Bacterial Contamination of Antiseptics, Disinfectants, and Hand Hygiene Products Used in Healthcare Settings in Low- and Middle-Income Countries—A Systematic Review
Abstract
1. Introduction
2. Research Questions of the Review
- What is the frequency and microbiological spectrum of the bacterial contamination of AS, DI, and HH products used in human healthcare in LMICs?
- What are the risk factors for bacterial contamination?
- What are best practices to mitigate the risk of bacterial contamination?
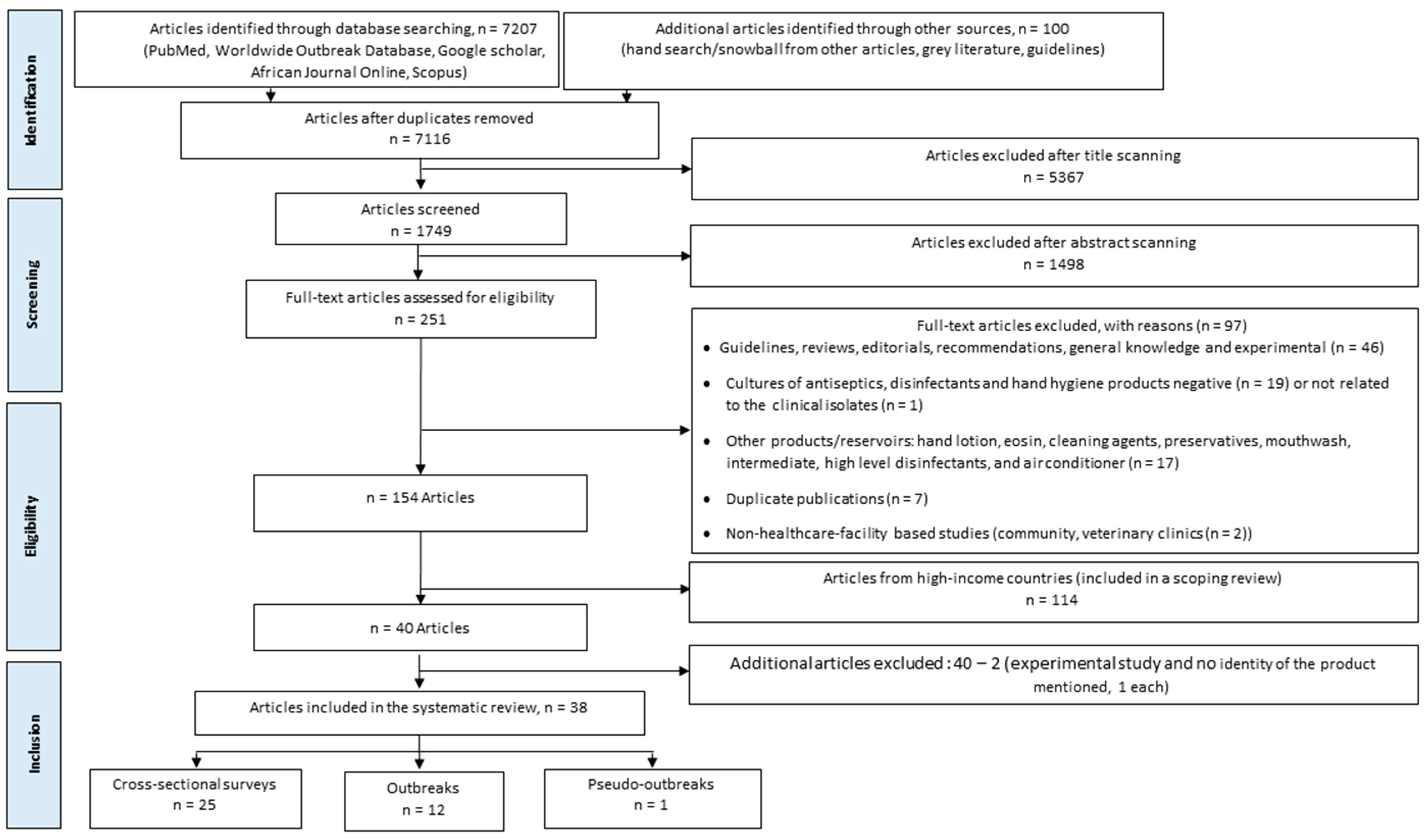
3. Materials and Methods
3.1. Review Protocol and Registration
3.2. Terms and Definitions
3.3. Search Strategy
3.4. Data Extraction
3.5. Risk of Bias Assessment and Synthesis of Results
4. Results and Discussion
4.1. (Pseudo)outbreaks and Cross-Sectional Surveys: Overview
4.2. Products Involved
4.3. Epidemic and Microbiological Methods Used

| United Nations Geoscheme/Countries | Cross-Sectional | Outbreak a | Total |
|---|---|---|---|
| Eastern Africa | 3 | - | 3 |
| Ethiopia | 2 | - | 2 |
| Kenya | 1 | - | 1 |
| Northern Africa | - | 1 | 1 |
| Tunisia | - | 1 | 1 |
| Southern Africa | - | 1 | 1 |
| South Africa | - | 1 | 1 |
| Western Africa | 6 | 2 | 8 |
| Nigeria | 6 | 1 | 7 |
| Senegal | - | 1 | 1 |
| Eastern Asia | 1 | - | 1 |
| China | 1 | - | 1 |
| Southeastern Asia | 5 | 3 | 8 |
| Malaysia | 2 | 2 | 4 |
| Thailand | 3 | 1 | 4 |
| Southern Asia | 4 | 2 | 6 |
| India | 4 | 1 | 5 |
| Nepal | - | 1 | 1 |
| Western Asia | 4 | 1 | 5 |
| Iraq | 1 | - | 1 |
| Lebanon | - | 1 | 1 |
| Palestine | 2 | - | 2 |
| Turkey | 1 | - | 1 |
| Latin America and the Caribbean | 2 | 3 | 5 |
| Argentina | - | 1 | 1 |
| Brazil | 1 | - | 1 |
| Colombia | - | 1 a | 1 |
| Mexico | - | 1 | 1 |
| Trinidad and Tobago | 1 | - | 1 |
| Total | 25 | 13 | 38 |
| Decades | Alcohol | CHG a | CHG-QUAT b | Chlorine | Liquid Soap c | Total |
|---|---|---|---|---|---|---|
| 1980s | - | 2 | - | 1 | - | 3 |
| 2000s | 1 | 1 | 2 | - | 1 | 5 |
| 2010s | - | 1 a | - | - | 2 | 3 |
| 2020s | - | 1 | - | - | 1 | 2 |
| Total | 1 | 5 | 2 | 1 | 4 | 13 |
| Decades | Alcohol | CHG a | CHG-QUAT | QUAT | Iodophor | Phenol b | Chlorine | H2O2 | Liquid Soap c | Bar Soap d | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1970s | - | - | - | - | - | 1 | - | - | - | - | 1 |
| 1990s | 2 | 1 | 2 | 1 | 1 | 5 | 3 | - | - | - | 15 |
| 2000s | 2 | 4 | 5 | 2 | - | 7 | 6 | 1 | 2 | 3 | 32 |
| 2010s | 2 | - | 2 | - | - | 2 | 3 | - | 6 | 1 | 16 |
| 2020s | 1 | - | - | - | - | - | - | - | - | - | 1 |
| Total | 7 | 5 | 9 | 3 | 1 | 15 | 12 | 1 | 8 | 4 | 65 |
4.4. Microorganisms Involved
| Contaminating Bacteria | Alcohol | CHG | CHG-QUAT | Chlorine | Liquid Soap a | Total |
|---|---|---|---|---|---|---|
| Enterobacterales | - | 1 | - | 1 | 0/2/2 | 6 |
| Enterobacter cloacae | - | - | - | 1 | 1 | 2 |
| Serratia marcescens | - | 1 | - | - | 1 | 2 |
| Citrobacter spp. | - | - | - | - | 1 e | 1 |
| Klebsiella pneumoniae | - | - | - | - | 1 e | 1 |
| Non-fermentative Gram-negative rods | 1 | 4 | 1 | - | 1/0/0 | 7 |
| Burkholderia cepacia | 1 | 1 b | 1 | - | - | 3 |
| Achromobacter spp. c | - | 1 | - | - | 1 | 2 |
| Pseudomonas aeruginosa | - | 1 | - | - | - | 1 |
| Elizabethkingia meningoseptica | - | 1 | - | - | - | 1 |
| Gram-positive cocci d | - | - | 5 | - | - | 5 d |
| Coagulase-negative staphylococci | - | - | 5 | - | - | 5 |
| Total | 1 | 5 | 6 | 1 | 1/2/2 | 18 |
4.5. Factors Associated with Contamination
| Contaminating Bacteria | Alcohol | CHG a | CHG-QUAT | QUAT | Iodophor | Phenol | Chlorine | H2O2 | Liquid Soap | Bar Soap | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Enterobacterales and non-cholerae Vibrio | 3 | 6/2 | 4 | 1 | - | 5 | 8 | 3 | 1/10/4 | 6/3 | 56 |
| Enterobacter spp. b | 1 | 4 | 1 | - | - | 1 | 3 | 2 | 3 | 2 | 17 |
| Escherichia coli | - | 1 | 1 | - | - | 3 | 1 | - | 3 | 2 | 11 |
| Klebsiella spp. c | 1 | - | - | 1 | - | 1 | 2 | - | 4 | 1 | 10 |
| Proteus spp. d | - | 1 | 2 | - | - | - | 2 | 1 | 2 | 1 | 9 |
| Hafnia alvei | 1 | 2 | - | - | - | - | - | - | - | - | 3 |
| Serratia marcescens | - | - | - | - | - | - | - | - | 1 | 1 | 2 |
| Citrobacter spp. | - | - | - | - | - | - | - | - | 1 | 1 | 2 |
| Vibrio shilonii | - | - | - | - | - | - | - | - | - | 1 | 1 |
| Coliform (not identified) | - | - | - | - | - | - | - | - | 1 | - | 1 |
| Non-fermentative Gram-negative rods | 3 | 7/5 | 7 | 4 | 1 | 9 | 8 | 1 | 1/6/2 | 6/10 | 70 |
| Pseudomonas aeruginosa | 1 | 1 | 2 | 1 | 1 | 2 | 4 | 1 | 3 | 4 | 20 |
| Pseudomonas spp. e | 1 | 3 | 1 | 1 | - | 1 | 2 | - | 5 | 2 | 16 |
| Acinetobacter spp. f | 1 | 2 | 2 | - | - | 2 | 2 | - | - | 3 | 12 |
| Moraxella spp. | - | 2 | - | 1 | - | 2 | - | - | - | - | 5 |
| Achromobacter spp. g | - | 2 | 1 | - | - | 1 | - | - | - | - | 4 |
| Flavobacterium spp. | - | 2 | - | - | - | 1 | - | - | - | - | 3 |
| Burkholderia cepacia | - | - | - | - | - | - | - | - | 1 | - | 1 |
| Chryseobacterium indologenes | - | - | - | - | - | - | - | - | - | 1 | 1 |
| Stenotrophomonas maltophilia | - | - | 1 | - | - | - | - | - | - | - | 1 |
| Other non-fermentative Gram-negative rods h | - | - | - | 1 | - | - | - | - | - | 6 | 7 |
