Community Participation Trajectories over the 5 Years after Traumatic Brain Injury in Older Veterans: A U.S. Veterans Affairs Model Systems Study
Abstract
1. Introduction
2. Method
2.1. Procedure and Participants
2.2. Measures
2.2.1. Sociodemographic Characteristics
2.2.2. Injury Characteristics
2.2.3. Participation Assessment with Recombined Tools-Objective (PART-O)
2.3. Data Analyses
3. Results
3.1. Little’s MCAR Tests
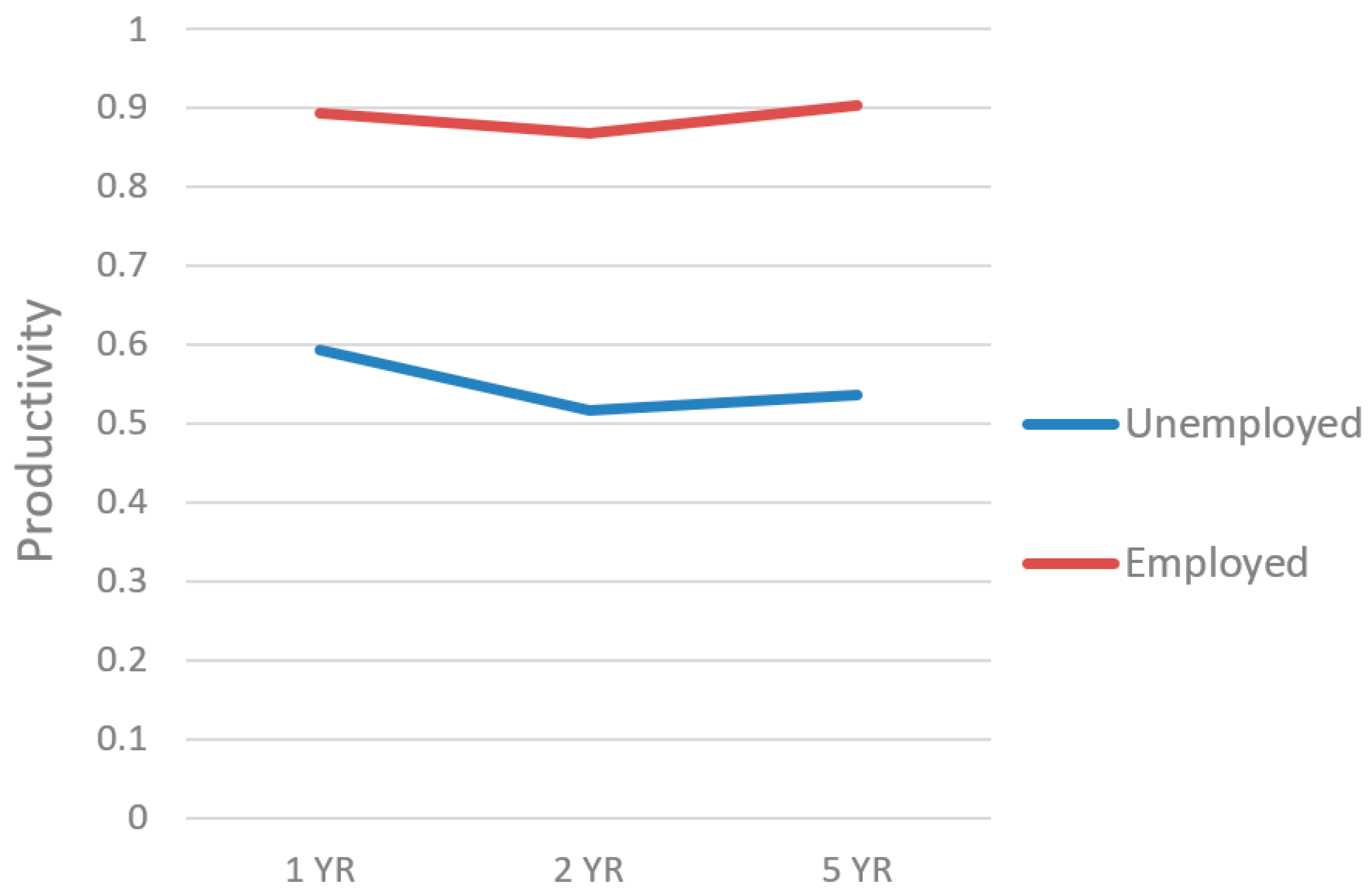
