Demographic and Geographic Trends in Gunshot Wound-Associated Orthopedic Injuries among Children, Adolescents, and Young Adults in New York State from 2016–2020
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Ethical Approval
2.3. Data Source and Patient Population
2.4. Inclusion and Exclusion Criteria
2.5. Variables Measured
2.6. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Incidence from 2016 to 2020
3.3. Geographic Incidence
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, L.K.; Mannix, R. Increasing Fatality Rates from Preventable Deaths in Teenagers and Young Adults. JAMA 2018, 320, 543–544. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.K.; Fleegler, E.W.; Goyal, M.K.; Doh, K.F.; Laraque-Arena, D.; Hoffman, B.D.; Injury, V.; Poison Prevention, C.O. Firearm-Related Injuries and Deaths in Children and Youth. Pediatrics 2022, 150, e2022060071. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, E.J.; Richmond, T.S.; Hoskins, K. Youth Firearm Injury: A Review for Pediatric Critical Care Clinicians. Crit. Care Clin. 2023, 39, 357–371. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, R.M.; Walton, M.A.; Carter, P.M. The Major Causes of Death in Children and Adolescents in the United States. N. Engl. J. Med. 2018, 379, 2468–2475. [Google Scholar] [CrossRef] [PubMed]
- Andrews, A.L.; Killings, X.; Oddo, E.R.; Gastineau, K.A.B.; Hink, A.B. Pediatric Firearm Injury Mortality Epidemiology. Pediatrics 2022, 149, e2021052739. [Google Scholar] [CrossRef] [PubMed]
- Quiroz, H.J.; Casey, L.C.; Parreco, J.P.; Willobee, B.A.; Rattan, R.; Lasko, D.S.; Perez, E.A.; Sola, J.E.; Thorson, C.M. Human and economic costs of pediatric firearm injury. J. Pediatr. Surg. 2020, 55, 944–949. [Google Scholar] [CrossRef] [PubMed]
- Boschert, E.N.; Stubblefield, C.E.; Reid, K.J.; Schwend, R.M. Twenty-two Years of Pediatric Musculoskeletal Firearm Injuries: Adverse Outcomes for the Very Young. J. Pediatr. Orthop. 2021, 41, e153–e160. [Google Scholar] [CrossRef] [PubMed]
- Rosas, S.; Gwam, C.U.; Araiza, E.T.; Roche, M.W.; Emory, C.L.; Carroll, E.A.; Halvorson, J.J.; Plate, J.F. Economic impact of orthopaedic care for non-fatal gunshot wounds: Analysis of a public health crisis. Ann. Transl. Med. 2021, 9, 210. [Google Scholar] [CrossRef] [PubMed]
- Naranje, S.M.; Gilbert, S.R.; Stewart, M.G.; Rush, J.K.; Bleakney, C.A.; McKay, J.E.; Warner, W.C., Jr.; Kelly, D.M.; Sawyer, J.R. Gunshot-associated Fractures in Children and Adolescents Treated at Two Level 1 Pediatric Trauma Centers. J. Pediatr. Orthop. 2016, 36, 1–5. [Google Scholar] [CrossRef]
- Evans, P.T.; Pennings, J.S.; Samade, R.; Lovvorn, H.N., 3rd; Martus, J.E. The financial burden of musculoskeletal firearm injuries in children with and without concomitant intra-cavitary injuries. J. Pediatr. Surg. 2020, 55, 1754–1760. [Google Scholar] [CrossRef]
- Hsu, Y.T.; Chen, Y.W.; Chang, D.C.; Perez, N.P.; Westfal, M.L.; Hung, Y.C.; Kelleher, C.M.; Masiakos, P.T.; Sacks, C.A. Annual Incidence of Hospitalization for Nonfatal Firearm-Related Injuries in New York from 2005 to 2016. JAMA Netw. Open 2021, 4, e2115713. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.S.; Donnelly, K.; Patel, S.J.; Badolato, G.M.; Boyle, M.D.; McCarter, R.; Goyal, M.K. Firearms Injuries Involving Young Children in the United States during the COVID-19 Pandemic. Pediatrics 2021, 148, e2020042697. [Google Scholar] [CrossRef] [PubMed]
- New York State Department of Health: Statewide Planning and Research Cooperative System (SPARCS). Available online: https://www.health.ny.gov/statistics/sparcs/ (accessed on 15 January 2022).
- Statewide Planning and Research Cooperative System Data Submission Compliance Protocol. 2024. Available online: https://www.health.ny.gov/statistics/sparcs/docs/sparcs_compliance.pdf (accessed on 2 June 2024).
