A Scoping Review for Hamstring Injury Risk Monitoring in Australian Rules Football
Abstract
1. Introduction
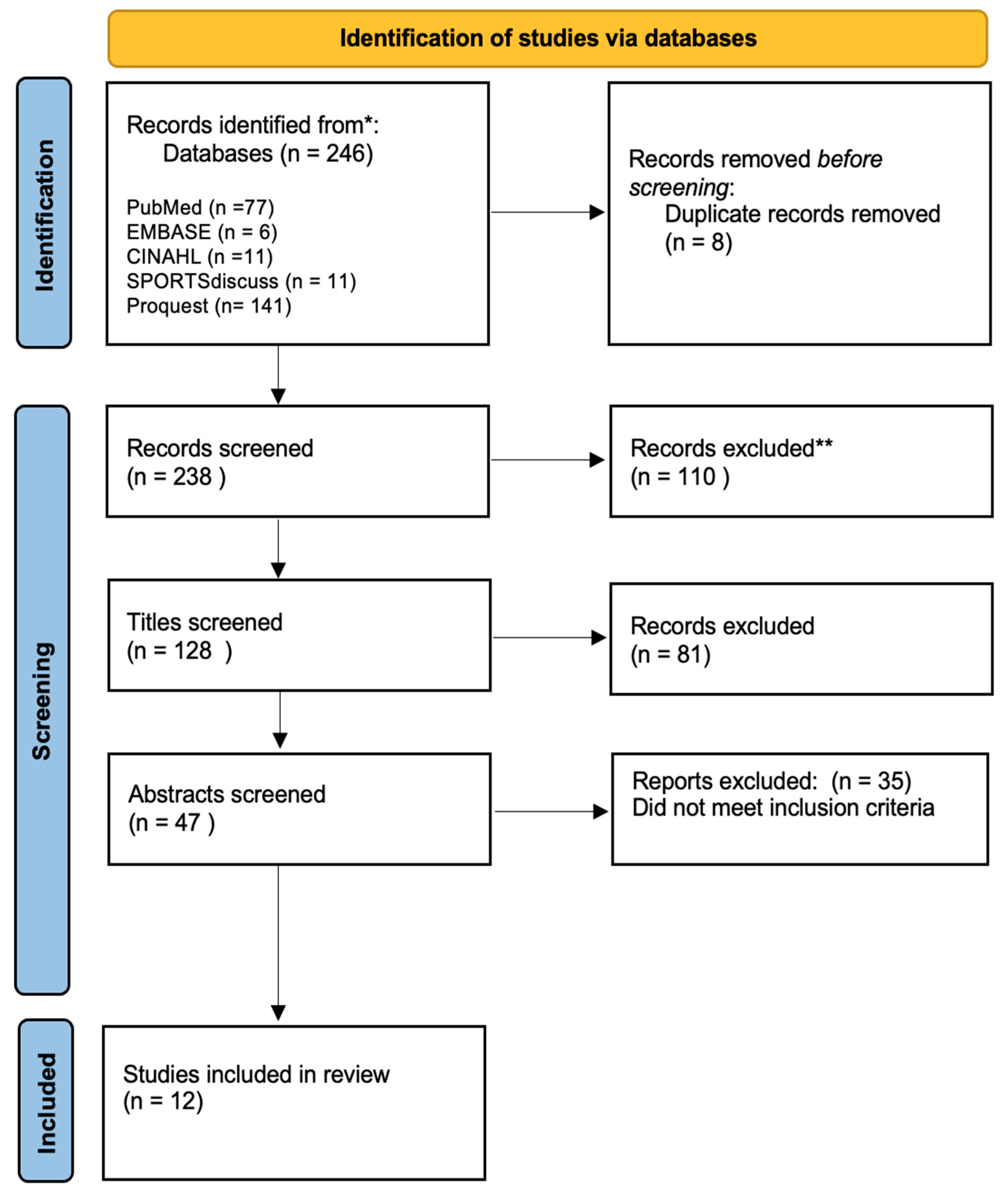
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy, Data Collection and Extraction
3. Results
3.1. Modifiable Factors
3.1.1. High-Speed Running Exposure
3.1.2. Gluteus Maximus (GMAX) and Medius (GMED) Size and Activation
3.1.3. Eccentric Hamstring Strength
3.1.4. Long Head of Biceps Femoris Fascicle Length
3.1.5. Use of Interchanges
3.1.6. Knee and Hip Proprioception
3.1.7. Hamstring Stiffness
3.2. Non-Modifiable Factors
3.2.1. History of Injuries
3.2.2. Age
3.2.3. Size of a Hamstring Injury on MRI to Predict Recurrence
| Risk Factor | Reference | Predictors of Injury Results, p-Value, Odds Ratio (OR), Confidence Intervals (CI) |
|---|---|---|
| High-speed running | [21] |
|
| [22] |
| |
| Gluteus medius (GMED) and gluteus maximus (GMAX) muscle volume and activation (EMG) | [23] |
|
| Unilateral hamstring stiffness | [25] |
|
| Long head of bicep femoris fascicle length | [10] |
|
| Increased use of interchanges | [4] |
|
| Eccentric hamstring strength | [11] |
|
| [12] |
| |
| [6] |
| |
| Hip and knee proprioception | [24] |
|
4. Discussion
5. Holistic Approach to Injury Profiling
- Hamstring strength and in particular monitoring of eccentric hamstring strength is highly recommended. This requires further and up to date research, expanding the hamstring strength monitoring to also include the quadriceps, and systematically monitoring the H:Q ratio in male AFL players. We recommend that researchers in AFL consider exploring the utility of the eccentric H:Q ratio, as this been proposed as more reflective of injury mechanism than conventional concentric ratios [37,49].