3.2. PART-O Productivity
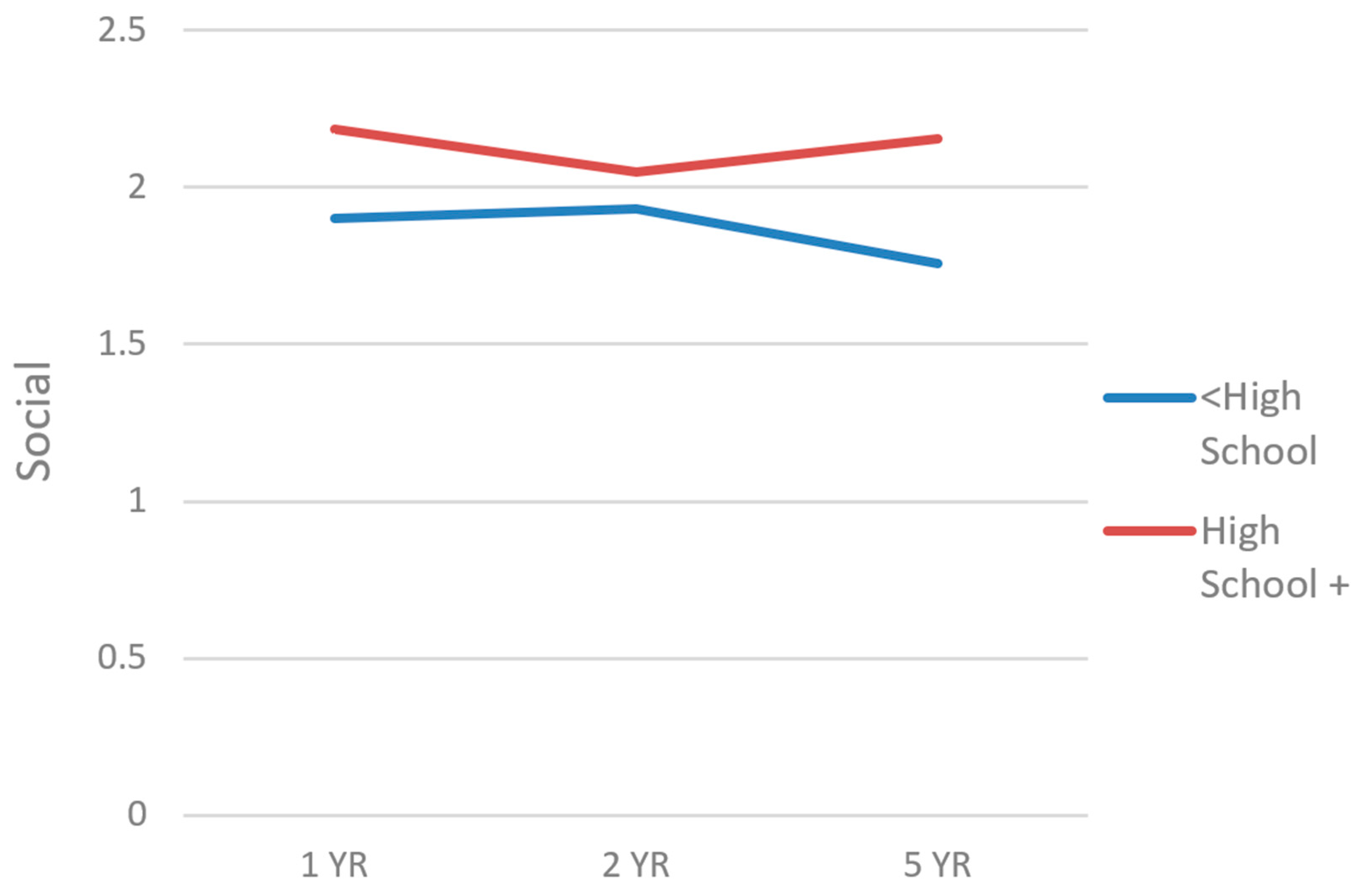
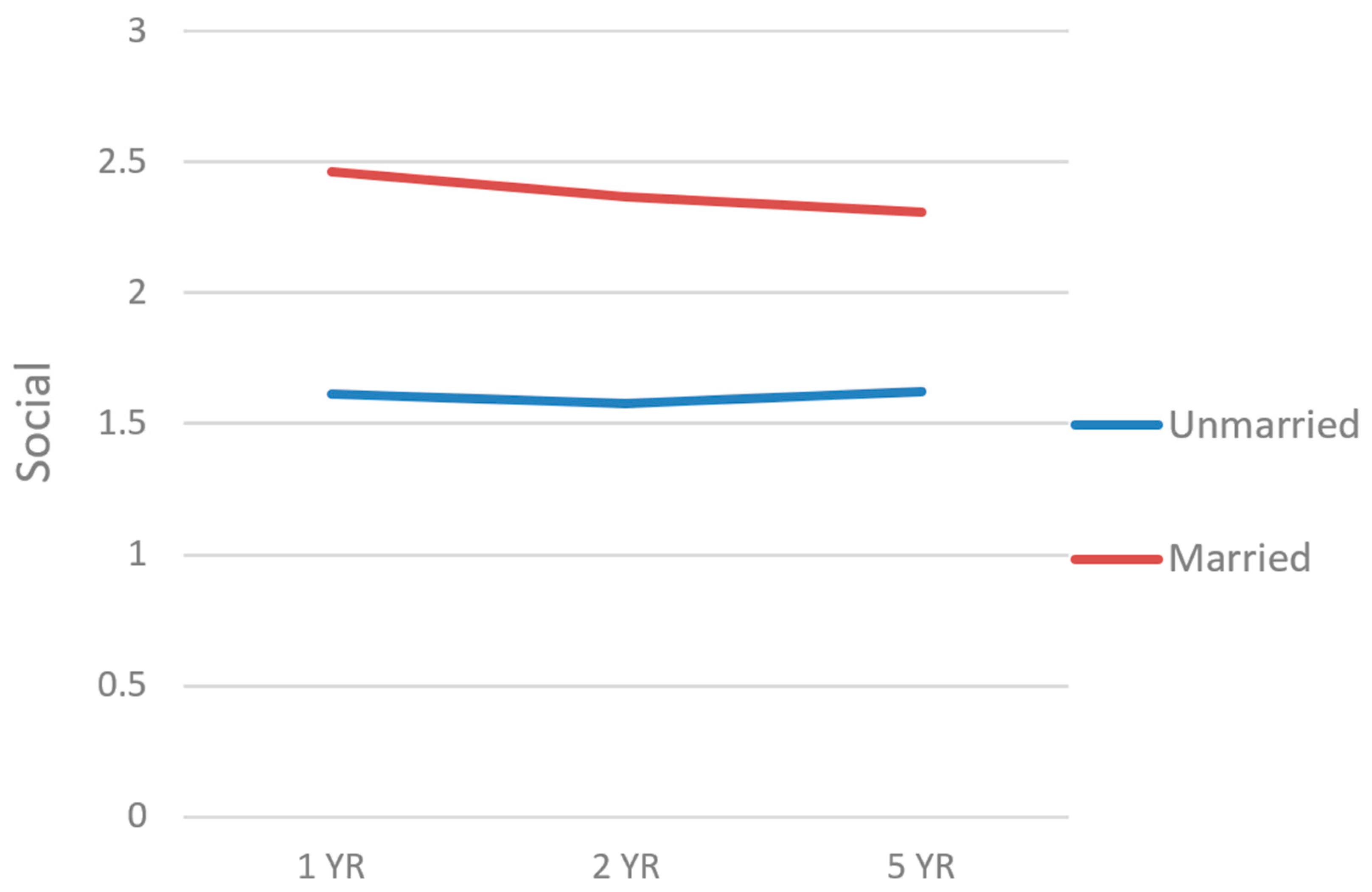
3.3. PART-O Social
3.4. PART-O Out and About
4. Discussion
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- US Census Bureau. The Older Population: 2020; 2020 Census Brief C2020BR-07; US Census Bureau: Suitland, MD, USA, 2023. Available online: https://www.census.gov/library/publications/2023/decennial/c2020br-07.html (accessed on 28 March 2024).
