Acute Management of Paroxysmal Atrial Fibrillation with Intravenous Flecainide plus Oral Beta-Blockers
Abstract
1. Introduction
2. Methods
2.1. Patient Population
2.2. Outcomes
2.3. Flecainide Administration
2.4. Statistical Analysis
3. Results
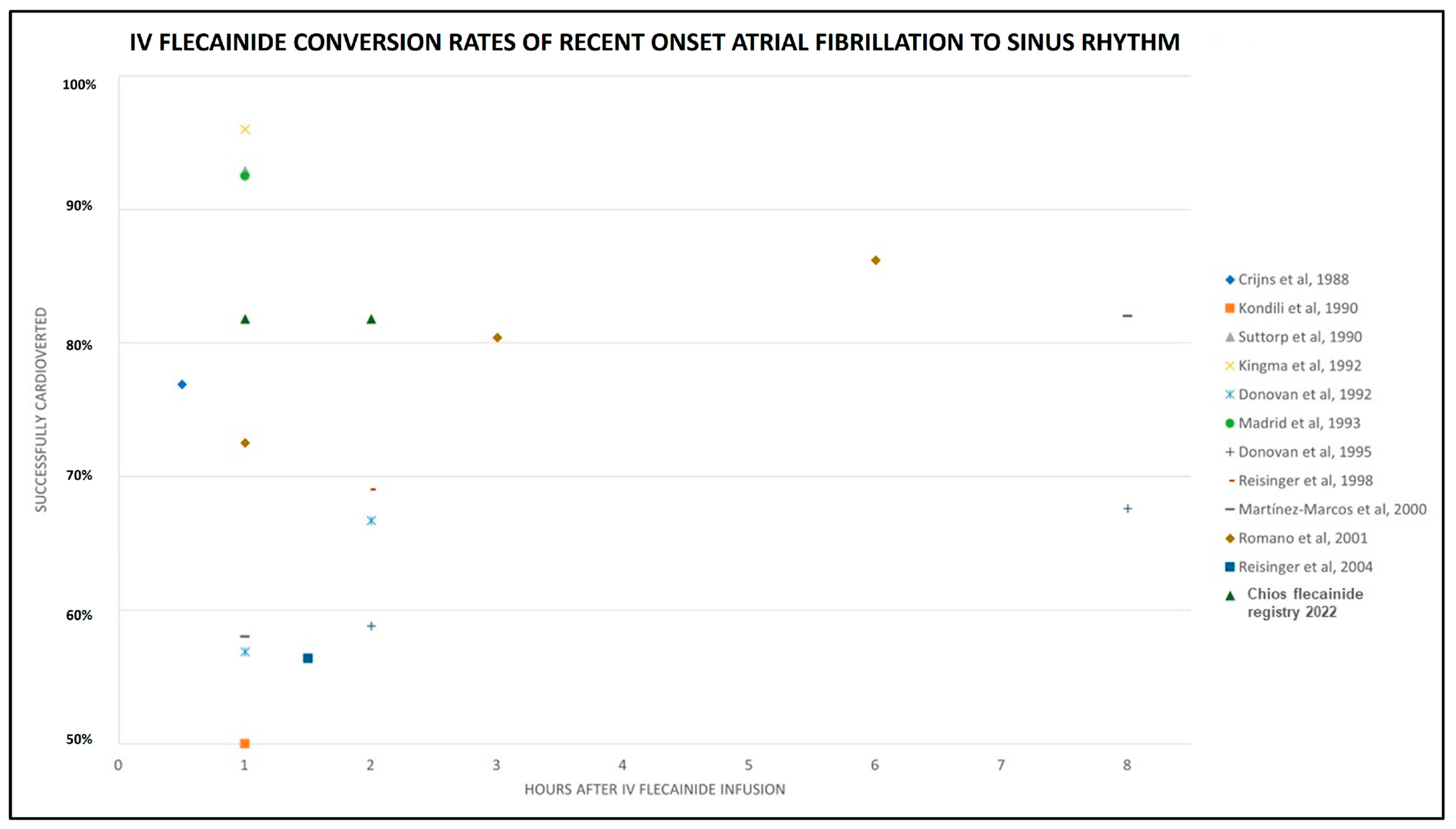
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andrikopoulos, G.K.; Pastromas, S.; Tzeis, S. Flecainide: Current status and perspectives in arrhythmia management. World J. Cardiol. 2015, 7, 76–85. [Google Scholar] [CrossRef]
- Echt, D.S.; Ruskin, J.N. Use of Flecainide for the Treatment of Atrial Fibrillation. Am. J. Cardiol. 2020, 125, 1123–1133. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021, 42, 373–498. [Google Scholar]
- Markey, G.C.; Salter, N.; Ryan, J. Intravenous Flecainide for Emergency Department Management of Acute Atrial Fibrillation. J. Emerg. Med. 2018, 54, 320–327. [Google Scholar] [CrossRef]
- Falk, R.H. Proarrhythmia in patients treated for atrial fibrillation or flutter. Ann. Intern. Med. 1992, 117, 141–150. [Google Scholar] [CrossRef]
- McNamara, R.L.; Tamariz, L.J.; Segal, J.B.; Bass, E.B. Management of atrial fibrillation: Review of the evidence for the role of pharmacologic therapy, electrical cardioversion, and echocardiography. Ann. Intern. Med. 2003, 139, 1018–1033. [Google Scholar] [CrossRef]
- Valentino, M.A.; Panakos, A.; Ragupathi, L.; Williams, J.; Pavri, B. Flecainide Toxicity: A Case Report and Systematic Review of its Electrocardiographic Patterns and Management. Cardiovasc. Toxicol. 2017, 17, 260–266. [Google Scholar] [CrossRef]
- Paolini, E.; Stronati, G.; Guerra, F.; Capucci, A. Flecainide: Electrophysiological properties, clinical indications, and practical aspects. Pharmacol. Res. 2019, 148, 104443. [Google Scholar] [CrossRef]
- Ghataoura, R.; Patil, S. Flecainide toxicity: A presentation to the emergency department with literature review. BMJ Case Rep. 2020, 13, e232691. [Google Scholar] [CrossRef]
- Newson, J.M.; Santos, C.D.; Walters, B.L.; Todd, B.R. The Case of Flecainide Toxicity: What to Look for and How to Treat. J. Emerg. Med. 2020, 59, e43–e47. [Google Scholar] [CrossRef]
- Lavalle, C.; Magnocavallo, M.; Straito, M.; Santini, L.; Forleo, B.G.; Grimaldi, M.; Badagliacca, R.; Lanata, L.; Licci, R.P. Flecainide How and When: A Practical Guide in Supraventricular Arrhythmias. J. Clin. Med. 2021, 10, 1456. [Google Scholar] [CrossRef]
- Apostolakis, S.; Oeff, M.; Tebbe, U.; Fabritz, L.; Breithardt, G.; Kirchhof, P. Flecainide acetate for the treatment of atrial and ventricular arrhythmias. Expert. Opin. Pharmacother. 2013, 14, 347–357. [Google Scholar] [CrossRef]