- Application of a practical and contemporary technique for determining lower body stiffness, such as that reported by Watsford and associates [25].
- Athlete wellbeing and behavioral monitoring inclusive of sleep, recovery, nutritional habits, and psychosocial factors. However, researchers need to determine stronger causational links between negative psychosocial factors and increased HSI risk.
6. Limitations
7. Advances in Hamstring Injury Risk Prediction and Monitoring
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Saw, R.; Finch, C.F.; Samra, D.; Baquie, P.; Cardoso, T.; Hope, D.; Orchard, J.W. Injuries in Australian Rules Football: An Overview of Injury Rates, Patterns, and Mechanisms Across All Levels of Play. Sports Health 2018, 10, 208–216. [Google Scholar] [CrossRef] [PubMed]
- AFL. Australian Football League 125th Annual Report 2021. 2021. Available online: https://resources.afl.com.au/afl/document/2022/03/10/76a16be1-6439-4020-af33-1cac86639f7e/2021-AFL-Annual-Report.pdf?_ga=2.37701280.1286951292.1649741969-125751827.1649741969 (accessed on 10 September 2022).
- AFL. 2012 AFL Injury Report. 2012. Available online: http://i.nextmedia.com.au/Assets/AFLInjuryReportFor2012.pdf (accessed on 10 September 2022).
- Orchard, J.W.; Driscoll, T.; Seward, H.; Orchard, J.J. Relationship between interchange usage and risk of hamstring injuries in the Australian Football League. J. Sci. Med. Sport 2012, 15, 201–206. [Google Scholar] [CrossRef] [PubMed]
- AFL. 2018 AFL Injury Report. 2018. Available online: https://s.afl.com.au/staticfile/AFL%20Tenant/2018-AFL-Injury-Report.pdf (accessed on 10 September 2022).
