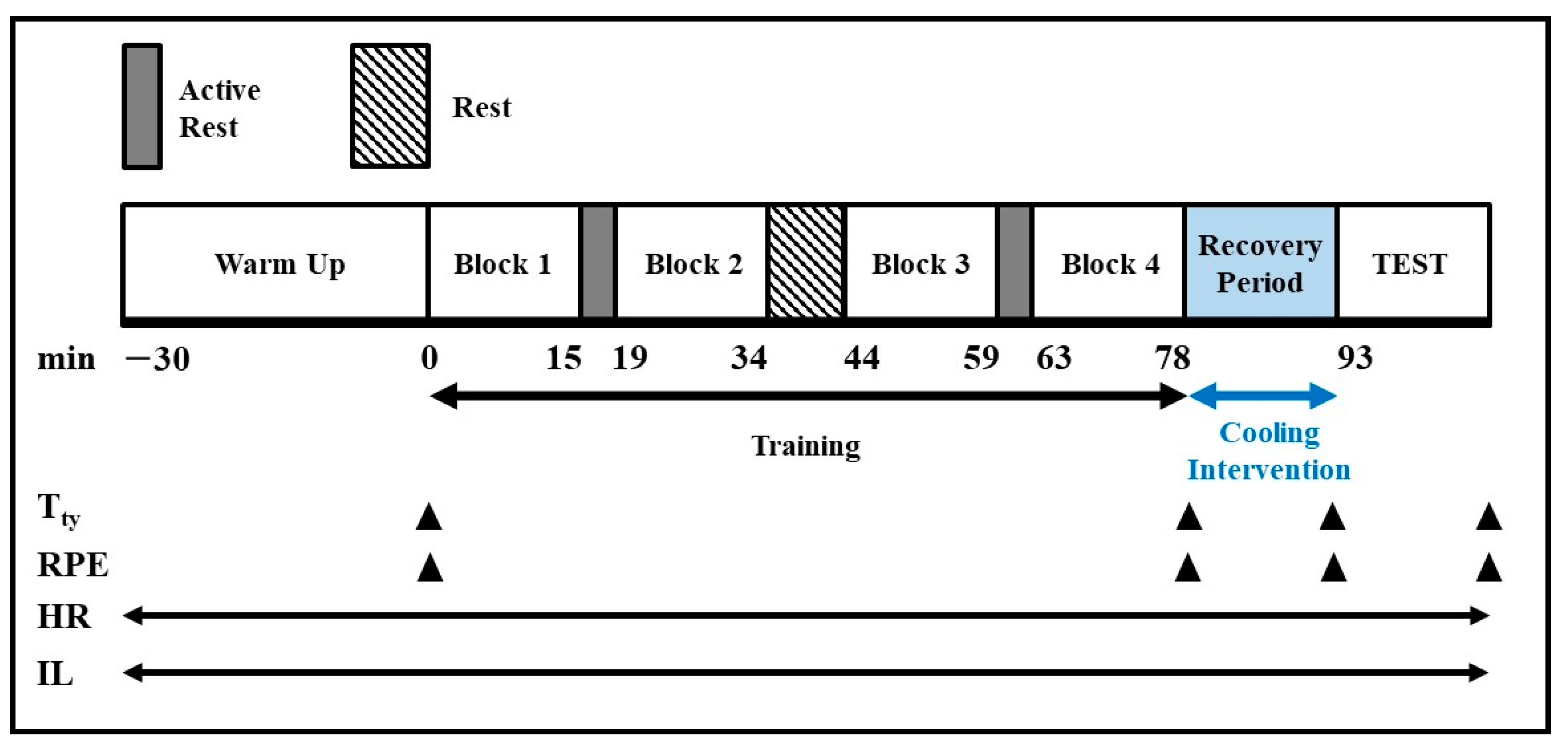
2.2. Study Design
2.3. Cooling Procedures
2.4. Measurements
2.5. Statistical Analysis
3. Results
3.1. Subjects
3.2. Tympanic Temperature and Heat Storage
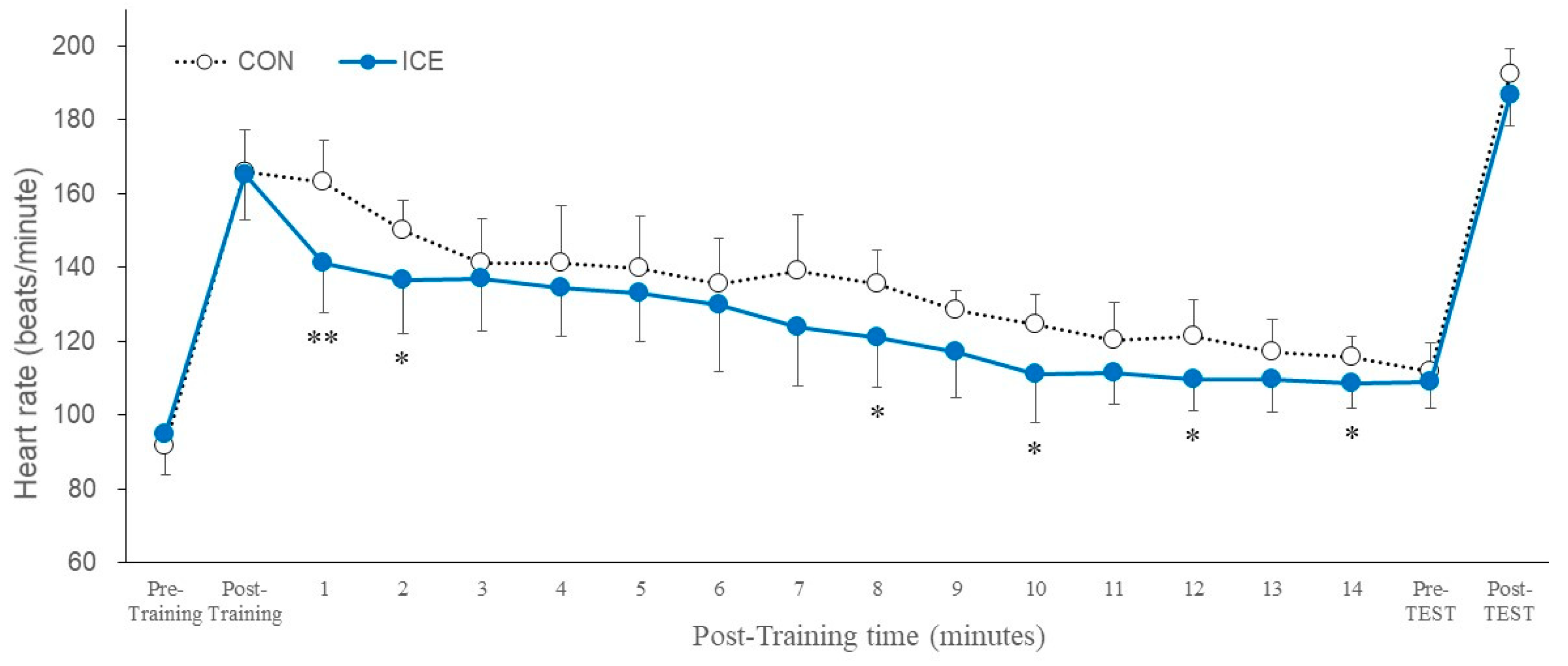
3.3. Heart Rate
3.4. Rating of Perceived Exertion
3.5. Physical Performance Test
3.6. Intensity of Locomotion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gauer, R.; Meyers, B.K. Heat-Related Illnesses. Am. Fam. Physician 2019, 99, 482–489. [Google Scholar] [PubMed]
- Knochel, J.P. Heat Stroke and Related Heat Stress Disorders. Dis. Mon. 1989, 35, 301–377. [Google Scholar] [PubMed]
- Périard, J.D.; Travers, G.J.S.; Racinais, S.; Sawka, M.N. Cardiovascular Adaptations Supporting Human Exercise-Heat Acclimation. Auton. Neurosci. 2016, 196, 52–62. [Google Scholar] [CrossRef]
- González-Alonso, J.; Teller, C.; Andersen, S.L.; Jensen, F.B.; Hyldig, T.; Nielsen, B. Influence of Body Temperature on the Development of Fatigue during Prolonged Exercise in the Heat. J. Appl. Physiol. 1999, 86, 1032–1039. [Google Scholar] [CrossRef] [PubMed]
- Racinais, S.; Alonso, J.M.; Coutts, A.J.; Flouris, A.D.; Girard, O.; González-Alonso, J.; Hausswirth, C.; Jay, O.; Lee, J.K.W.; Mitchell, N.; et al. Consensus Recommendations on Training and Competing in the Heat. Br. J. Sports Med. 2015, 49, 1164–1173. [Google Scholar] [CrossRef] [PubMed]
- Adams, W.M.; Hosokawa, Y.; Casa, D.J. Body-Cooling Paradigm in Sport: Maximizing Safety and Performance During Competition. J. Sport Rehabil. 2016, 25, 382–394. [Google Scholar] [CrossRef] [PubMed]
- Maley, M.J.; Minett, G.M.; Bach, A.J.E.; Zietek, S.A.; Stewart, K.L.; Stewart, I.B. Internal and External Cooling Methods and Their Effect on Body Temperature, Thermal Perception and Dexterity. PLoS ONE 2018, 13, e0191416. [Google Scholar] [CrossRef] [PubMed]
- Douzi, W.; Dugué, B.; Vinches, L.; Al Sayed, C.; Hallé, S.; Bosquet, L.; Dupuy, O. Cooling during Exercise Enhances Performances, but the Cooled Body Areas Matter: A Systematic Review with Meta-Analyses. Scand. J. Med. Sci. Sports 2019, 29, 1660–1676. [Google Scholar] [CrossRef]