- Aliot, E.; Capucci, A.; Crijns, H.J.; Goette, A.; Tamargo, J. Twenty-five years in the making: Flecainide is safe and effective for the management of atrial fibrillation. Europace 2011, 13, 161–173. [Google Scholar] [CrossRef]
- Bonora, A.; Turcato, G.; Franchi, E.; Taioli, G.; Dilda, A.; Zerman, G.; Maccagnani, A.; Pistorelli, C.; Olivieri, O. Efficacy and safety in pharmacological cardioversion of recent-onset atrial fibrillation: A propensity score matching to compare amiodarone vs class IC antiarrhythmic drugs. Intern. Emerg. Med. 2017, 12, 853–859. [Google Scholar] [CrossRef]
- Fernández de Simón, A.; Coll-Vinent, B.; Martín, A. Cardioversion in recent onset atrial fibrillation. Emergencias 2019, 31, 227–233. (In English) [Google Scholar] [PubMed]
- DeSouza, I.S.; Tadrous, M.; Sexton, T.; Bennabas, R.; Carmelli, G.; Sinnert, R. Pharmacologic cardioversion of recent-onset atrial fibrillation: A systematic review and network meta-analysis. Europace 2020, 22, 854–869. [Google Scholar] [CrossRef]
- Crijns, H.J.G.M.; Van Wijk, L.M.; Van Gilst, W.H.; Kingma, J.H.; Van Gelder, I.C.; Lie, I. Acute Conversion of Atrial Fibrillation to Sinus Rhythm: Clinical Efficacy of Flecainide Acetate. Comparison of Two Regimens. Eur. Heart J. 1988, 9, 634–638. [Google Scholar] [CrossRef]
- Kondili, A.; Kastrati, A.; Popa, Y. Comparative evaluation of verapamil, flecainide and propafenone for the acute conversion of atrial fibrillation to sinus rhythm. Wien. Klin. Wochenschr. 1990, 102, 510–513. [Google Scholar]
- Suttorp, M.J.; Kingma, J.H.; Jessurun, E.R.; Lia-A-Huen, L.; Van Hemel, N.M.; Lie, K.L. The value of class IC antiarrhythmic drugs for acute conversion of paroxysmal atrial fibrillation or flutter to sinus rhythm. J. Am. Coll. Cardiol. 1990, 16, 1722–1727. [Google Scholar] [CrossRef]
- Kingma, J.H.; Suttorp, M.J. Acute pharmacologic conversion of atrial fibrillation and flutter: The role of flecainide, propafenone, and verapamil. Am. J. Cardiol. 1992, 70, 56A–60A, discussion 60A–61A. [Google Scholar] [CrossRef]
- Donovan, K.D.; Dobb, G.J.; Coombs, L.J.; Weekes, J.N.; Murdock, C.J.; Clarke, G.M. Efficacy of flecainide for the reversion of acute onset atrial fibrillation. Am. J. Cardiol. 1992, 70, 50A–54A, discussion 54A–55A. [Google Scholar] [CrossRef]
- Madrid, A.H.; Moro, C.; Marı´n-Huerta Mestre, J.L.; Noco, L.; Costa, A. Comparison of flecainide and procainamide in cardioversion of atrial fibrillation. Eur. Heart J. 1993, 14, 1127–1131. [Google Scholar] [CrossRef]