- Smith, N.A.; Franettovich Smith, M.M.; Bourne, M.N.; Barrett, R.S.; Hides, J.A. A prospective study of risk factors for hamstring injury in Australian football league players. J. Sports Sci. 2021, 39, 1395–1401. [Google Scholar] [CrossRef] [PubMed]
- Sammito, S.; Hadzic, V.; Karakolis, T.; Kelly, K.R.; Proctor, S.P.; Stepens, A.; White, G.; Zimmermann, W.O. Risk factors for musculoskeletal injuries in the military: A qualitative systematic review of the literature from the past two decades and a new prioritizing injury model. Mil. Med. Res. 2021, 8, 66. [Google Scholar] [CrossRef]
- Gabbe, B.J.; Bennell, K.L.; Finch, C.F.; Wajswelner, H.; Orchard, J.W. Predictors of hamstring injury at the elite level of Australian football. Scand. J. Med. Sci. Sports 2006, 16, 7–13. [Google Scholar] [CrossRef]
- Verrall, G.M.; Slavotinek, J.P.; Barnes, P.G.; Fon, G.T.; Spriggins, A.J. Clinical risk factors for hamstring muscle strain injury: A prospective study with correlation of injury by magnetic resonance imaging. Br. J. Sports Med. 2001, 35, 435–439. [Google Scholar] [CrossRef]
- Opar, D.A.; Ruddy, J.D.; Williams, M.D.; Maniar, N.; Hickey, J.T.; Bourne, M.N.; Pizzari, T.; Timmins, R.G. Screening Hamstring Injury Risk Factors Multiple Times in a Season Does Not Improve the Identification of Future Injury Risk. Med. Sci. Sports Exerc. 2022, 54, 321–329. [Google Scholar] [CrossRef]
- Opar, D.A.; Williams, M.D.; Timmins, R.G.; Hickey, J.; Duhig, S.J.; Shield, A.J. Eccentric hamstring strength and hamstring injury risk in Australian footballers. Med. Sci. Sports Exerc. 2015, 47, 857–865. [Google Scholar] [CrossRef]
- Opar, D.A.; Williams, M.D.; Timmins, R.G.; Hickey, J.; Duhig, S.J.; Shield, A.J. The effect of previous hamstring strain injuries on the change in eccentric hamstring strength during preseason training in elite Australian footballers. Am. J. Sports Med. 2015, 43, 377–384. [Google Scholar] [CrossRef]
- Bourne, M.N.; Schuermans, J.; Witvrouw, E.; Aagaard, P.; Shield, A.J. Neuromuscular Factors Related to Hamstring Muscle Function, Performance and Injury. In Prevention and Rehabilitation of Hamstring Injuries; Thorborg, K., Shield, A.J., Opar, D.A., Eds.; Springer Nature: Berlin/Heidelberg, Germany, 2020; pp. 117–144. [Google Scholar] [CrossRef]
- Picerno, P. The Hamstrings-Injury-Mechanism Debate: Are We Close to an Agreement? J. Sport Rehabil. 2017, 26, 120–121. [Google Scholar] [CrossRef]
- Liu, H.; Garrett, W.E.; Moorman, C.T.; Yu, B. Injury rate, mechanism, and risk factors of hamstring strain injuries in sports: A review of the literature. J. Sport Health Sci. 2012, 1, 92–101. [Google Scholar] [CrossRef]
- Bourne, M.N.; Duhig, S.J.; Timmins, R.G.; Williams, M.D.; Opar, D.A.; Al Najjar, A.; Kerr, G.K.; Shield, A.J. Impact of the Nordic hamstring and hip extension exercises on hamstring architecture and morphology: Implications for injury prevention. Br. J. Sports Med. 2017, 51, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Esculier, J.-F.; Maggs, K.; Maggs, E.; Dubois, B. A Contemporary Approach to Patellofemoral Pain in Runners. J. Athl. Train. 2020, 55, 1206–1214. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Social. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Swann, C.; Moran, A.; Piggott, D. Defining elite athletes: Issues in the study of expert performance in sport psychology. Psychol. Sport Exerc. 2015, 16, 3–14. [Google Scholar] [CrossRef]
- Duhig, S.; Shield, A.J.; Opar, D.; Gabbett, T.J.; Ferguson, C.; Williams, M. Effect of high-speed running on hamstring strain injury risk. Br. J. Sports Med. 2016, 50, 1536–1540. [Google Scholar] [CrossRef]
- Ruddy, J.D.; Pollard, C.W.; Timmins, R.G.; Williams, M.D.; Shield, A.J.; Opar, D.A. Running exposure is associated with the risk of hamstring strain injury in elite Australian footballers. Br. J. Sports Med. 2018, 52, 919–928. [Google Scholar] [CrossRef]