| Other Gram-negative rods (not identified) | - | - | 1 | - | - | - | - | - | - | - | 1 |
| Gram-positive bacteria | 3 | 3/1 | 3 | 1 | - | 3 | 5 | 2 | 2/0/5 | 2/4 | 34 |
| Bacillus spp. i | 2 | 3 | 1 | - | - | 1 | 2 | 1 | 2 | 1 | 13 |
| Staphylococcus aureus | - | - | 1 | - | - | 2 | 2 | 2 | 4 | 11 | |
| Coagulase-negative staphylococci | 1 j | 1 | - | 1 | - | - | 1 | 1 | 2 | - | 7 |
| Gram-positive rods (not identified) | - | - | 1 | - | - | - | - | - | - | - | 1 |
| Corynebacterium spp. | - | - | - | - | - | - | - | - | - | 1 | 1 |
| Enterococcus spp. | - | - | -- | - | - | - | - | - | 1 | 1 | |
| Yeast | - | - | - | - | - | - | - | - | 1 | 2 | 3 |
| Total | 9 | 16/8 | 15 | 6 | 1 | 17 | 21 | 6 | 4/16/12 | 15/18 | 164 |
4.6. Attribution and Transmission
4.7. Interventions
4.8. Internal and External Validity
5. Best Practices to Mitigate the Risk of Bacterial Contamination
6. Outstanding Issues and Research Questions
7. Limitations and Strengths
8. Conclusions
| Item Scored | Thong 1981 [55] | Anyiwo 1982 [47] | Cissé 1987 [49] | Kaitwatcharachai 2000 [75] | Parasakthi 2000 [51] | Nasser 2004 [53] | Espinosa de los Monteros 2008 [54] | Ben Saida 2009 [77] | Khanna 2013 [76] | Stoesser 2015 [48] | Valderrama-Beltrán 2019 [44] | Clara 2021 [52] | Said 2022 [56] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| The healthcare setting was well-described |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Title and Abstract provided information about the “outbreak” or “cross-sectional survey” |  |  |  |  |  |  |  |  |  |  |  |  |  |
| The outbreak setting was well-described |  |  |  |  |  |  |  |  |  |  |  |  |  |
| The (pseudo)outbreak was well-described |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Outbreak index organism microbiological methods were described in sufficient detail |  |  |  |  |  |  |  |  |  |  |  |  |  |
| The outbreak investigation included a clinical epidemic investigation |  |  |  |  |  |  |  |  |  |  |  |  |  |
| The outbreak environmental investigation was oriented by the clinical epidemic investigation |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Product and active ingredients were provided |  |  |  |  |  |  |  |  |  |  |  |  |  |
| The use and application of the product(s) were well-described |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Correct terminology was used (antiseptics, disinfectants, hand hygiene products) |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Microbiological culture methods used were appropriate and well-described |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Antibiotic susceptibility testing methods were reported and appropriate |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Microbiological typing methods used were appropriate |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Reporting of results was complete and appropriate |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Risk factors were assessed |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Additional investigations for risk factors were conducted and reported (interview, questionnaire, review of procedures) |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Evidence for reservoir was assessed |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Evidence for transmission was assessed |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Evidence for root cause was assessed |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Item Scored | Khor 1977 [45] | Olayemi 1994 [78] | Danchaivijitr 1995 [82] | Kajanahareutai 1995 [79] | Keah 1995 [70] | Arjunwadkar 2001 [81] | Ogunsola 2002 [57] | Gajadhar 2003 [60] | Danchaivijitr 2005 [58] | Subbannayya 2005 [65] | Tytler 2006 [59] | Afolabi 2007 [73] | Zhang 2008 [68] | El-Mahmood 2009 [61] | Muchina 2009 [69] | Zeiny 2009 [66] | Aktas 2010 [62] | Caetano 2011 [71] | Deress 2014 [74] | Singh 2014 [80] | Akabueze 2015 [63] | Biswal 2015 [67] | Salma 2016 [84] | Altaher 2016 [72] | Firesbhat 2021 [64] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Healthcare setting was well-described |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Title and Abstract provided information about the “outbreak” or “cross-sectional survey” |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Objectives were clearly described |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Product and active ingredient were provided |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| The use and application of the product(s) were well-described |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Correct terminology was used (antiseptics, disinfectants, hand hygiene products) |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Sample selection and numbers (denominators) were provided |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Sufficiently large sample sizes were provided |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Microbiological culture methods used were appropriate |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Antibiotic susceptibility testing methods were reported as appropriate |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Additional investigations were conducted and well-reported (interview, questionnaire, review of procedures) |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Reporting of results was complete and appropriate |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