- Donovan, K.D.; Power, B.M.; Hockings, B.E.; Dobb, G.; Lee, K.-Y. Intravenous flecainide versus amiodarone for recent-onset atrial fibrillation. Am. J. Cardiol. 1995, 75, 693–697. [Google Scholar] [CrossRef]
- Reisinger, J.; Gatterer, E.; Heinze, G.; Lenz, K.; Slany, J.; Kuhn, P. Prospective comparison of flecainide versus sotalol for immediate conversion of atrial fibrillation. Am. J. Cardiol. 1998, 81, 1450–1454. [Google Scholar] [CrossRef]
- Martínez-Marcos, F.J.; García-Garmendia, J.L.; Ortega-Carpio, A.; Fernadez Gomez, J.M.; Santos, J.M.; Camacho, C. Comparison of intravenous flecainide, propafenone, and amiodarone for conversion of acute atrial fibrillation to sinus rhythm. Am. J. Cardiol. 2000, 86, 950–953. [Google Scholar] [CrossRef]
- Romano, S.; Fattore, L.; Toscano, G.; Corsini, F.; Coppo, A.; Catanzaro, M.; Romano, A.; Martone, A.; Caccavale, F.; Iodice, E.; et al. Efficacia ed effetti collaterali del trattamento con propafenone e flecainide della fibrillazione atriale di recente insorgenza. Ital. Heart J. Suppl. 2001, 2, 41–45. (In Italian) [Google Scholar] [PubMed]
- Reisinger, J.; Gatterer, E.; Lang, W.; Vanicek, T.; Eisserer, G.; Bachleitner, T.; Niemeth, C.; Aicher, F.; Grander, W.; Heinze, G.; et al. Flecainide versus ibutilide for immediate cardioversion of atrial fibrillation of recent onset. Eur. Heart J. 2004, 25, 1318–1324. [Google Scholar] [CrossRef]
- Hassan, O.F.; Al Suwaidi, J.; Salam, A.M. Anti-arrhythmic agents in the treatment of atrial fibrillation. J. Atr. Fibrillation 2013, 6, 864. [Google Scholar]
- Rattanawong, P.; Shen, W.; El Masry, H.; Sorajja, D.; Srivathsan, K.; Valverde, A.; Scott, L.R. Guidance on Short-Term Management of Atrial Fibrillation in Coronavirus Disease 2019. J. Am. Heart Assoc. 2020, 9, e017529. [Google Scholar] [CrossRef]
- Schnaubelt, S.; Domanovits, H.; Niederdoeckl, J.; Schuetz, N.; Cacioppo, F.; Oppenauer, J.; Spiel, A.O.; Laggner, A.N. The Impact of the COVID-19 Pandemic on Incidences of Atrial Fibrillation and Electrical Cardioversion at a Tertiary Care Emergency Department: An Inter- and Intra-year Analysis. Front. Med. 2020, 7, 595881. [Google Scholar] [CrossRef]
- Blomström-Lundqvist, C. Effects of COVID-19 lockdown strategies on management of atrial fibrillation. Eur. Heart J. 2020, 41, 3080–3082. [Google Scholar] [CrossRef]
- Holmes, B.; Heel, R.C. Flecainide: A preliminary review of its pharmacodynamic properties and therapeutic efficacy. Drugs. 1985, 29, 1–33. [Google Scholar] [CrossRef]