- Franettovich Smith, M.M.; Bonacci, J.; Mendis, M.D.; Christie, C.; Rotstein, A.; Hides, J.A. Gluteus medius activation during running is a risk factor for season hamstring injuries in elite footballers. J. Sci. Med. Sport 2017, 20, 159–163. [Google Scholar] [CrossRef]
- Smith, N.A.; Cameron, M.; Treleaven, J.; Hides, J.A. Lower limb joint position sense and prospective hamstring injury. Musculoskelet. Sci. Pract. 2021, 53, 102371. [Google Scholar] [CrossRef]
- Watsford, M.L.; Murphy, A.J.; McLachlan, K.A.; Bryant, A.L.; Cameron, M.L.; Crossley, K.M.; Makdissi, M. A prospective study of the relationship between lower body stiffness and hamstring injury in professional Australian rules footballers. Am. J. Sports Med. 2010, 38, 2058–2064. [Google Scholar] [CrossRef] [PubMed]
- Warren, P.; Gabbe, B.J.; Schneider-Kolsky, M.; Bennell, K.L. Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite Australian footballers. Br. J. Sports Med. 2010, 44, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Verrall, G.M.; Slavotinek, J.P.; Barnes, P.G.; Fon, G.T.; Esterman, A. Assessment of physical examination and magnetic resonance imaging findings of hamstring injury as predictors for recurrent injury. J. Orthop. Sports Phys. Ther. 2006, 36, 215–224. [Google Scholar] [CrossRef]
- Buckthorpe, M.; Wright, S.; Bruce-Low, S.; Nanni, G.; Sturdy, T.; Gross, A.S.; Bowen, L.; Styles, B.; Della Villa, S.; Davison, M.; et al. Recommendations for hamstring injury prevention in elite football: Translating research into practice. Br. J. Sports Med. 2019, 53, 449–456. [Google Scholar] [CrossRef]
- McBurnie, A.J.; Harper, D.J.; Jones, P.A.; Dos’Santos, T. Deceleration Training in Team Sports: Another Potential ‘Vaccine’ for Sports-Related Injury? Sports Med. 2022, 52, 1–12. [Google Scholar] [CrossRef]
- Gronwald, T.; Klein, C.; Hoenig, T.; Pietzonka, M.; Bloch, H.; Edouard, P.; Hollander, K. Hamstring injury patterns in professional male football (soccer): A systematic video analysis of 52 cases. Br. J. Sports Med. 2022, 56, 165–171. [Google Scholar] [CrossRef]
- Wollin, M.; Thorborg, K.; Drew, M.; Pizzari, T. A novel hamstring strain injury prevention system: Post-match strength testing for secondary prevention in football. Br. J. Sports Med. 2020, 54, 498–499. [Google Scholar] [CrossRef]
- Timmins, R.G.; Bourne, M.N.; Shield, A.J.; Williams, M.D.; Lorenzen, C.; Opar, D.A. Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): A prospective cohort study. Br. J. Sports Med. 2016, 50, 1524–1535. [Google Scholar] [CrossRef]
- van Dyk, N.; Bahr, R.; Burnett, A.F.; Whiteley, R.; Bakken, A.; Mosler, A.; Farooq, A.; Witvrouw, E. A comprehensive strength testing protocol offers no clinical value in predicting risk of hamstring injury: A prospective cohort study of 413 professional football players. Br. J. Sports Med. 2017, 51, 1695–1702. [Google Scholar] [CrossRef]
- Freckleton, G.; Pizzari, T. Risk factors for hamstring muscle strain injury in sport: A systematic review and meta-analysis. Br. J. Sports Med. 2013, 47, 351–358. [Google Scholar] [CrossRef]
- Young, W.B.; Newton, R.U.; Doyle, T.L.A.; Chapman, D.; Cormack, S.; Stewart, C.; Dawson, B. Physiological and anthropometric characteristics of starters and non-starters and playing positions in elite Australian Rules football: A case study. J. Sci. Med. Sport 2005, 8, 333–345. [Google Scholar] [CrossRef]
- Croisier, J.-L.; Ganteaume, S.; Binet, J.; Genty, M.; Ferret, J.-M. Strength Imbalances and Prevention of Hamstring Injury in Professional Soccer Players:A Prospective Study. Am. J. Sports Med. 2008, 36, 1469–1475. [Google Scholar] [CrossRef]
