The Influence of Diet, Exercise and Lifestyle Factors on Ocular Health
Definition
1. Introduction
2. Diet
3. Exercise
4. Air Pollution
5. Smoking/Vaping
6. Mental Health and Chronic Stress
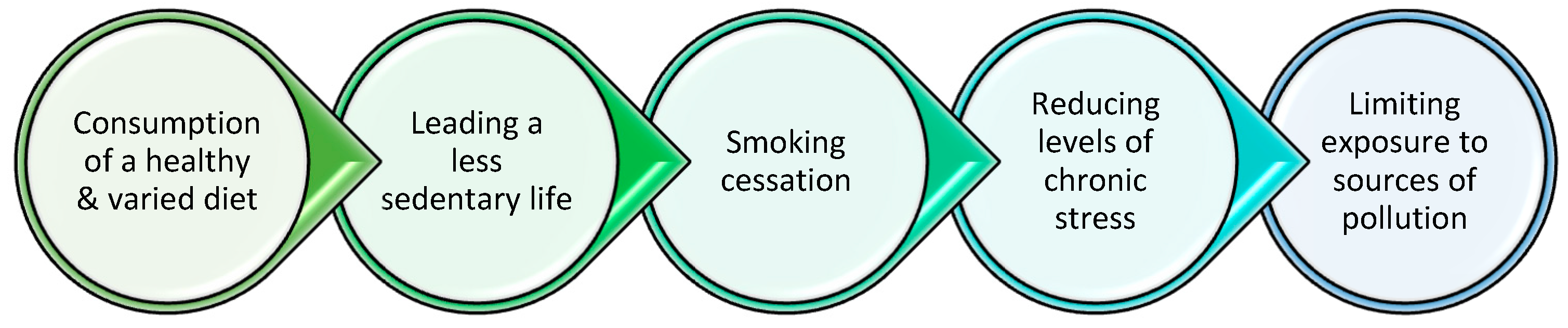
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Flaxman, S.R.; Bourne, R.R.; Resnikoff, S.; Ackland, P.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; et al. Global causes of blindness and distance vision impairment 1990–2020: A systematic review and meta-analysis. Lancet Glob. Health 2017, 5, e1221–e1234. [Google Scholar] [CrossRef]
- Steinmetz, J.D.; Bourne, R.R.; Briant, P.S.; Flaxman, S.R.; Taylor, H.R.; Jonas, J.B.; Abdoli, A.A.; Abrha, W.A.; Abualhasan, A.; Abu-Gharbieh, E.G.; et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The Right to Sight: An analysis for the Global Burden of Disease Study. Lancet Glob. Health 2021, 9, e144–e160. [Google Scholar] [CrossRef] [PubMed]
- Markoulli, M.; Ahmad, S.; Arcot, J.; Arita, R.; Benitez-del-Castillo, J.; Caffery, B.; Downie, L.E.; Edwards, K.; Flanagan, J.; Labetoulle, M.; et al. TFOS Lifestyle: Impact of nutrition on the ocular surface. Ocul. Surf. 2023, 29, 226–271. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, M.; Senni, C.; Bernabei, F.; Cicero, A.F.G.; Vagge, A.; Maestri, A.; Scorcia, V.; Giannaccare, G. The Role of Nutrition and Nutritional Supplements in Ocular Surface Diseases. Nutrients 2020, 12, 952. [Google Scholar] [CrossRef]
- Arivuchudar, R.; Tamilchudar, R. An Overview on the Sway of Nutritional Supplements on Dry Eye Disease. Res. J. Pharm. Technol. 2020, 13, 5004–5008. [Google Scholar] [CrossRef]
- Napolitano, P.; Filippelli, M.; Davinelli, S.; Bartollino, S.; dell’Omo, R.; Costagliola, C. Influence of gut microbiota on eye diseases: An overview. Ann. Med. 2021, 53, 750–761. [Google Scholar] [CrossRef] [PubMed]
- Bu, Y.; Chan, Y.K.; Wong, H.L.; Poon, S.H.L.; Lo, A.C.Y.; Shih, K.C.; Tong, L. A review of the impact of alterations in gut microbiome on the immunopathogenesis of ocular diseases. J. Clin. Med. 2021, 10, 4694. [Google Scholar] [CrossRef]
- Chapman, N.A.; Jacobs, R.J.; Braakhuis, A.J. Role of diet and food intake in age-related macular degeneration: A systematic review. Clin. Exp. Ophthalmol. 2019, 47, 106–127. [Google Scholar] [CrossRef]
- Grant, M.B.; Bernstein, P.S.; Boesze-Battaglia, K.; Chew, E.; Curcio, C.A.; Kenney, M.C.; Klaver, C.; Philp, N.J.; Rowan, S.; Sparrow, J.; et al. Inside out: Relations between the microbiome, nutrition, and eye health. Exp. Eye Res. 2022, 224, 109216. [Google Scholar] [CrossRef]
- Wu, Y.; Xie, Y.; Yuan, Y.; Xiong, R.; Hu, Y.; Ning, K.; Ha, J.; Wang, W.; Han, X.; He, M. The Mediterranean diet and age-related eye diseases: A systematic review. Nutrients 2023, 15, 2043. [Google Scholar] [CrossRef]
- Weikel, K.A.; Garber, C.; Baburins, A.; Taylor, A. Nutritional modulation of cataract. Nutr. Rev. 2014, 72, 30–47. [Google Scholar] [CrossRef]
