Abstract
Healthcare-associated infections (HAIs), also referred to as nosocomial or hospital-acquired infections, are a significant cause of death worldwide, with hand hygiene being the most powerful means to tackle them. The present study had a twofold aim: first, to assess the level of knowledge and the degree of compliance with hand hygiene practices based on healthcare workers’ self-reports; second, to evaluate whether behavioral economics techniques, specifically a poster combining an image and an informational message, designed according to the published literature, can increase the level of healthcare workers’ compliance with hand hygiene. Factors that potentially affect compliance were also examined. This study involved distributing a questionnaire to healthcare workers in Greek public hospitals, from which 314 completed responses were collected during the last quarter of 2023. Participants were randomly and evenly assigned to an intervention group that received a nudging poster or to a control group, which did not. Self-reported compliance with hand hygiene practices was high, based on two latent variables derived through exploratory factor analysis, although knowledge of germ transmission was moderate, as reflected in the relevant knowledge question scores. However, nudging had no statistically significant effect on hand hygiene behavior. Compliance was associated with several factors, including gender, age, work experience, profession, perceived adequacy of available hygiene-related resources, and perceived consequences of nosocomial infections on patient outcomes.
1. Introduction
Healthcare-associated infections [1] increase morbidity and mortality, impose a financial burden on hospitals and society through prolonged hospital stays and higher treatment costs, and lead to unnecessary resource expenditure [2,3,4]. Research on HAI-related costs has shown that patients with HAIs may incur expenses up to 2.5 times higher than those without [5], can increase mean Diagnosis-Related Group (DRG) costs by 53.4% [6], and impose a greater burden of disability than major public health concerns, such as road traffic accidents [7].
In the countries of the European Union and European Economic Area (EU/EEA), it is estimated that more than 3.5 million cases of HAIs occur annually, leading to over 90,000 deaths and accounting for approximately 2.5 million disability-adjusted life years (DALYs); these figures exceed the cumulative burden of other infections including influenza and tuberculosis in the EU/EEA [8]. However, it is estimated that nearly half (~50%) of HAIs are considered preventable. In this context, implementing infection prevention and control measures in healthcare facilities is essential to reducing HAIs [8].
Regarding Greece, it is estimated that more than 400 DALYs per 100,000 population can be attributed to infections caused by resistant bacteria, a figure that is double that of the EU/EEA, which accounts for less than 200 DALYs per 100,000 population [9]. In fact, across all relevant studies from 2011 to 2012 onwards [10,11,12], Greece has consistently ranked among the EU countries with the highest prevalence of cases attributed to HAI.
The majority of HAIs are transmitted through direct contact, especially from the hands of healthcare workers (HCWs) [13]. Furthermore, as the hands of healthcare personnel are considered the main cause of pathogen transmission, proper hand hygiene is one of the most important preventive behaviors [14,15]. Globally, in the absence of specific improvement interventions, the average hand hygiene compliance rate is approximately 40%, rising to 60% in critical care facilities, such as intensive care units [14,16]. In Greece, recent data indicate that average compliance is around 55–60% [11].
Healthcare professionals are the cornerstone of the healthcare system and, therefore, have become the target group of efforts to reduce HAIs by strengthening compliance with hand hygiene practices. The contribution of healthcare workers is so important that the World Health Organization (WHO) designated May 5 as “World Hand Hygiene Day” to raise awareness [17]. A 17-month study by Sickbert–Bennett et al. (2016) showed that enhanced hand hygiene practices reduced nosocomial infection-related deaths and saved USD 5 million [18]. During COVID-19, hand hygiene compliance in high-income countries increased from 70% to 90.25% due to heightened awareness and stress among healthcare workers [19]. Nudging techniques in such a high compliance environment might not make much of a difference since, presumably, heightened awareness around hygiene makes extra reminders less necessary [20].
After the pandemic, however, studying healthcare workers’ attitudes towards patient safety and hand hygiene becomes once more vital for reducing infections, as it has been argued that the increase in hand hygiene compliance among healthcare workers during that period was temporary or dependent on the severity of each phase [21,22,23].
In fact, a problem healthcare workers face is a lack of time, as they are often under heavy, constant pressure to stick to strict protocols and simultaneously manage time efficiently to cope with the workload. These circumstances sometimes push hand hygiene down the list of priorities [24]. In this context, improving hand hygiene might be imperative since it is a simple, easy, and low-cost practice contributing substantially to reducing HAIs [25].
Various behavioral economic tools have been developed to improve healthcare workers’ compliance with hand hygiene, which is essential for preventing infections. Compliance might not always be achieved despite ongoing training, often due to high workloads [17,26]. Thus, creating an environment that encourages hand hygiene is crucial for maintaining safety and preventing the spread of infection [27].
Nudges, such as messages, images, posters (image and message combinations), and visual and environmental cues, are effective in increasing personnel and visitors’ compliance with hand hygiene in various healthcare contexts [15]. Nudges, recognized as a cost-effective method for promoting desired behaviors based on behavioral economics, have become an international trend in public health and hygiene compliance [28]. Its primary advantage is that it freely steers individual choices by modifying the choice architecture in which decisions are made while employing straightforward methods with minimal implementation costs [29]. Nudging enables individuals to choose freely and predictably, without altering economic incentives, intending to increase personal well-being and social welfare [30].
Many types of nudges have been assessed and used in healthcare, with varying degrees of success in different settings [15,31]. Healthcare workers seem to respond well to specific interventions and improve hand hygiene, like placement of antiseptic stations and visual reminders [32]. While visual cues and social norms are effective in other settings, they do not work well with healthcare professionals concerning hand hygiene [33]. One possible reason could be that visual cues exposed in every corner tend to become invisible to many health professionals and lose their effectiveness [34]. To address this issue, Birnbach (2017) suggested making these reminders more eye-catching by using bold colors, fonts, or unique designs to help them stand out in the often chaotic hospital environment [24]. A comparison of a nudge on nursing staff, reframing hand hygiene as a moment of care for the patient, and a boost, focusing on improving risk literacy, showed that they are both effective, with the nudge having a stronger immediate effect and the boost a longer-lasting one [29].
It has also been shown that providing data-driven feedback using technology, like hand hygiene tracking systems with gentle reminders such as eye images above antiseptic stations, improves compliance, especially for health professionals with heavy workloads [35,36,37,38]. An internal audit Finnish survey documented that continuous monitoring helps maintain higher compliance with WHO standards, albeit at a higher cost [39]. In contrast, implementing an automatic training system seems to improve hand hygiene technique but not compliance [40].
Behavior is crucial in an organization since healthcare staff shapes its safety culture. For instance, colleagues who consistently follow hand hygiene procedures act as role models for others to do the same [41]. Senior doctors or nurses can either inspire or mislead, as less experienced staff often copy what they see, even regarding hand hygiene [42,43]. Therefore, nudging, motivating, or educating staff may spread hand hygiene compliance within the healthcare facility.
The rationale for the present study stems from the fact that contextual differences are essential for the effectiveness of nudges [44]. Therefore, in the post-COVID era, we aim to provide evidence of the effectiveness of a poster nudge applied to healthcare workers who have a very heavy workload in Greek hospitals.
2. Materials and Methods
Using a questionnaire-based randomized experiment, we tested the hypothesis that a nudging intervention in the form of an image with an accompanying text message enhances healthcare workers’ compliance with hand hygiene protocols. Alongside compliance, we evaluated participants’ knowledge of key aspects of microbial transmission in healthcare settings. Compliance behavior was assessed by means of two latent constructs derived from exploratory factor analysis, and it was further examined for potential associations with a range of factors, including sociodemographic and professional characteristics.
This study was approved by the Research Ethics Committee of the University of Macedonia (protocol number: 34/22 June 2023) and the 4th Regional Health Authority (protocol number 45212/6 September 2023). The survey protocol involved questionnaire administration in four hospitals operating within its jurisdiction. All four hospitals were large public hospitals in Thessaloniki, the second-largest city in Greece and its co-capital. These hospitals accommodate approximately 44.8% of the beds in the hospitals of the 4th Regional Health Authority, serve 50.6% of hospitalized patients (with a representative case mix), account for 49.9% of hospitalization days, and receive 40.4% of patients examined in emergency departments and outpatient clinics [45].
Data collection occurred between October and December 2023. A total of 740 questionnaires were distributed to healthcare workers, who were approached either by e-mail or in person at their workplace. They were invited to complete the questionnaire online or return the paper version within two weeks. The online version was hosted on Google Forms. The questionnaire consisted of two parts: A and B. After completing part A, participants were asked to indicate their birth month. Based on this response, the online system automatically redirected those assigned to the intervention group (even-numbered birth months) to the nudge exposure section (including the related assessment question) before proceeding to part B (Figure 1). In contrast, participants in the control group (odd-numbered birth months) were directed straight to part B without access to the nudge section. The same procedure was applied to the paper version, where the birth month determined whether the respondent received the questionnaire with or without the nudge. The questionnaire content remained identical across groups, apart from including the nudge and its assessment in the intervention version. Participants were unaware that the questionnaire existed in two versions or that any group assignment would occur. No research team member had access to participant-identifying data; the Google Forms setting to collect email addresses was disabled, and informed consent was required before (anonymous) participation.
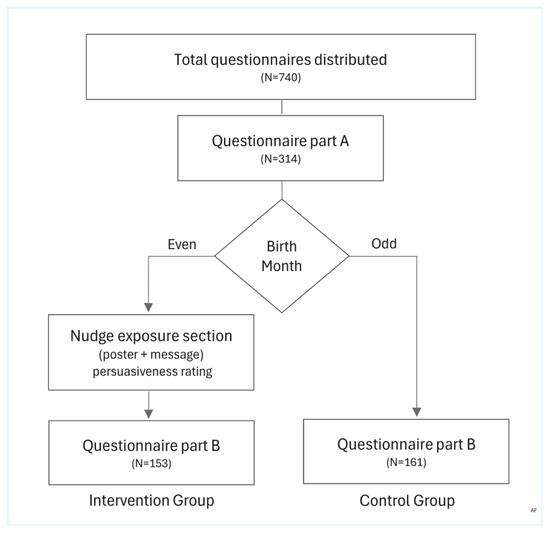
Figure 1.