- Cheung, R.T.; Smith, A.W.; Wong del, P. H:q ratios and bilateral leg strength in college field and court sports players. J. Hum. Kinet. 2012, 33, 63–71. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; Bizzini, M.; Rampinini, E.; Cereda, F.; Maffiuletti, N.A. Reliability of isokinetic strength imbalance ratios measured using the Cybex NORM dynamometer. Clin. Physiol. Funct. Imaging 2008, 28, 113–119. [Google Scholar] [CrossRef]
- Gabbe, B.J.; Bennell, K.L.; Finch, C.F. Why are older Australian football players at greater risk of hamstring injury? J. Sci. Med. Sport 2006, 9, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Pollock, N.; Patel, A.; Chakraverty, J.; Suokas, A.; James, S.L.J.; Chakraverty, R. Time to return to full training is delayed and recurrence rate is higher in intratendinous (‘c’) acute hamstring injury in elite track and field athletes: Clinical application of the British Athletics Muscle Injury Classification. Br. J. Sports Med. 2016, 50, 305–310. [Google Scholar] [CrossRef]
- Macdonald, B.; McAleer, S.; Kelly, S.; Chakraverty, R.; Johnston, M.; Pollock, N. Hamstring rehabilitation in elite track and field athletes: Applying the British Athletics Muscle Injury Classification in clinical practice. Br. J. Sports Med. 2019, 53, 1464–1473. [Google Scholar] [CrossRef]
- Hägglund, M.; Waldén, M.; Ekstrand, J. Previous injury as a risk factor for injury in elite football: A prospective study over two consecutive seasons. Br. J. Sports Med. 2006, 40, 767–772. [Google Scholar] [CrossRef]
- Hägglund, M.; Waldén, M.; Ekstrand, J. Risk factors for lower extremity muscle injury in professional soccer: The UEFA Injury Study. Am. J. Sports Med. 2013, 41, 327–335. [Google Scholar] [CrossRef]
- Buckthorpe, M.; Gimpel, M.; Wright, S.; Sturdy, T.; Stride, M. Hamstring muscle injuries in elite football: Translating research into practice. Br. J. Sports Med. 2018, 52, 628–629. [Google Scholar] [CrossRef]
- Salavati, M.; Akhbari, B.; Mohammadi, F.; Mazaheri, M.; Khorrami, M. Knee injury and Osteoarthritis Outcome Score (KOOS); reliability and validity in competitive athletes after anterior cruciate ligament reconstruction. Osteoarthr. Cartil. 2011, 19, 406–410. [Google Scholar] [CrossRef] [PubMed]
- Thorborg, K.; Hölmich, P.; Christensen, R.; Petersen, J.; Roos, E.M. The Copenhagen Hip and Groin Outcome Score (HAGOS): Development and validation according to the COSMIN checklist. Br. J. Sports Med. 2011, 45, 478–491. [Google Scholar] [CrossRef]
- Appaneal, R.N.; Perna, F.M. Encyclopedia of Sport and Exercise Psychology; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2014. [Google Scholar] [CrossRef]
- Ivarsson, A.; Johnson, U.; Andersen, M.B.; Tranaeus, U.; Stenling, A.; Lindwall, M. Psychosocial Factors and Sport Injuries: Meta-analyses for Prediction and Prevention. Sports Med. 2017, 47, 353–365. [Google Scholar] [CrossRef]
- Aagaard, P.; Simonsen, E.B.; Trolle, M.; Bangsbo, J.; Klausen, K. Isokinetic hamstring/quadriceps strength ratio: Influence from joint angular velocity, gravity correction and contraction mode. Acta Physiol. Scand. 1995, 154, 421–427. [Google Scholar] [CrossRef]
- Kellis, E.; Sahinis, C.; Baltzopoulos, V. Is hamstrings-to-quadriceps torque ratio useful for predicting anterior cruciate ligament and hamstring injuries? A systematic and critical review. J. Sport Health Sci. 2023, 12, 343–358. [Google Scholar] [CrossRef]
- Silvers-Granelli, H.J.; Cohen, M.; Espregueira-Mendes, J.; Mandelbaum, B. Hamstring muscle injury in the athlete: State of the art. J. ISAKOS 2021, 6, 170–181. [Google Scholar] [CrossRef]
- Tsilimigkras, T.; Kakkos, I.; Matsopoulos, G.K.; Bogdanis, G.C. Enhancing Sports Injury Risk Assessment in Soccer Through Machine Learning and Training Load Analysis. J. Sports Sci. Med. 2024, 23, 537–547. [Google Scholar] [CrossRef]
