Digital Planning-Based Technologies to Support Memory-Related Functioning in Older Adults with Mild Cognitive Impairment: A Systematic Scoping Study
Abstract
1. Introduction
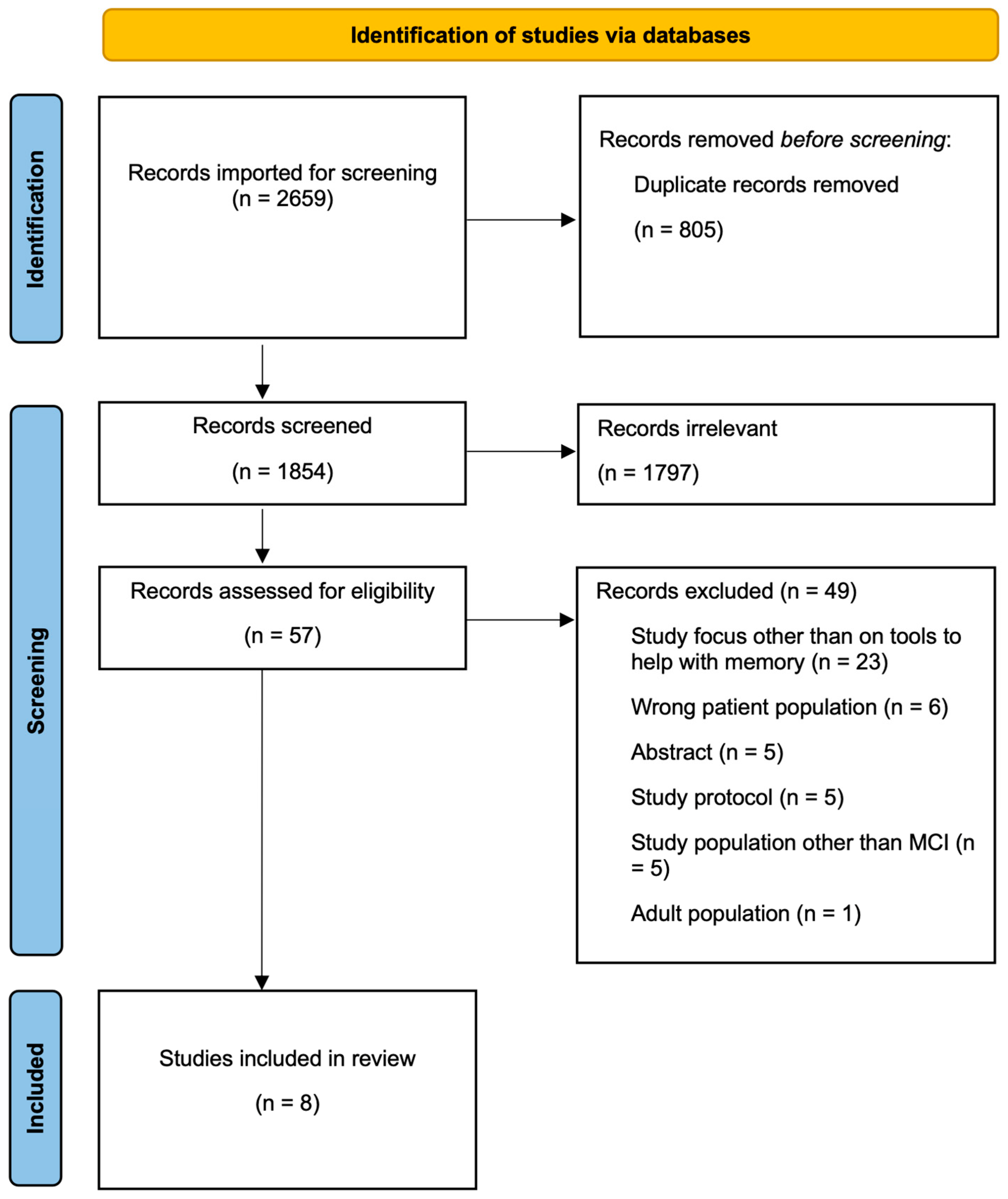
2. Materials and Methods
2.1. Study Design
2.2. Identification of the Research Question
- What does the existing literature report on digital planning-based technology to support memory-related functioning for individuals with MCI?