Flowchart of the process, stages, and participant groups involved in distributing and collecting the study questionnaires.
The nudge consisted of a poster combining an image with text, aligned with the “use of messages and images” category described by Ledderer et al. (2020), who classified nudge interventions into eight categories to provide a coherent overview of push techniques [46].
The formulation of the questionnaire was based on existing studies and official guidelines and documents [47,48,49,50,51,52,53]. In particular, the items chosen were slightly adapted, mainly by paraphrasing or applying a different scale, in order to adjust them to the frame of our study. Demographic (gender, age, and education level) and job-related characteristics (years of work experience, profession) were gathered along with health background information (yes/no items: participant or family member belonging to a vulnerable group, own history of healthcare-associated infection, and family member’s history of healthcare-associated infection). In addition, two questions captured whether participants had received formal training on hand hygiene in the past three years (yes/no), as well as their perceptions of the adequacy of resources provided by the healthcare facility for hand hygiene, assessed on a 5-point Likert scale ranging from 1 (Not at all) to 5 (Very much).
Subsequently, five items were adapted from a WHO (2009) instrument that assessed participants’ knowledge of microbial transmission [53]. These items addressed the following: (K1) the most frequent sources of germs; (K2) the main route of cross-transmission of microbes between patients; (K3) hand hygiene actions preventing germ transmission to patients; (K4) hand hygiene actions preventing germ transmission to healthcare workers; and (K5) practices that should be avoided to prevent microbial colonization of the hands. Each item provided one or more answers, and participants were asked to select the options they considered accurate. Next, the degree of healthcare workers’ compliance with hand hygiene rules was measured using twelve items. A five-point Likert scale ranged from 1 (Never) to 5 (Always). The items included in this section of the questionnaire refer to the following: (C1) adherence to suitable hand hygiene practices at all times; (C2) reminding colleagues to follow hand hygiene rules; (C3) removing gloves after patient care (i.e., not reusing them between patients); (C4) hand cleaning before patient contact; (C5) hand cleaning after patient contact; (C6) hand cleaning after handling waste; (C7) hand cleaning before wearing gloves; (C8) hand cleaning after removing gloves; (C9) full compliance with the overall protocol; (C10) hand cleaning before contact with personal items; (C11) reminding patients to wash their hands after using the toilet; and (C12) showing greater motivation to comply with hand hygiene practices due to the impact of the COVID-19 pandemic.
The next section included three items designed to measure healthcare workers’ perceptions [54] of the significance of hand hygiene: (P1) perceived consequences of HAIs on patient health outcomes; (P2) perceived importance of hand hygiene in comparison to other patient safety issues; and (P3) perceived effectiveness of hand hygiene in preventing HAIs. A 5-point scale was used for measurement, with values ranging from 1 (Not at all) to 5 (Very much).
Next, respondents had to enter their birth month, which—as previously noted—served as the randomization criterion for their allocation to either the intervention or the control group. After this point, unlike the control group, only the intervention group was exposed to a nudge poster (Figure 2) accompanied by a text message. The latter read: “Your hands have the power to protect lives. Through diligent hand hygiene, you can ward off invisible threats and safeguard the vulnerable. With every act of hand hygiene, you contribute to building a healthier, safer world. Stand united with unwavering determination, knowing that your simple yet meaningful actions have the power to make a lasting impact.” The poster consisted of a central image depicting a hand with a microbial illustration in the palm, symbolizing the risk of pathogen transmission. It was headed by the core message “Clean Your Hands, Save Lives,” drawn from the relevant WHO campaign [55]. Surrounding the central image were four key statistics—both absolute and relative—on HAIs, sourced from the literature [8,56]. Additionally, the poster included motivational nudges such as: “It’s all in your hands”, “Protect Yourself and Others”, and “Contribute to increasing the compliance rate”.
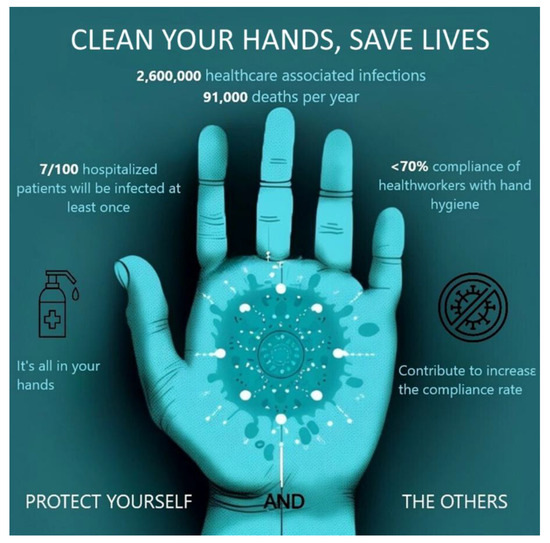
Figure 2.
Nudge poster alerting hospital staff about hand hygiene.
Because hand hygiene primarily protects patients, the messages were designed to reinforce personal responsibility and promote altruistic behavior [57]. This patient-oriented messaging approach was considered more effective, as focusing on the health of healthcare professionals may be subject to confirmation bias and, therefore, less impactful. Thus, it has been suggested that interventions in hand hygiene should focus on its consequences for others [29]. The messages conveyed by the poster fall into three categories [58] as the purpose of the combined poster design was primarily to attract attention, provide basic information (“informational”), raise awareness (“conscience-raising”), and influence healthcare workers to adopt more thorough hand hygiene practices (“instructional”). The significance of the accompanying message was to increase the motivation of healthcare workers through emotional appeal. The green background color of the poster was chosen for its positive association with success, as it aims to promote positive behaviors [59,60]. After being exposed to the poster, the respondents from the intervention group were asked a question to assess its persuasiveness, measured on a 5-point scale, ranging from 1 (not persuasive at all) to 5 (extremely persuasive).
Participants then proceeded to part B of the questionnaire, where they were asked to respond to twelve items (C1’–C12’) regarding compliance with hand hygiene. These items were essentially identical to the initial set (C1–C12), with the only difference being that the second set referred to participants’ future intention to comply (hereafter referred to as “Intended Compliance”) rather than their behavior at the time of the study (hereafter referred to as “Current Compliance”). It should be noted that this part B was completed by both groups, meaning all participants reported their intended compliance with hand hygiene rules in the near future, regardless of whether they had been exposed to the message (nudge) or not. A 5-point scale was again used, ranging from 1 (Never) to 5 (Always).
The final variable (S) measured the perceived importance of each participant’s (own) hand hygiene behavior in preventing the spread of HAIs. Again, a five-point scale was used, ranging from 1 (not important at all) to 5 (very important).
The data were statistically analyzed using IBM SPSS Statistics (version 26). A chi-square (χ2) test of independence was employed to examine whether randomization was successful by assessing potential differences in demographic and other characteristics between the intervention and control groups, whilst Kolmogorov–Smirnov normality tests were applied to determine possible normality of the data. Information on the questionnaire variables was summarized using descriptive statistics. Exploratory factor analysis using principal axis factoring with Promax rotation was conducted to derive scales from the twelve items measuring self-reported compliance. Reliability was assessed using Cronbach’s alpha coefficient, and values above 0.60 were considered acceptable. Spearman correlations with associated p-values, Mann–Whitney U, Wilcoxon signed-rank, and Kruskal–Wallis tests were used for statistical inference. Finally, linear regression models were applied to estimate the effects of nudging on the two constructed scales reflecting hospital staff hand hygiene behavior: Scale-1 (Hand Hygiene Behavior Near the Patient) and Scale-2 (General Hand Hygiene Behavior in the Hospital). The level of statistical significance was set at 5%.
3. Results
3.1. Final Full Sample
A total of 740 questionnaires were distributed, of which 314 were returned fully completed, yielding a response rate of 42.4%, with a distribution across professional categories that closely reflected the overall composition of healthcare personnel in public hospitals nationwide. Specifically, according to country-level data reported by the Hellenic Statistical Authority [61] for 2022, nursing staff accounted for 50.9%, medical staff 31.4%, allied health professionals (laboratory staff) 10.2%, and other staff 7.5%. In the present study, the corresponding figures were 53.8% for nursing staff, 26.8% for medical staff, 13.1% for laboratory staff, and 6.4% for other categories. This distribution across professions showed no significant deviation when considering all public hospitals nationwide, χ2 (3, N = 314) = 5.80, p = 0.122, or even when including both public and private hospitals, χ2 (3, N = 314) = 5.42, p = 0.121.
The sociodemographic and professional characteristics of the final full sample (N = 314) are presented in the first two columns of Table 1.

Table 1.
Characteristics of hospital employees in the intervention and control groups.
3.2. Descriptive Statistics of the Intervention and Control Groups
Regarding the distribution of participants between the two groups based on the parity (even- or odd-numbered) of their birth month, 153 were allocated to the intervention (nudge) group and 161 to the control group. The absolute and relative frequencies across the various characteristics and their (sub)categories are presented in the corresponding columns of Table 1.