- US Census Bureau. Table 2: Projected Age and Sex Composition of the Population: 2017–2060. Available online: https://www.census.gov/data/tables/2017/demo/popproj/2017-summary-tables.html (accessed on 28 March 2024).
- Arias, E.; Xu, J. United States Life Tables, 2018; National Vital Statistics Reports Vol 69, No 12; Centers for Disease Control and Prevention National Center for Health Statistics: Hyattsville, MD, USA, 2020. Available online: https://blogs.cdc.gov/nchs/2020/11/20/7035/ (accessed on 28 March 2024).
- Wang, J.; Cidade, M.; Larsen, M.; Pearman, G.; Schimpf, M.; Dhanireddy, P. Main Results Report, Prepared for S. A. S. (SAS) O. of S. P. and A. (OSPA) V. H. A. 2018 Survey of Veteran Enrollees’ Health and Use of Health Care; Department of Veterans Affairs: Rockville, MD, USA, 2019.
- US Government Accountability Office. VA Health Care: Veterans’ Use of Long-Term Care Is Increasing, and VA Faces Challenges in Meeting the Demand; GAO-20-284; US Government Accountability Office: Washington, DC, USA, 2020. Available online: https://www.gao.gov/assets/gao-20-284.pdf (accessed on 12 June 2023).
- Betancourt, J.A.; Granados, P.S.; Pacheco, G.J.; Reagan, J.; Shanmugam, R.; Topinka, J.B.; Beauvais, B.M.; Ramamonjiarivelo, Z.H.; Fulton, L.V. Exploring Health Outcomes for U.S. Veterans Compared to Non-Veterans from 2003 to 2019. Healthcare 2021, 9, 604. [Google Scholar] [CrossRef]
- Vinson, L.; Goodman, D.; Hutton, D.; Kuykendall, L. Report of the Caring for Behaviorally and Medically Complex Inpatients in VHA: Assessment of Program Needs and Models of Care. VHA Complex Patient Care Implementation Task Force; Department of Veterans Affairs: Washington, DC, USA, 2017.
- O’malley, K.A.; Vinson, L.; Pless Kaiser, A.; Sager, Z.; Hinrichs, K. Mental Health and Aging Veterans: How the Veterans Health Administration Meets the Needs of Aging Veterans. Public Policy Aging Rep. 2020, 30, 19–23. [Google Scholar] [CrossRef]
- Harvey, L.A.; Close, J.C.T. Traumatic Brain Injury in Older Adults: Characteristics, Causes and Consequences. Injury 2012, 43, 1821–1826. [Google Scholar] [CrossRef]
- Mosenthal, A.C.; Lavery, R.F.; Addis, M.; Kaul, S.; Ross, S.; Marburger, R.; Deitch, E.A.; Livingston, D.H. Isolated Traumatic Brain Injury: Age Is an Independent Predictor of Mortality and Early Outcome. J. Trauma Acute Care Surg. 2002, 52, 907. [Google Scholar] [CrossRef]
- Thompson, H.J.; McCormick, W.C.; Kagan, S.H. Traumatic Brain Injury in Older Adults: Epidemiology, Outcomes, and Future Implications. J. Am. Geriatr. Soc. 2006, 54, 1590–1595. [Google Scholar] [CrossRef]
- Cusimano, M.D.; Saarela, O.; Hart, K.; Zhang, S.; McFaull, S.R. A Population-Based Study of Fall-Related Traumatic Brain Injury Identified in Older Adults in Hospital Emergency Departments. Neurosurg. Focus 2020, 49, E20. [Google Scholar] [CrossRef]
- Dams-O’Connor, K.; Cuthbert, J.P.; Whyte, J.; Corrigan, J.D.; Faul, M.; Harrison-Felix, C. Traumatic Brain Injury among Older Adults at Level I and II Trauma Centers. J. Neurotrauma 2013, 30, 2001–2013. [Google Scholar] [CrossRef]
- Peterson, A.B.; Thomas, K.E.; Zhou, H. CDC Surveillance Report of Traumatic Brain Injury-Related Deaths by Age Group, Sex, and Mechanism of Injury—United States, 2018 and 2019; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2022. Available online: https://stacks.cdc.gov/view/cdc/122988 (accessed on 12 June 2023).
