1. Introduction
A pneumonic illness of unknown origin was first identified in Wuhan, Hubei province, China, in December 2019. The World Health Organization (WHO) recognized the disease as being caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). The acronym COVID-19 (coronavirus disease-2019) was then coined to term the illness. Since its first appearance, it has spread all over the world, thus representing a true global public health challenge. The WHO declared that the disease was a
“public health emergency of international concern” on 20 January 2020. Following that, it was declared as a “
pandemic” on 11 March 2020. As of 22 January 2022, the pandemic has caused more than 346 million cases and 5.58 million deaths, undoubtedly making it one of the worst infections in human history [
1]. However, the epidemiological study of the pandemic is still ongoing, and, thus, it is affected by the need to steadily update data, which are often incomplete, owing to the emergency-induced chaos [
2].
Of note, the COVID-19 pandemic has been found to have a strong link with socio-economic phenomena.
2. Syndemic Definition
Merrill Singer, an American medical anthropologist, coined the neologism “
syndemic” by merging the two words synergy and epidemic in the mid-1990s [
2,
3]. “
Syndemic” defines a theory according to which epidemics arise from the complex interplay between the spread of a disease and social/environmental/economic factors, which, in turn, negatively impact the disease itself. To date, the concept of “
syndemic” has generally been applied to chronic medical conditions [
2,
3]. Conversely, disease co-occurrence, with or without any interaction, is known as “
comorbidity”.
The terms “
comorbidity” and “
syndemic” are different, since the first term tends to only focus on nosography, whereas “
syndemic” mostly refers to the concomitant socio-economic factors. However, there is some overlap between the two terms. Two or more diseases can be comorbid with or without any social and/or economic influence. Conversely, the term “
syndemic” is characterized by the influence of the accompanying economic and social features (such as poverty, exploitation, and oppressive social relationships), which, taken together, increase a person’s susceptibility to an illness [
4].
The syndemic approach to diseases is now gaining increasing recognition in the public domain and global health research settings.
Epidemiologists and medical anthropologists study health disparity, which is linked to poverty, stress, and violence. Racial and ethnic inequalities in access to healthcare are becoming increasingly more evident globally during the current COVID-19 pandemic, and they are having markedly negative long-lasting effects on health [
5].
The term “
syndemic” was used for the first time to describe community-level disparity patterns in substance abuse, violence, the occurrence of HIV/AIDS, and the occurrence of other conditions, and to help understand their relationships, especially as they are related to modifiable behaviors, in the USA [
2,
3]. Rather than being separate entities, substance abuse, violence, and AIDS—referred to as SAVA to stress their mutual relationship—represent a single syndetic (i.e., a closely interrelated complex of health and social crises) that continues to take a significant toll on the lives and well-being of the urban poor [
6].
Specifically, a “syndemic” approach examines why certain diseases occur in clusters. This approach also studies the pathways through which a biological state or disease interacts with socio-economic conditions in individuals/groups of people, thereby exacerbating the overall disease burden. A degraded social environment, the conditions of community inequality and injustice, and disease are considered the worst features contributing to a patient’s increased vulnerability.
Although often used to explain conditions such as sepsis, the term
syndemic is not limited to infectious diseases. Non-communicable illnesses, such as cardiovascular disorders, diabetes, hypertension, chronic obstructive pulmonary disease, and cancer, also occur in the same settings as infectious diseases, that is, in low-income urban populations, and they affect the health of the individual and strains the healthcare system [
7].
An example of this is type 1 diabetes in children. The immune basis of type 1 diabetes has been well defined. Since the autoimmune reaction and beta-cell loss start long before the diagnosis of type 1 diabetes, it is not surprising that the incidence of type 1 diabetes rose in concert with the peak occurrence of COVID-19, as well as with the pandemic containment measures in the 3 months following the appearance of COVID-19. Thus, it appears that type 1 diabetes is not caused by SARS-CoV-2 infection but, rather, is the result of environmental changes associated with the pandemic itself or pandemic containment measures [
8].