| Best Practices/Recommendations | References |
|---|---|
| General recommendations | |
| [60,117,118,119] |
| Selection, procurement, reception control, stock management, and supplier evaluation | |
| [5,60,71,102,103,109,117,120,121] |
| Container and dispenser characteristics | |
| [109,122,123] |
| Preparation process (dilution, bottling, and labeling) | |
| [5,53,60,61,70,84,103,115,124,125,126,127,128] |
| Storage and Distribution | |
| [5,70,103] |
| In-use | |
| [5,27,65,66,71,73,103,109,128,129,130,131,132,133,134] |
| Container reprocessing | |
| [5,71,101,107,108,109,128,130,132] |
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization, (WHO). Progress on WASH in Health Care Facilities 2000–2021: Special Focus on WASH and Infection Prevention and Control (IPC); World Health Organization and the United Nations Children’s Fund (UNICEF): Geneva, Switzerland, 2022. [Google Scholar]
- Chemaly, R.F.; Simmons, S.; Dale, C.; Ghantoji, S.S.; Rodriguez, M.; Gubb, J.; Stachowiak, J.; Stibich, M. The role of the healthcare environment in the spread of multidrug-resistant organisms: Update on current best practices for containment. Ther. Adv. Infect. Dis. 2014, 2, 79–90. [Google Scholar] [CrossRef]
- Boyce, J.M. Modern technologies for improving cleaning and disinfection of environmental surfaces in hospitals. Antimicrob. Resist. Infect. Control 2016, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization, (WHO). Minimum Requirements for Infection Prevention and Control Programmes. Available online: https://www.who.int/publications/i/item/9789241516945 (accessed on 1 June 2022).
- World Health Organization, (WHO). WHO Guidelines on Hand Hygiene in Health Care. Available online: https://www.who.int/publications/i/item/9789241597906 (accessed on 1 June 2022).
- Weber, D.J.; Sickbert-Bennett, E.E.; Kanamori, H.; Rutala, W.A. New and emerging infectious diseases (Ebola, Middle Eastern respiratory syndrome coronavirus, carbapenem-resistant Enterobacteriaceae, Candida auris): Focus on environmental survival and germicide susceptibility. Am. J. Infect. Control 2019, 47, A29–A38. [Google Scholar] [CrossRef] [PubMed]
- Kanamori, H.; Rutala, W.A.; Weber, D.J. The Role of Patient Care Items as a Fomite in Healthcare-Associated Outbreaks and Infection Prevention. Clin. Infect. Dis. 2017, 65, 1412–1419. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.; Hardy, L.; Semret, M.; Lunguya, O.; Phe, T.; Affolabi, D.; Yansouni, C.; Vandenberg, O. Diagnostic Bacteriology in District Hospitals in Sub-Saharan Africa: At the Forefront of the Containment of Antimicrobial Resistance. Front. Med. 2019, 6, 205. [Google Scholar] [CrossRef]
- Lompo, P.; Heroes, A.-S.; Agbobli, E.; Kühne, V.; Tinto, H.; Affolabi, D.; Jacobs, J. Bacterial Contamination of Antiseptics, Disinfectants and Products Used for Hand Hygiene in Healthcare Facilities in High-Income Countries: A Scoping Review. Hygiene 2023. accepted for publication. [Google Scholar]
- Loftus, M.J.; Guitart, C.; Tartari, E.; Stewardson, A.J.; Amer, F.; Bellissimo-Rodrigues, F.; Lee, Y.F.; Mehtar, S.; Sithole, B.L.; Pittet, D. Hand hygiene in low- and middle-income countries. Int. J. Infect. Dis. 2019, 86, 25–30. [Google Scholar] [CrossRef]
- Zingg, W.; Storr, J.; Park, B.J.; Jernigan, J.A.; Harbarth, S.; Grayson, M.L.; Tacconelli, E.; Allegranzi, B.; Cardo, D.; Pittet, D. Broadening the infection prevention and control network globally; 2017 Geneva IPC-think tank (part 3). Antimicrob. Resist. Infect. Control 2019, 8, 74. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Lompo, P.; Van den Poel, B. Bacterial Contamination of Disinfectants, Antiseptics and Products Used for Hand Hygiene in Hospitals in Low- and Middle-Income Countries: A Review of Frequency, Spectrum of Microorganisms, Risk Factors and Best Practices for Risk Mitigation. CRD42021266. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021266271 (accessed on 6 August 2021).
- World Health Organization, (WHO). World Health Organization Model List of Essential Medicine. Available online: https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2021.02 (accessed on 1 June 2022).
- Centers for Disease Control and Prevention, (CDC). Best Practices for Environmental Cleaning in Healthcare Facilities: In Resource-Limited Settings. Available online: http://www.icanetwork.co.za/icanguideline2019/ (accessed on 12 July 2022).
- Rutala, W.A.; Weber, D.J. Disinfection, sterilization, and antisepsis: Principles, practices, current issues, new research, and new technologies. Am. J. Infect. Control 2019, 47, A1–A2. [Google Scholar] [CrossRef]
- World Bank. World Bank Country Classifications by Income Level. Available online: https://databank.worldbank.org/home.aspx (accessed on 25 May 2022).