- Mathew, M.C.; Ervin, A.M.; Tao, J.; Davis, R.M. Antioxidant vitamin supplementation for preventing and slowing the progression of age-related cataract. Cochrane Database Syst. Rev. 2012, 6, CD004567. [Google Scholar] [CrossRef]
- Chang, K.H.; Hsu, P.Y.; Lin, C.J.; Lin, C.L.; Juo, S.H.H.; Liang, C.L. Traffic-related air pollutants increase the risk for age-related macular degeneration. J. Investig. Med. 2019, 67, 1076–1081. [Google Scholar] [CrossRef]
- Downie, L.E.; Ng, S.M.; Lindsley, K.B.; Akpek, E.K. Omega-3 and omega-6 polyunsaturated fatty acids for dry eye disease. Cochrane Database Syst. Rev. 2019, 12, CD011016. [Google Scholar] [CrossRef]
- Ng, A.; Woods, J.; Jahn, T.; Jones, L.W.; Ritter, J.S. Effect of a novel omega-3 and omega-6 fatty acid supplement on dry eye disease: A 3-month randomized controlled trial. Optom. Vis. Sci. 2022, 99, 67–75. [Google Scholar] [CrossRef]
- Saccà, S.C.; Izzotti, A.; Rossi, P.; Traverso, C. Glaucomatous outflow pathway and oxidative stress. Exp. Eye Res. 2007, 84, 389–399. [Google Scholar] [CrossRef]
- Zanon-Moreno, V.; Marco-Ventura, P.; Lleo-Perez, A.; Pons-Vazquez, S.; Garcia-Medina, J.J.; Vinuesa-Silva, I.; Moreno-Nadal, M.A.; Pinazo-Duran, M.D. Oxidative stress in primary open-angle glaucoma. J. Glaucoma 2008, 17, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Martucci, A.; Nucci, C. Evidence on neuroprotective properties of coenzyme Q10 in the treatment of glaucoma. Neural Regen. Res. 2019, 14, 197–200. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.S.; Harris, A.; Kristinsson, J.K.; Ciulla, T.A.; Kagemann, C.; Ritch, R. Ginkgo biloba extract increases ocular blood flow velocity. J. Ocul. Pharmacol. Ther. 1999, 15, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Song, J.E.; Kim, J.M.; Lee, M.Y.; Jang, H.J.; Park, K.H. Effects of consumption of alcohol on intraocular pressure: Korea National Health and Nutrition Examination Survey 2010 to 2011. Nutrients 2020, 12, 2420. [Google Scholar] [CrossRef]
- Bae, J.H.; Kim, J.M.; Lee, J.M.; Song, J.E.; Lee, M.Y.; Chung, P.W.; Park, K.H. Effects of consumption of coffee, tea, or soft drinks on open-angle glaucoma: Korea National Health and Nutrition Examination Survey 2010 to 2011. PLoS ONE 2020, 15, e0236152. [Google Scholar] [CrossRef]
- Kim, J.; Aschard, H.; Kang, J.H.; Lentjes, M.A.; Do, R.; Wiggs, J.L.; Khawaja, A.P.; Pasquale, L.R.; Modifiable Risk Factors for Glaucoma Collaboration. Intraocular pressure, glaucoma, and dietary caffeine consumption: A gene–diet interaction study from the UK Biobank. Ophthalmology 2021, 128, 866–876. [Google Scholar] [CrossRef]
- Jeong, K.J.; Choi, J.G.; Park, E.J.; Kim, H.E.; Yoo, S.M.; Park, S.G. Relationship between dry eye syndrome and frequency of coffee consumption in Korean adults: Korea National Health and Nutrition Examination Survey V, 2010–2012. Korean J. Fam. Med. 2018, 39, 290. [Google Scholar] [CrossRef]
- García-Marqués, J.V.; Talens-Estarelles, C.; García-Lázaro, S.; Wolffsohn, J.S.; Cervino, A. Systemic, environmental and lifestyle risk factors for dry eye disease in a mediterranean caucasian population. Contact Lens Anterior Eye 2022, 45, 101539. [Google Scholar] [CrossRef]