With the aim of overcoming the lack of any national, state, and local public health data on the unbalanced economic and social impact of COVID-19, USA counties and zip codes in Illinois as well as New York City were matched with COVID-19 deaths, established COVID-19 cases and positive COVID-19 swabs. The given period was from 23 January 2020 to 5 May 2020. The use of zip codes allowed us to identify areas with high rates of poverty, crowding, and a high black population, as well as the Index of Concentration at the Extremes. The source of the data was the dataset USA Facts. By 5 May 2020, the COVID-19 death rates were 143.2/100,000/year vs. 83.3/100,000/year in low versus high poverty counties (≥20% vs. <5% of persons below poverty); 124.4/100,000/year vs. 48.2/100,000/year in counties in the highest versus lowest quintile, relative to household crowding; and 127.7/100,000/year vs. 25.9/100,000/year, relative to counties in the highest versus lowest quintile for the percentage of black population. As such, severe social inequities in the USA were found to relate to COVID-19 outcomes. This report supports the need for a change in policy and resource allocation [
9].
Another example of
syndemic inequality in access to care is related to COVID-19 therapy. Intravenous or subcutaneous anti–SARS-CoV-2 monoclonal antibodies are usually provided to non- hospitalized subjects suffering from mild-to-moderate positivity of SARS-CoV-2 infection and to those at increased risk of progressing to severe disease and admission to hospital. According to the Centers for Disease Control and Prevention, some racial and ethnic communities—namely Black, Hispanic or Latino, and American-Indian or Alaska-native subjects—are at an increased risk of requiring admission to hospital or passing away due to COVID-19 in comparison to Caucasians. The same groups are also those who are less often offered monoclonal antibodies [
10].
3. Syndemic Pandemic
The harmful combination of the COVID-19 pandemic with widely diffused non-communicable diseases has put a strain on already existing social and economic discrepancies. In other words, access to the healthcare system for the treatment of non-communicable diseases, which was already significantly limited for lower classes, has become even more difficult in the COVID-19 era.
We believe that public health officials are taking the wrong approach in managing this outbreak. Unfortunately, public health officials have so far considered COVID-19 simply as an infectious disease. Richard Horton, Editor-in-chief of The Lancet, elegantly stressed this feature of the pandemic in a recent editorial. The link between COVID-19 and non-communicable illnesses with an underlying history of social and economic inequality brings out the negative consequences of each distinct illness [
11]. The
syndemic model is an emerging approach to healthcare in clinical practice. We should start thinking beyond the traditional historical concept of diseases as separate entities that are apart from other illnesses and not subject to social differences. Dr Horton concluded that “COVID-19 is a
syndemic, not a pandemic” [
11].
3.1. Theoretical Background
Applying the concept of syndemic to COVID-19 has the potential to help politicians and healthcare program implementers in their attempts to improve the health of the general population in view of facing other similar crises in the future.
Considering social factors, such as social disparity, differentiates syndemic processes from the classic biomedical notion of comorbidity and also differentiates syndemics among human beings from synergistic disease interplay among animals. Syndemic theory relies on recognizing the pivotal role of biosocial interrelationships. The latter is of particularly relevance to humans and it represents a new approach that has not been recognized in the past.
Concerning the word syndemic, which can also be spelled as syn-demic, the first of the two words comes from the Greek word σύν, meaning “together”. It is used when two or more agents act together to generate a greater effect than each of them acting alone. The second word, e.g., demic, is a suffix which derives from another Greek word, δῆμος, meaning “people”. It has been previously used in three cornerstone concepts in public health: epidemic, a term that is used to describe greater than expected jumps in the frequency of an illness in a given population; pandemic, an epidemic spreading across multiple populations or even worldwide, such as COVID-19; and endemic, a disease that is well established in a population and remains year after year.
The syndemic perspective begs the questions of what predisposing factors have given rise to the spread of COVID-19 (for instance, overcrowded built environments, pollution, and climate change), what inequalities has COVID-19 exacerbated among vulnerable populations, and what strategies could be employed to detect and reduce such inequalities. To reach these aims, a scientific, rather than empirical, approach is preferred [
12].