- Curran, E.T. Pseudo outbreaks and no-infection outbreaks (part 2). J. Infect. Prev. 2013, 14, 108–113. [Google Scholar] [CrossRef]
- Curran, E.T. Outbreak Column 7: Pseudo-outbreaks (part 1). J. Infect. Prev. 2013, 14, 69–74. [Google Scholar] [CrossRef]
- List of Prokaryotic names with Standing in Nomenclature, (LPSN). List of Prokaryotic Names with Standing in Nomenclature. Available online: https://lpsn.dsmz.de/text/valid-publication-of-new-names (accessed on 20 June 2022).
- European Committee on Antimicrobial Susceptibility Testing (EUCAST). Expected Resistant Phenotypes Version 1.1 March 2022. Available online: https://www.eucast.org/ (accessed on 1 May 2022).
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef]
- Institute for Hygiene and Environmental Medicine Charité—University Medicine Berlin Worldwide Database for Nosocomial Outbreaks. Available online: https://www.outbreak-database.com/Home.aspx (accessed on 31 May 2022).
- Opengrey OPENGREY.EU—Grey Literature Database. Available online: https://opengrey.eu/ (accessed on 31 May 2022).
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- World Health Organization, (WHO). Technical Brief on Water, Sanitation, Hygiene and Wastewater Management to Prevent Infections and Reduce the Spread of Antimicrobial Resistance. Available online: https://apps.who.int/iris/bitstream/handle/10665/332243/9789240006416-eng.pdf?ua=1 (accessed on 25 November 2022).
- Centers for Disease Control and Prevention, (CDC). Infection Control. Available online: https://www.cdc.gov/infectioncontrol/index.html (accessed on 22 November 2022).
- Centers for Disease Control and Prevention, (CDC). Healthcare Infection Control Practices Advisory Committee, (HICPAC). Available online: https://www.cdc.gov/hicpac/index.html (accessed on 12 July 2022).
- International Federation of Infection Control, (IFIC). The International Federation of Infection Control. Available online: https://theific.org/ (accessed on 22 November 2022).
- Médecins Sans Frontières, (MSF). Médecins Sans Frontières. Available online: https://www.msf.fr/ (accessed on 28 November 2022).
- Johns Hopkins Program for International Education in Gynecology and Obstetrics, (Jhpiego). Available online: https://www.jhpiego.org/about/history-mission/ (accessed on 12 July 2022).
- Enhancing the QUAlity and Transparency of health Research, (EQUATOR Network). Enhancing the QUAlity and Transparency of Health Research. Available online: https://www.equator-network.org/ (accessed on 22 August 2022).
- Stone, S.P.; Cooper, B.S.; Kibbler, C.C.; Cookson, B.D.; Roberts, J.A.; Medley, G.F.; Duckworth, G.; Lai, R.; Ebrahim, S.; Brown, E.M.; et al. The ORION statement: Guidelines for transparent reporting of outbreak reports and intervention studies of nosocomial infection. Lancet Infect. Dis. 2007, 7, 282–288. [Google Scholar] [CrossRef]
- Turner, P.; Fox-Lewis, A.; Shrestha, P.; Dance, D.A.B.; Wangrangsimakul, T.; Cusack, T.-P.; Ling, C.L.; Hopkins, J.; Roberts, T.; Limmathurotsakul, D.; et al. Microbiology Investigation Criteria for Reporting Objectively (MICRO): A framework for the reporting and interpretation of clinical microbiology data. BMC Med. 2019, 17, 70. [Google Scholar] [CrossRef]
- Moffa, M.; Guo, W.; Li, T.; Cronk, R.; Abebe, L.S.; Bartram, J. A systematic review of nosocomial waterborne infections in neonates and mothers. Int. J. Hyg. Environ. Health 2017, 220, 1199–1206. [Google Scholar] [CrossRef]
- Stone, S.; Cookson, B. Endorsing Reporting Guidelines: The Journal of Infection Prevention helps show the way! J. Infect. Prev. 2016, 17, 264–266. [Google Scholar] [CrossRef]
- Agarwal, P.; Singh, M.; Sharma, D. Bacteriological Evaluation of Antiseptic Solutions Used to Keep Cheattle’s Forceps. Indian J. Surg. 2015, 77, 1027–1031. [Google Scholar] [CrossRef]
- Boukadida, J.; Monastiri, K.; Snoussi, N.; Jeddi, M.; Berche, P. Nosocomial neonatal meningitis by Alcaligenes xylosoxidans transmitted by aqueous eosin. Pediatr. Infect. Dis. J. 1993, 12, 696–697. [Google Scholar] [CrossRef]
- Boukadida, J.; Monastri, K.; Snoussi, N. Acaligenes Xylosoxydans: L’origine de l’infection Est Le plus Souvent Une Solution d’antiseptique. Arch. Pédiat. 1998, 5, 1171–1172. [Google Scholar] [CrossRef] [PubMed]
- Ben Salem, N.; Monastiri, K.; Sboui, H.; Boukadida, J.; Snoussi, N.; Salem, N. Les méningites néonatales à Alcaligenes xylosoxidans par contamination de l’éosine aqueuse. Arch. Pédiatr. 1998, 6, 226–227. [Google Scholar] [CrossRef] [PubMed]
- Pegues, D.A.; Arathoon, E.G.; Samayoa, B.; Del Valle, G.T.; Anderson, R.L.; Riddle, C.F.; O’Hara, C.M.; Miller, J.; Hill, B.C.; Highsmith, A.K.; et al. Epidemic gram-negative bacteremia in a neonatal intensive care unit in Guatemala. Am. J. Infect. Control 1994, 22, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Pinna, A.; Usai, D.; Sechi, L.A.; Zanetti, S.; Jesudasan, N.C.; Thomas, P.A.; Kaliamurthy, J. An Outbreak of Post-Cataract Surgery Endophthalmitis Caused by Pseudomonas aeruginosa. Ophthalmology 2009, 116, 2321–2326. [Google Scholar] [CrossRef] [PubMed]
- Ngwa, C.; Ogri-Okwaji, M.; Odugbemi, T. The role of medical personnel and the environment in the transmission of healthcare-associated infections in the paediatric unit of a University Teaching Hospital. Int. J. Biol. Chem. Sci. 2010, 4, 1529–1542. [Google Scholar] [CrossRef]
- Valderrama-Beltrán, S.L.; Gualtero-Trujillo, S.M.; Rodríguez-Peña, J.; Linares-Miranda, C.J.; Gonzalez-Rubio, P.; Vega-Galvis, M.C.; Riaño-Forero, I.; Cortés-Fraile, G.C.; Ariza-Ayala, B.E. Pseudobrote por Burkholderia cepacia en dos unidades de cuidados intensivos de un Hospital Universitario en Bogotá—Colombia. Infectio 2019, 23, 143–147. [Google Scholar] [CrossRef]
- Khor, S.Y.; Jegathesan, M. In-use testing of disinfectants in Malaysian government hospitals. Med. J. Malays. 1977, 32, 85–89. [Google Scholar]
- Lowbury, E.J.L. Contamination of Cetrimide and Other Fluids with Pseudomonas pyocyanea. Br. J. Ind. Med. 1951, 8, 22–25. [Google Scholar] [CrossRef]
- Anyiwo, C.; Coker, A.; Daniel, S. Pseudomonas aeruginosa in postoperative wounds from chlorhexidine solutions. J. Hosp. Infect. 1982, 3, 189–191. [Google Scholar] [CrossRef]
- Stoesser, N.; Sheppard, A.E.; Shakya, M.; Sthapit, B.; Thorson, S.; Giess, A.; Kelly, D.; Pollard, A.J.; Peto, T.E.A.; Walker, A.S.; et al. Dynamics of MDR Enterobacter cloacae outbreaks in a neonatal unit in Nepal: Insights using wider sampling frames and next-generation sequencing. J. Antimicrob. Chemother. 2015, 70, 1008–1015. [Google Scholar] [CrossRef]
- Cisse, M.F.; Samb, A.; Mboup, S.; Gaye, A.; David, M.P.; Sow, H.D.; Sanokho, A. On a Nosocomial Transmission of Enterobacter Cloacae in a Tropical Area Children Hospital. Med. Mal. Infect. 1987, 5, 260–263. [Google Scholar] [CrossRef]
- Mapping AMR and AMU Partnership (MAAP). Incomplete Antimicrobial Resistance (AMR) Data in Africa: The Crisis within the Crisis. African Society for Laboratory Medicine. 2022, pp. 1–12. Available online: https://aslm.org/wp-content/uploads/2022/09/ASLM_MAAP_Infographic_090922.pdf?x26552 (accessed on 27 November 2022).