- New York State Department of Health: New York State Trauma Centers. Available online: https://www.health.ny.gov/professionals/ems/state_trauma/trauma2.htm (accessed on 2 June 2024).
- United States Census Bureau: Population and Housing Unit Estimates. Available online: https://www.census.gov/programs-surveys/popest.html (accessed on 15 January 2022).
- Congiusta, D.V.; Oettinger, J.P.; Merchant, A.M.; Vosbikian, M.M.; Ahmed, I.H. Epidemiology of orthopaedic fractures due to firearms. J. Clin. Orthop. Trauma 2021, 12, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Tarkunde, Y.R.; Clohisy, C.J.; Calfee, R.P.; Halverson, S.J.; Wall, L.B. Firearm Injuries to the Wrist and Hand in Children and Adults: An Epidemiologic Study. Hand 2023, 18, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Perkins, C.; Scannell, B.; Brighton, B.; Seymour, R.; Vanderhave, K. Orthopaedic firearm injuries in children and adolescents: An eight-year experience at a major urban trauma center. Injury 2016, 47, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, S.; Mandelbaum, A.; Dobaria, V.; Williamson, C.G.; Tran, Z.; Sullins, V.; Benharash, P. National Trends in the Cost Burden of Pediatric Gunshot Wounds Across the United States. J. Pediatr. 2021, 236, 172–178.e174. [Google Scholar] [CrossRef] [PubMed]
- Parikh, K.; Silver, A.; Patel, S.J.; Iqbal, S.F.; Goyal, M. Pediatric Firearm-Related Injuries in the United States. Hosp. Pediatr. 2017, 7, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Choi, P.M.; Hong, C.; Bansal, S.; Lumba-Brown, A.; Fitzpatrick, C.M.; Keller, M.S. Firearm injuries in the pediatric population: A tale of one city. J. Trauma Acute Care Surg. 2016, 80, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.S.; Castilla, D.M.; Schulman, C.I.; Perez, E.A.; Neville, H.L.; Sola, J.E. Twenty years of pediatric gunshot wounds: An urban trauma center’s experience. J. Surg. Res. 2013, 184, 556–560. [Google Scholar] [CrossRef]
- Bayouth, L.; Lukens-Bull, K.; Gurien, L.; Tepas, J.J., 3rd; Crandall, M. Twenty years of pediatric gunshot wounds in our community: Have we made a difference? J. Pediatr. Surg. 2019, 54, 160–164. [Google Scholar] [CrossRef]
- Kalesan, B.; Vyliparambil, M.A.; Bogue, E.; Villarreal, M.D.; Vasan, S.; Fagan, J.; DiMaggio, C.J.; Stylianos, S.; Galea, S.; Firearm Injury Research Group. Race and ethnicity, neighborhood poverty and pediatric firearm hospitalizations in the United States. Ann. Epidemiol. 2016, 26, 1–6.e2. [Google Scholar] [CrossRef] [PubMed]