- What are the types and functions of digital planning-based digital compensatory aids/tools used to support memory-related functioning for individuals with MCI?
- What is the reported effectiveness of these interventions in supporting memory-related functioning for individuals with MCI?
2.3. Selection of Pertinent Studies
2.4. Selection of Relevant Articles
2.5. Data Extraction
2.6. Collation and Summarization of Results
3. Results
3.1. Characteristics of the Included Studies
- One digital memory notebook that integrates scheduling, journaling, reminders, and motivational tools to support everyday functioning [33].
- A tablet app used by caregivers to develop a visual map, which assists individuals with MCI to accomplish activities more effectively [34].
- An electronic memory and management aid application with smart-home integration that helps perform daily tasks consistently [35].
| Authors, Year, Country | Type of Study | Population | Type of Intervention | Technology Used (Device Required) | Functions of Intervention | Memory-Related Functioning Domain |
|---|---|---|---|---|---|---|
| Baric et al., 2019, Sweden [28] | Focus group interviews | 20 older adults (mean age 73: range 60–85) with access to an electronic device | Reminders and alarms | RemindMe: An interactive digital calendar with SMS-based reminders (Smartphone) | Active reminders requiring user response; logs responses and scheduled events for personalized activity history | Planning, scheduling, and task execution support |
| Boatman et al., 2019, USA [34] | Longitudinal, pre-post measure design | 7 long-term care residents with MCI or AD (mean age 81; range 68–92) | Digital visual mapping | Tablet-based visual mapping software with ADL-specific templates (Tablet device) | Step-by-step visual prompts using images and keywords to support task sequencing and ADL completion | Support for memory recall and task planning in instrumental activities of daily living |
| Hackett et al., 2022, USA [29] | Within-participant, counter balanced cross-over design | 10 older adults (mean age 80; range 67–93) with MCI or dementia | Reminders and alarms | SmartPrompt: Reminder app informed by neuropsychological theory (Smartphone) | Auditory and visual task prompts, motivational feedback, and structured task completion logging | Prospective memory, motivation, and episodic memory support |
| Nishiura et al., 2021, Japan [31] | Cross-over randomized stratified study | 20 older adults (>65) with dementia and 7 healthy older adults | Electronic calendar | Page-a-day calendar app on Android tablets (Tablet) | Displays date/time with alarms and task prompts; up to five scheduled events with step-by-step cues after alarm dismissal | Time orientation, daily task prompting, global cognition support |
| Pang & Kim 2021, South Korea [32] | Quasi-experimental with non-equivalent control group, | 42 postmenopausal women (>50) with MCI | Electronic calendar | “One Day” calendar application (Smartphone) | Sections for scheduled tasks, to-do lists, and daily journaling to support memory and task organization | Memory contentment, attention, executive function |
| Raghunath et al., 2020, USA [33] | Iterative usability testing | 20 older adults (>50) with MCI (n = 14) or traumatic brain injury (TBI) (n = 3), and caregivers (n = 3) | Digital memory notebook application | Digital Memory Notebook (DMN) (iOS Tablet) | Centralized task management with to-do lists, calendar, notes, and reminders; includes motivational prompts and smart home integration | Prospective and retrospective memory, planning, daily task execution |
| Schmitter-Edgecombe et al., 2022, USA [35] | Longitudinal study | 32 older adults (>50) with amnestic MCI | Smart-home integrated memory aid | EMMA (Electronic Memory and Management Aid) app (Smartphone) | Task scheduling, activity logging, real-time prompts, and training reminders; integrated with smart-home for context-aware support | Supports habit formation, prospective memory, and daily task management |
| Scullin et al., 2022, USA [30] | Randomized controlled trial | 52 older adults with MCI or mild dementia | Reminders and alarms | Reminder app and digital voice recorder app (Smartphone) | Prospective memory support, reminder notifications for scheduled tasks (calls and photos) | Prospective memory, IADLs |
3.2. Types of Technologies Identified and Categorized
3.3. Reminders and Alarms
3.4. Electronic Calendar
3.5. Comprehensive Digital Memory Notebook
3.6. Digital Visual Mapping
3.7. Smart-Home Integration
3.8. Effectiveness of the Interventions
4. Discussion
4.1. Implications for Clinical Practice
4.2. Implications for Policy
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| EMA | External Memory Aid |
| EMMA | Electronic Memory and Management Aid |
| ET | Everyday technology |
| DMN | Digital Memory Notebook |
| IADL | Instrumental activities of daily living |
| LTC | Long-term care |
| MCI | Mild cognitive impairment |
| MMSE | Mini-Mental State Examination |
| PRESS | Peer Review of Electronic Search Strategies |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PRISMA-ScR | PRISMA Extension for Scoping Reviews |
| TAM | Technology Assessment Model |
| TBI | Traumatic brain injury |
Appendix A. Search Strategy
Appendix A.1. Medline
- exp Cognitive Dysfunction/or Cognition Disorders/
- ((cognit* or mental) adj3 (defect* or decline or declines or disorder or disorders or dysfunction or dysfunctions or impairment or impairments or disability or disabilities)).ti,ab,kw.