- Parasakthi, N.; Vadivelu, J.; Ariffin, H.; Iyer, L.; Palasubramaniam, S.; Arasu, A. Epidemiology and molecular characterization of nosocomially transmitted multidrug-resistant Klebsiella pneumoniae. Int. J. Infect. Dis. 2000, 4, 123–128. [Google Scholar] [CrossRef]
- Clara, L.; Staneloni, M.I.; Salazar, E.; Greco, G.; Visus, M.; Lizzi, A.; Alexander, V.; Gutkind, G.; Radice, M.; Papalia, M. Report of two events of nosocomial outbreak and pseudo-outbreak due to contamination with Achromobacter spp. Rev. Argent. Microbiol. 2022, 54, 175–180. [Google Scholar] [CrossRef]
- Nasser, R.M.; Rahi, A.C.; Haddad, M.F.; Daoud, Z.; Irani-Hakime, N.; Almawi, W.Y. Outbreak of Burkholderia Cepacia Bacteremia Traced to Contaminated Hospital Water Used for Dilution of an Alcohol Skin Antiseptic. Infect. Control Hosp. Epidemiol. 2004, 25, 231–239. [Google Scholar] [CrossRef]
- Monteros, L.E.D.L.; Silva-Sanchez, J.; Jiménez, L.; Rojas, T.; Garza-Ramos, U.; Valverde, V. Outbreak of Infection by Extended-Spectrum β-Lactamase SHV-5-Producing Serratia marcescens in a Mexican Hospital. J. Chemother. 2008, 20, 586–592. [Google Scholar] [CrossRef]
- Thong, M.L.; Puthucheary, S.D.; Lee, E.L. Flavobacterium meningosepticum infection: An epidemiological study in a newborn nursery. J. Clin. Pathol. 1981, 34, 429–433. [Google Scholar] [CrossRef]
- Said, M.; Mitton, B.; Skosana, L.B.; Kopotsa, K.; Naidoo, R.; Amutenya, V. Outbreak and control of Achromobacter denitrificans at an academic hospital in Pretoria, South Africa. Infect. Control Hosp. Epidemiol. 2022, 44, 24–30. [Google Scholar] [CrossRef]
- Ogunsola, F.T.; Orji, B.O.; Oduyebo, O. Contamination Levels of In-Use Disinfectants in a Teaching Hospiatal in Lagos, Nigeria. Afr. J. Med. Sci. 2002, 31, 111–114. [Google Scholar]
- Danchaivijitr, S.; Dhiraputra, C.; Rongrungruang, Y.; Srihapol, N.; Pumsuwan, V. Microbial Contamination of Antiseptics and Disinfectants. J. Med. Assoc. Thai. 2005, 88 (Suppl. 10), S133–S139. [Google Scholar]
- Tytler, B.A.; Adeyemi, J.O.; Adetoran, E.O.; Biyama, H.M. Microbial contamination of disinfectant solutions in some health care institutions of three towns in Northern Nigeria. J. Pharm. Bioresour. 2006, 3, 77–82. [Google Scholar] [CrossRef]
- Gajadhar, T.; Lara, A.; Sealy, P.; Adesiyun, A.A. Microbial contamination of disinfectants and antiseptics in four major hospitals in Trinidad. Rev. Panam. Salud Publica 2003, 14, 193–199. [Google Scholar] [CrossRef] [PubMed]
- El-Mahmood, A.M.; Doughari, J.H. Bacteriological Examination of Some Diluted Disinfectants Routinely Used in the Specialist Hospital Yola, Nigeria. Afr. J. Pharm. Pharmacol. 2009, 3, 185–190. [Google Scholar]
- Aktaş, E.; Taşpınar, E.; Alay, D.; Ögedey, E.D.K.; Külah, C.; Cömert, F. Extrinsic Contamination of Liquid Soap with Various Gram-Negative Bacteria in a Hospital in Turkey. Infect. Control Hosp. Epidemiol. 2010, 31, 1199–1201. [Google Scholar] [CrossRef] [PubMed]
- Akabueze, E.C.; Obi, S.C.; Nwankwo, E.O. Evaluation Of Disinfectants By The In-Use Technique In Healthcare Facilities In Kogi State North Central Nigeria. Niger. J. Microbiol. 2015, 28, 2833–2837. [Google Scholar]
- Firesbhat, A.; Tigabu, A.; Tegene, B.; Gelaw, B. Bacterial profile of high-touch surfaces, leftover drugs and antiseptics together with their antimicrobial susceptibility patterns at University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. BMC Microbiol. 2021, 21, 309. [Google Scholar] [CrossRef]
- Subbannayya, K.; Bhat, G.; Junu, V.; Shetty, S.; Jisho, M. Can soaps act as fomites in hospitals? J. Hosp. Infect. 2006, 62, 244–245. [Google Scholar] [CrossRef]
- Zeiny, S.M. Isolation of Some Microorganisms from Bar Soaps and Liquid Soaps in Hospital Environments. Iraqi J. Pharm. Sci. 2009, 18, 28–32. [Google Scholar] [CrossRef]
- Biswal, M.; Prasad, A.; Dhaliwal, N.; Gupta, A.; Taneja, N. Increase in hospital purchase of hand hygiene products: The importance of focusing on the right product. Am. J. Infect. Control 2015, 43, 765–766. [Google Scholar] [CrossRef]
- Zhang, W.; Yuan, Y.; Bian, C.; Zhang, W.; Wang, L.; Tu, X.; Huang, H. Characterization of Bacillus amyloliquefacien contaminating 75% alcohol disinfectant. Front. Med. China 2008, 2, 113–116. [Google Scholar] [CrossRef]