No statistically significant differences between the two groups were indicated by chi-square (χ2) test results for all measured characteristics, confirming that randomization was successful. The vast majority of participants were women, and the most dominant age groups were healthcare employees in the 26–35 and 46–55 age ranges. Over one-third had postgraduate degrees, and more than half were nurses, with doctors constituting about one-fourth of the sample. Hospital participants had various working experiences, with more than 20 years of work being the most frequent category. For the remaining characteristics not included in Table 1, the proportions of participants exhibiting each characteristic across the combined groups are presented below, along with the p-values from chi-square (χ2) tests of independence, indicating whether statistically significant differences existed between the intervention and control groups. Specifically, a total of 27% of participants reported that they or a family member belonged to a vulnerable group (p = 0.197), 19.4% reported having been infected in a healthcare facility (p = 0.132), and 17.2% stated that a family member had been infected in a healthcare facility (p = 0.090). Additionally, 66.8% of participants had received formal training on hand hygiene in the past three years (p = 0.129). Furthermore, 58.3% of participants strongly believed that the hospital provided the necessary means for hand hygiene, 31.8% had a moderate view, and only 9.9% felt the resources were inadequate (p = 0.811).
Kolmogorov–Smirnov tests indicated that the questionnaire items did not follow a normal distribution (p < 0.05) and therefore appropriate descriptive statistics, factor analytic methods, and non-parametric inference tests were employed.
3.3. Knowledge of Microbial Transmission
Table 2 presents the descriptive statistics of the knowledge scores (N = 314) derived from questionnaire items (K1–K5) regarding microbial transmission. The overall mean score of 2.74 (out of 5.00) indicates that participants answered approximately 54.8% of the relevant questions correctly—a finding that reflects a moderate overall knowledge level of the participants. The mode value is 3.00, while the observed scores range from 0.75 to 5.00. The overall distribution appeared roughly symmetric (skewness = 0.06) and slightly platykurtic (kurtosis = −0.42). However, the results from formal normality tests (Kolmogorov–Smirnov p < 0.001; Shapiro–Wilk p = 0.003) showed a statistically significant deviation from the normal distribution. Bootstrap estimates showed minimal bias and narrow 95% confidence intervals, indicating strong reliability of the mean and standard deviation values.

Table 2.
Descriptive statistics of knowledge scores and normality test results.
The distribution of participants’ knowledge scores for the five questionnaire items (K1–K5) is presented in Table 3. Items K1 and K2 were single-answer multiple-choice questions, with correct response rates well below 50% (31.5% and 45.5%, respectively). The remaining items (K3–K5) were multipart yes/no questions, scored in 0.25-point increments based on the number of correct responses. Although fully correct responses were even less frequent (7.00%, 21.70%, and 37.30%), the highest proportion of participants scored above 50%, most commonly at the 0.75 level, followed by the 0.50 level.

Table 3.
Distribution of participant scores for knowledge items K1–K5.
To visualize the distribution of participants’ aggregated knowledge scores across the scoring range, Figure 3 presents a histogram overlaid with a boundary-corrected Epanechnikov kernel density estimate (KDE).
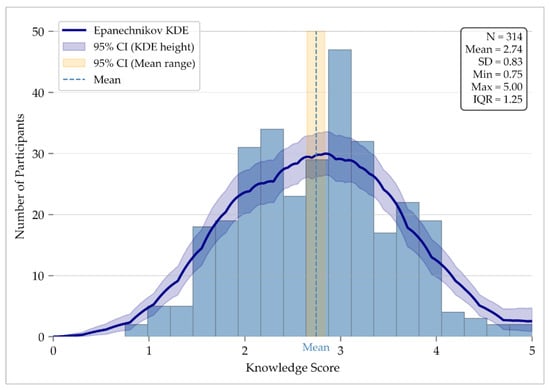
Figure 3.
Histogram of knowledge scores with a boundary-corrected Epanechnikov kernel density estimate (h = 0.70), scaled to participant counts and constrained to the 0–5 range. The blue band shows the pointwise 95% confidence interval derived from 2000 bootstrap resamples. The dashed line marks the sample mean, while the orange band shows its 95% confidence interval.
3.4. Development of Scales Measuring Self-Reported Compliance with Hand Hygiene Rules
Two scales meant to capture HCWs’ self-reported compliance with hand hygiene were derived using exploratory factor analysis on the twelve relevant items (C1–C12). Items with factor loadings > 0.50 and at least 0.20 higher than cross-loadings were retained. The Kaiser–Meyer–Olkin (KMO) value of sampling adequacy was high (0.868), and Bartlett’s test was significant (p < 0.001), confirming the data’s suitability. The two resulting factors explained 45.18% of the total variance. Table 4 presents the item loadings along with the corresponding Cronbach’s alpha coefficients. The two factors—named and hereafter referred to as Scale-1 (Hand Hygiene Behavior Near the Patient) and Scale-2 (General Hand Hygiene Behavior in the Hospital)—demonstrate adequate internal consistency and are conceptually meaningful, reflecting underlying latent variables regarding compliance with hand hygiene in the context of patient contact, when this is performed closely (directly) or more distantly (indirectly), proxied by the former and the latter, respectively.

Table 4.
Scales measuring self-reported compliance with hand hygiene, associated factor loadings, and Cronbach’s reliability coefficients.
The frequency distributions of the composite scores of the two scales are depicted in the overlaid graphs of Figure 4. Scale-1 scores are positively skewed, with a peak frequency at the maximum value (5.00), indicating a strong concentration of high self-reported hygiene behavior near the patient. In contrast, Scale-2 scores follow a more symmetrical, bell-shaped distribution, with the highest frequencies occurring between 3.67 and 4.00. The contrast in shape and central tendency between the two scales is clearly illustrated in the superimposed polygon curves: Scale-1 demonstrates limited dispersion and a strong mode at the upper end, whereas Scale-2 reflects greater variability and lower average adherence.
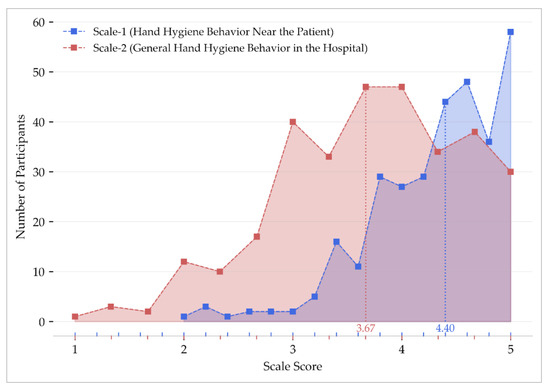
Figure 4.
Frequency distribution of composite scores for the two hand hygiene scales. Polygonal curves with shaded areas depict the overall score distribution. Square markers show frequencies at each score, and vertical dotted lines indicate median values.
3.5. Healthcare Workers’ Compliance with Hand Hygiene Rules
Table 5 presents the medians, interquartile ranges, and minimum and maximum values for both derived scales (Scale-1 and Scale-2), as well as for the four individual items (C1, C6, C7, and C12) that were not assigned to either factor due to low factor loadings. The table is further complemented by three questionnaire items (P1, P2, and P3) assessing healthcare workers’ perceptions of the significance of hand hygiene and the final item (S) addressing the perceived importance of personal contribution to HAI prevention.

Table 5.
Descriptive statistics for scales and items.
The numerical values in Table 5 indicate a high level of self-reported compliance for both Scale-1 and Scale-2, with the former (Hand Hygiene Behavior Near the Patient) clearly in the lead. The latter (General Hand Hygiene Behavior in the Hospital) follows closely, exhibiting a score well above moderate, reflecting a high degree of compliance. More specifically, the high median score (4.40) of Scale-1 in conjunction with its narrow interquartile range (0.80) reveals a strong degree and consistency of self-reported compliance regarding patient-proximal contexts. Meanwhile, the lower median (3.67) and wider variability (IQR = 1.33) of Scale-2 indicate that relevant practices are weaker and less uniformly followed across broader clinical aspects. Finally, the bootstrapped 95% confidence intervals support the precision of both estimates. The remaining four individual items not assigned to either scale due to low factor loadings reveal varying patterns of behavior: item C6 (cleaning hands after handling waste) demonstrates near-universal compliance, with a median of 5 and no variability, while C1 (adherence at all times) and C12 (COVID-19-related motivation) show high but more variable scores (medians of 4, IQRs of 1). Interestingly, item C7 (cleaning hands before glove application) exhibits the lowest median (3). The three perception-related items (P1–P3) consistently score highly (medians 4–5, IQRs = 1), reflecting clear agreement on the critical role of hand hygiene in protecting patients and controlling infections. Finally, item S, which addresses perceived self-contribution to HAI prevention, is rated uniformly high (median = 5, minimal variability), reflecting a well-established sense of personal responsibility.
Regarding the frequency distribution of Likert scale points for the individual item components of the two scales, the heatmap of Figure 5 illustrates meaningful trends in how healthcare workers understand and describe their hygiene-related behaviors between the two separate dimensions. In the first group of items (Scale-1—Hand Hygiene Behavior Near the Patient), most responses cluster at the upper end of the Likert scale, especially in C3, C5, and C8, indicating that staff follow hand-cleaning rules closely during patient care. Questions C4 and C9 also show good adherence, although the answers are more spread out, which may point to inconsistencies before patient contact or after removing gloves. On the other hand, responses to Scale-2 (General Hand Hygiene Behavior in the Hospital) are more mixed. While C10 suggests that most participants stick to their daily hygiene routines, C2 and C11, which involve reminding colleagues or patients, show fewer high responses, which may indicate that professionals are more confident managing their hygiene than speaking up about others’ practices, which might be a valuable target for future improvement efforts.