- Gould, K.R.; Ponsford, J.L.; Johnston, L.; Schönberger, M. Relationship Between Psychiatric Disorders and 1-Year Psychosocial Outcome Following Traumatic Brain Injury. J. Head Trauma Rehabil. 2011, 26, 79. [Google Scholar] [CrossRef]
- Krishnamoorthy, V.; Distelhorst, J.T.; Vavilala, M.S.; Thompson, H. Traumatic Brain Injury in the Elderly: Burden, Risk Factors, and Prevention. J. Trauma Nurs.|JTN 2015, 22, 204. [Google Scholar] [CrossRef]
- Livingston, D.H.; Lavery, R.F.; Mosenthal, A.C.; Knudson, M.M.; Lee, S.; Morabito, D.; Manley, G.T.; Nathens, A.; Jurkovich, G.; Hoyt, D.B.; et al. Recovery at One Year Following Isolated Traumatic Brain Injury: A Western Trauma Association Prospective Multicenter Trial. J. Trauma Acute Care Surg. 2005, 59, 1298. [Google Scholar] [CrossRef]
- Mushkudiani, N.A.; Engel, D.C.; Steyerberg, E.W.; Butcher, I.; Lu, J.; Marmarou, A.; Slieker, F.; McHugh, G.S.; Murray, G.D.; Maas, A.I.R. Prognostic Value of Demographic Characteristics in Traumatic Brain Injury: Results from The IMPACT Study. J. Neurotrauma 2007, 24, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Rapoport, M.J.; Feinstein, A. Outcome Following Traumatic Brain Injury in the Elderly: A Critical Review. Brain Inj. 2000, 14, 749–761. [Google Scholar] [CrossRef]
- Marquez de la Plata, C.D.; Hart, T.; Hammond, F.M.; Frol, A.B.; Hudak, A.; Harper, C.R.; O’Neil-Pirozzi, T.M.; Whyte, J.; Carlile, M.; Diaz-Arrastia, R. Impact of Age on Long-Term Recovery From Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2008, 89, 896–903. [Google Scholar] [CrossRef] [PubMed]
- Rothweiler, B.; Temkin, N.R.; Dikmen, S.S. Aging Effect on Psychosocial Outcome in Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 1998, 79, 881–887. [Google Scholar] [CrossRef]
- Maiden, M.J.; Cameron, P.A.; Rosenfeld, J.V.; Cooper, D.J.; McLellan, S.; Gabbe, B.J. Long-Term Outcomes after Severe Traumatic Brain Injury in Older Adults. A Registry-Based Cohort Study. Am. J. Respir. Crit. Care Med. 2020, 201, 167–177. [Google Scholar] [CrossRef]
- Testa, J.A.; Malec, J.F.; Moessner, A.M.; Brown, A.W. Outcome After Traumatic Brain Injury: Effects of Aging on Recovery. Arch. Phys. Med. Rehabil. 2005, 86, 1815–1823. [Google Scholar] [CrossRef]
- van der Vlegel, M.; Mikolić, A.; Hee, Q.L.; Kaplan, Z.R.; Helmrich, I.R.R.; van Veen, E.; Andelic, N.; Steinbuechel, N.v.; Plass, A.M.; Zeldovich, M. Health Care Utilization and Outcomes in Older Adults after Traumatic Brain Injury: A CENTER-TBI Study. Injury 2022, 53, 2774–2782. [Google Scholar] [CrossRef] [PubMed]
- Kuhne, C.A.; Ruchholtz, S.; Kaiser, G.M.; Nast-Kolb, D. Mortality in Severely Injured Elderly Trauma Patients—When Does Age Become a Risk Factor? World J. Surg. 2005, 29, 1476–1482. [Google Scholar] [CrossRef] [PubMed]
- Kojima, T.; Akishita, M.; Nakamura, T.; Nomura, K.; Ogawa, S.; Iijima, K.; Eto, M.; Ouchi, Y. Association of Polypharmacy with Fall Risk among Geriatric Outpatients. Geriatr. Gerontol. Int. 2011, 11, 438–444. [Google Scholar] [CrossRef]
- Dams-O’Connor, K.; Gibbons, L.E.; Landau, A.; Larson, E.B.; Crane, P.K. Health Problems Precede Traumatic Brain Injury in Older Adults. J. Am. Geriatr. Soc. 2016, 64, 844–848. [Google Scholar] [CrossRef]
- Cifu, D.X.; Kreutzer, J.S.; Marwitz, J.H.; Rosenthal, M.; Englander, J.; High, W. Functional Outcomes of Older Adults with Traumatic Brain Injury: A Prospective, Multicenter Analysis. Arch. Phys. Med. Rehabil. 1996, 77, 883–888. [Google Scholar] [CrossRef] [PubMed]
- LeBlanc, J.; de Guise, E.; Gosselin, N.; Feyz, M. Comparison of Functional Outcome Following Acute Care in Young, Middle-Aged and Elderly Patients with Traumatic Brain Injury. Brain Inj. 2006, 20, 779–790. [Google Scholar] [CrossRef] [PubMed]
- Mosenthal, A.C.; Livingston, D.H.; Lavery, R.F.; Knudson, M.M.; Lee, S.; Morabito, D.; Manley, G.T.; Nathens, A.; Jurkovich, G.; Hoyt, D.B.; et al. The Effect of Age on Functional Outcome in Mild Traumatic Brain Injury: 6-Month Report of a Prospective Multicenter Trial. J. Trauma Acute Care Surg. 2004, 56, 1042. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, F.C.; Levin, H.S.; Presley, R.M.; Searcy, J.; Colohan, A.R.; Eisenberg, H.M.; Jann, B.; Bertolino-Kusnerik, L. Neurobehavioural Consequences of Closed Head Injury in Older Adults. J. Neurol. Neurosurg. Psychiatry 1994, 57, 961–966. [Google Scholar] [CrossRef]