- Magno, M.S.; Utheim, T.P.; Morthen, M.K.; Snieder, H.; Jansonius, N.M.; Hammond, C.J.; Vehof, J. The relationship between caffeine intake and dry eye disease. Cornea 2023, 42, 186–193. [Google Scholar] [CrossRef]
- Osei, K.A.; Ovenseri-Ogbomo, G.; Kyei, S.; Ntodie, M. The effect of caffeine on tear secretion. Optom. Vis. Sci. 2014, 91, 171–177. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, J.H.; Nam, W.H.; Yi, K.; Choi, D.G.; Hyon, J.Y.; Wee, W.R.; Shin, Y.J. Oral alcohol administration disturbs tear film and ocular surface. Ophthalmology 2012, 119, 965–971. [Google Scholar] [CrossRef] [PubMed]
- Galor, A.; Britten-Jones, A.C.; Feng, Y.; Ferrari, G.; Goldblum, D.; Gupta, P.K.; Merayo-Lloves, J.; Na, K.S.; Naroo, S.A.; Nichols, K.K.; et al. TFOS Lifestyle: Impact of lifestyle challenges on the ocular surface. Ocul. Surf. 2023, 28, 262–303. [Google Scholar] [CrossRef] [PubMed]
- Shetty, R.; Deshpande, K.; Deshmukh, R.; Jayadev, C.; Shroff, R. Bowman break and subbasal nerve plexus changes in a patient with dry eye presenting with chronic ocular pain and vitamin D deficiency. Cornea 2016, 35, 688–691. [Google Scholar] [CrossRef] [PubMed]
- Acar, M.; Firat, H.; Acar, U.; Ardic, S. Ocular surface assessment in patients with obstructive sleep apnea–hypopnea syndrome. Sleep Breath. 2013, 17, 583–588. [Google Scholar] [CrossRef]
- Gupta, P.K.; Venkateswaran, N.; Heinke, J.; Stinnett, S.S. Association of meibomian gland architecture and body mass index in a pediatric population. Ocul. Surf. 2020, 18, 657–662. [Google Scholar] [CrossRef]
- Di Vincenzo, R.; Kierzkowska, E.; Osiecki, H. Bioavailability. J. Complement. Med. CM 2004, 3, 62–71. [Google Scholar]
- Burke, A.; Lichtenstein, G.R.; Rombeau, J.L. Nutrition and ulcerative colitis. Baillière’s Clin. Gastroenterol. 1997, 11, 153–174. [Google Scholar] [CrossRef]
- Ismail, A.M.A.; El-Azeim, A.S.A.; Saif, H.F.A.E.A. Effect of aerobic exercise alone or combined with Mediterranean diet on dry eye in obese hypertensive elderly. Ir. J. Med. Sci. 2023, 192, 3151–3161. [Google Scholar] [CrossRef] [PubMed]
- Chakravarthy, U.; Williams, M. The royal college of ophthalmologists guidelines on AMD: Executive summary. Eye 2013, 27, 1429–1431. [Google Scholar] [CrossRef]
- Munch, I.C.; Linneberg, A.; Larsen, M. Precursors of age-related macular degeneration: Associations with physical activity, obesity, and serum lipids in the inter99 eye study. Investig. Ophthalmol. Vis. Sci. 2013, 54, 3932–3940. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Herod, S.M.; Cardinal, B.J.; Noakes, T.D. Physical activity and the brain: A review of this dynamic, bi-directional relationship. Brain Res. 2013, 1539, 95–104. [Google Scholar] [CrossRef]