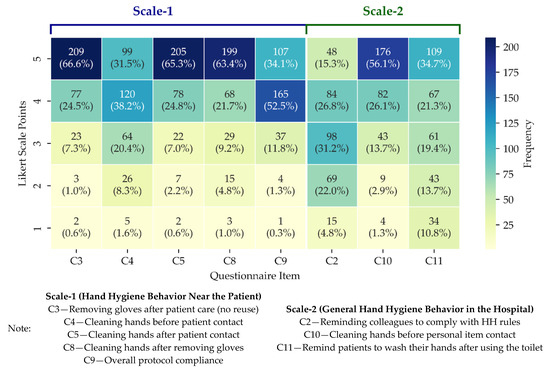
Figure 5.
Heatmap of response frequencies for Scale-1 and Scale-2 items. Each cell shows the count and column-wise percentage for each Likert point. Darker shades indicate higher frequencies.
3.6. The Effectiveness of Nudging on Hand Hygiene Behavior
The difference between participants’ stated compliance with hand hygiene rules at the time of the study (Current Compliance) and their stated intention to comply in the near future (Intended Compliance) is shown for both scales in Table 6 for the intervention and control groups.

Table 6.
Median scores of Current and Intended Compliance, and medians of within-group paired differences (Intended–Current) across intervention and control groups for the two hygiene behavior scales.
The Wilcoxon non-parametric signed-rank test indicated a statistically significant difference between Current Compliance and Intended Compliance for both groups (intervention and control) on both scales (Scale-1 and Scale-2).
Subsequently, to assess whether the nudge (poster) was effective, we examined, for both scales, whether the difference between Current Compliance and Intended Compliance (Table 6) differed significantly between the two groups (intervention and control). To this end, the Mann–Whitney test was employed, which revealed no significant difference between the groups for either Scale-1 (p = 0.123) or Scale-2 (p = 0.694). Therefore, our analysis does not support the main hypothesis that healthcare workers’ compliance behavior would improve after exposure to a nudging poster. It should be noted, however, that the perceived persuasiveness of the nudge poster, reported by those who saw it (i.e., the intervention group), was high (median rating = 4, indicating a “very persuasive” message). Yet it did not appear sufficient to alter participants’ future intentions toward closer compliance with hand hygiene practices to a significantly higher degree compared to those who did not see it (i.e., the control group).
3.7. Factors Affecting Hand Hygiene Behavior and Nudging Effect
Spearman’s correlations revealed a positive association between perceived adequacy of hygiene resources and compliance on both scales (Scale-1: ρ = 0.247, p < 0.001; Scale-2: ρ = 0.225, p < 0.001). Compliance was also positively related to the perceived importance of hand hygiene compared to other safety issues (Scale-1: ρ = 0.295, p < 0.001; Scale-2: ρ = 0.281, p < 0.001), its effectiveness in preventing infections (Scale-1: ρ = 0.225, p < 0.001; Scale-2: ρ = 0.232, p < 0.001), and the role of individual behavior (Scale-1: ρ = 0.273, p < 0.001; Scale-2: ρ = 0.266, p < 0.001). No significant correlation was found between perceived infection consequences and compliance (Scale-1: ρ = 0.013, p = 0.822; Scale-2: ρ = 0.070, p = 0.218).
Kruskal–Wallis tests showed no significant link between work experience and Scale-1 (p = 0.239), but Scale-2 scores differed significantly (p = 0.009), with post hoc analysis indicating higher compliance in those with >21 years vs. <5 years (p = 0.006). Profession was significantly associated with both scales (p < 0.001). Doctors reported lower compliance compared to nurses and other staff (Scale-1: p < 0.001; Scale-2: p = 0.001) and scored lower than lab staff on Scale-2 (p = 0.010). Age was also significant (Scale-1 and Scale-2: p < 0.001). Participants aged 26–35 scored lower than all older groups (p < 0.001); those aged 20–25 scored lower than participants >56 (Scale-1: p = 0.039; Scale-2: p = 0.011).
Mann–Whitney tests showed that female participants reported slightly higher compliance (Scale-1: p = 0.010; Scale-2: p = 0.015). Median scores for women were 4.4 (Scale-1) and 4.0 (Scale-2), compared to 4.2 and 3.67 for men. No significant associations were found with education (p = 0.923; p = 0.996), vulnerability due to health status (p = 0.264; p = 0.186), personal (p = 0.081; p = 0.899) or family history of HAIs (p = 0.981; p = 0.793), or prior hand hygiene training (p = 0.703; p = 0.708).
Lastly, the findings of the multivariate analysis are presented in Table 7. It is evident that, among all variables, only age was found to have a statistically significant (positive) effect on the dependent variables in both models. More specifically, hospital employees aged 26–35 appear to exhibit a greater intended positive change in hand hygiene behavior compared to their counterparts in other age groups. The findings also indicate that the month of birth (“Group” in Table 7)—that is, whether a healthcare worker belonged to the nudged group (intervention) or to the group that was not exposed to the poster (control)—does not influence the difference between Current Compliance (as reported up to the time of the study) and Intended Compliance (as reported for the near future) with hand hygiene rules. This implies that, within the scope of the present analysis, nudging was not associated with a statistically significant effect on stated behavior.

Table 7.
Regression analyses for the difference between Intended and Current Compliance with hand hygiene rules: Model 1 pertains to Hand Hygiene Behavior Near the Patient; Model 2 pertains to General Hand Hygiene Behavior in the Hospital.
4. Discussion
Healthcare-associated infections (HAIs) continue to pose a major global challenge, prompting policy efforts to reduce their incidence through behavioral interventions, particularly among healthcare workers who play a critical role in infection control [27]. This study had two primary objectives. First, it assessed hospital employees’ self-reported compliance with routine hand hygiene practices, as well as their knowledge of key principles related to microbial transmission within the hospital setting. Second, it evaluated whether a nudge-based intervention—consisting of a poster and an accompanying message aligned with official recommendations—could positively influence hygiene-related behavior in the short term.
To address these aims, we conceptualized two distinct dimensions of self-reported compliance: “Hand Hygiene Behavior Near the Patient” (Scale-1), which focuses on practices immediately preceding or following patient contact, and “General Hand Hygiene Behavior in the Hospital” (Scale-2), which reflects broader, routine hygiene behaviors throughout the clinical environment. The results indicated high baseline levels of compliance (Current Compliance), with participants anticipating even higher adherence in the near future (Intended Compliance). However, both the intervention and control groups demonstrated similar changes over time, suggesting that the observed increases were not clearly attributable to the nudge intervention.
These relatively high self-reported compliance levels may have been influenced by the recent pandemic, which contributed to improved compliance with safety protocols [62]. In Greece, hand hygiene compliance among HCWs was reported at approximately 33% before the COVID-19 pandemic [63,64], increasing to 50–60% during the following period [11]. The pandemic emerged as a significant motivator for HCWs’ compliance with safety protocols, driven by persistent media coverage, fear of virus transmission, and an elevated risk perception, especially due to direct patient contact [19]. Interestingly, an outlier among the individual findings was the low compliance with “hand cleaning before using gloves,” which showed the lowest median among all compliance items. Although somewhat surprising, this finding can be explained by the ongoing confusion surrounding the topic, even after the pandemic; some HCWs continue to use gloves as a substitute for hand hygiene, mistakenly believing that gloves alone are sufficient to prevent the spread of microorganisms [65,66,67,68]. Despite its specificity, this finding holds value, as it could be used to trigger a review and steps to address this important gap in practice.
Beyond the pandemic, participation in formal hand hygiene training, as reported by two-thirds of participants, may also have contributed to high self-reported compliance—an observation consistent with other studies linking compliance to prior training [69,70]. However, despite this training and elevated self-reported compliance, the average knowledge level was only slightly above the midpoint (54.8%), with just 28.6% of responses fully correct, meaning that 71.4% contained at least one incorrect selection. Only 22.0% answered all components correctly in multiple selection questions, revealing that four out of five HCWs could not cope with questions in areas requiring knowledge involving multiple preventive actions.
This apparent inconsistency—where training does not necessarily translate into comprehensive knowledge—has also been recorded elsewhere. A related study, for example, found that although nearly 90% of nurses had received recent training, their knowledge remained insufficient. Interestingly, the same study noted that these knowledge gaps did not significantly affect compliance, which remained high, with a mean score of 4.3 out of 5.0 [69]. Research shows that official programs of training do not always lead to better-educated personnel [71], and even greater knowledge does not automatically result in better compliance [72,73]. Medical students, for instance, reported better hand hygiene practices than resident physicians, despite having lower knowledge, indicating that parameters beyond knowledge influence behavior [74]. Therefore, combining cognitive, emotional, and behavioral methods with motivational approaches may be more effective [75,76].
Resource availability also affects compliance. Six out of ten participants were very satisfied with the hygiene supplies, three were moderately satisfied, and one rated availability as poor. Greater adequacy of such resources was associated with higher compliance on both scales. Previous studies have also linked resource adequacy and satisfaction to improved compliance [47,72,77]. Additionally, the quality level of hand hygiene products, as well as their accessibility and closeness to the point of patient care or treatment, has also been recognized as an important factor [77,78].
Encouragingly, the hospital staff appear to recognize the serious impact of healthcare-associated infections on patient outcomes, the importance of hand hygiene in comparison to other safety issues in preventing infections, the effectiveness of hand hygiene in reducing hospital-acquired infections, and the significance of their own behavior in tackling them. Greater awareness is often linked to better compliance, and many healthcare workers view hand hygiene not only as a professional responsibility but also as a moral obligation [43].
Associations between compliance and sociodemographic characteristics are also worth noting. Women reported slightly higher compliance than men, possibly due to early habits or a greater tendency toward socially acceptable behaviors [79] and a greater tendency to follow socially accepted behaviors [80]. Though younger professionals often display better attitudes [81], those aged 26–35 in our study reported lower compliance, suggesting that the age–behavior relationship is not linear. In line with previous research, physicians had the lowest compliance, likely due to limited hand hygiene training in medical education [82,83,84]. This result is consistent with earlier studies, which report higher compliance among nurses than physicians following either push interventions [32] or more general hygiene programs and guidelines [64,85,86,87,88,89].