- Price, J.F.; Kertesz, N.J.; Snyder, C.S. Flecainide and sotalol: A new combination therapy for refractory supraventricular tachycardia in children <1 year of age. J. Am. Coll. Cardiol. 2002, 39, 517–520. [Google Scholar]
- Ermakov, S.; Gerstenfeld, E.P. Use of flecainide in combination antiarrhythmic therapy in patients with arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm. 2017, 14, 564–569. [Google Scholar] [CrossRef]
- Tsiachris, D.; Doundoulakis, I.; Pagkalidou, E.; Kordalis, A.; Deftereos, S.; Gatzoulis, K.A.; Tsioufis, K.; Stefanadis, C. Pharmacologic Cardioversion in Patients with Paroxysmal Atrial Fibrillation: A Network Meta-Analysis. Cardiovasc. Drugs Ther. 2021, 35, 293–308. [Google Scholar] [CrossRef]
- Tsiachris, D.; Doundoulakis, I.; Tsioufis, P.; Pagkalidou, E.; Antoniou, C.K.; Zafeiropoulos, S.M.; Gatzoulis, K.A.; Tsioufis, K.; Stefanadis, C. Reappraising the role of class Ic antiarrhythmics in atrial fibrillation. Eur. J. Clin. Pharmacol. 2022, 78, 1039–1045. [Google Scholar] [CrossRef]
- Arcari, L.; Luciani, M.; Cacciotti, L.; Musumeci, M.B.; Spuntarelli, V.; Pistella, E.; Martolini, D.; Manzo, D.; Pucci, M.; Marone, C.; et al. Incidence and determinants of high-sensitivity troponin and natriuretic peptides elevation at admission in hospitalized COVID-19 pneumonia patients. Intern. Emerg. Med. 2020, 15, 1467–1476. [Google Scholar] [CrossRef]

| All Patients (n = 121) | Successful Conversion to SR at 2 h (n = 99) | Not Successful Conversion to SR at 2 h (n = 22) | p Value (Successful vs. No Successful Conversion) | |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) * | 61.4 ± 8.2 | 61.1 ± 8.7 | 62.7 ± 9.1 | 0.439 |
| Females, n (%) | 48 (39.7) | 40 (40.4) | 8 (36.4) | 0.726 |
| Males, n (%) | 73 (60.3) | 59 (59.6) | 14 (63.6) | |
| Height (cm) | 170 ± 7.8 | 170 ± 8.1 | 172 ± 6.3 | 0.140 |
| Weight (kg) | 83 ± 10.7 | 82 ± 10.8 | 84 ± 10.3 | 0.392 |
| BMI (kg/m2) | 28.5 ± 2.6 | 28.5 ± 2.6 | 28.4 ± 3.0 | 0.824 |
| BSA (m2) | 1.97 ± 0.16 | 1.97 ± 0.16 | 2.0 ± 0.15 | 0.289 |
| History | ||||
| Arterial hypertension, n (%) | 60 (49.6) | 46 (46.5) | 14 (63.6) | 0.145 |
| Diabetes mellitus, n (%) | 36 (29.8) | 26 (26.3) | 10 (45.5) | 0.075 |
| Stroke, n (%) | 0 | 0 | 0 | n/a |
| Vascular disease, n (%) | 0 | 0 | 0 | n/a |
| Dyslipidemia, n (%) | 70 (57.9) | 56 (56.6) | 14 (63.6) | 0.544 |
| Smoking, n (%) | 56 (46.3) | 44 (44.4) | 12 (54.5) | 0.390 |
| Thyroid disease, n (%) | 44 (36.4) | 34 (34.3) | 10 (45.5) | 0.327 |
| CHA2DS2VASc | 1.6 ± 1.2 | 1.5 ± 1.2 | 1.9 ± 1.0 | 0.148 |
| HASBLED | 0.7 ± 0.8 | 0.7 ± 0.8 | 1.0 ± 0.6 | 0.052 |
| Clinical | ||||