- Goldstein, F.C.; Levin, H.S.; Goldman, W.P.; Kalechstein, A.D.; Clark, A.N.; Kenehan-Altonen, T. Cognitive and Behavioral Sequelae of Closed Head Injury in Older Adults According to Their Significant Others. J. Neuropsychiatry Clin. Neurosci. 1999, 11, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Caron, L.; Ouellet, M.-C.; Hudon, C.; Predovan, D.; Sirois, M.-J.; de Guise, É.; Lamontagne, M.-È.; Émond, M.; Le Sage, N.; Beaulieu-Bonneau, S. Cognitive Functioning Following Traumatic Brain Injury in Older Adults: Associations with Social Participation and Health-Related Quality of Life. Brain Inj. 2022, 36, 1099–1108. [Google Scholar] [CrossRef] [PubMed]
- Deb, S.; Burns, J. Neuropsychiatric Consequences of Traumatic Brain Injury: A Comparison between Two Age Groups. Brain Inj. 2007, 21, 301–307. [Google Scholar] [CrossRef]
- Goldstein, F.C.; Levin, H.S.; Goldman, W.P.; Clark, A.N.; Altonen, T.K. Cognitive and Neurobehavioral Functioning after Mild versus Moderate Traumatic Brain Injury in Older Adults. J. Int. Neuropsychol. Soc. 2001, 7, 373–383. [Google Scholar] [CrossRef]
- Green, R.E.; Colella, B.; Christensen, B.; Johns, K.; Frasca, D.; Bayley, M.; Monette, G. Examining Moderators of Cognitive Recovery Trajectories After Moderate to Severe Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2008, 89, S16–S24. [Google Scholar] [CrossRef]
- Hume, C.H.; Wright, B.J.; Kinsella, G.J. Systematic Review and Meta-Analysis of Outcome after Mild Traumatic Brain Injury in Older People. J. Int. Neuropsychol. Soc. 2022, 28, 736–755. [Google Scholar] [CrossRef]
- Moretti, L.; Cristofori, I.; Weaver, S.M.; Chau, A.; Portelli, J.N.; Grafman, J. Cognitive Decline in Older Adults with a History of Traumatic Brain Injury. Lancet Neurol. 2012, 11, 1103–1112. [Google Scholar] [CrossRef]
- Rapoport, M.J.; Herrmann, N.; Shammi, P.; Kiss, A.; Phillips, A.; Feinstein, A. Outcome After Traumatic Brain Injury Sustained in Older Adulthood: A One-Year Longitudinal Study. Am. J. Geriatr. Psychiatry 2006, 14, 456–465. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, J.S.; Kiptanui, Z.; Tsang, Y.; Khokhar, B.; Liu, X.; Simoni-Wastila, L.; Zuckerman, I.H. Depression among Older Adults Following Traumatic Brain Injury: A National Analysis. Am. J. Geriatr. Psychiatry 2015, 23, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, J.S.; Barbour, L.; Abariga, S.A.; Rao, V.; Perfetto, E.M. Risk of Depression after Traumatic Brain Injury in a Large National Sample. J. Neurotrauma 2019, 36, 300–307. [Google Scholar] [CrossRef]
- Menzel, J.C. Depression in the Elderly after Traumatic Brain Injury: A Systematic Review. Brain Inj. 2008, 22, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Passler, J.S.; Sander, A.M.; Temkin, N.R.; Barber, J.; Gardner, R.C.; Manley, G.T. Depression in Older Adults 12 Months After Traumatic Brain Injury: A TRACK-TBI Study. Arch. Phys. Med. Rehabil. 2022, 103, 83–89. [Google Scholar] [CrossRef]
- Albrecht, J.S.; Peters, M.E.; Smith, G.S.; Rao, V. Anxiety and Post-Traumatic Stress Disorder among Medicare Beneficiaries Following Traumatic Brain Injury. J. Head Trauma Rehabil. 2017, 32, 178–184. [Google Scholar] [CrossRef]
- Osborn, A.J.; Mathias, J.L.; Fairweather-Schmidt, A.K.; Anstey, K.J. Anxiety and Comorbid Depression Following Traumatic Brain Injury in a Community-Based Sample of Young, Middle-Aged and Older Adults. J. Affect. Disord. 2017, 213, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Whelan-Goodinson, R.; Ponsford, J.L.; Schönberger, M.; Johnston, L. Predictors of Psychiatric Disorders Following Traumatic Brain Injury. J. Head Trauma Rehabil. 2010, 25, 320. [Google Scholar] [CrossRef]
- Kristman, V.L.; Brison, R.J.; Bédard, M.; Reguly, P.; Chisholm, S. Prognostic Markers for Poor Recovery After Mild Traumatic Brain Injury in Older Adults: A Pilot Cohort Study. J. Head Trauma Rehabil. 2016, 31, E33. [Google Scholar] [CrossRef]