- Muchina, W.P.; Muchina, E.N. Transmitting infection: Testing disinfectants used in maternity units. Afr. J. Midwifery Womens Health 2009, 3, 12–15. [Google Scholar] [CrossRef]
- Keah, K.C.; Jegathesan, M.; Tan, S.C.; Chan, S.H.; Chee, O.M.; Cheong, Y.M.; Suleiman, A.B. Bacterial contamination of hospital disinfectants. Med. J. Malays. 1995, 50, 291–297. [Google Scholar]
- Caetano, J.A.; Lima, M.A.; Miranda, M.D.C.; Serufo, J.C.; Ponte, P.R.L. Identification of Bacterial Contamination in Liquid Soap for Hospital Use. Rev. Esc. Enferm. 2011, 45, 148–155. [Google Scholar]
- Altaher, A.M.; Ghafoor, E.S.A.; Amudi, W.I.; Alderby, D.K. Comparative Identification of Bacterial Quality in Liquid Soap between Nasser and European Gaza Hospitals, Khanyounis Governorate. Asian J. Pharm. Nurs. Med. Sci. 2016, 4, 77–83. [Google Scholar]
- Afolabi, B.A.; Oduyebo, O.O.; Ogunsola, E.F. Bacterial flora of commonly used soaps in three hospitals in Nigeria. E. Afr. Med. J. 2007, 84, 489–495. [Google Scholar] [CrossRef]
- Deress, T.; Girma, M.; Birhan, W.; Biadgo, B.; Alemu, A. Isolation of Bacteria from Commonly Used Antiseptic and Disinfectant Solutions in Gondar University Hospital. North West Ethiopia. Am. J. Nurs. Res. 2014, 2, 44–49. [Google Scholar] [CrossRef]
- Kaitwatcharachai, C.; Silpapojakul, K.; Jitsurong, S.; Kalnauwakul, S. An outbreak of Burkholderia cepacia bacteremia in hemodialysis patients: An epidemiologic and molecular study. Am. J. Kidney Dis. 2000, 36, 199–204. [Google Scholar] [CrossRef]
- Khanna, A.; Khanna, M.; Aggarwal, A. Serratia Marcescens—A Rare Opportunis—Tic Nosocomial Pathogen and Measures to Limit its Spread in Hospitalized Patients. J. Clin. Diagn. Res. 2013, 7, 243–246. [Google Scholar] [CrossRef]
- Ben Saida, N.; Marzouk, M.; Ferjeni, A.; Boukadida, J. A three-year surveillance of nosocomial infections by methicillin-resistant Staphylococcus haemolyticus in newborns reveals the disinfectant as a possible reservoir. Pathol. Biol. 2009, 57, e29–e35. [Google Scholar] [CrossRef]
- Olayemi, A.B.; Obayan, Y. Contaminated Disinfectants in Health Clinics in Ilorin, Nigeria. Infect. Control Hosp. Epidemiol. 1994, 15, 581–582. [Google Scholar] [CrossRef]
- Kajanahareutai, S.; Rahule, S.; Sirikulsatien, P.; Sangkasuwan, S.; Yospol, P. Efficacy and contamination of in-use disinfectants in Rajavithi General Hospital. J. Med. Assoc. Thail. 1995, 78, S36–S39. [Google Scholar]
- Singh, S.; Jeet, K.; Bareja, R.; Grover, P.S.; Mishra, V.; Goyal, R.K.; Behara, R.N. In-use tests for detection of microbial contamination in hospital disinfectants and antiseptics. IOSR J. Dent. Med. Sci. 2014, 13, 85–89. [Google Scholar] [CrossRef]
- Arjunwadkar, V.P.; Bal, A.M.; Joshi, S.A.; Kagal, A.S.; Bharadwaj, R. Contaminated antiseptics--an unnecessary hospital hazard. Indian J. Med. Sci. 2001, 55, 396–398. [Google Scholar]
- Danchaivijtr, S.; Chokloikaew, S.; Trakoolsomboon, S.; Tangtrakool, T. Contamination of Mercurochrome and Chlorhexidine-Cetrimide in a Teachaing Hospital. J. Med. Assoc. Thai. 1995, 78, S40–S43. [Google Scholar]
- Kelsey, J.C.; Maurer, I.M. An In-Use Test for Hospital Disinfectants. Mon. Bull. Minist. Health Emerg. Public Health Lab. Serv. 1966, 25, 180–184. [Google Scholar]
- Salama, A.S.A. Microbiological Quality of Soaps and Efficacy of Antiseptics and Disinfectants Used in Hospitals in Gaza—Palestine. Master Thesis, The Islamic University–Gaza Research, Gaza, Palestine, 2016. [Google Scholar]
- United Nations, (UN). Countries or Areas /Geographical Regions. Available online: https://unstats.un.org/unsd/methodology/m49/#geo-regions (accessed on 1 June 2022).
- Jean, S.; Lee, W.; Chen, F.; Ou, T.; Hsueh, P. Elizabethkingia meningoseptica: An important emerging pathogen causing healthcare-associated infections. J. Hosp. Infect. 2014, 86, 244–249. [Google Scholar] [CrossRef]
- Curran, E.T.; Dalziel, C.E. Outbreak column 18: The undervalued work of outbreak: Prevention, preparedness, detection and management. J. Infect. Prev. 2015, 16, 266–272. [Google Scholar] [CrossRef]
- World Health Organization, (WHO). Guidelines for the Prevention and Control of Carbapenem-Resistant Enterobacteriaceae, Acinetobacter Baumannii and Pseudomonas Aeruginosa in Health Care Facilities. Available online: https://www.who.int/publications/i/item/9789241550178 (accessed on 25 November 2022).