- Wang, M.T.; Muntz, A.; Wolffsohn, J.S.; Craig, J.P. Association between dry eye disease, self-perceived health status, and self-reported psychological stress burden. Clin. Exp. Optom. 2021, 104, 835–840. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, B.E.; Cooley, S.S.; Davidorf, F. The relationship between perceived stress and self-reported visual function in patients with neovascular age-related macular degeneration (AMD). Investig. Ophthalmol. Vis. Sci. 2015, 56, 1370. [Google Scholar]
- Risner, D.; Ehrlich, R.; Kheradiya, N.S.; Siesky, B.; McCranor, L.; Harris, A. Effects of exercise on intraocular pressure and ocular blood flow: A review. J. Glaucoma 2009, 18, 429–436. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Swenor, B.K.; Ramulu, P.Y. Age-related macular degeneration is associated with less physical activity among US adults: Cross-sectional study. PLoS ONE 2015, 10, e0125394. [Google Scholar] [CrossRef]
- Praidou, A.; Harris, M.; Niakas, D.; Labiris, G. Physical activity and its correlation to diabetic retinopathy. J. Diabetes Its Complicat. 2017, 31, 456–461. [Google Scholar] [CrossRef]
- Yan, X.; Han, X.; Wu, C.; Shang, X.; Zhang, L.; He, M. Effect of physical activity on reducing the risk of diabetic retinopathy progression: 10-year prospective findings from the 45 and up Study. PLoS ONE 2021, 16, e0239214. [Google Scholar] [CrossRef]
- Dirani, M.; Crowston, J.; van Wijngaarden, P. Physical inactivity as a risk factor for diabetic retinopathy? A review. Clin. Exp. Ophthalmol. 2014, 42, 574–581. [Google Scholar] [CrossRef]
- Zhang, Q.; Jiang, Y.; Deng, C.; Wang, J. Effects and potential mechanisms of exercise and physical activity on eye health and ocular diseases. Front. Med. 2024, 11, 1353624. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.H.; Khachadurian, A.K.; Amorosa, L.F.; Clemow, L.; Ruderman, N.B. Tenyear experience with an exercise-based outpatient life-style modification program in the treatment of diabetes mellitus. Diabetes Care 1992, 15, 1800–1810. [Google Scholar] [CrossRef]
- Irvine, C.; Taylor, N.F. Progressive resistance exercise improves glycaemic control in people with type 2 diabetes mellitus: A systematic review. Aust. J. Physiother. 2009, 55, 237–246. [Google Scholar] [CrossRef]
- Pollock, M.L.; Carroll, J.F.; Graves, J.E.; Leggett, S.H.; Braith, R.W.; Limacher, M.A.R.I.A.N.; Hagberg, J.M. Injuries and adherence to walk/jog and resistance training programs in the elderly. Med. Sci. Sports Exerc. 1991, 23, 1194–1200. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Li, F.; Zhou, R.; Gao, K.; Liang, L.; Zhang, X. Aerobic exercise increases tear secretion and decreases inflammatory cytokines in healthy subjects. Asia-Pac. J. Ophthalmol. 2020, 9, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Bennitt, F.B.; Wozniak, S.; Causey, K.; Spearman, S.; Okereke, C.; Garcia, V.; Hashmeh, N.; Ashbaugh, C.; Abdelkader, A.; Abdoun, M.; et al. Global, regional, and national burden of household air pollution, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2025, 405, 1167–1181. [Google Scholar] [CrossRef]
- World Health Organization. Ambient (Outdoor) Air Pollution. 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 12 June 2025).