- Pierce, C.A.; Hanks, R.A. Life Satisfaction After Traumatic Brain Injury and the World Health Organization Model of Disability. Am. J. Phys. Med. Rehabil. 2006, 85, 889. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability and Health; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Temkin, N.R.; Corrigan, J.D.; Dikmen, S.S.; Machamer, J. Social Functioning After Traumatic Brain Injury. J. Head Trauma Rehabil. 2009, 24, 460. [Google Scholar] [CrossRef] [PubMed]
- Huebner, R.A.; Johnson, K.; Bennett, C.M.; Schneck, C. Community Participation and Quality of Life Outcomes After Adult Traumatic Brain Injury. Am. J. Occup. Ther. 2003, 57, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Kalpinski, R.J.; Williamson, M.L.C.; Elliott, T.R.; Berry, J.W.; Underhill, A.T.; Fine, P.R. Modeling the Prospective Relationships of Impairment, Injury Severity, and Participation to Quality of Life Following Traumatic Brain Injury. BioMed Res. Int. 2013, 2013, e102570. [Google Scholar] [CrossRef] [PubMed]
- Sashika, H.; Takada, K.; Kikuchi, N. Rehabilitation Needs and Participation Restriction in Patients with Cognitive Disorder in the Chronic Phase of Traumatic Brain Injury. Medicine 2017, 96, e5968. [Google Scholar] [CrossRef] [PubMed]
- Erler, K.S.; Whiteneck, G.G.; Juengst, S.B.; Locascio, J.J.; Bogner, J.A.; Kaminski, J.; Giacino, J.T. Predicting the Trajectory of Participation After Traumatic Brain Injury: A Longitudinal Analysis. J. Head Trauma Rehabil. 2018, 33, 257. [Google Scholar] [CrossRef] [PubMed]
- Juengst, S.B.; Erler, K.S.; Neumann, D.; Kew, C.L.; Goldin, Y.; O’Neil-Pirozzi, T.M.; Rabinowitz, A.; Niemeier, J.; Bushnik, T.; Dijkers, M. Participation Importance and Satisfaction across the Lifespan: A Traumatic Brain Injury Model Systems Study. Rehabil. Psychol. 2022, 67, 344–355. [Google Scholar] [CrossRef] [PubMed]
- Lamberty, G.J.; Nakase-Richardson, R.; Farrell-Carnahan, L.; McGarity, S.; Bidelspach, D.; Harrison-Felix, C.; Cifu, D.X. Development of a Traumatic Brain Injury Model System Within the Department of Veterans Affairs Polytrauma System of Care. J. Head Trauma Rehabil. 2014, 29, E1. [Google Scholar] [CrossRef]
- Bogner, J.; Bellon, K.; Kolakowsky-Hayner, S.A.; Whiteneck, G. Participation Assessment With Recombined Tools–Objective (PART-O). J. Head Trauma Rehabil. 2013, 28, 337. [Google Scholar] [CrossRef]
- Bogner, J.A.; Whiteneck, G.G.; Corrigan, J.D.; Lai, J.-S.; Dijkers, M.P.; Heinemann, A.W. Comparison of Scoring Methods for the Participation Assessment With Recombined Tools–Objective. Arch. Phys. Med. Rehabil. 2011, 92, 552–563. [Google Scholar] [CrossRef]
- Whiteneck, G.G.; Dijkers, M.P.; Heinemann, A.W.; Bogner, J.A.; Bushnik, T.; Cicerone, K.D.; Corrigan, J.D.; Hart, T.; Malec, J.F.; Millis, S.R. Development of the Participation Assessment With Recombined Tools–Objective for Use After Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2011, 92, 542–551. [Google Scholar] [CrossRef] [PubMed]
- Ludlow, L.; Klein, K. Suppressor Variables: The Difference Between ‘Is’ Versus ‘Acting As’. J. Stat. Educ. 2014, 22, 2. [Google Scholar] [CrossRef]
- Niemeier, J.P.; Hammond, F.M.; O’Neil-Pirozzi, T.M.; Venkatesan, U.M.; Bushnik, T.; Zhang, Y.; Kennedy, R.E. Refining Understanding of Life Satisfaction in Elderly Persons with Traumatic Brain Injury Using Age-Defined Cohorts: A TBI Model Systems Study. Brain Inj. 2021, 35, 1284–1291. [Google Scholar] [CrossRef] [PubMed]
- Cuthbert, J.P.; Harrison-Felix, C.; Corrigan, J.D.; Bell, J.M.; Haarbauer-Krupa, J.K.; Miller, A.C. Unemployment in the United States After Traumatic Brain Injury for Working-Age Individuals: Prevalence and Associated Factors 2 Years Postinjury. J. Head Trauma Rehabil. 2015, 30, 160. [Google Scholar] [CrossRef] [PubMed]
- Malone, C.; Erler, K.S.; Giacino, J.T.; Hammond, F.M.; Juengst, S.B.; Locascio, J.J.; Nakase-Richardson, R.; Verduzco-Gutierrez, M.; Whyte, J.; Zasler, N.; et al. Participation Following Inpatient Rehabilitation for Traumatic Disorders of Consciousness: A TBI Model Systems Study. Front. Neurol. 2019, 10, 1314. [Google Scholar] [CrossRef] [PubMed]