- Anderson, K.; Keynes, R. Infected Cork Closures and Apparent Survival of Organisms in Antiseptic Solutions. Br. Med. J. 1958, 2, 274–275. [Google Scholar] [CrossRef]
- Boyce, J.M.; Sullivan, L.; Booker, A.; Baker, J. Quaternary Ammonium Disinfectant Issues Encountered in an Environmental Services Department. Infect. Control Hosp. Epidemiol. 2016, 37, 340–342. [Google Scholar] [CrossRef]
- Jagals, P.; Jagals, C.; Bokako, T.C. The effect of container-biofilm on the microbiological quality of water used from plastic household containers. J. Water Health 2003, 1, 101–108. [Google Scholar] [CrossRef]
- Günther, F.; Merle, U.; Frank, U.; Gaida, M.M.; Mutters, N.T. Pseudobacteremia outbreak of biofilm-forming Achromobacter xylosoxidans—Environmental transmission. BMC Infect. Dis. 2016, 16, 584. [Google Scholar] [CrossRef]
- Ling, M.L.; How, K.B. Pseudomonas aeruginosa outbreak linked to sink drainage design. Health Infect. 2013, 18, 143–146. [Google Scholar] [CrossRef]
- Keah, K.C.; Jegathesan, M.; Tan, S.C.; Chan, S.H.; Chee, O.M.; Cheong, Y.M.; Suleiman, A.B. Disinfection: Gaps between recommended and actual practice. Southeast Asian J. Trop. Med. Public Health 1995, 26, 795–798. [Google Scholar]
- Mustapha, M.M.; Srinivasa, V.R.; Griffith, M.P.; Cho, S.-T.; Evans, D.R.; Waggle, K.; Ezeonwuka, C.; Snyder, D.J.; Marsh, J.W.; Harrison, L.H.; et al. Genomic Diversity of Hospital-Acquired Infections Revealed through Prospective Whole-Genome Sequencing-Based Surveillance. Msystems 2022, 7, e0138421. [Google Scholar] [CrossRef]
- International Society For Infectious Diseases (ISID). A Guide to Infection Control in the Hospital, 5th ed.; PMPH-USA: Boston, MA, USA, 2014; ISBN 0974903108. [Google Scholar]
- Mapping Antimicrobial Resistance and Antimicrobial Use Partnership Measure Levels of Antimicrobial Resistance (AMR) and Antimicrobial Use (AMU). Based on Existing, Historical, Records, Assess the Relationship between the Two and Provide Policy Recommendations to Strengthen AMR and Antimicrobial Consumption (AMC) Surveillance. Available online: https://aslm.org/what-we-do/maap/ (accessed on 27 November 2022).
- United States Food and Drug Administration, (FDA). Federal Register. Available online: https://www.govinfo.gov/content/pkg/FR-2012-11-21/pdf/2012-28321.pdf (accessed on 28 August 2022).
- World Health Organization, (WHO). Global Guidelines for the Prevention of Surgical Site Infection. Available online: http://apps.who.int/bookorders.%0A (accessed on 1 June 2022).
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Kampf, G.; Degenhardt, S.; Lackner, S.; Jesse, K.; Von Baum, H.; Ostermeyer, C. Poorly processed reusable surface disinfection tissue dispensers may be a source of infection. BMC Infect. Dis. 2014, 14, 37. [Google Scholar] [CrossRef]
- Gräf, W.; Kersch, D.; Scherzer, G. Microbial Contamination of Wall-Attached, One-Way Dispensers of Fluid Soaps. Zbl. Bakt. Hyg. 1988, 186, 166–179. [Google Scholar]
- Badrikian, L.; Boïko-Alaux, V.L. ‘Antiseptoguide—Guide D’Utilisation Des Antiseptiques, 3rd ed.; CHU de Clermont Ferrand: Ferrand, France, 2006. [Google Scholar]
- Bloomfield, S.F.; Carling, P.C.; Exner, M. A unified framework for developing effective hygiene procedures for hands, environmental surfaces and laundry in healthcare, domestic, food handling and other settings. GMS Hyg. Infect. Control 2017, 12, 1–16. [Google Scholar] [CrossRef]
- Das, A.; Mandal, L.; Chatterjee, S.; Ray, P.; Marwaha, R. Is hand washing safe? J. Hosp. Infect. 2008, 69, 303–304. [Google Scholar] [CrossRef]
- Bánsághi, S.; Soule, H.; Guitart, C.; Pittet, D.; Haidegger, T. Critical Reliability Issues of Common Type Alcohol-Based Handrub Dispensers. Antimicrob. Resist. Infect. Control 2020, 9, 90. [Google Scholar] [CrossRef]
- Bauer-Savage, J.; Pittet, D.; Kim, E.; Allegranzi, B. Local Production of WHO-Recommended Alcohol-Based Handrubs: Feasibility, Advantages, Barriers and Costs. Bull. World Health Organ. 2013, 91, 963–969. [Google Scholar] [CrossRef]
- Kohan, C.; Ligi, C.; Dumigan, D.G.; Boyce, J.M. The importance of evaluating product dispensers when selecting alcohol-based handrubs. Am. J. Infect. Control 2002, 30, 373–375. [Google Scholar] [CrossRef] [PubMed]
- Assadian, O.; Kramer, A.; Christiansen, B.; Exner, M.; Martiny, H.; Sorger, A.; Suchomel, M. Recommendations and requirements for soap and hand rub dispensers in healthcare facilities. GMS Krankenhhyg. Interdiszip. 2012, 7, Doc03. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization, (WHO). WHO Recommendations on Newborn Health. Available online: https://www.who.int/westernpacific/health-topics/newborn-health (accessed on 25 November 2022).
- Farthing, K.; Wares, K.; Siani, H. When 2% chlorhexidine isn’t 2%! Implications on MRSA decolonization guidelines. J. Hosp. Infect. 2022, 127, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Tack, B.; Ravinetto, R.; Allegaert, K. Collaborative partnerships as a solution for poor access to essential antimicrobial medicines: What can we learn from the chlorhexidine gel example? BMJ Paediatr. Open 2022, 6, e001661. [Google Scholar] [CrossRef]
- Zapka, C.A.; Campbell, E.J.; Maxwell, S.L.; Gerba, C.P.; Dolan, M.J.; Arbogast, J.W.; Macinga, D.R. Bacterial Hand Contamination and Transfer after Use of Contaminated Bulk-Soap-Refillable Dispensers. Appl. Environ. Microbiol. 2011, 77, 2898–2904. [Google Scholar] [CrossRef] [PubMed]
- Blanc, D.; Magalhaes, B.G.; Abdelbary, M.; Prod’Hom, G.; Greub, G.; Wasserfallen, J.; Genoud, P.; Zanetti, G.; Senn, L. Hand soap contamination by Pseudomonas aeruginosa in a tertiary care hospital: No evidence of impact on patients. J. Hosp. Infect. 2016, 93, 63–67. [Google Scholar] [CrossRef]
- Muchina, W.P. Infection Control and Prevention Practices in Public Maternity Units in Kenya. Doctoral Dissertation, University of Nairobi, Nairobi, Kenya, 2005. [Google Scholar]
- GRADE Working Group. The Grading of Recommendations Assessment, Development and Evaluation (Short GRADE) Working Group. Available online: https://www.gradeworkinggroup.org/ (accessed on 22 November 2022).