As for professional experience, participants with more years of experience reported greater adherence to Scale-2, while Scale-1 compliance was consistent across experience levels. Generally, staff with greater experience tend to be more systematic in following hygiene protocols [90]. According to our findings, other factors, such as postgraduate education, belonging to a vulnerable group, or prior infection experience, did not significantly affect compliance, although earlier studies found some associations [91].
Regarding the effectiveness of the nudge, our results showed no significant difference between the intervention and control groups in self-reported change from Current Compliance to Intended Compliance, even though the nudge poster itself was rated as highly persuasive by participants in the intervention group. The difference measured 0.20 and 0.33 points (out of 5) for Scale-1 and Scale-2, respectively, translating into anticipated improvements of ~4.5% and ~9%. These figures are reasonable, given the already high baseline compliance, which naturally limits the margin for further improvement.
Additionally, the compliance assessment method may have influenced the results, as self-reports and direct observations often lead to different outcomes. HCWs may overestimate or underestimate their compliance because of social desirability pressures or misjudgment of their own behavior, potentially causing a mismatch between observed and self-reported hand hygiene practices [73,92,93,94]. While overt observation is considered more objective, it should not be overlooked that it is also affected by the Hawthorne effect, where awareness of being observed increases compliance during observation periods [73,77,93]. Face-to-face feedback may also trigger similar changes in behavior for the same reason [19].
Still, a few likely explanations could clarify the intervention’s limited impact. Healthcare workers may have become indifferent to posters due to frequent exposure. The topic is often discussed, and participants may feel well-informed. Additionally, completing the questionnaire might have acted as a reminder in itself, diminishing the distinct effect of the poster. This could explain why Intended Compliance increased similarly in both groups. Future studies could explore reminder-based activities where healthcare workers revisit essential hygiene principles and reflect on their practices over time.
Although our specific intervention yielded no measurable effect, poster-based nudges can still be useful, depending on context. Research from other countries suggests that visual prompts can support compliance [95]. While visual nudges may prove effective in some settings, they may have limited impact in others, highlighting the need for varied approaches within a broader strategy that includes resource availability, managerial support, and tailored messaging [24]. A co-design approach involving end-users may also have enhanced the impact of the nudge [66].
In conclusion, while nudges have been widely promoted and can enhance hand hygiene [15], our findings—based on a sample from public Greek hospitals—suggest that the specific nudge used was ineffective, reinforcing the view that nudges must be context-sensitive and supported by enabling conditions. Even when posters act as reminders in certain settings, their impact may be limited if functional antiseptic stations are not placed near patients, especially in hospital environments where the prevailing healthcare culture, high patient load, staff shortages, heavy workloads, and routine tasks reduce attention to standard hand hygiene practices [72,91,96,97].
Looking ahead, encouraging hand hygiene through role modeling and combining it with education may help improve compliance [21]. While several interventions—nudges, feedback, posters, accessible hand rubs, and multimodal strategies—have shown effectiveness in some settings [88,95,96], it remains unclear which strategy or combination works best [13,36,37,38,39]. Emerging AI-driven nudges show promise, with studies reporting up to 30% improvement in compliance, as machine learning systems can detect non-compliance trends and deliver personalized prompts during critical moments [98].
Despite the randomized design, this study has certain limitations. The sample came from a representative but relatively small number of public hospitals, so generalizing the findings should be done with caution, following a decreasing scale of confidence—from the prefecture to the Regional Health Authority, to the national level. Furthermore, the response rate of 42.4% observed in this study is considered moderate; however, this limitation appears to be a broader issue rather than a shortcoming specific to this study’s methodology, as it lies within the range of rates typically reported in survey-based research targeting healthcare personnel, which often range from 35% to 53% [99,100,101,102]. A gradual decline in response rates has been noted in recent decades. This level of participation may be attributed to the heavy workload, limited time availability, and survey fatigue experienced by healthcare professionals, particularly those in demanding roles [103]. Still, despite the moderate response rate, the representativeness of the sample across the nationwide distribution of professional categories—verified by a χ2 test, as shown in Section 3—helps mitigate this shortcoming and supports the credibility of this study’s findings. Additionally, this study did not assess long-term effects or include objective indicators, such as actual disinfectant use, relying instead on self-reported intentions.
Building on these findings, future research should explore how visual (e.g., color, imagery) and textual (e.g., clarity, tone) elements affect staff engagement across settings. Tracking disinfectant use before and after interventions could offer more grounded insights. Tools such as real-time monitoring or automatic reminders may help adapt interventions to each hospital’s needs. Finally, understanding when and why nudges succeed in different facilities should be a research priority, as they may contribute to improving safety, effectiveness, and efficiency in infection control.
5. Conclusions
Evaluating the effectiveness of nudges before applying them in real-world healthcare policy is essential, as success is not guaranteed in every setting. This study used a questionnaire to assess basic knowledge of microbial transmission and self-reported hygiene compliance, comparing a nudged group (via poster) to a control group. The results showed moderate knowledge and high reported compliance in direct patient care, with slightly lower—but still high—compliance in general hospital hygiene. Doctors reported lower compliance, and several factors were found to influence behavior.
Although overall compliance was high, the specific nudge did not produce a statistically significant additional effect. This may be due to already high baseline compliance or time pressure in a demanding hospital environment. It is also possible that the poster lacked impact, as staff are frequently exposed to similar hygiene messages, which could reduce responsiveness. If further improvement is needed, future research should explore and compare alternative nudging techniques, such as boosting or personalized approaches, along with their cost-effectiveness, to better inform policy decisions.
Author Contributions
Conceptualization, V.A., S.S. and D.A.N.; methodology, V.A., S.S. and A.F.; investigation: S.S.; formal analysis, V.A., S.S. and A.F.; writing—original draft preparation, S.S. and A.F.; writing—review and editing, V.A. and D.A.N.; resources: S.S.; supervision, V.A. and D.A.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Research Ethics Committee of the University of Macedonia (protocol number: 34/22 June 2023) as well as the 4th Regional Health Authority (protocol number 45212/6 September 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request.
Acknowledgments
We would like to thank Dimitris Tsalikakis, the 4th Regional Health Authority, and the Hospital Managers for approving and facilitating this research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. The Burden of Health Care-Associated Infection Worldwide. Available online: https://www.who.int/news-room/feature-stories/detail/the-burden-of-health-care-associated-infection-worldwide (accessed on 2 April 2025).
- Gidey, K.; Gidey, M.T.; Hailu, B.Y.; Gebreamlak, Z.B.; Niriayo, Y.L. Clinical and Economic Burden of Healthcare-Associated Infections: A Prospective Cohort Study. PLoS ONE 2023, 18, e0282141. [Google Scholar] [CrossRef]
- Li, P.; Li, Y.; Zhang, Y.; Bao, J.; Yuan, R.; Lan, H.; Sun, M. Economic Burden Attributable to Healthcare-Associated Infections in Tertiary Public Hospitals of Central China: A Multi-Centre Case-Control Study. Epidemiol. Infect. 2022, 150, e155. [Google Scholar] [CrossRef] [PubMed]
- Luangasanatip, N.; Hongsuwan, M.; Lubell, Y.; Limmathurotsakul, D.; Srisamang, P.; Day, N.P.J.; Graves, N.; Cooper, B.S. Cost-Effectiveness of Interventions to Improve Hand Hygiene in Healthcare Workers in Middle-Income Hospital Settings: A Model-Based Analysis. J. Hosp. Infect. 2018, 100, 165–175. [Google Scholar] [CrossRef]
- Thi Anh Thu, L.; Thi Hong Thoa, V.; Thi Van Trang, D.; Phuc Tien, N.; Thuy Van, D.; Thi Kim Anh, L.; Wertheim, H.F.L.; Truong Son, N. Cost-Effectiveness of a Hand Hygiene Program on Health Care-Associated Infections in Intensive Care Patients at a Tertiary Care Hospital in Vietnam. Am. J. Infect. Control 2015, 43, e93–e99. [Google Scholar] [CrossRef]
- Orlando, S.; Cicala, M.; De Santo, C.; Mosconi, C.; Ciccacci, F.; Guarente, L.; Carestia, M.; Liotta, G.; Di Giovanni, D.; Buonomo, E.; et al. The Financial Burden of Healthcare-Associated Infections: A Propensity Score Analysis in an Italian Healthcare Setting. Infect. Prev. Pract. 2025, 7, 100406. [Google Scholar] [CrossRef] [PubMed]
- Morris, A.J.; Hensen, M.; Graves, N.; Cai, Y.; Wolkewitz, M.; Roberts, S.A.; Grae, N. The Burden of Healthcare-Associated Infections in New Zealand Public Hospitals 2021. Infect. Control Hosp. Epidemiol. 2024, 45, 1176–1182. [Google Scholar] [CrossRef]
- ECDC Healthcare-Associated Infections. Available online: https://www.ecdc.europa.eu/en/healthcare-associated-infections (accessed on 27 February 2025).
- Kopsidas, I.; Theodosiadis, D.; Triantafyllou, C.; Koupidis, S.; Fanou, A.; Hatzianastasiou, S. Preventing Antimicrobial Resistance and Promoting Appropriate Antimicrobial Use in Inpatient Health Care in Greece. Available online: https://www.who.int/europe/publications/i/item/WHO-EURO-2022-5837-45602-65411 (accessed on 27 February 2025).
- ECDC Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Acute Care Hospitals—2022–2023. Available online: https://www.ecdc.europa.eu/en/publications-data/PPS-HAI-AMR-acute-care-europe-2022-2023 (accessed on 27 February 2025).