- Duffield, R.; Green, R.; Castle, P.; Maxwell, N. Precooling Can Prevent the Reduction of Self-Paced Exercise Intensity in the Heat. Med. Sci. Sports Exerc. 2010, 42, 577–584. [Google Scholar] [CrossRef]
- Kay, D.; Taaffe, D.R.; Marino, F.E. Whole-Body Pre-Cooling and Heat Storage during Self-Paced Cycling Performance in Warm Humid Conditions. J. Sports Sci. 1999, 17, 937–944. [Google Scholar] [CrossRef]
- Siegel, R.; Maté, J.; Watson, G.; Nosaka, K.; Laursen, P.B. Pre-Cooling with Ice Slurry Ingestion Leads to Similar Run Times to Exhaustion in the Heat as Cold Water Immersion. J. Sports Sci. 2012, 30, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Sleivert, G.G.; Cotter, J.D.; Roberts, W.S.; Febbraio, M.A. The Influence of Whole-Body vs. Torso Pre-Cooling on Physiological Strain and Performance of High-Intensity Exercise in the Heat. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2001, 128, 657–666. [Google Scholar] [CrossRef]
- Naito, T.; Haramura, M.; Muraishi, K.; Yamazaki, M.; Takahashi, H. Impact of Ice Slurry Ingestion During Break-Times on Repeated-Sprint Exercise in the Heat. Sports Med. Int. Open 2020, 4, E45–E52. [Google Scholar] [CrossRef] [PubMed]
- Morito, A.; Inami, T.; Hirata, A.; Yamada, S.; Shimomasuda, M.; Haramoto, M.; Kato, K.; Tahara, S.; Oguma, Y.; Ishida, H.; et al. Ice Slurry Ingestion Improves Physical Performance during High-Intensity Intermittent Exercise in a Hot Environment. PLoS ONE 2022, 17, e0274584. [Google Scholar] [CrossRef]
- Siegel, R.; Maté, J.; Brearley, M.B.; Watson, G.; Nosaka, K.; Laursen, P.B. Ice Slurry Ingestion Increases Core Temperature Capacity and Running Time in the Heat. Med. Sci. Sports Exerc. 2010, 42, 717–725. [Google Scholar] [CrossRef]
- Booth, J.; Marino, F.; Ward, J.J. Improved Running Performance in Hot Humid Conditions Following Whole Body Precooling. Med. Sci. Sports Exerc. 1997, 29, 943–949. [Google Scholar] [CrossRef]
- Choo, H.C.; Nosaka, K.; Peiffer, J.J.; Ihsan, M.; Abbiss, C.R. Ergogenic Effects of Precooling with Cold Water Immersion and Ice Ingestion: A Meta-Analysis. Eur. J. Sport Sci. 2018, 18, 170–181. [Google Scholar] [CrossRef]