- Nassis, G.P.; Verhagen, E.; Brito, J.; Figueiredo, P.; Krustrup, P. A review of machine learning applications in soccer with an emphasis on injury risk. Biol. Sport 2023, 40, 233–239. [Google Scholar] [CrossRef]
- Lahti, J.; Mendiguchia, J.; Ahtiainen, J.; Anula, L.; Kononen, T.; Kujala, M.; Matinlauri, A.; Peltonen, V.; Thibault, M.; Toivonen, R.-M.; et al. Multifactorial individualised programme for hamstring muscle injury risk reduction in professional football: Protocol for a prospective cohort study. BMJ Open Sport Exerc. Med. 2020, 6, e000758. [Google Scholar] [CrossRef]
- Majumdar, A.; Bakirov, R.; Hodges, D.; Scott, S.; Rees, T. Machine Learning for Understanding and Predicting Injuries in Football. Sports Med.-Open 2022, 8, 73. [Google Scholar] [CrossRef]
- Ayala, F.; López-Valenciano, A.; Gámez Martín, J.A.; De Ste Croix, M.; Vera-Garcia, F.J.; García-Vaquero, M.d.P.; Ruiz-Pérez, I.; Myer, G.D. A Preventive Model for Hamstring Injuries in Professional Soccer: Learning Algorithms. Int. J. Sports Med. 2019, 40, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Leckey, C.; van Dyk, N.; Doherty, C.; Lawlor, A.; Delahunt, E. Machine learning approaches to injury risk prediction in sport: A scoping review with evidence synthesis. Br. J. Sports Med. 2025, 59, 491–500. [Google Scholar] [CrossRef]
| PICOS Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| P (Population) | Healthy adult male athletes playing Australian Rules Football at a professional, semi-professional, elite competitive level 1 and were 18 yrs or older | Female-only participants, or the male-only data could not be extracted; based on participants competing at non-elite or non-professional level; incorporated participants who were non-Australian Rules Football athletes |
| I (Intervention) | Studies analyzing screening tools or assessments for HSI | Training studies outcomes only with no use of screening tools or assessments |
| C (Comparators) | Optional | Examining the effect of HSI rehabilitation or prevention programs, or reviewing return to play (RTP) criteria post-HSI |
| O (Outcomes) | New data on musculoskeletal morphology, functional performance, and biopsychological risk factors in HSIs | Review papers, conference proceedings, or case studies |
| S (Study designs) | No restrictions on the types of study designs eligible for inclusion | N/A |
| Risk Factor | Reference | Predictors of Injury Results, p-Value, Odds Ratio (OR), Confidence Intervals (CI) |
|---|---|---|
| History of HSI | [6] |
|
| [26] |
| |
| Age | [6] |
|
| [25] |
| |
| History of lower limb injury (groin, calf and ACL) | [6] |
|
| [4] |
| |
| Size of a hamstring injury on MRI | [27] |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chapman, D.W.; Humphreys, S.; Spencer, S.; Tai, N.; Øyen, D.; Netto, K.; Waller, R. A Scoping Review for Hamstring Injury Risk Monitoring in Australian Rules Football. Encyclopedia 2025, 5, 72. https://doi.org/10.3390/encyclopedia5020072
Chapman DW, Humphreys S, Spencer S, Tai N, Øyen D, Netto K, Waller R. A Scoping Review for Hamstring Injury Risk Monitoring in Australian Rules Football. Encyclopedia. 2025; 5(2):72. https://doi.org/10.3390/encyclopedia5020072
Chicago/Turabian StyleChapman, Dale Wilson, Sorcha Humphreys, Shannon Spencer, Nathan Tai, Dag Øyen, Kevin Netto, and Robert Waller. 2025. "A Scoping Review for Hamstring Injury Risk Monitoring in Australian Rules Football" Encyclopedia 5, no. 2: 72. https://doi.org/10.3390/encyclopedia5020072
APA StyleChapman, D. W., Humphreys, S., Spencer, S., Tai, N., Øyen, D., Netto, K., & Waller, R. (2025). A Scoping Review for Hamstring Injury Risk Monitoring in Australian Rules Football. Encyclopedia, 5(2), 72. https://doi.org/10.3390/encyclopedia5020072