- Garcia-San Miguel, L.; Saez-Nieto, J.A.; Medina, M.J.; Lopez Hernandez, S.; Sanchez-Romero, I.; Ganga, B.; Asensio, A. Contamination of Liquid Soap for Hospital Use with Raoultella Planticola. J. Hosp. Infect. 2014, 86, 219–220. [Google Scholar] [CrossRef]
- Lehours, P.; Rogues, A.M.; Occhialini, A.; Boulestreau, H.; Gachie, J.P.; Mégraud, F. Investigation of an Outbreak Due to Alcaligenes Xylosoxydans Subspecies Xylosoxydans by Random Amplified Polymorphic DNA Analysis. Eur. J. Clin. Microbiol. Infect. Dis. 2002, 21, 108–113. [Google Scholar] [CrossRef]
- D’Errico, M.M.; Savini, S.; Prospero, E.; Annino, I. Report on a Packaged Handwashing Antiseptic Contaminated with Pseudomonas Aeruginosa. Infect. Control Hosp. Epidemiol. 2000, 21, 302. [Google Scholar] [CrossRef]
- Ahn, Y.; Kim, J.M.; Lee, Y.J.; Lipuma, J.J.; Hussong, D.; Marasa, B.S.; Cerniglia, C.E. Effects of Extended Storage of Chlorhexidine Gluconate and Benzalkonium Chloride Solutions on the Viability of Burkholderia Cenocepacia. J. Microbiol. Biotechnol. 2017, 27, 2211–2220. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Practical Guidelines for Infection Control in Health Care Facilities; WHO: Geneva, Switzerland, 2003; ISBN 92-9022-238-7. [Google Scholar]
- Lanini, S.; D’Arezzo, S.; Puro, V.; Martini, L.; Imperi, F.; Piselli, P.; Montanaro, M.; Paoletti, S.; Visca, P.; Ippolito, G. Molecular Epidemiology of a Pseudomonas Aeruginosa Hospital Outbreak Driven by a Contaminated Disinfectant-Soap Dispenser. PLoS ONE 2011, 6, e17064. [Google Scholar] [CrossRef]
- Lorenz, L.A.; Ramsay, B.D.; Goeres, D.M.; Fields, M.W.; Zapka, C.A.; Macinga, D.R. Evaluation and Remediation of Bulk Soap Dispensers for Biofilm. Biofouling 2012, 28, 99–109. [Google Scholar] [CrossRef]
- Lee, S.; Han, S.W.; Kim, G.; Song, D.Y.; Lee, J.C.; Kwon, K.T. An Outbreak of Burkholderia Cenocepacia Associated with Contaminated Chlorhexidine Solutions Prepared in the Hospital. Am. J. Infect. Control 2013, 41, 93–96. [Google Scholar] [CrossRef]
- Médecins Sans Frontières, (MSF). Antiseptics and Disinfectants. MSF Medical Guidelines. 2019. Available online: https://medicalguidelines.msf.org/en/viewport/EssDr/english/antiseptics-and-disinfectants-16688206.html#section-target-5 (accessed on 12 November 2022).
- Weber, D.J.; Rutala, W.A.; Sickbert-Bennett, E.E. Outbreaks Associated with Contaminated Antiseptics and Disinfectants. Antimicrob. Agents Chemother. 2007, 51, 4217–4224. [Google Scholar] [CrossRef]
- Burdon, D.W.; Whitby, J.L. Contamination of Hospital Disinfectants with Pseudomonas Species. Br. Med. J. 1967, 2, 153–155. [Google Scholar] [CrossRef]
- EngenderHealth. Infection Prevention: A Reference Booklet for Health Care Providers, 2nd ed.; EngenderHealth: New York, NY, USA, 2011. [Google Scholar]
- Lee, C.S.; Lee, H.B.; Cho, Y.G.; Park, J.H.; Lee, H.S. Hospital-Acquired Burkholderia Cepacia Infection Related to Contaminated Benzalkonium Chloride. Hosp. Infect. Soc. 2008, 68, 280–282. [Google Scholar] [CrossRef]
- Momeni, S.S.; Tomlin, N.; Ruby, J.D. Isolation of Raoultella Planticola from Refillable Antimicrobial Liquid Soap Dispensers in a Dental Setting. J. Am. Dent. Assoc. 2015, 146, 241–245. [Google Scholar] [CrossRef]
- Oie, S.; Kamiya, A. Microbial Contamination of Antiseptic-Soaked Cotton Balls. Biol. Pharm. Bull. 1997, 20, 667–669. [Google Scholar] [CrossRef]
- Sartor, C.; Jacomo, V.; Duvivier, C.; Tissot-Dupont, H.; Sambuc, R.; Drancourt, M. Nosocomial Serratia Marcescens Infections Associated with Extrinsic Contamination of a Liquid Nonmedicated Soap. Infect. Control Hosp. Epidemiol. 2000, 21, 196–199. [Google Scholar] [CrossRef]
- Weinbren, M.J.; Collins, M.; Heathcote, R.; Umar, M.; Nisar, M.; Ainger, C.; Masters, P. Optimization of the Blood Culture Pathway: A Template for Improved Sepsis Management and Diagnostic Antimicrobial Stewardship. J. Hosp. Infect. 2018, 98, 232–235. [Google Scholar] [CrossRef]
- Chattman, M.; Maxwell, S.L.; Gerba, C.P. Occurrence of Heterotrophic and Coliform Bacteria in Liquid Hand Soaps from Bulk Refillable Dispensers in Public Facilities. J. Environ. Health 2011, 73, 26–29. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lompo, P.; Agbobli, E.; Heroes, A.-S.; Van den Poel, B.; Kühne, V.; Kpossou, C.M.G.; Zida, A.; Tinto, H.; Affolabi, D.; Jacobs, J. Bacterial Contamination of Antiseptics, Disinfectants, and Hand Hygiene Products Used in Healthcare Settings in Low- and Middle-Income Countries—A Systematic Review. Hygiene 2023, 3, 93-124. https://doi.org/10.3390/hygiene3020010
Lompo P, Agbobli E, Heroes A-S, Van den Poel B, Kühne V, Kpossou CMG, Zida A, Tinto H, Affolabi D, Jacobs J. Bacterial Contamination of Antiseptics, Disinfectants, and Hand Hygiene Products Used in Healthcare Settings in Low- and Middle-Income Countries—A Systematic Review. Hygiene. 2023; 3(2):93-124. https://doi.org/10.3390/hygiene3020010
Chicago/Turabian StyleLompo, Palpouguini, Esenam Agbobli, Anne-Sophie Heroes, Bea Van den Poel, Vera Kühne, Cyprien M. Gutemberg Kpossou, Adama Zida, Halidou Tinto, Dissou Affolabi, and Jan Jacobs. 2023. "Bacterial Contamination of Antiseptics, Disinfectants, and Hand Hygiene Products Used in Healthcare Settings in Low- and Middle-Income Countries—A Systematic Review" Hygiene 3, no. 2: 93-124. https://doi.org/10.3390/hygiene3020010
APA StyleLompo, P., Agbobli, E., Heroes, A.-S., Van den Poel, B., Kühne, V., Kpossou, C. M. G., Zida, A., Tinto, H., Affolabi, D., & Jacobs, J. (2023). Bacterial Contamination of Antiseptics, Disinfectants, and Hand Hygiene Products Used in Healthcare Settings in Low- and Middle-Income Countries—A Systematic Review. Hygiene, 3(2), 93-124. https://doi.org/10.3390/hygiene3020010