- Yeo, Z.W.; Fan, P.W.P.; Nio, A.Q.X.; Byrne, C.; Lee, J.K.W. Ice Slurry on Outdoor Running Performance in Heat. Int. J. Sports Med. 2012, 33, 859–866. [Google Scholar] [CrossRef]
- Naito, T.; Nakamura, M.; Muraishi, K.; Eda, N.; Ando, K.; Takemura, A.; Akazawa, N.; Hasegawa, H.; Takahashi, H. In-Play Optimal Cooling for Outdoor Match-Play Tennis in the Heat. Eur. J. Sport Sci. 2022, 22, 326–335. [Google Scholar] [CrossRef]
- Misailidi, M.; Mantzios, K.; Papakonstantinou, C.; Ioannou, L.G.; Flouris, A.D. Environmental and Psychophysical Heat Stress in Adolescent Tennis Athletes. Int. J. Sports Physiol. Perform. 2021, 16, 1895–1900. [Google Scholar] [CrossRef]
- Nassis, G.P.; Brito, J.; Dvorak, J.; Chalabi, H.; Racinais, S. The Association of Environmental Heat Stress with Performance: Analysis of the 2014 FIFA World Cup Brazil. Br. J. Sports Med. 2015, 49, 609–613. [Google Scholar] [CrossRef] [PubMed]
- Read, D.; Weaving, D.; Phibbs, P.; Darrall-Jones, J.; Roe, G.; Weakley, J.; Hendricks, S.; Till, K.; Jones, B. Movement and Physical Demands of School and University Rugby Union Match-Play in England. BMJ Open Sport Exerc. Med. 2017, 2, e000147. [Google Scholar] [CrossRef] [PubMed]
- Heat Guidelines. Available online: https://passport.world.rugby/player-welfare-medical/medical-protocols-for-match-day-medical-staff/heat-guidelines/ (accessed on 3 October 2022).
- Bangsbo, J.; Iaia, F.M.; Krustrup, P. The Yo-Yo Intermittent Recovery Test: A Useful Tool for Evaluation of Physical Performance in Intermittent Sports. Sports Med. 2008, 38, 37–51. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.P.; Stokes, K.A.; Weston, L.; Trewartha, G. The Bath University Rugby Shuttle Test (BURST): A Pilot Study. Int. J. Sports Physiol. Perform. 2010, 5, 64–74. [Google Scholar] [CrossRef]
- Barber, S.; Pattison, J.; Brown, F.; Hill, J. Efficacy of Repeated Cold Water Immersion on Recovery After a Simulated Rugby Union Protocol. J. Strength Cond. Res. 2020, 34, 3523–3529. [Google Scholar] [CrossRef]