- or/1–2
- computers, handheld/or smartphone/or cell phone/
- mobile applications/or user-computer interface/
- self-help devices/or communication aids for disabled/
- calendar-based technolog*.ti,ab,kw.
- digital memory notebook*.ti,ab,kw.
- compensatory aid*.ti,ab,kw.
- (smartphone* or smart-phone* or tablet or tablets or (digital adj tool*) or (mobile adj application*)).ti,ab,kw.
- palm computer*.ti,ab,kw.
- palm pilot.ti,ab,kw.
- pocket PC.ti,ab,kw.
- ((mobile or cell) adj3 (phone* or device*)).ti,ab,kw.
- ((handheld or hand held) adj (device* or computer*)).ti,ab,kw.
- self-help device*.ti,ab,kw.
- personal digital assistant.ti,ab,kw.
- ambient assisted living.ti,ab,kw.
- or/4–18
- 3 and 19
- (aged or aging or ageing or elder* or ((old or retired) adj2 (people* or patient* or inpatient* or in-patient* or outpatient* or out-patient* or client* or person* or individual* or wom#n or man or men or age)) or older* or geriatr* or gerontolog* or senior* or senescen* or retiree* or sexagenarian* or septuagenarian* or octagenarian* or nonagenarian* or centenarian* or supercentenarian* or veteran*).ti,ab. or elderly/or elderly patients/or retired people/or old age/or aging/or geriatrics/
- 20 and 21
Appendix A.2. Embase
- cognitive defect/or experimental cognitive defect/or mild cognitive impairment/or postoperative cognitive dysfunction/
- ((cognit* or mental) adj2 (defect* or decline or declines or disorder or disorders or dysfunction or dysfunctions or impairment or impairments or disability or disabilities)).ti,ab,kw.
- or/1–2
- personal digital assistant/
- smartphone/or mobile phone/or smart device/
- self help device/
- exp communication aid/
- exp mobile application/
- human machine interface/
- calendar-based technolog*.ti,ab,kw.
- digital memory notebook*.ti,ab,kw.
- compensatory aid*.ti,ab,kw.
- (smartphone* or smart-phone* or tablet or tablets or (digital adj tool*) or (mobile adj application*)).ti,ab,kw.
- palm computer*.ti,ab,kw.
- palm pilot.ti,ab,kw.
- pocket PC.ti,ab,kw.
- ((cell or mobile) adj2 (phone* or device*)).ti,ab,kw.
- ((handheld or hand held) adj (device* or computer*)).ti,ab,kw.
- self-help device*.ti,ab,kw.
- personal digital assistant.ti,ab,kw.
- or/4–20
- (aged or aging or ageing or elder* or ((old or retired) adj2 (people* or patient* or inpatient* or in-patient* or outpatient* or out-patient* or client* or person* or individual* or wom#n or man or men or age)) or older* or geriatr* or gerontolog* or senior* or senescen* or retiree* or sexagenarian* or septuagenarian* or octagenarian* or nonagenarian* or centenarian* or supercentenarian* or veteran*).ti,ab.
- exp aged/
- retirement/
- geriatrics/
- exp aging/
- or/22–26
- 3 and 21 and 27
Appendix A.3. APA PsycINFO
- cognitive impairment/or mild cognitive impairment/
- ((cognit* or mental) adj2 (defect* or decline or declines or disorder or disorders or dysfunction or dysfunctions or impairment or impairments or disability or disabilities)).ti,ab.