- Hughes, B.D.; Cummins, C.B.; Shan, Y.; Mehta, H.B.; Radhakrishnan, R.S.; Bowen-Jallow, K.A. Pediatric firearm injuries: Racial disparities and predictors of healthcare outcomes. J. Pediatr. Surg. 2020, 55, 1596–1603. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Moriarty, K.P.; Tashjian, D.B.; Patterson, L.A. Guns and states: Pediatric firearm injury. J. Trauma Acute Care Surg. 2013, 75, 50–53; discussion 53. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.K.; Badolato, G.M.; Patel, S.J.; Iqbal, S.F.; Parikh, K.; McCarter, R. State Gun Laws and Pediatric Firearm-Related Mortality. Pediatrics 2019, 144, e20183283. [Google Scholar] [CrossRef]
- Hamilton, E.C.; Miller, C.C., 3rd; Cox, C.S., Jr.; Lally, K.P.; Austin, M.T. Variability of child access prevention laws and pediatric firearm injuries. J. Trauma Acute Care Surg. 2018, 84, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Charder, N.; Liberatos, P.; Trobiano, M.; Dornbush, R.L.; Way, B.B.; Lerman, A. The Influence of New York’s SAFE Act on Individuals Seeking Mental Health Treatment. Psychiatr. Q. 2021, 92, 473–487. [Google Scholar] [CrossRef]
- Gollub, E.L.; Ben Taleb, Z. Gender in Children’s Firearm Deaths: Using the Data to Guide Interventions. Am. J. Med. 2016, 129, e141. [Google Scholar] [CrossRef]
- Donnelly, M.R.; Barie, P.S.; Grigorian, A.; Kuza, C.M.; Schubl, S.; de Virgilio, C.; Lekawa, M.; Nahmias, J. New York State and the Nation: Trends in Firearm Purchases and Firearm Violence during the COVID-19 Pandemic. Am. Surg. 2021, 87, 690–697. [Google Scholar] [CrossRef]
- Kim, D.Y.; Phillips, S.W. When COVID-19 and guns meet: A rise in shootings. J. Crim. Justice 2021, 73, 101783. [Google Scholar] [CrossRef]
- Abdallah, H.O.; Zhao, C.; Kaufman, E.; Hatchimonji, J.; Swendiman, R.A.; Kaplan, L.J.; Seamon, M.; Schwab, C.W.; Pascual, J.L. Increased Firearm Injury during the COVID-19 Pandemic: A Hidden Urban Burden. J. Am. Coll. Surg. 2021, 232, 159–168.e153. [Google Scholar] [CrossRef]
- Pino, E.C.; Gebo, E.; Dugan, E.; Jay, J. Trends in Violent Penetrating Injuries during the First Year of the COVID-19 Pandemic. JAMA Netw. Open 2022, 5, e2145708. [Google Scholar] [CrossRef] [PubMed]
- Inclan, P.M.; Velicki, K.; Christ, R.; Miller, A.N.; Brogan, D.M.; Dy, C.J. An Epidemic Amidst a Pandemic: Musculoskeletal Firearm Injuries during the COVID-19 Pandemic. J. Bone Jt. Surg. Am. 2022, 104, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Tatebe, L.C.; Sanchez, J.; Pekarek, S.; Koo, N.; Mis, J.; Schlanser, V.; Bokhari, F.; Dennis, A.J. Pediatric Firearm-Related Injuries: Taking Kids Out of Harm’s Way Begins with Targeted Prevention. J. Surg. Res. 2021, 267, 719–725. [Google Scholar] [CrossRef]