- Simpson, G.K.; McRae, P.; Hallab, L.; Daher, M.; Strettles, B. Participation in Competitive Employment after Severe Traumatic Brain Injury: New Employment versus Return to Previous (Pre-Injury) Employment. Neuropsychol. Rehabil. 2020, 30, 995–1012. [Google Scholar] [CrossRef] [PubMed]
- Howe, E.I.; Andelic, N.; Perrin, P.B.; Røe, C.; Sigurdardottir, S.; Arango-Lasprilla, J.C.; Lu, J.; Løvstad, M.; Forslund, M.V. Employment Probability Trajectories Up to 10 Years after Moderate-to-Severe Traumatic Brain Injury. Front. Neurol. 2018, 9, 1051. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on the Review of the Department of Veterans Affairs Examinations for Traumatic Brain Injury. Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans; National Academies Press: Washington, DC, USA, 2019. [Google Scholar]
- Dahan-Oliel, N.; Gelinas, I.; Mazer, B. Social Participation in the Elderly: What Does the Literature Tell Us? Medicine 2008, 20, 2. [Google Scholar] [CrossRef]
- Kearney, P.; Plax, T.G.; Lentz, P.S. Participation in Community Organizations and Socioeconomic Status as Determinants of Seniors’ Life Satisfaction. Act. Adapt. Aging 1985, 6, 31–37. [Google Scholar] [CrossRef]
- McQuistion, K.; Zens, T.; Jung, H.S.; Beems, M.; Leverson, G.; Liepert, A.; Scarborough, J.; Agarwal, S. Insurance Status and Race Affect Treatment and Outcome of Traumatic Brain Injury. J. Surg. Res. 2016, 205, 261–271. [Google Scholar] [CrossRef]
- Asemota, A.O.; George, B.P.; Cumpsty-Fowler, C.J.; Haider, A.H.; Schneider, E.B. Race and Insurance Disparities in Discharge to Rehabilitation for Patients with Traumatic Brain Injury. J. Neurotrauma 2013, 30, 2057–2065. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Kumar, R.G.; Wisniewski, S.R.; Fabio, A. Disparities in Health Care Utilization of Adults with Traumatic Brain Injuries Are Related to Insurance, Race, and Ethnicity: A Systematic Review. J. Head Trauma Rehabil. 2018, 33, E40. [Google Scholar] [CrossRef] [PubMed]
- Gorman, J.A.; Chamberlin, E.S.; Stevenson, B.J.; Calixte, R.; Crossman, D.M.; Ahern, M.E.; Mack, J.; Russo, A.; Federman, E.J. Using Veterans Socials to Build a Community: Feasibility of the VOICES Intervention. Community Ment. Health J. 2022, 58, 1544–1553. [Google Scholar] [CrossRef] [PubMed]
- McLean, A.M.; Jarus, T.; Hubley, A.M.; Jongbloed, L. Associations between Social Participation and Subjective Quality of Life for Adults with Moderate to Severe Traumatic Brain Injury. Disabil. Rehabil. 2014, 36, 1409–1418. [Google Scholar] [CrossRef] [PubMed]
- Dizon, L.; Wiles, J.; Peiris-John, R. What Is Meaningful Participation for Older People? An Analysis of Aging Policies. Gerontologist 2020, 60, 396–405. [Google Scholar] [CrossRef] [PubMed]
- Aroogh, M.D.; Shahboulaghi, F.M. Social Participation of Older Adults: A Concept Analysis. Int. J. Community Based Nurs. Midwifery 2020, 8, 55. [Google Scholar]
- Sander, A.M.; Clark, A.; Pappadis, M.R. What Is Community Integration Anyway?: Defining Meaning following Traumatic Brain Injury. J. Head Trauma Rehabil. 2010, 25, 121. [Google Scholar] [CrossRef]

| Characteristics | (N = 185) |
|---|---|
| Age, M (SD) | 64.23 (6.79) |
| Sex, n (%) | |
| Male | 177 (95.7) |
| Female | 8 (4.3) |
| Race/Ethnicity, n (%) | |
| White | 137 (74.1) |
| Black | 19 (10.3) |
| Hispanic | 14 (7.6) |
| Asian | 1 (0.5) |
| American Indian | 3 (1.6) |
| Multiracial/Multiethnic | 5 (2.7) |
| Missing | 6 (3.2) |
| Education, M (SD) | 13.40 (2.73) |
| Marital Status n (%) | |
| Married | 99 (53.5) |
| Unmarried | 86 (46.5) |
| Insurance, n (%) | |
| Private | 36 (19.5) |
| Other | 116 (62.7) |
| Missing | 33 (17.8) |
| Employment at Injury, n (%) | |
| Competitively Employed | 73 (39.5) |
| Not Competitively Employed | 112 (60.5) |
| Problematic Substance Use, n (%) | 70 (37.8) |
| Pre-TBI Health, n (%) | |
| Limitations to Learning | 27 (14.6) |
| Limitations to Dressing | 8 (4.3) |
| Limitations to Working | 31 (16.8) |
| Limitations to Going Out of the Home | 10 (5.4) |
| Pre-TBI Mental Health Treatment, n (%) | 93 (50.3) |