- or/1–2
- computer applications/or computer assisted instruction/or mobile applications/
- exp mobile devices/
- calendar-based technolog*.ti,ab.
- digital memory notebook*.ti,ab.
- compensatory aid*.ti,ab.
- (smartphone* or smart-phone* or tablet or tablets or (digital adj tool*) or (mobile adj application*)).ti,ab.
- palm computer*.ti,ab.
- palm pilot.ti,ab.
- pocket PC.ti,ab.
- ((mobile or cell) adj3 (phone* or device*)).ti,ab.
- ((handheld or hand held) adj (device* or computer*)).ti,ab.
- self-help device*.ti,ab.
- personal digital assistant.ti,ab.
- ambient assisted living.ti,ab.
- or/4–17
- (aged or aging or ageing or elder* or ((old or retired) adj2 (people* or patient* or inpatient* or in-patient* or outpatient* or out-patient* or client* or person* or individual* or wom#n or man or men or age)) or older* or geriatr* or gerontolog* or senior* or senescen* or retiree* or sexagenarian* or septuagenarian* or octagenarian* or nonagenarian* or centenarian* or supercentenarian* or veteran*).ti,ab.
- exp aging/
- older adulthood/
- retirement/
- geriatrics/
- or/19–23
- 3 and 18 and 24
Appendix A.4. CINAHL
| # | Query |
|---|---|
| S22 | S2 AND S17 AND S21 |
| S21 | S18 OR S19 OR S20 |
| S20 | (MH “Geriatrics+”) |
| S19 | (MH “Aged+”) |
| S18 | TI ((aged or aging or ageing or elder* or ((old or retired) N2 (people* or patient* or inpatient* or in-patient* or outpatient* or out-patient* or client* or person* or individual* or wom#n or man or men or age)) or older* or geriatr* or gerontolog* or senior* or senescen* or retiree* or sexagenarian* or septuagenarian* or octagenarian* or nonagenarian* or centenarian* or supercentenarian* or veteran*)) OR AB ((aged or aging or ageing or elder* or ((old or retired) N2 (people* or patient* or inpatient* or in-patient* or outpatient* or out-patient* or client* or person* or individual* or wom#n or man or men or age)) or older* or geriatr* or gerontolog* or senior* or senescen* or retiree* or sexagenarian* or septuagenarian* or octagenarian* or nonagenarian* or centenarian* or supercentenarian* or veteran*)) |
| S17 | S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 |
| S16 | TI personal digital assistant OR AB personal digital assistant |
| S15 | TI self-help device* OR AB self-help device* |
| S14 | TI (((handheld or hand held) N1 (device* or computer*))) OR AB ( ((handheld or hand held) N1 (device* or computer*))) |
| S13 | TI (((cell or mobile) N2 (phone* or device*))) OR AB (((cell or mobile) N2 (phone* or device*))) |
| S12 | TI pocket PC OR AB pocket PC |
| S11 | TI palm pilot OR AB palm pilot |
| S10 | TI palm computer* OR AB palm computer* |
| S9 | TI ((smartphone* or smart-phone* or tablet or tablets or (digital N1 tool*) or (mobile N1 application*))) OR AB ((smartphone* or smart-phone* or tablet or tablets or (digital N1 tool*) or (mobile N1 application*))) |
| S8 | TI compensatory aid* OR AB compensatory aid* |
| S7 | TI digital memory notebook* OR AB digital memory notebook* |