- Kind, A.J.H.; Buckingham, W.R. Making Neighborhood-Disadvantage Metrics Accessible—The Neighborhood Atlas. N. Engl. J. Med. 2018, 378, 2456–2458. [Google Scholar] [CrossRef] [PubMed]
- University of Wisconsin School of Medicine and Public Health 2019 Area Deprivation Index v2.0. Available online: https://www.neighborhoodatlas.medicine.wisc.edu/ (accessed on 2 June 2024).
- Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry Social Vulnerability Index. Available online: https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html (accessed on 19 February 2022).

| Variable | Mean ± SD or Count (%) |
|---|---|
| N | 637 |
| Age (years) | 18 ± 3 |
| Sex | Male: 583 (91.5%) |
| Female: 54 (8.5%) | |
| Race | Black: 446 (70.0%) |
| Hispanic: 96 (15.0%) | |
| Other: 55 (8.6%) | |
| White: 37 (5.8%) | |
| Asian: 3 (0.5%) | |
| Insurance | Medicaid: 309 (49.0%) |
| Managed care: 297 (46.5%) | |
| Self-pay: 24 (3.8%) | |
| Other: 7 (1.1%) | |
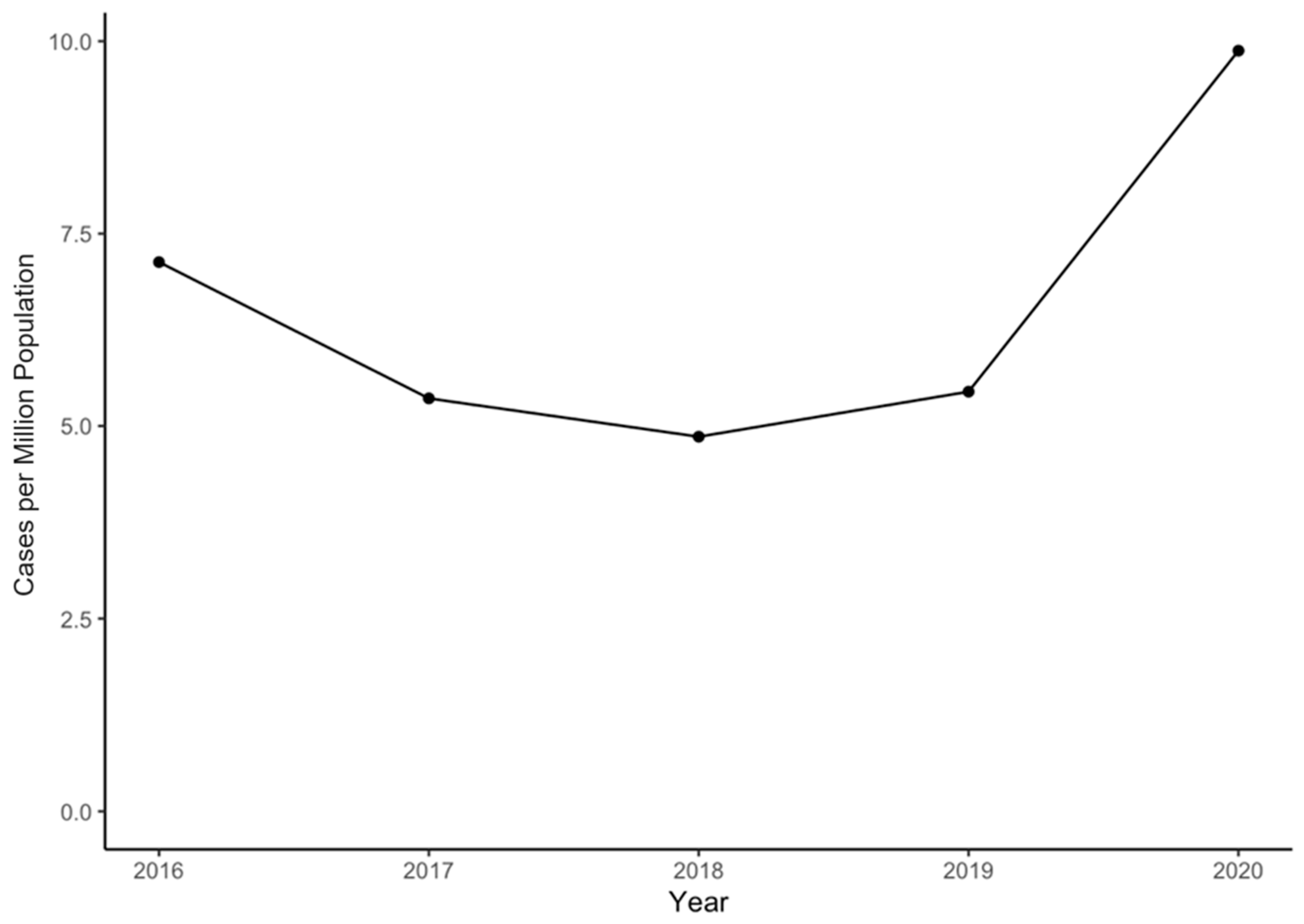
| Year | 2016: 140 (22%), incidence 7.13 PMP |
| 2017: 105 (16%), incidence 5.36 PMP | |
| 2018: 95 (15%), incidence 4.86 PMP | |
| 2019: 106 (17%), incidence 5.45 PMP | |
| 2020: 191 (30%), incidence 9.88 PMP |
| Year | IRR with 95% CI | Coefficient p-Value | Pearson Chi-Square p-Value |
|---|---|---|---|
| 2020 | — | — | <0.001 |
| 2019 | 0.55 [0.44, 0.70] | <0.001 | |
| 2018 | 0.5 [0.39, 0.63] | <0.001 | |
| 2017 | 0.55 [0.43, 0.70] | <0.001 | |
| 2016 | 0.73 [0.59, 0.91] | 0.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.C.; Shankar, D.S.; Anil, U.; Carter, C.W. Demographic and Geographic Trends in Gunshot Wound-Associated Orthopedic Injuries among Children, Adolescents, and Young Adults in New York State from 2016–2020. Trauma Care 2024, 4, 189-197. https://doi.org/10.3390/traumacare4020015
Lin CC, Shankar DS, Anil U, Carter CW. Demographic and Geographic Trends in Gunshot Wound-Associated Orthopedic Injuries among Children, Adolescents, and Young Adults in New York State from 2016–2020. Trauma Care. 2024; 4(2):189-197. https://doi.org/10.3390/traumacare4020015
Chicago/Turabian StyleLin, Charles C., Dhruv S. Shankar, Utkarsh Anil, and Cordelia W. Carter. 2024. "Demographic and Geographic Trends in Gunshot Wound-Associated Orthopedic Injuries among Children, Adolescents, and Young Adults in New York State from 2016–2020" Trauma Care 4, no. 2: 189-197. https://doi.org/10.3390/traumacare4020015
APA StyleLin, C. C., Shankar, D. S., Anil, U., & Carter, C. W. (2024). Demographic and Geographic Trends in Gunshot Wound-Associated Orthopedic Injuries among Children, Adolescents, and Young Adults in New York State from 2016–2020. Trauma Care, 4(2), 189-197. https://doi.org/10.3390/traumacare4020015