- National Public Health Organization (NPHO) Findings from the Surveillance of Antimicrobial Resistance, Antibiotic Use, and Health Care-Associated Infections [In Greek]. 2023. Available online: https://eody.gov.gr/wp-content/uploads/2023/08/AMR-HAI-REPORT-EODY-28-8-2023.pdf (accessed on 20 February 2025).
- Suetens, C.; Latour, K.; Kärki, T.; Ricchizzi, E.; Kinross, P.; Moro, M.L.; Jans, B.; Hopkins, S.; Hansen, S.; Healthcare-Associated Infections Prevalence Study Group; et al. Prevalence of Healthcare-Associated Infections, Estimated Incidence and Composite Antimicrobial Resistance Index in Acute Care Hospitals and Long-Term Care Facilities: Results from Two European Point Prevalence Surveys, 2016 to 2017. Eurosurveillance 2018, 23, 1800516. [Google Scholar] [CrossRef]
- Gould, D.J.; Moralejo, D.; Drey, N.; Chudleigh, J.H.; Taljaard, M. Interventions to Improve Hand Hygiene Compliance in Patient Care. Cochrane Database Syst. Rev. 2017, 9, CD005186. [Google Scholar] [CrossRef]
- Stadler, R.N.; Tschudin-Sutter, S. What Is New with Hand Hygiene? Curr. Opin. Infect. Dis. 2020, 33, 327–332. [Google Scholar] [CrossRef]
- Tzikas, A.; Koulierakis, G. A Systematic Review of Nudges on Hand Hygiene against the Spread of COVID-19. J. Behav. Exp. Econ. 2023, 105, 102046. [Google Scholar] [CrossRef]
- World Health Organization. WHO Research for Hand Hygiene in Health Care 2023–2030: Summary. Available online: https://www.who.int/publications/i/item/9789240073715 (accessed on 4 March 2025).
- Lotfinejad, N.; Peters, A.; Tartari, E.; Fankhauser-Rodriguez, C.; Pires, D.; Pittet, D. Hand Hygiene in Health Care: 20 Years of Ongoing Advances and Perspectives. Lancet Infect. Dis. 2021, 21, e209–e221. [Google Scholar] [CrossRef] [PubMed]
- Sickbert-Bennett, E.E.; DiBiase, L.M.; Willis, T.M.S.; Wolak, E.S.; Weber, D.J.; Rutala, W.A. Reduction of Healthcare-Associated Infections by Exceeding High Compliance with Hand Hygiene Practices. Emerg. Infect. Dis. 2016, 22, 1628–1630. [Google Scholar] [CrossRef]
- Wang, Y.; Yang, J.; Qiao, F.; Feng, B.; Hu, F.; Xi, Z.-A.; Wu, W.; Ni, Z.-L.; Liu, L.; Yuan, Y. Compared Hand Hygiene Compliance among Healthcare Providers before and after the COVID-19 Pandemic: A Rapid Review and Meta-Analysis. Am. J. Infect. Control 2022, 50, 563–571. [Google Scholar] [CrossRef]
- Weijers, R.J.; de Koning, B.B.; Paas, F. Nudging in Education: From Theory towards Guidelines for Successful Implementation. Eur. J. Psychol. Educ. 2021, 36, 883–902. [Google Scholar] [CrossRef]
- Armstrong-Novak, J.; Juan, H.Y.; Cooper, K.; Bailey, P. Healthcare Personnel Hand Hygiene Compliance: Are We There Yet? Curr. Infect. Dis. Rep. 2023, 25, 123–129. [Google Scholar] [CrossRef]
- Moore, L.D.; Robbins, G.; Quinn, J.; Arbogast, J.W. The Impact of COVID-19 Pandemic on Hand Hygiene Performance in Hospitals. Am. J. Infect. Control 2021, 49, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Williams, V.; Kovacs-Litman, A.; Muller, M.P.; Hota, S.; Powis, J.E.; Ricciuto, D.R.; Mertz, D.; Katz, K.; Castellani, L.; Kiss, A.; et al. Impact of COVID-19 on Hospital Hand Hygiene Performance: A Multicentre Observational Study Using Group Electronic Monitoring. CMAJ Open 2021, 9, E1175–E1180. [Google Scholar] [CrossRef] [PubMed]
- Birnbach, D.J.; Rosen, L.F.; Fitzpatrick, M.; Everett-Thomas, R.; Arheart, K.L. A Ubiquitous but Ineffective Intervention: Signs Do Not Increase Hand Hygiene Compliance. J. Infect. Public Health 2017, 10, 295–298. [Google Scholar] [CrossRef]
- Kamanga, P.; Ngala, P.; Hebron, C. Improving Hand Hygiene in a Low-resource Setting: A Nurse-led Quality Improvement Project. Int. Wound J. 2021, 19, 482–492. [Google Scholar] [CrossRef]
- Scheithauer, S.; Batzer, B.; Dangel, M.; Passweg, J.; Widmer, A. Workload Even Affects Hand Hygiene in a Highly Trained and Well-Staffed Setting: A Prospective 365/7/24 Observational Study. J. Hosp. Infect. 2017, 97, 11–16. [Google Scholar] [CrossRef]
- Schmidtke, K.A.; Aujla, N.; Marshall, T.; Hussain, A.; Hodgkinson, G.P.; Arheart, K.; Marti, J.; Birnbach, D.J.; Vlaev, I. Using Environmental Engineering to Increase Hand Hygiene Compliance: A Cross-over Study Protocol. BMJ Open 2017, 7, e017108. [Google Scholar] [CrossRef]
- Murayama, H.; Takagi, Y.; Tsuda, H.; Kato, Y. Applying Nudge to Public Health Policy: Practical Examples and Tips for Designing Nudge Interventions. Int. J. Environ. Res. Public Health 2023, 20, 3962. [Google Scholar] [CrossRef]
- Van Roekel, H.; Reinhard, J.; Grimmelikhuijsen, S. Improving Hand Hygiene in Hospitals: Comparing the Effect of a Nudge and a Boost on Protocol Compliance. Behav. Public Policy 2022, 6, 52–74. [Google Scholar] [CrossRef]
- Thaler, R.H.; Sunstein, C.R. Nudge: Improving Decisions about Health, Wealth, and Happiness; Yale University Press: New Haven, CT, USA, 2008; ISBN 978-0-300-14681-3. [Google Scholar]
- Caris, M.G.; Labuschagne, H.A.; Dekker, M.; Kramer, M.H.H.; van Agtmael, M.A.; Vandenbroucke-Grauls, C.M.J.E. Nudging to Improve Hand Hygiene. J. Hosp. Infect. 2018, 98, 352–358. [Google Scholar] [CrossRef]
- Elia, F.; Calzavarini, F.; Bianco, P.; Vecchietti, R.G.; Macor, A.F.; D’Orazio, A.; Dragonetti, A.; D’Alfonso, A.; Belletrutti, L.; Floris, M.; et al. A Nudge Intervention to Improve Hand Hygiene Compliance in the Hospital. Intern. Emerg. Med. 2022, 17, 1899–1905. [Google Scholar] [CrossRef]
- Stella, S.A.; Stace, R.J.; Knepper, B.C.; Reese, S.M.; Keniston, A.; Burden, M.; Young, H.L. The Effect of Eye Images and a Social Norms Message on Healthcare Provider Hand Hygiene Adherence. Infect. Control Hosp. Epidemiol. 2019, 40, 748–754. [Google Scholar] [CrossRef]
- Sendall, M.C.; McCosker, L.K.; Halton, K. Cleaning Staff’s Attitudes about Hand Hygiene in a Metropolitan Hospital in Australia: A Qualitative Study. Int. J. Environ. Res. Public. Health 2019, 16, 1067. [Google Scholar] [CrossRef]
- Gaube, S.; Tsivrikos, D.; Dollinger, D.; Lermer, E. How a Smiley Protects Health: A Pilot Intervention to Improve Hand Hygiene in Hospitals by Activating Injunctive Norms through Emoticons. PLoS ONE 2018, 13, e0197465. [Google Scholar] [CrossRef]
- Iversen, A.-M.; Stangerup, M.; From-Hansen, M.; Hansen, R.; Sode, L.P.; Kostadinov, K.; Hansen, M.B.; Calum, H.; Ellermann-Eriksen, S.; Knudsen, J.D. Light-Guided Nudging and Data-Driven Performance Feedback Improve Hand Hygiene Compliance among Nurses and Doctors. Am. J. Infect. Control 2021, 49, 733–739. [Google Scholar] [CrossRef]
- Iversen, A.-M.; Hansen, M.B.; Alsner, J.; Kristensen, B.; Ellermann-Eriksen, S. Effects of Light-Guided Nudges on Health Care Workers’ Hand Hygiene Behavior. Am. J. Infect. Control 2023, 51, 1370–1376. [Google Scholar] [CrossRef] [PubMed]
- Nevo, I.; Fitzpatrick, M.; Thomas, R.-E.; Gluck, P.A.; Lenchus, J.D.; Arheart, K.L.; Birnbach, D.J. The Efficacy of Visual Cues to Improve Hand Hygiene Compliance. Simul. Healthc. J. Soc. Simul. Healthc. 2010, 5, 325–331. [Google Scholar] [CrossRef]
- Ojanperä, H.; Kanste, O.I.; Syrjala, H. Hand-Hygiene Compliance by Hospital Staff and Incidence of Health-Care-Associated Infections, Finland. Bull. World Health Organ. 2020, 98, 475–483. [Google Scholar] [CrossRef]
- Kwok, Y.L.A.; Callard, M.; McLaws, M.-L. An Automated Hand Hygiene Training System Improves Hand Hygiene Technique but Not Compliance. Am. J. Infect. Control 2015, 43, 821–825. [Google Scholar] [CrossRef]
- Dixit, D.; Hagtvedt, R.; Reay, T.; Ballermann, M.; Forgie, S. Attitudes and Beliefs about Hand Hygiene among Paediatric Residents: A Qualitative Study. BMJ Open 2012, 2, e002188. [Google Scholar] [CrossRef] [PubMed]
- Al-Maani, A.; Al Wahaibi, A.; Al-Zadjali, N.; Al-Sooti, J.; AlHinai, M.; Al Badawi, A.; Al Saidi, A.; AlZadjali, N.; Elshoubary, W.; Al-Harthi, K.; et al. The Impact of the Hand Hygiene Role Model Project on Improving Healthcare Workers’ Compliance: A Quasi-Experimental Observational Study. J. Infect. Public Health 2022, 15, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, M.; Rakhshanderou, S.; Safari-Moradabadi, A.; Barkati, H. Exploring Determinants of Hand Hygiene among Hospital Nurses: A Qualitative Study. BMC Nurs. 2020, 19, 109. [Google Scholar] [CrossRef]
- Sunstein, C.R. Nudges That Fail. Behav. Public Policy 2017, 1, 4–25. [Google Scholar] [CrossRef]
- Ministry of Health Bi-Health. Available online: https://www.moh.gov.gr/articles/bihealth/stoixeia-noshleytikhs-kinhshs (accessed on 2 April 2025).