| S6 | TI calendar-based technolog* OR AB calendar-based technolog* |
| S5 | (MH “Mobile Applications”) |
| S4 | (MH “Computers, Hand-Held+”) OR (MH “Cellular Phone”) |
| S3 | S1 OR S2 |
| S2 | TI (((cognit* or mental) N2 (defect* or decline or declines or disorder or disorders or dysfunction or dysfunctions or impairment or impairments or disability or disabilities))) OR AB (((cognit* or mental) N2 (defect* or decline or declines or disorder or disorders or dysfunction or dysfunctions or impairment or impairments or disability or disabilities))) |
| S1 | (MH “Mild Cognitive Impairment”) |
References
- Petersen, R.C. Normal Aging, Mild Cognitive Impairment and Alzheimer’s Disease. Neurologist 1995, 4, 326–344. [Google Scholar]
- Bai, W.; Chen, P.; Cai, H.; Zhang, Q.; Su, Z.; Cheung, T.; Jackson, T.; Sha, S.; Xiang, Y.-T. Worldwide Prevalence of Mild Cognitive Impairment among Community Dwellers Aged 50 Years and Older: A Meta-Analysis and Systematic Review of Epidemiology Studies. Age Ageing 2022, 51, afac173. [Google Scholar] [CrossRef]
- Rajan, K.B.; Weuve, J.; Barnes, L.L.; McAninch, E.A.; Wilson, R.S.; Evans, D.A. Population Estimate of People with Clinical AD and Mild Cognitive Impairment in the United States (2020–2060). Alzheimer’s Dement. 2021, 17, 1966–1975. [Google Scholar] [CrossRef]
- Watt, J.A.; Isaranuwatchai, W.; Grossman, L.; Straus, S.E. Disease-Modifying Drugs for Alzheimer Disease: Implications for People in Canada. CMAJ 2023, 195, E1446–E1448. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick-Lewis, D.; Warren, R.; Ali, M.U.; Sherifali, D.; Raina, P. Treatment for Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Can. Med. Assoc. Open Access J. 2015, 3, E419–E427. [Google Scholar] [CrossRef] [PubMed]
- Busse, A.; Angermeyer, M.C.; Riedel-Heller, S.G. Progression of Mild Cognitive Impairment to Dementia: A Challenge to Current Thinking. Br. J. Psychiatry 2006, 189, 399–404. [Google Scholar] [CrossRef]
- Jack, C.R.; Knopman, D.S.; Jagust, W.J.; Shaw, L.M.; Aisen, P.S.; Weiner, M.W.; Petersen, R.C.; Trojanowski, J.Q. Hypothetical Model of Dynamic Biomarkers of the Alzheimer’s Pathological Cascade. Lancet Neurol. 2010, 9, 119–128. [Google Scholar] [CrossRef]
- Chandler, J.M.; Rentz, D.M.; Zagar, A.; Kim, Y.; Schwartz, R.L.; Fillit, H. Disease Progression and Costs at the 3-Year Follow-up of the GERAS-US Study. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2023, 15, e12430. [Google Scholar] [CrossRef]
- Robinson, R.L.; Rentz, D.M.; Andrews, J.S.; Zagar, A.; Kim, Y.; Bruemmer, V.; Schwartz, R.L.; Ye, W.; Fillit, H.M. Costs of Early Stage Alzheimer’s Disease in the United States: Cross-Sectional Analysis of a Prospective Cohort Study (GERAS-US)1. J Alzheimer’s Dis. 2020, 75, 437–450. [Google Scholar] [CrossRef]
- Alzheimer Society of Canada Report Summarys: Prevalence and Monetary Costs of Dementia in Canada (2016): A Report by the Alzheimer Society of Canada Alzheimer Society of Canada. Health Promot. Chronic Dis. Prev. Canada Res. Policy Pract. 2016, 36, 231.