| Days in Posttraumatic Amnesia, M (SD) | 43.58 (77.19) |
| Deployment to a Combat Zone, n (%) | 85 (49.5) |
| Cause of TBI, n (%) | |
| Motor Vehicle | 29 (15.7) |
| Motorcycle | 45 (24.3) |
| Bicycle | 12 (6.5) |
| All-Terrain Vehicle/Cycle (ATV/ATC) | 4 (2.2) |
| Gunshot Wound | 1 (0.5) |
| Assaults with Blunt Instrument | 7 (3.8) |
| Other Violence | 7 (3.8) |
| Fall | 66 (35.7) |
| Hit by Falling/Flying Object | 4 (2.2) |
| Pedestrian | 8 (4.3) |
| Other/Unknown | 2 (1.0) |
| Data Present % | Year 1 | Year 2 | Year 5 |
|---|---|---|---|
| PART-O Productivity | 73.5 | 70.8 | 39.5 |
| PART-O Social | 71.4 | 70.3 | 40.0 |
| PART-O Out and About | 74.6 | 71.4 | 40.0 |
| PART-O Productivity | PART-O Social | PART-O Out and About | ||||
|---|---|---|---|---|---|---|
| Characteristics | b-Weight | p-Value | b-Weight | p-Value | b-Weight | p-Value |
| Intercept | 0.74 | 0.203 | 10.06 | 0.113 | 0.99 | 0.100 |
| Time | −0.02 | 0.413 | −0.05 | 0.097 | −0.05 | 0.080 |
| Age | 0.00 | 0.956 | −0.04 | 0.029 | −0.02 | 0.271 |
| Sex (1 = male, 0 = female) | −0.41 | 0.280 | −0.17 | 0.697 | −0.05 | 0.900 |
| Race/Ethnicity | 0.08 | 0.696 | 0.03 | 0.887 | −0.20 | 0.342 |
| Education | 0.02 | 0.559 | 0.08 | 0.021 | 0.05 | 0.079 |
| Marital Status | −0.07 | 0.652 | 1.14 | <0.001 | 0.00 | 0.978 |
| Insurance Status | −0.09 | 0.615 | −0.43 | 0.033 | −0.19 | 0.297 |
| Problematic Substance Use | 0.09 | 0.552 | −0.26 | 0.121 | −0.24 | 0.112 |
| Pre-TBI Health Limitations | ||||||
| Learning | −0.43 | 0.073 | 0.19 | 0.490 | −0.14 | 0.554 |
| Dressing | 0.22 | 0.520 | 0.37 | 0.341 | 0.08 | 0.823 |
| Going Out of the Home | −0.16 | 0.670 | −0.25 | 0.567 | −0.63 | 0.109 |
| Working | 0.06 | 0.797 | −0.21 | 0.418 | 0.05 | 0.833 |
| Pre-TBI Mental Health Treatment | 0.27 | 0.106 | 0.00 | 0.993 | 0.16 | 0.348 |
| Days in Post Traumatic Amnesia | −0.15 | 0.079 | −0.13 | 0.186 | −0.11 | 0.218 |
| Deployment to a Combat Zone | 0.17 | 0.275 | −0.04 | 0.820 | 0.08 | 0.606 |
| Employment at Injury | 0.43 | 0.023 | −0.04 | 0.859 | −0.04 | 0.826 |
| Violent Cause of Injury | 0.24 | 0.474 | 0.13 | 0.726 | 0.07 | 0.837 |
| Interaction Effects | b-Weight | p-Value |
|---|---|---|
| PART-O Productivity | ||
| Time * Employed at Time of Injury | 0.16 | 0.624 |
| Part-O Social | ||
| Time * Age | −0.00 | 0.383 |
| Time * Education | 0.01 | 0.093 |
| Time * Marital Status | −0.04 | 0.270 |
| Time * Private Insurance vs. Other | 0.09 | 0.112 |
| PART-O Out and About | ||
| Time * Education Level | 0.00 | 0.535 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vasic, S.; Xia, B.; Dini, M.E.; Klyce, D.W.; Tyler, C.M.; Juengst, S.B.; Liou-Johnson, V.; Talley, K.G.; Dams-O’Connor, K.; Kumar, R.G.; et al. Community Participation Trajectories over the 5 Years after Traumatic Brain Injury in Older Veterans: A U.S. Veterans Affairs Model Systems Study. Trauma Care 2024, 4, 174-188. https://doi.org/10.3390/traumacare4020014
Vasic S, Xia B, Dini ME, Klyce DW, Tyler CM, Juengst SB, Liou-Johnson V, Talley KG, Dams-O’Connor K, Kumar RG, et al. Community Participation Trajectories over the 5 Years after Traumatic Brain Injury in Older Veterans: A U.S. Veterans Affairs Model Systems Study. Trauma Care. 2024; 4(2):174-188. https://doi.org/10.3390/traumacare4020014
Chicago/Turabian StyleVasic, Stefan, Bridget Xia, Mia E. Dini, Daniel W. Klyce, Carmen M. Tyler, Shannon B. Juengst, Victoria Liou-Johnson, Kelli G. Talley, Kristen Dams-O’Connor, Raj G. Kumar, and et al. 2024. "Community Participation Trajectories over the 5 Years after Traumatic Brain Injury in Older Veterans: A U.S. Veterans Affairs Model Systems Study" Trauma Care 4, no. 2: 174-188. https://doi.org/10.3390/traumacare4020014
APA StyleVasic, S., Xia, B., Dini, M. E., Klyce, D. W., Tyler, C. M., Juengst, S. B., Liou-Johnson, V., Talley, K. G., Dams-O’Connor, K., Kumar, R. G., Venkatesan, U. M., Engelman, B., & Perrin, P. B. (2024). Community Participation Trajectories over the 5 Years after Traumatic Brain Injury in Older Veterans: A U.S. Veterans Affairs Model Systems Study. Trauma Care, 4(2), 174-188. https://doi.org/10.3390/traumacare4020014