- Ledderer, L.; Kjær, M.; Madsen, E.K.; Busch, J.; Fage-Butler, A. Nudging in Public Health Lifestyle Interventions: A Systematic Literature Review and Metasynthesis. Health Educ. Behav. 2020, 47, 749–764. [Google Scholar] [CrossRef]
- Ahmed, J.; Malik, F.; Memon, Z.A.; Bin Arif, T.; Ali, A.; Nasim, S.; Ahmad, J.; Khan, M.A. Compliance and Knowledge of Healthcare Workers Regarding Hand Hygiene and Use of Disinfectants: A Study Based in Karachi. Cureus 2020, 12, e7036. [Google Scholar] [CrossRef]
- Al-Anazi, S.; Al-Dhefeery, N.; Al-Hjaili, R.; Al-Duwaihees, A.; Al-Mutairi, A.; Al-Saeedi, R.; Al-Dhaen, R.; Al-Rabiah, S.; Sharaf-Alddin, R. Compliance with Hand Hygiene Practices among Nursing Staff in Secondary Healthcare Hospitals in Kuwait. BMC Health Serv. Res. 2022, 22, 1325. [Google Scholar] [CrossRef]
- CDC Guideline for Hand Hygiene in Healthcare Settings. 2002. Available online: https://www.cdc.gov/infection-control/hcp/hand-hygiene/index.html (accessed on 9 April 2025).
- Chitamanni, P.; Allana, A.; Hand, I. Quality Improvement Project to Improve Hand Hygiene Compliance in a Level III Neonatal Intensive Care Unit. Children 2023, 10, 1484. [Google Scholar] [CrossRef] [PubMed]
- Diwan, V.; Gustafsson, C.; Rosales Klintz, S.; Joshi, S.C.; Joshi, R.; Sharma, M.; Shah, H.; Pathak, A.; Tamhankar, A.J.; Stålsby Lundborg, C. Understanding Healthcare Workers Self-Reported Practices, Knowledge and Attitude about Hand Hygiene in a Medical Setting in Rural India. PLoS ONE 2016, 11, e0163347. [Google Scholar] [CrossRef]
- World Health Organization & WHO Patient Safety. WHO Guidelines on Hand Hygiene in Health Care; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- World Health Organization. Hand Hygiene Knowledge Questionnaire for Health-Care Workers; WHO: Geneva, Switzerland, 2009; Available online: https://cdn.who.int/media/docs/default-source/integrated-health-services-(ihs)/hand-hygiene/monitoring/surveyform/hand-hygiene-knowledge-questionnaire.doc?sfvrsn=dbb4da65_2 (accessed on 30 October 2024).
- World Health Organization. Perception Survey for Health-Care Workers; WHO: Geneva, Switzerland, 2009; Available online: https://cdn.who.int/media/docs/default-source/integrated-health-services-(ihs)/hand-hygiene/monitoring/surveyform/perception-survey-for-health-care-workers.doc?sfvrsn=8fa7cb79_2 (accessed on 30 October 2024).
- Tartari, E.; Kilpatrick, C.; Allegranzi, B.; Pittet, D. WHO SAVE LIVES: Clean Your Hands Campaign. Lancet Infect. Dis. 2022, 22, 577–579. [Google Scholar] [CrossRef] [PubMed]
- Stead, S.; Vogt, L.; Antons, D.; Salge, T.O.; Gecht, J.; Klasen, M.; Sopka, S. Hospital Resource Endowments and Nosocomial Infections: Longitudinal Evidence from the English National Health Service on Clostridioides Difficile between 2011 and 2019. J. Hosp. Infect. 2023, 134, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Jenner, E.A.; Jones, F.; Fletcher, B.C.; Miller, L.; Scott, G.M. Hand Hygiene Posters: Selling the Message. J. Hosp. Infect. 2005, 59, 77–82. [Google Scholar] [CrossRef]
- Jenner, E.A.; Jones, F.; Fletcher, B.C.; Miller, L.; Scott, G.M. Hand Hygiene Posters: Motivators or Mixed Messages? J. Hosp. Infect. 2005, 60, 218–225. [Google Scholar] [CrossRef]
- Moller, A.C.; Elliot, A.J.; Maier, M.A. Basic Hue-Meaning Associations. Emotion 2009, 9, 898–902. [Google Scholar] [CrossRef]
- Prasetyo, D.B.; Sofyan, L.; Muchtar, P.A.; Dewi, D.F. Nudging to Handwash during the Pandemic—The Use of Visual Priming and Salience. Anal. Soc. Issues Public Policy 2022, 22, 836–856. [Google Scholar] [CrossRef]
- Hellenic Statistical Authority. Hospital Census 2022; Hellenic Statistical Authority: Piraeus, Greece, 2024. [Google Scholar]
- Weijers, R.J.; De Koning, B.B. Nudging to Increase Hand Hygiene during the COVID-19 Pandemic: A Field Experiment. Can. J. Behav. Sci. Rev. Can. Sci. Comport. 2021, 53, 353–357. [Google Scholar] [CrossRef]
- Astrinaki, E.; Messaritaki, A.; Mourtou, E.; Niakas, D. Hand hygiene compliance in a Greek university hospital. Arch. Hell. Med. 2016, 33, 639–644. [Google Scholar]
- Kouni, S.; Mougkou, K.; Kurlaba, G.; Nteli, C.; Lourida, A.; Maroudi-Manta, S.; Zaoutis, T.; Coffin, S. P130: Assessment of Hand Hygiene Practices at the Two Children’s Hospitals in Greece. Antimicrob. Resist. Infect. Control 2013, 2, P130. [Google Scholar] [CrossRef]
- Moghnieh, R.; Soboh, R.; Abdallah, D.; El-Helou, M.; Al Hassan, S.; Ajjour, L.; Tamim, H.; Al Tabbah, S.; Nasreddine, W.; Mugharbil, A. Health Care Workers’ Compliance to the My 5 Moments for Hand Hygiene: Comparison of 2 Interventional Methods. Am. J. Infect. Control 2017, 45, 89–91. [Google Scholar] [CrossRef]
- Blair, C.-J.; McCrudden, C.; Brazier, A.; Huf, S.; Gregory, A.; O’Driscoll, F.; Galletly, T.; Leon-Villapalos, C.; Brown, H.; Clay, K.; et al. A Helping Hand: Applying Behavioural Science and Co-Design Methodology to Improve Hand Hygiene Compliance in the Hospital Setting. PLoS ONE 2024, 19, e0310768. [Google Scholar] [CrossRef]
- Fuller, C.; Savage, J.; Besser, S.; Hayward, A.; Cookson, B.; Cooper, B.; Stone, S. “The Dirty Hand in the Latex Glove”: A Study of Hand Hygiene Compliance When Gloves Are Worn. Infect. Control Hosp. Epidemiol. 2011, 32, 1194–1199. [Google Scholar] [CrossRef]
- CDC Clinical Safety: Hand Hygiene for Healthcare Workers. Available online: https://www.cdc.gov/clean-hands/hcp/clinical-safety/index.html (accessed on 13 March 2025).