- Lin, P.-J.; Neumann, P.J. The Economics of Mild Cognitive Impairment. Alzheimer’s Dement. 2013, 9, 58–62. [Google Scholar] [CrossRef]
- Winblad, B.; Palmer, K.; Kivipelto, M.; Jelic, V.; Fratiglioni, L.; Wahlund, L.-O.; Nordberg, A.; Bäckman, L.; Albert, M.; Almkvist, O.; et al. Mild Cognitive Impairment—Beyond Controversies, towards a Consensus: Report of the International Working Group on Mild Cognitive Impairment. J. Intern. Med. 2004, 256, 240–246. [Google Scholar] [CrossRef]
- Petersen, R.C.; Caracciolo, B.; Brayne, C.; Gauthier, S.; Jelic, V.; Fratiglioni, L. Mild Cognitive Impairment: A Concept in Evolution. J. Intern. Med. 2014, 275, 214–228. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.P.Y.; Chan, C.C.H.; Chu, M.M.L.; Ng, T.Y.L.; Chu, L.W.; Hui, F.S.L.; Yuen, H.K.; Fisher, A.G. Activities of Daily Living Performance in Dementia. Acta Neurol. Scand. 2007, 116, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Rogers, W.A.; Fisk, A.D. Toward a Psychological Science of Advanced Technology Design for Older Adults. J. Gerontol. Ser. B 2010, 65B, 645–653. [Google Scholar] [CrossRef]
- Dieciuc, M.; Zhang, S.; Gray, N.; Lustria, M.L.A.; Carr, D.C.; Charness, N.; Boot, W.R. Terms of Engagement: Understanding the Motivations, Preferences, and Attitudes of Older Adults Toward Mobile Cognitive Assessment and Training. Gerontol. 2024, 64, gnad048. [Google Scholar] [CrossRef]
- Gaber, S.N.; Nygård, L.; Brorsson, A.; Kottorp, A.; Malinowsky, C. Everyday Technologies and Public Space Participation among People with and without Dementia. Can. J. Occup. Ther. 2019, 86, 400–411. [Google Scholar] [CrossRef] [PubMed]
- Vega, J.N.; Newhouse, P.A. Mild Cognitive Impairment: Diagnosis, Longitudinal Course, and Emerging Treatments. Curr. Psychiatry Rep. 2014, 16, 490. [Google Scholar] [CrossRef]
- Benge, J.F.; Kiselica, A.M.; Aguirre, A.; Hilsabeck, R.C.; Douglas, M.; Paydarfar, D.; Scullin, M.K. Technology Use and Subjective Cognitive Concerns in Older Adults. Arch. Gerontol. Geriatr. 2023, 106, 104877. [Google Scholar] [CrossRef]
- Guzman-Parra, J.; Barnestein-Fonseca, P.; Guerrero-Pertiñez, G.; Anderberg, P.; Jimenez-Fernandez, L.; Valero-Moreno, E.; Goodman-Casanova, J.M.; Cuesta-Vargas, A.; Garolera, M.; Quintana, M.; et al. Attitudes and Use of Information and Communication Technologies in Older Adults With Mild Cognitive Impairment or Early Stages of Dementia and Their Caregivers: Cross-Sectional Study. J. Med. Internet. Res. 2020, 22, e17253. [Google Scholar] [CrossRef]
- Andreassen, M.; Danielsson, H.; Hemmingsson, H.; Jaarsma, T. An Interactive Digital Calendar with Mobile Phone Reminders (RemindMe) for People with Cognitive Impairment: A Pilot Randomized Controlled Trial. Scand. J. Occup. Ther. 2022, 29, 270–281. [Google Scholar] [CrossRef]
- Benge, J.F.; Dinh, K.L.; Logue, E.; Phenis, R.; Dasse, M.N.; Scullin, M.K. The Smartphone in the Memory Clinic: A Study of Patient and Care Partner’s Utilisation Habits. Neuropsychol. Rehabil. 2020, 30, 101–115. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for Conducting Systematic Scoping Reviews. Int. J. Evid. Based Health 2015, 13, 141–146. [Google Scholar] [CrossRef]
- Petersen, R.C. Mild Cognitive Impairment as a Diagnostic Entity. J. Intern. Med. 2004, 256, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Baric, V.; Andreassen, M.; Öhman, A.; Hemmingsson, H. Using an Interactive Digital Calendar with Mobile Phone Reminders by Senior People—A Focus Group Study. BMC Geriatr. 2019, 19, 116. [Google Scholar] [CrossRef] [PubMed]
- Hackett, K.; Lehman, S.; Divers, R.; Ambrogi, M.; Gomes, L.; Tan, C.C.; Giovannetti, T. Remind Me to Remember: A Pilot Study of a Novel Smartphone Reminder Application for Older Adults with Dementia and Mild Cognitive Impairment. Neuropsychol. Rehabil. 2022, 32, 22–50. [Google Scholar] [CrossRef] [PubMed]
- Scullin, M.K.; Jones, W.E.; Phenis, R.; Beevers, S.; Rosen, S.; Dinh, K.; Kiselica, A.; Keefe, F.J.; Benge, J.F. Using Smartphone Technology to Improve Prospective Memory Functioning: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2022, 70, 459–469. [Google Scholar] [CrossRef]