- Borg, G.A.V. Psychophysical Bases of Perceived Exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Adams, W.C.; Mack, G.W.; Langhans, G.W.; Nadel, E.R. Effects of Varied Air Velocity on Sweating and Evaporative Rates during Exercise. J. Appl. Physiol. 1992, 73, 2668–2674. [Google Scholar] [CrossRef]
- Du Bois, D.; Du Bois, E.F. A Formula to Estimate the Approximate Surface Area If Height and Weight Be Known. Nutrition 1989, 5, 303–311. [Google Scholar]
- Hettiarachchi, I.T.; Hanoun, S.; Nahavandi, D.; Nahavandi, S. Validation of Polar OH1 Optical Heart Rate Sensor for Moderate and High Intensity Physical Activities. PLoS ONE 2019, 14, e0217288. [Google Scholar] [CrossRef]
- Morito, A.; Inami, T.; Hirata, A.; Yamada, S.; Shimomasuda, M.; Kato, K.; Tahara, S.; Kohtake, N. Effect of Ingestion of Ice Slurry on the Sleep Quality of Rugby Union Players in the Summer Season. Physiologia 2022, 2, 46–54. [Google Scholar] [CrossRef]
- Nakazaki, K.; Kitamura, S.; Motomura, Y.; Hida, A.; Kamei, Y.; Miura, N.; Mishima, K. Validity of an Algorithm for Determining Sleep/Wake States Using a New Actigraph. J. Physiol. Anthropol. 2014, 33, 31. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Nakamura, D.; Yasumatsu, M.; Takahashi, H. Effect of Ice Slurry Ingestion on Core Temperature and Blood Pressure Response after Exercise in a Hot Environment. J. Therm. Biol. 2021, 98, 102922. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Nakao, K.; Takahashi, N.; Son, S.Y.; Bakri, I.; Tochihara, Y. Validity of Infrared Tympanic Temperature for the Evaluation of Heat Strain While Wearing Impermeable Protective Clothing in Hot Environments. Ind. Health 2011, 49, 714–725. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Temiz, Y.; Taghavi, H.; Cornelius, E.L.; Mori, H.; Michel, B. An Earbud-Type Wearable (A Hearable) with Vital Parameter Sensors for Early Detection and Prevention of Heat-Stroke. In Proceedings of the 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; Volume 2019, pp. 7049–7055. [Google Scholar] [CrossRef]