- Diaz, E.; Smith-Sivertsen, T.; Pope, D.; Lie, R.T.; Diaz, A.; McCracken, J.; Arana, B.; Smith, K.R.; Bruce, N. Eye discomfort, headache and back pain among Mayan Guatemalan women taking part in a randomised stove intervention trial. J. Epidemiol. Community Health 2007, 61, 74–79. [Google Scholar] [CrossRef]
- Shin, J.; Lee, H.; Kim, H. Association between exposure to ambient air pollution and age-related cataract: A nationwide population-based retrospective cohort study. Int. J. Environ. Res. Public Health 2020, 17, 9231. [Google Scholar] [CrossRef]
- Millen, A.E.; Dighe, S.; Kordas, K.; Aminigo, B.Z.; Zafron, M.L.; Mu, L. Air pollution and chronic eye disease in adults: A scoping review. Ophthalmic Epidemiol. 2024, 31, 1–10. [Google Scholar] [CrossRef]
- Wang, W.; He, M.; Li, Z.; Huang, W. Epidemiological variations and trends in health burden of glaucoma worldwide. Acta Ophthalmol. 2019, 97, e349–e355. [Google Scholar] [CrossRef] [PubMed]
- Chua, S.Y.; Khawaja, A.P.; Morgan, J.; Strouthidis, N.; Reisman, C.; Dick, A.D.; Khaw, P.T.; Patel, P.J.; Foster, P.J.; UK Biobank Eye and Vision Consortium. The relationship between ambient atmospheric fine particulate matter (PM2. 5) and glaucoma in a large community cohort. Investig. Ophthalmol. Vis. Sci. 2019, 60, 4915–4923. [Google Scholar] [CrossRef] [PubMed]
- Hetland, R.B.; Cassee, F.R.; Låg, M.; Refsnes, M.; Dybing, E.; Schwarze, P.E. Cytokine release from alveolar macrophages exposed to ambient particulate matter: Heterogeneity in relation to size, city and season. Part. Fibre Toxicol. 2005, 2, 4. [Google Scholar] [CrossRef]
- Vohra, K.; Vodonos, A.; Schwartz, J.; Marais, E.A.; Sulprizio, M.P.; Mickley, L.J. Global mortality from outdoor fine particle pollution generated by fossil fuel combustion: Results from GEOS-Chem. Environ. Res. 2021, 195, 110754. [Google Scholar] [CrossRef] [PubMed]
- Kappos, A.D.; Bruckmann, P.; Eikmann, T.; Englert, N.; Heinrich, U.; Höppe, P.; Koch, E.; Krause, G.H.; Kreyling, W.G.; Rauchfuss, K.; et al. Health effects of particles in ambient air. Int. J. Hyg. Environ. Health 2004, 207, 399–407. [Google Scholar] [CrossRef]
- Holguin, F. Traffic, outdoor air pollution, and asthma. Immunol. Allergy Clin. N. Am. 2008, 28, 577–588. [Google Scholar] [CrossRef]
- Chua, S.Y.; Khawaja, A.P.; Desai, P.; Rahi, J.S.; Day, A.C.; Hammond, C.J.; Khaw, P.T.; Foster, P.J. The association of ambient air pollution with cataract surgery in UK biobank participants: Prospective cohort study. Investig. Ophthalmol. Vis. Sci. 2021, 62, 7. [Google Scholar] [CrossRef]
- Grant, A.; Leung, G.; Aubin, M.J.; Kergoat, M.J.; Li, G.; Freeman, E.E. Fine particulate matter and age-related eye disease: The Canadian longitudinal study on aging. Investig. Ophthalmol. Vis. Sci. 2021, 62, 7. [Google Scholar] [CrossRef]
- Chua, S.Y.; Warwick, A.; Peto, T.; Balaskas, K.; Moore, A.T.; Reisman, C.; Desai, P.; Lotery, A.J.; Dhillon, B.; Khaw, P.T.; et al. Association of ambient air pollution with age-related macular degeneration and retinal thickness in UK Biobank. Br. J. Ophthalmol. 2022, 106, 705–711. [Google Scholar] [CrossRef]
- Saha, A.; Kulkarni, P.K.; Shah, A.; Patel, M.; Saiyed, H.N. Ocular morbidity and fuel use: An experience from India. Occup. Environ. Med. 2005, 62, 66–69. [Google Scholar] [CrossRef]