- Nishiura, Y.; Nihei, M.; Nakamura-Thomas, H.; Inoue, T. Effectiveness of Using Assistive Technology for Time Orientation and Memory, in Older Adults with or without Dementia. Disabil. Rehabil. Assist. Technol. 2021, 16, 472–478. [Google Scholar] [CrossRef]
- Pang, Y.; Kim, O. Effects of Smartphone-Based Compensatory Cognitive Training and Physical Activity on Cognition, Depression, and Self-Esteem in Women with Subjective Cognitive Decline. Brain Sci. 2021, 11, 1029. [Google Scholar] [CrossRef]
- Raghunath, N.; Dahmen, J.; Brown, K.; Cook, D.; Schmitter-Edgecombe, M. Creating a Digital Memory Notebook Application for Individuals with Mild Cognitive Impairment to Support Everyday Functioning. Disabil. Rehabil. Assist. Technol. 2020, 15, 421–431. [Google Scholar] [CrossRef]
- Boatman, F.; Golden, M.; Jin, J.; Kim, Y.; Law, S.; Lu, A.; Merriam, N.; Zola, S. Assistive Technology: Visual Mapping Combined with Mobile Software Can Enhance Quality of Life and Ability to Carry out Activities of Daily Living in Individuals with Impaired Memory. Technol. Health Care 2020, 28, 121–128. [Google Scholar] [CrossRef]
- Schmitter-Edgecombe, M.; Brown, K.; Luna, C.; Chilton, R.; Sumida, C.A.; Holder, L.; Cook, D. Partnering a Compensatory Application with Activity-Aware Prompting to Improve Use in Individuals with Amnestic Mild Cognitive Impairment: A Randomized Controlled Pilot Clinical Trial. J. Alzheimer’s Dis. 2022, 85, 73–90. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.T.; Rogers, W.A. Developing a Healthcare Technology Acceptance Model (H-TAM) for Older Adults with Hypertension. Ageing Soc. 2023, 43, 814–834. [Google Scholar] [CrossRef]
- Shang, X.; Liu, Z.; Gong, C.; Hu, Z.; Wu, Y.; Wang, C. Knowledge Mapping and Evolution of Research on Older Adults’ Technology Acceptance: A Bibliometric Study from 2013 to 2023. Humanit. Soc. Sci. Commun. 2024, 11, 1115. [Google Scholar] [CrossRef]
- Zubatiy, T.; Vickers, K.L.; Saurman, J.L.; Goldstein, F.; Rodriguez, A.; Mathur, N.; Mynatt, E. A Distributed Cognition Approach to Understanding Compensatory Calendaring Cognitive Systems of Older Adults with Mild Cognitive Impairment and Their Care Partners. In Proceedings of the 15th International Conference on Ubiquitous Computing & Ambient Intelligence (UCAmI 2023), Riviera Maya, Mexico, 28–30 November 2023; Springer: Cham, Switherland, 2023; pp. 190–201. [Google Scholar]
- Shin, Y.; Barankevich, R.; Lee, J.; Kalantari, S. PENCODER: Design for Prospective Memory and Older Adults. In Proceedings of the Extended Abstracts of the 2021 CHI Conference on Human Factors in Computing Systems, Virtual, 8–13 May 2021; Association for Computing Machinery: New York, NY, USA, 2021; pp. 1–7. [Google Scholar]
- Luna, C.; Cook, D.J.; Schmitter-Edgecombe, M. But Will They Use It? Predictors of Adoption of an Electronic Memory Aid in Individuals with Amnestic Mild Cognitive Impairment. Neuropsychology 2023, 37, 955–965. [Google Scholar] [CrossRef] [PubMed]
- Chudoba, L.A.; Church, A.S.; Dahmen, J.B.; Brown, K.D.; Schmitter-Edgecombe, M. The Development of a Manual-Based Digital Memory Notebook Intervention with Case Study Illustrations. Neuropsychol. Rehabil. 2020, 30, 1829–1851. [Google Scholar] [CrossRef]
- Lanzi, A.; Bourgeois, M.S. Structured External Memory Aid Treatment for Mild Cognitive Impairment. Am. J. Speech Lang. Pathol. 2020, 29, 474–484. [Google Scholar] [CrossRef]
- Lanzi, A.; Wallace, S.E.; Bourgeois, M. Group External Memory Aid Treatment for Mild Cognitive Impairment. Aphasiology 2019, 33, 320–336. [Google Scholar] [CrossRef]
- Lanzi, A.M.; Saylor, A.K.; Dedrick, R.F.; Bourgeois, M.S.; Cohen, M.L. The Functional External Memory Aid Tool Version 2.0: A How-To Clinical Guide. Am. J. Speech-Lang. Pathol. 2023, 32, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Public Health Agency of Canada. A Dementia Strategy for Canada: Together We Achieve—2023 Annual Report. Available online: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/dementia-strategy-annual-report-parliament-2023.html (accessed on 28 October 2024).