- Masè, M.; Micarelli, A.; Falla, M.; Regli, I.B.; Strapazzon, G. Insight into the Use of Tympanic Temperature during Target Temperature Management in Emergency and Critical Care: A Scoping Review. J. Intensive Care 2021, 9, 43. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.A.S.; Tipton, M.J.; Kenny, G.P. Considerations for the Measurement of Core, Skin and Mean Body Temperatures. J. Therm. Biol. 2014, 46, 72–101. [Google Scholar] [CrossRef]
- Easton, C.; Fudge, B.W.; Pitsiladis, Y.P. Rectal, Telemetry Pill and Tympanic Membrane Thermometry during Exercise Heat Stress. J. Therm. Biol. 2007, 32, 78–86. [Google Scholar] [CrossRef]
- Onitsuka, S.; Nakamura, D.; Onishi, T.; Arimitsu, T.; Takahashi, H.; Hasegawa, H. Ice Slurry Ingestion Reduces Human Brain Temperature Measured Using Non-Invasive Magnetic Resonance Spectroscopy. Sci. Rep. 2018, 8, 2757. [Google Scholar] [CrossRef] [PubMed]
- Kiyatkin, E.A. Brain Temperature and Its Role in Physiology and Pathophysiology: Lessons from 20 Years of Thermorecording. Temperature 2019, 6, 271–333. [Google Scholar] [CrossRef]
- Ferreira, F.C.; Vaz Padilha, M.C.S.; Tobadini, E.; Carandina, A.; Montano, N.; da Silva Soares, P.P.; Rodrigues, G.D. The Interplay between Heated Environment and Active Standing Test on Cardiovascular Autonomic Control in Healthy Individuals. Physiol. Meas. 2021, 42, 085002. [Google Scholar] [CrossRef]
- Dehkharghani, S.; Fleischer, C.C.; Qiu, D.; Yepes, M.; Tong, F. Cerebral Temperature Dysregulation: MR Thermographic Monitoring in a Nonhuman Primate Study of Acute Ischemic Stroke. Am. J. Neuroradiol. 2017, 38, 712–720. [Google Scholar] [CrossRef]
- Onitsuka, S.; Zheng, X.; Hasegawa, H. Ice Slurry Ingestion before and during Exercise Inhibit the Increase in Core and Deep-Forehead Temperatures in the Second Half of the Exercise in a Hot Environment. J. Therm. Biol. 2020, 94, 102760. [Google Scholar] [CrossRef] [PubMed]
- Morito, A.; Yamada, S.; Shimomasuda, M.; Haramoto, M.; Nagai, W.; Takaoka, A.; Naito, T.; Saito, T.; Nakamura, M.; Kohtake, N. An Exploratory Study of Heat Stroke Biomarkers in Blood and Saliva in Healthy Male Adult Subjects—An Open-Label, Crossover Study. Jpn. Pharmacol. Ther. 2022, 50, 1041–1048. [Google Scholar]