3.2. Lockdown
The first line approach suggested by governments and epidemiologists worldwide to hamper viral transmission and reduce contagion was based on non-pharmaceutical interventions, such as intensified hand hygiene, social distancing, self-isolation, quarantine, and lockdown of whole countries. This approach is quite similar to that used for plague containment, the old “quarantine” [
13]. However, we now know that COVID-19 affects “fragile” people with non-communicable diseases the most. The state-imposed restrictions have various degrees of strictness, but all share a noteworthy increase in social isolation and discrimination. There is no doubt that overcrowded nursing homes with a lack of social distancing and isolation have represented the most dramatic outbreak during the COVID-19 pandemic and that elderly poor people were forced into this environment, thus representing an example of inequality [
14].
The first consequences of the COVID-19 emergency restrictions are likely to have unequally triggered multiple health impacts. They will range from unbalanced experiences of lockdown (loss of jobs and income, living in overcrowded spaces, being confined in buildings with no access to leisure time activities) to how the restrictions themselves worsening the social features of health (e.g., very limited access to healthcare systems for patients with diseases other than COVID-19, since all hospitals are overcrowded with COVID-19 patients), and then to disparities in health consequences due to the lockdown (reduced sports activity, increased mental health depression and gender-based violence).
The world economy has been dramatically affected by COVID-19 and its complications. The aftermaths of economic disasters appear to be similarly unequally distributed, thus making heath disparities worse [
15]. For example, in a study assessing the impact of COVID-19-related aftermaths on household income and food security in two African countries (Kenya and Uganda), a significant income drop was detected in approx. 70% of the sample. Food availability decreased by 38% and 44% in Kenya and Uganda, respectively, and dietary also quality worsened. In this respect, in both countries, the regular consumption of fruits decreased by around 30% during the pandemic compared to previously. The income-poor households and people depending on labor income without any savings were the most vulnerable. On the contrary, farmers were less likely to struggle with the same troubles. The findings suggest that in the future, the government should focus their efforts on building strong financial institutions to support the recovery of businesses in the medium term, ensuring the resilience of food supply chains [
16]. The Covid-19 pandemic is challenging, not only for health sectors but also for public administration systems. As soon as the current unprecedented circumstances normalize, administrators and politicians should learn from the current crisis by gathering and analyzing data, building international networks, and preparing themselves to better cope with the next crisis [
17].
Compliance with the COVID-19-related restrictive measures introduced by local governments to prevent contagion varies significantly depending on many factors, including different cultural features. In particular, individualism, which gives special value to personal freedom, makes government action more difficult, whilst collectivism, emphasizing the wellbeing of people, makes government measures easier. This is particularly evident when making a comparison between the US and China [
18], but also within the US itself. In fact, analyzing a database of more than 3000 counties of the 50 American states, the percentage of those wearing masks was found to be higher in more collectivistic US states [
19]. On the other hand, culture, identified as the existence of shared beliefs and values by members of the same nation or state, has a significant impact on the quality of the government itself. The impact is stronger than that exerted by other factors such as institutions and economic development [
20].
In research carried out in the US, partisanship, defined as party identification, intended 2020 Presidential vote, and self-placed ideological positioning, proved to play a pivotal role in shaping individual responses to restrictions since the early beginning of the COVID-19 pandemic [
21].
Additionally, social media has an influence on people’s response to COVID-19-imposed restricted mobility. In fact, the higher the number of Twitter messages containing words such as “stay home”, “stay safe”, “wear mask”, “wash hands”, and “social distancing”, the more mobility was seen to decrease [
22].
4. Vaccine Inequality
As stated above, during the early phases of COVID-19, the world community was totally unprepared to face the outbreak and the above-stated non-pharmaceutical interventions were the only possible way to reduce COVID-19 mortality and morbidity [
23]. Fortunately, a number of vaccines have been developed, approved by governments and distributed throughout the world. Along with non-pharmaceutical interventions (such as masking and social distancing), there has been a reduction in the number of infections and deaths. On the other hand, COVID-19 vaccines represent a feasible solution and strategy for significantly limiting the spread of the disease, above and beyond what can be achieved with masking and social distancing in the long-term [
24].