| Time from AF onset (hours) | 12 ± 6.7 | 11.3 ± 5.9 | 15.3 ± 8.9 | 0.069 |
| Heart rate at arrival (bpm) | 139 ± 17 | 136 (75–160) | 138 (107–150) | 0.686 |
| EF, % | 59.8 ± 1.6 | 59.9 ± 1.6 | 59.6 ± 1.5 | 0.342 |
| MR (any degree), n (%) | 102 (84.3) | 82 (82.8) | 20 (90.9) | 0.641 |
| LA diameter (PLAX), mm | 39.6 ± 3.8 | 39.3 ± 3.9 | 40.7 ± 2.9 | 0.111 |
| Intervention | ||||
| IV Flecainide, n (%) | 121 (100) | 99 (100) | 22 (100) | n/a |
| b-blocker | 121 (100) | 99 (100) | 22 (100) | 0.208 |
| Sotalol, n (%) | 13 (10.7) | 13 (13.1) | 0 | |
| Bisoprolol, n (%) | 46 (38.0) | 38 (38.4) | 8 (36.4) | |
| Metoprolol, n (%) | 48 (39.7) | 36 (36.4) | 12 (54.5) | |
| Betaxolol, n (%) | 14 (11.6) | 12 (12.1) | 2 (9.1) | |
| Successful Conversion to SR at 2 h (n = 99) | No Successful Conversion to SR at 2 h (n = 22) | p Value | |
|---|---|---|---|
| Conversion time, min * | 11.7 (3–23) | n/a | n/a |
| Hospitalization duration, h * | 10.9 ± 3.0 | 30.7 ± 7.4 | <0.001 |
| Proarrhythmic events, n (%) | 0 | 0 | n/a |
| Severe hypotension, n (%) | 0 | 0 | n/a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kartalis, A.; Afendoulis, D.; Voutas, P.; Moutafi, M.; Papagiannis, N.; Garoufalis, S.; Kartalis, N.; Smyrnioudis, N.; Ziakas, A.; Didagelos, M. Acute Management of Paroxysmal Atrial Fibrillation with Intravenous Flecainide plus Oral Beta-Blockers. Int. J. Transl. Med. 2024, 4, 334-341. https://doi.org/10.3390/ijtm4020021
Kartalis A, Afendoulis D, Voutas P, Moutafi M, Papagiannis N, Garoufalis S, Kartalis N, Smyrnioudis N, Ziakas A, Didagelos M. Acute Management of Paroxysmal Atrial Fibrillation with Intravenous Flecainide plus Oral Beta-Blockers. International Journal of Translational Medicine. 2024; 4(2):334-341. https://doi.org/10.3390/ijtm4020021
Chicago/Turabian StyleKartalis, Athanasios, Dimitrios Afendoulis, Petros Voutas, Maria Moutafi, Nikolaos Papagiannis, Stefanos Garoufalis, Nikolaos Kartalis, Nikolaos Smyrnioudis, Antonios Ziakas, and Matthaios Didagelos. 2024. "Acute Management of Paroxysmal Atrial Fibrillation with Intravenous Flecainide plus Oral Beta-Blockers" International Journal of Translational Medicine 4, no. 2: 334-341. https://doi.org/10.3390/ijtm4020021
APA StyleKartalis, A., Afendoulis, D., Voutas, P., Moutafi, M., Papagiannis, N., Garoufalis, S., Kartalis, N., Smyrnioudis, N., Ziakas, A., & Didagelos, M. (2024). Acute Management of Paroxysmal Atrial Fibrillation with Intravenous Flecainide plus Oral Beta-Blockers. International Journal of Translational Medicine, 4(2), 334-341. https://doi.org/10.3390/ijtm4020021