- Fullerton, D.G.; Bruce, N.; Gordon, S.B. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 843–851. [Google Scholar] [CrossRef]
- Nita, M.; Grzybowski, A. Smoking and eye pathologies. A systemic review. Part I. Anterior eye segment pathologies. Curr. Pharm. Des. 2017, 23, 629–638. [Google Scholar] [CrossRef]
- Asiamah, R.; Ampo, E.; Ampiah, E.E.; Nketia, M.O.; Kyei, S. Impact of smoking on ocular health: A systematic review and meta-meta-analysis. Eur. J. Ophthalmol. 2025, 35, 1506–1518. [Google Scholar] [CrossRef]
- Pokhrel, A.K.; Smith, K.R.; Khalakdina, A.; Deuja, A.; Bates, M.N. Case–control study of indoor cooking smoke exposure and cataract in Nepal and India. Int. J. Epidemiol. 2005, 34, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Raju, P.; George, R.; Ramesh, S.V.; Arvind, H.; Baskaran, M.; Vijaya, L. Influence of tobacco use on cataract development. Br. J. Ophthalmol. 2006, 90, 1374–1377. [Google Scholar] [CrossRef] [PubMed]
- Khan, J.C.; Thurlby, D.A.; Shahid, H.; Clayton, D.G.; Yates, J.R.W.; Bradley, M.; Moore, A.T.; Bird, A.C. Smoking and age related macular degeneration: The number of pack years of cigarette smoking is a major determinant of risk for both geographic atrophy and choroidal neovascularisation. Br. J. Ophthalmol. 2006, 90, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, R.B.; Coletta, R.D.; Silvério, K.G.; Benevides, L.; Casati, M.Z.; Da Silva, J.S.; Nociti, F.H. Impact of smoking on inflammation: Overview of molecular mechanisms. Inflamm. Res. 2011, 60, 409–424. [Google Scholar] [CrossRef]
- Iho, S.; Tanaka, Y.; Takauji, R.; Kobayashi, C.; Muramatsu, I.; Iwasaki, H.; Nakamura, K.; Sasaki, Y.; Nakao, K.; Takahashi, T. Nicotine induces human neutrophils to produce IL-8 through the generation of peroxynitrite and subsequent activation of NF-κB. J. Leucoc. Biol. 2003, 74, 942–951. [Google Scholar] [CrossRef]
- Moss, S.E.; Klein, R.; Klein, B.E. Incidence of dry eye in an older population. Arch. Ophthalmol. 2004, 122, 369–373. [Google Scholar] [CrossRef]
- Altinors, D.D.; Akça, S.; Akova, Y.A.; Bilezikçi, B.; Goto, E.; Dogru, M.; Tsubota, K. Smoking associated with damage to the lipid layer of the ocular surface. Am. J. Ophthalmol. 2006, 141, 1016–1021. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.; Jacob, G.P.; Abraham, L.; Noushad, B. The effect of smoking on the ocular surface and the precorneal tear film. Australas. Med. J. 2012, 5, 221. [Google Scholar] [CrossRef] [PubMed]
- Sayin, N.; Kara, N.; Pekel, G.; Altinkaynak, H. Effects of chronic smoking on central corneal thickness, endothelial cell, and dry eye parameters. Cutan. Ocul. Toxicol. 2014, 33, 201–205. [Google Scholar] [CrossRef]
- Xu, L.; Zhang, W.; Zhu, X.Y.; Suo, T.; Fan, X.Q.; Fu, Y. Smoking and the risk of dry eye: A Meta-analysis. Int. J. Ophthalmol. 2016, 9, 1480. [Google Scholar] [CrossRef]
- Patel, S.; Tohme, N.; Gorrin, E.; Kumar, N.; Goldhagen, B.; Galor, A. Prevalence and risk factors for chalazion in an older veteran population. Br. J. Ophthalmol. 2022, 106, 1200–1205. [Google Scholar] [CrossRef]
- Martheswaran, T.; Shmunes, M.H.; Ronquillo, Y.C.; Moshirfar, M. The impact of vaping on ocular health: A literature review. Int. Ophthalmol. 2021, 41, 2925–2932. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Wu, X.; Lin, X.; Lin, H. The prevalence of depression and depressive symptoms among eye disease patients: A systematic review and meta-analysis. Sci. Rep. 2017, 7, 46453. [Google Scholar] [CrossRef]