- Deshayes, T.A.; De La Flore, A.; Gosselin, J.; Beliveau, J.; Jeker, D.; Goulet, E.D.B. The Impact of an Ice Slurry-Induced Gastrointestinal Heat Sink on Gastrointestinal and Rectal Temperatures Following Exercise. Sports 2019, 7, 198. [Google Scholar] [CrossRef] [PubMed]


| Variables | CON | ICE |
|---|---|---|
| Age, years | 19.1 ± 1.0 | 18.9 ± 0.7 |
| Height, m | 1.73 ± 0.06 | 1.71 ± 0.05 |
| Body mass, kg | 83.6 ± 8.7 | 84.1 ± 7.9 |
| BMI, kg/m2 | 28.1 ± 2.0 | 28.9 ± 3.6 |
| VO2 max, mL/kg/min | 45.6 ± 2.2 | 46.0 ± 3.3 |
| Group | Pre-Training | Post-Training | Pre-TEST | Post-TEST |
|---|---|---|---|---|
| CON | 10.1 ± 1.4 | 15.5 ± 1.4 | 14.9 ± 1.8 | 18.3 ± 1.2 |
| ICE | 10.4 ± 1.9 | 16.4 ± 1.3 | 15.4 ± 1.3 | 18.6 ± 0.5 |
| Group | Total Running Distance (m) | Total Running Time (min) |
|---|---|---|
| CON | 1095.0 ± 265.3 | 6.6 ± 1.6 |
| ICE | 1142.9 ± 394.5 | 6.9 ± 2.4 |
| Group | Training (Counts) | TEST (Counts) |
|---|---|---|
| CON | 1282.8 ± 111.7 | 238.9 ± 41.8 |
| ICE | 1306.1 ± 42.0 | 242.9 ± 74.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morito, A.; Inami, T.; Hirata, A.; Yamada, S.; Shimomasuda, M.; Kato, K.; Tahara, S.; Kohtake, N. Effect of Ice Slurry Ingestion on Post-Exercise Physiological Responses in Rugby Union Players. Physiologia 2022, 2, 154-163. https://doi.org/10.3390/physiologia2040013
Morito A, Inami T, Hirata A, Yamada S, Shimomasuda M, Kato K, Tahara S, Kohtake N. Effect of Ice Slurry Ingestion on Post-Exercise Physiological Responses in Rugby Union Players. Physiologia. 2022; 2(4):154-163. https://doi.org/10.3390/physiologia2040013
Chicago/Turabian StyleMorito, Akihisa, Takayuki Inami, Akihiro Hirata, Satoshi Yamada, Masatsugu Shimomasuda, Keita Kato, Shigeyuki Tahara, and Naohiko Kohtake. 2022. "Effect of Ice Slurry Ingestion on Post-Exercise Physiological Responses in Rugby Union Players" Physiologia 2, no. 4: 154-163. https://doi.org/10.3390/physiologia2040013
APA StyleMorito, A., Inami, T., Hirata, A., Yamada, S., Shimomasuda, M., Kato, K., Tahara, S., & Kohtake, N. (2022). Effect of Ice Slurry Ingestion on Post-Exercise Physiological Responses in Rugby Union Players. Physiologia, 2(4), 154-163. https://doi.org/10.3390/physiologia2040013