Nonetheless, despite the excellent efficacy and acceptable risk profiles of the vaccines, mass immunization campaigns are successful only when the vaccine rates are high, which results in herd immunity. Mass vaccination can control the viral transmission dynamics as well as provide fragile individuals with immune protection. Unfortunately, a significant percentage of individuals, despite being willing to receive a vaccination against COVID-19, are unable to do so because they are immune-deficient or immune-suppressed; their conditions do not allow them to achieve immunity levels which are sufficiently strong [
25].
Apart from these clinical reasons, further heterogeneous circumstances, such as a lack of trust for scientific evidence and vaccination, beliefs concerning the supposed aggressiveness of COVID-19 and/or the effectiveness and adverse events of vaccines, and objective and perceived obstacles to immunization, can have negative consequences on the progress of mass vaccination campaigns, causing harmful health risks. In fact, as per the WHO, vaccine acceptance represents one of the more important challenges to public health [
26]. Vaccine hesitancy is a multifaceted phenomenon which comes from a combination of different factors, ranging from socio-economic and educational variables to behavioral components [
27,
28]. For the sake of scientific honesty, the suspicion surrounding attempts to minimize some side effects to the vaccines did not help promote trust in vaccination [
29,
30,
31].
Specifically, the COVID-19 pandemic has affected individuals in more than 220 countries and regions. It has by far adversely influenced healthcare sectors, the supply chains of production of anti-viral medications and vaccines and their delivery, logistics, and distribution. In the meantime, many wealthy nations started promoting immunization campaigns, immunizing more than 50% of their entire population; some countries have even given third and fourth doses (a booster and a second booster, respectively) of COVID-19 vaccines. In contrast, the vast majority of developing countries, particularly African continent, are still having difficulty obtaining enough vaccines to start their own vaccination campaigns [
32].
Low-income countries form collaborative networks to co-finance vaccine acquisition, such as the “COVID-19 Vaccines Global Access” (COVAX), the World Bank and the African Union’s COVID-19 “Africa Vaccine Acquisition Task Team” (AVATT) platforms, with the aim of supporting balanced and sustainable access to COVID-19 vaccines [
33,
34].
It is interesting to cite the paper by Wagner and Coll., who studied the number of infections and potential risk of coronavirus variants emersion in two hypothetical regions, e.g., one with high access and the other with low access to vaccines. They found that for the first, sharing vaccines with the second would be much better with the aim of reducing COVID-19 burdens in countries with less access, lowering the number of case imports and minimizing the harmful risk of the occurrence of highly contagious viral mutations [
35].
To objectively assess inequities in vaccine allocation, distribution, and uptake in low- and middle-income countries, a search was carried out, employing machine-learning [
36]. This study has provided important information for those people working in global and public health systems, decision and policymakers, and all the important persons involved in vaccine roll-out. The most important aspects of the vaccine roll-out process have been identified, and these include: focusing on giving vaccines to children (children are a potential reservoir of coronavirus and may suffer from MIS-C/PIMS themselves) rather than expediting vaccination of the entire population [
37]; increasing confidence in the COVID-19 vaccine with the use of famous figures as role-models and all the possible available promotional tools: training and recruiting more people to increase the vaccination process; and increasing government budgets for buying and distributing the vaccines [
36]. Setting up databases such as the ‘Response2covid19’, a living dataset of governments’ responses to COVID-19 involving more than 200 countries and which is updated every month can help in generating robust data to support public health and economic decision making [
38].
5. Anthropological Approach
The syndemic perspective implies that human beings should be considered as the cornerstone of any pathological process (“anthropological approach”). It provides scientists with a biosocial conception of health. Therefore, a more philosophical perspective is necessary if we wish to stay free from COVID-19. Dealing with the SARS-CoV-2 infection means paying close attention to non-communicable diseases more than in the recent past. These diseases are not limited to wealthy countries. Conversely, they are diffused around the world, particularly among the poorest in the world.