- Astell, A.J.; Bouranis, N.; Hoey, J.; Lindauer, A.; Mihailidis, A.; Nugent, C.; Robillard, J.M. Technology and Dementia: The Future Is Now. Dement. Geriatr. Cogn. Disord. 2019, 47, 131. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Peer-reviewed scientific articles | Editorials, letters to editors, thesis/dissertations, and book reviews |
| Studies where participants were 50 years old or older with diagnosed mild cognitive impairment | Studies in which participants exclusively had cognitive impairment due to an acquired brain injury (e.g., stroke, traumatic brain injury, etc.) |
| Studies focusing on digital planning-based technologies to support memory-related functioning | Studies involving experimental animal models of cognitive dysfunction |
| Studies published in any language where English translation is available. | Studies not in the English language or without available translations |
| Outcome Domain | Number of Studies | Number of Studies Reporting Improvement | % of Assessed Studies | Studies Reporting Improvement |
|---|---|---|---|---|
| Task performance (e.g., task completion, IADLs) | 7 | 6 | 86% | [29,30,31,32,33,34] |
| Specific cognitive functions (e.g., memory, executive function) | 6 | 5 | 83% | [29,30,31,32,34] |
| Global cognitive function | 3 | 1 | 33% | [31] |
| Usability/acceptability | 8 | 8 | 100% | [28,29,30,31,32,33,34,35] |
| Adherence/engagement | 5 | 4 | 80% | [28,30,33,35] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sriranganathan, A.; Kathiravelu, S.; Li, T.; Sikora, L.; McClymont, S.; Locke, D.; Chandler, M.; Shandera-Ochsner, A.; Chan, A.D.C.; Rajabiyazdi, F.; et al. Digital Planning-Based Technologies to Support Memory-Related Functioning in Older Adults with Mild Cognitive Impairment: A Systematic Scoping Study. J. Ageing Longev. 2025, 5, 42. https://doi.org/10.3390/jal5040042
Sriranganathan A, Kathiravelu S, Li T, Sikora L, McClymont S, Locke D, Chandler M, Shandera-Ochsner A, Chan ADC, Rajabiyazdi F, et al. Digital Planning-Based Technologies to Support Memory-Related Functioning in Older Adults with Mild Cognitive Impairment: A Systematic Scoping Study. Journal of Ageing and Longevity. 2025; 5(4):42. https://doi.org/10.3390/jal5040042
Chicago/Turabian StyleSriranganathan, Aswen, Shaylene Kathiravelu, Tracy Li, Lindsey Sikora, Shekinah McClymont, Dona Locke, Melanie Chandler, Anne Shandera-Ochsner, Adrian D. C. Chan, Fateme Rajabiyazdi, and et al. 2025. "Digital Planning-Based Technologies to Support Memory-Related Functioning in Older Adults with Mild Cognitive Impairment: A Systematic Scoping Study" Journal of Ageing and Longevity 5, no. 4: 42. https://doi.org/10.3390/jal5040042
APA StyleSriranganathan, A., Kathiravelu, S., Li, T., Sikora, L., McClymont, S., Locke, D., Chandler, M., Shandera-Ochsner, A., Chan, A. D. C., Rajabiyazdi, F., Santos, O. A., Trudel, C., Jaiswal, A., & Thomas, N. (2025). Digital Planning-Based Technologies to Support Memory-Related Functioning in Older Adults with Mild Cognitive Impairment: A Systematic Scoping Study. Journal of Ageing and Longevity, 5(4), 42. https://doi.org/10.3390/jal5040042