- Galor, A.; Feuer, W.; Lee, D.J.; Florez, H.; Faler, A.L.; Zann, K.L.; Perez, V.L. Depression, post-traumatic stress disorder, and dry eye syndrome: A study utilizing the national United States Veterans Affairs administrative database. Am. J. Ophthalmol. 2012, 154, 340–346. [Google Scholar] [CrossRef]
- Van Der Vaart, R.; Weaver, M.A.; Lefebvre, C.; Davis, R.M. The association between dry eye disease and depression and anxiety in a large population-based study. Am. J. Ophthalmol. 2015, 159, 470–474. [Google Scholar] [CrossRef]
- Basilious, A.; Xu, C.Y.; Malvankar-Mehta, M.S. Dry eye disease and psychiatric disorders: A systematic review and meta-analysis. Eur. J. Ophthalmol. 2022, 32, 1872–1889. [Google Scholar] [CrossRef] [PubMed]
- Koçer, E.; Koçer, A.; Özsütçü, M.; Dursun, A.E.; Kirpinar, I. Dry eye related to commonly used new antidepressants. J. Clin. Psychopharmacol. 2015, 35, 411–413. [Google Scholar] [CrossRef]
- Vehof, J.; Snieder, H.; Jansonius, N.; Hammond, C.J. Prevalence and risk factors of dry eye in 79,866 participants of the population-based Lifelines cohort study in the Netherlands. Ocul. Surf. 2021, 19, 83–93. [Google Scholar] [CrossRef]
- Wen, W.; Wu, Y.; Chen, Y.; Gong, L.; Li, M.; Chen, X.; Yan, M.; Xiao, Z.; Sun, X. Dry eye disease in patients with depressive and anxiety disorders in Shanghai. Cornea 2012, 31, 686–692. [Google Scholar] [CrossRef]
- Cui, B.; Guo, X.; Zhou, W.; Zhang, X.; He, K.; Bai, T.; Lin, D.; Wei-Zhang, S.; Zhao, Y.; Liu, S.; et al. Exercise alleviates neovascular age-related macular degeneration by inhibiting AIM2 inflammasome in myeloid cells. Metabolism 2023, 144, 155584. [Google Scholar] [CrossRef]
- Tang, W.S.W.; Lau, N.X.M.; Krishnan, M.N.; Chin, Y.C.; Ho, C.S.H. Depression and eye disease—A narrative review of common underlying pathophysiological mechanisms and their potential applications. J. Clin. Med. 2024, 13, 3081. [Google Scholar] [CrossRef]
- Galor, A.; Felix, E.R.; Feuer, W.; Shalabi, N.; Martin, E.R.; Margolis, T.P.; Sarantopoulos, C.D.; Levitt, R.C. Dry eye symptoms align more closely to non-ocular conditions than to tear film parameters. Br. J. Ophthalmol. 2015, 99, 1126–1129. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Wang, M.T.; Vidal-Rohr, M.; Menduni, F.; Dhallu, S.; Ipek, T.; Acar, D.; Recchioni, A.; France, A.; Kingsnorth, A.; et al. Demographic and lifestyle risk factors of dry eye disease subtypes: A cross-sectional study. Ocul. Surf. 2021, 21, 58–63. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dhallu, S.K. The Influence of Diet, Exercise and Lifestyle Factors on Ocular Health. Encyclopedia 2025, 5, 159. https://doi.org/10.3390/encyclopedia5040159
Dhallu SK. The Influence of Diet, Exercise and Lifestyle Factors on Ocular Health. Encyclopedia. 2025; 5(4):159. https://doi.org/10.3390/encyclopedia5040159
Chicago/Turabian StyleDhallu, Sandeep Kaur. 2025. "The Influence of Diet, Exercise and Lifestyle Factors on Ocular Health" Encyclopedia 5, no. 4: 159. https://doi.org/10.3390/encyclopedia5040159
APA StyleDhallu, S. K. (2025). The Influence of Diet, Exercise and Lifestyle Factors on Ocular Health. Encyclopedia, 5(4), 159. https://doi.org/10.3390/encyclopedia5040159