- Kim, H.; Hwang, Y.H. Factors Contributing to Clinical Nurse Compliance with Infection Prevention and Control Practices: A Cross-Sectional Study. Nurs. Health Sci. 2020, 22, 126–133. [Google Scholar] [CrossRef] [PubMed]
- McCauley, L.; Kirwan, M.; Matthews, A. The Factors Contributing to Missed Care and Non-Compliance in Infection Prevention and Control Practices of Nurses: A Scoping Review. Int. J. Nurs. Stud. Adv. 2021, 3, 100039. [Google Scholar] [CrossRef] [PubMed]
- Zakeri, H.; Ahmadi, F.; Rafeemanesh, E.; Saleh, L.A. The Knowledge of Hand Hygiene among the Healthcare Workers of Two Teaching Hospitals in Mashhad. Electron. Physician 2017, 9, 5159–5165. [Google Scholar] [CrossRef]
- Alshagrawi, S.; Alhodaithy, N. Determinants of Hand Hygiene Compliance among Healthcare Workers in Intensive Care Units: A Qualitative Study. BMC Public Health 2024, 24, 2333. [Google Scholar] [CrossRef]
- Seyed Nematian, S.S.; Palenik, C.J.; Mirmasoudi, S.K.; Hatam, N.; Askarian, M. Comparing Knowledge and Self-Reported Hand Hygiene Practices with Direct Observation among Iranian Hospital Nurses. Am. J. Infect. Control 2017, 45, e65–e67. [Google Scholar] [CrossRef]
- Barroso, V.; Caceres, W.; Loftus, P.; Evans, K.H.; Shieh, L. Hand Hygiene of Medical Students and Resident Physicians: Predictors of Attitudes and Behaviour. Postgrad. Med. J. 2016, 92, 497–500. [Google Scholar] [CrossRef]
- Pfoh, E.; Dy, S.; Engineer, C. Interventions To Improve Hand Hygiene Compliance: Brief Update Review. In Making Health Care Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2013. [Google Scholar]
- Salamati, P.; Poursharifi, H.; Rahbarimanesh, A.A.; Koochak, H.E.; Najafi, Z. Effectiveness of Motivational Interviewing in Promoting Hand Hygiene of Nursing Personnel. Int. J. Prev. Med. 2013, 4, 441–447. [Google Scholar] [PubMed]
- Glowicz, J.B.; Landon, E.; Sickbert-Bennett, E.E.; Aiello, A.E.; deKay, K.; Hoffmann, K.K.; Maragakis, L.; Olmsted, R.N.; Polgreen, P.M.; Trexler, P.A.; et al. SHEA/IDSA/APIC Practice Recommendation: Strategies to Prevent Healthcare-Associated Infections through Hand Hygiene: 2022 Update. Infect. Control Hosp. Epidemiol. 2023, 44, 355–376. [Google Scholar] [CrossRef]
- Kirk, J.; Kendall, A.; Marx, J.F.; Pincock, T.; Young, E.; Hughes, J.M.; Landers, T. Point of Care Hand Hygiene-Where’s the Rub? A Survey of US and Canadian Health Care Workers’ Knowledge, Attitudes, and Practices. Am. J. Infect. Control 2016, 44, 1095–1101. [Google Scholar] [CrossRef]
- van de Mortel, T.; Bourke, R.; McLoughlin, J.; Nonu, M.; Reis, M. Gender Influences Handwashing Rates in the Critical Care Unit. Am. J. Infect. Control 2001, 29, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.L.; Warren, C.A.; Perez, E.; Louis, R.I.; Phillips, S.; Wheeler, J.; Cole, M.; Misra, R. Gender and Ethnic Differences in Hand Hygiene Practices among College Students. Am. J. Infect. Control 2008, 36, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Hong, Q.; Xu, Y. Evaluating Hand Hygiene Knowledge, Attitudes, and Practices among Healthcare Workers in Post-Pandemic H1N1 Influenza Control: A Cross-Sectional Study from China. Front. Public Health 2024, 12, 1432445. [Google Scholar] [CrossRef]
- Bounou, L.; Katelani, S.; Panagiotopoulou, K.-I.; Skouloudaki, A.-I.; Spyrou, V.; Orfanos, P.; Lagiou, P. Hand Hygiene Education of Greek Medical and Nursing Students: A Cross-Sectional Study. Nurse Educ. Pract. 2021, 54, 103130. [Google Scholar] [CrossRef]
- Cambil-Martin, J.; Fernandez-Prada, M.; Gonzalez-Cabrera, J.; Rodriguez-Lopez, C.; Almaraz-Gomez, A.; Lana-Perez, A.; Bueno-Cavanillas, A. Comparison of Knowledge, Attitudes and Hand Hygiene Behavioral Intention in Medical and Nursing Students. J. Prev. Med. Hyg. 2020, 61, E9–E14. [Google Scholar] [CrossRef]
- van de Mortel, T.F.; Apostolopoulou, E.; Petrikkos, G. A Comparison of the Hand Hygiene Knowledge, Beliefs, and Practices of Greek Nursing and Medical Students. Am. J. Infect. Control 2010, 38, 75–77. [Google Scholar] [CrossRef]
- Bredin, D.; O’Doherty, D.; Hannigan, A.; Kingston, L. Hand Hygiene Compliance by Direct Observation in Physicians and Nurses: A Systematic Review and Meta-Analysis. J. Hosp. Infect. 2022, 130, 20–33. [Google Scholar] [CrossRef]
- Erasmus, V.; Daha, T.J.; Brug, H.; Richardus, J.H.; Behrendt, M.D.; Vos, M.C.; van Beeck, E.F. Systematic Review of Studies on Compliance with Hand Hygiene Guidelines in Hospital Care. Infect. Control Hosp. Epidemiol. 2010, 31, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Sendlhofer, G.; Gombotz, V.; Pregartner, G.; Zierler, R.; Schwarz, C.; Tax, C.; Brunner, G. Hand Hygiene Compliance in Intensive Care Units: An Observational Study. Int. J. Nurs. Pract. 2020, 26, e12789. [Google Scholar] [CrossRef]
- Pittet, D.; Hugonnet, S.; Harbarth, S.; Mourouga, P.; Sauvan, V.; Touveneau, S.; Perneger, T.V. Effectiveness of a Hospital-Wide Programme to Improve Compliance with Hand Hygiene. Infection Control Programme. Lancet Lond. Engl. 2000, 356, 1307–1312. [Google Scholar] [CrossRef]
- Zeduri, M.; Sgueglia, A.; Vigezzi, G.; Ferrara, P.; Lanave, M.; Galvi, R.; Abela, S.; Novelli, V.; Muzzi, A.; Odone, A. Hospital Hand Hygiene after COVID-19: Has the Pandemic Heightened Healthcare Workers’ Awareness? Eur. J. Public Health 2022, 32, ckac129.182. [Google Scholar] [CrossRef]
- Sinopidis, X.; Tsekoura, E.; Plotas, P.; Gkentzi, D.; Roupakias, S.; Fouzas, S.; Karatza, A.; Skaperda, M.; Panagiotopoulou, O.; Spyridakis, I.; et al. Healthcare Workers’ Hand Hygiene Knowledge and Compliance Evaluation, in a Greek University Hospital. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 5667–5675. [Google Scholar] [CrossRef] [PubMed]
- Esfandiari, A.; Mahmoodi, M.; Seddigh, A.; Salari, H. Knowledge, Attitude, and Practice of Hand Hygiene among Healthcare Workers during the COVID-19 Pandemic in Referral Hospitals: A Case Study from Southern Iran. Res. Sq. 2023, Preprint. [Google Scholar] [CrossRef]
- Baloh, J.; Thom, K.A.; Perencevich, E.; Rock, C.; Robinson, G.; Ward, M.; Herwaldt, L.; Reisinger, H.S. Hand Hygiene before Donning Nonsterile Gloves: Healthcare Workers’ Beliefs and Practices. Am. J. Infect. Control 2019, 47, 492–497. [Google Scholar] [CrossRef] [PubMed]
- Boyce, J.M. Hand Hygiene Compliance Monitoring: Current Perspectives from the USA. J. Hosp. Infect. 2008, 70, 2–7. [Google Scholar] [CrossRef]
- Rahim, M.H.A.; Ibrahim, M.I.; Noor, S.S.M.; Fadzil, N.M. Predictors of Self-Reported Hand Hygiene Performance among Nurses at Tertiary Care Hospitals in East Coast Malaysia. Int. J. Environ. Res. Public. Health 2021, 18, 409. [Google Scholar] [CrossRef]
- Podvratnik, N.; Ovca, A.; Jevšnik, M. Effectiveness of Nudge Tools to Promote Hand Disinfection among Healthcare Professionals and Visitors in Health Institution: The Slovenian Pilot Study. Hygiene 2024, 4, 178–188. [Google Scholar] [CrossRef]
- Chakma, S.K.; Hossen, S.; Rakib, T.M.; Hoque, S.; Islam, R.; Biswas, T.; Islam, Z.; Islam, M.M. Effectiveness of a Hand Hygiene Training Intervention in Improving Knowledge and Compliance Rate among Healthcare Workers in a Respiratory Disease Hospital. Heliyon 2024, 10, e27286. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Tseng, C.-L. What Are Healthcare Workers’ Preferences for Hand Hygiene Interventions? A Discrete Choice Experiment. BMJ Open 2021, 11, e052195. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, S.; Bhattacharya, S. Leveraging AI-Driven Nudge Theory to Enhance Hand Hygiene Compliance: Paving the Path for Future Infection Control. Front. Public Health 2025, 12, 1522045. [Google Scholar] [CrossRef]
- Aerny-Perreten, N.; Domínguez-Berjón, M.F.; Esteban-Vasallo, M.D.; García-Riolobos, C. Participation and Factors Associated with Late or Non-Response to an Online Survey in Primary Care. J. Eval. Clin. Pract. 2015, 21, 688–693. [Google Scholar] [CrossRef]
- Cho, Y.I.; Johnson, T.P.; Vangeest, J.B. Enhancing Surveys of Health Care Professionals: A Meta-Analysis of Techniques to Improve Response. Eval. Health Prof. 2013, 36, 382–407. [Google Scholar] [CrossRef]
- Cunningham, C.T.; Quan, H.; Hemmelgarn, B.; Noseworthy, T.; Beck, C.A.; Dixon, E.; Samuel, S.; Ghali, W.A.; Sykes, L.L.; Jetté, N. Exploring Physician Specialist Response Rates to Web-Based Surveys. BMC Med. Res. Methodol. 2015, 15, 32. [Google Scholar] [CrossRef]
- Meyer, V.M.; Benjamens, S.; Moumni, M.E.; Lange, J.F.M.; Pol, R.A. Global Overview of Response Rates in Patient and Health Care Professional Surveys in Surgery. Ann. Surg. 2022, 275, e75–e81. [Google Scholar] [CrossRef]
- Baruch, Y.; Holtom, B.C. Survey Response Rate Levels and Trends in Organizational Research. Hum. Relat. 2008, 61, 1139–1160. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).