By providing a framework of the interplay between diseases and socioeconomic features, an understanding of the
syndemic theory can enhance our understanding of the pandemic we are living in, thus leading to major progress that cannot be reached when focusing on each disease as a separate entity [
2].
Non-communicable diseases represent about a third of the total disease burden. The WHO has suggested several affordable, cost-effective interventions, which could prevent almost 5 million deaths from occurring, mostly among the poorest in the world, over the next decade. This is in addition to preventing deaths from COVID-19 [
39].
Approaching COVID-19 as a
syndemic, especially with the new variants threating nations, implies a comprehensive vision that includes educating people, reducing unemployment, providing affordable housing and food, and saving the countryside from pollution and property speculation. Considering COVID-19 simply as a pandemic rules out broader much needed approaches. Drugs or vaccines by themselves will not solve the future economic crisis that is arising. Increasing awareness of COVID-19 as a
syndemic and the implementation of concrete measures to limit disparities are now needed to decrease the onslaught and spread of the epidemic and the burden of health disparities globally [
11]. As there are strong biological and environmental reasons to expect more serious epidemics than COVID-19, a
syndemic approach can help researchers, clinicians, and other healthcare providers to identify the presence of socio-economic factors interacting with the disease and adversely affecting one another [
40].
7. Monoclonal Antibodies and Equity
Many of us have already had the unpleasant experience of witnessing inequalities and that the most infected patients, those struggling for hospitalization, and having the worst outcomes are mostly of non-white race or belong to specific ethnic groups. This sad observation highlights the need to overcome these boundaries and to think about how we can provide people with access to health care facilities in an equal way. At the beginning of the outbreak, research helped scientists to identify some risk factors of those suffering from a more severe form of the coronavirus infection, namely the elderly, male gender, people with pre-existing lung disease, overweight/obesity, and diabetes [
43]. Since then, other risk factors, even more harmful, have been identified, including being of non-White race or coming from other ethnic groups (including Black, Asian, Hispanic, American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, and multiple other races). This is particularly evident in access to and use of neutralizing monoclonal antibody therapy, as previously outlined. The latter are designed to mimic the body’s natural immune response. Their use has been authorized on the basis of the emergency situation. When administered in the early phase of infection, monoclonal antibodies have proved to be effective in preventing COVID-19 from progressing to a severe form requiring hospitalization [
44]. Specifically, the provision of monoclonal antibodies was significantly less common (4% of the population or less) in all non-White communities compared with White communities.
Hispanic patients received monoclonal antibodies 58% less often than non-Hispanic patients. Black patients, Asians, or individuals of other descent received monoclonal antibodies 22%, 48%, and 47% less often, respectively, than White patients (November 2020–August 2021) [
45].
8. Other Supporting Evidence
The US Centers for Disease Control and Prevention have been continuing to collect data concerning COVID-19 infected, hospitalized, and deceased patients. However, data about race and ethnicity are missing. Notwithstanding this limitation, the gathered data show that in comparison with White Americans, Native Americans and Alaska Natives are one and a half times more likely to suffer from COVID-19. Furthermore, rates of hospitalized and deceased patients are also much higher in these groups. Again, only about 10% of the American Black population have been vaccinated at least once against coronavirus, although they account for 12–13% of the whole US population. A more proactive attitude is needed to address these major issues in advance [
46].
In a recently released paper [
47], social determinants of health, which have been previously mentioned as important factors linked with health inequities, have been studied regarding their association with COVID-19 death rates among communities of different descent and rural, suburban, and urban areas during the first year of the pandemic (22 January 2022–28 February 2022) in the USA.
All the American states and counties, as well as the District of Columbia, were included. Areas with a high presence of a single race or ethnicity and a high COVID-19 death rate were named “concentrated longitudinal-impact counties”. The three most represented racial and ethnic communities were observed to be: Black or African American, Hispanic or Latin, and non-Hispanic White populations.
Social determinants of health were identified, namely low income, lack of health insurance, lack of family physician, preventable hospital admissions, housing crisis, and limited access to internet. Their possible association with COVID-19 fatality (deaths per 100,000 population) was tested by using a complex statistical analysis. Again, four indexes were used to measure multiple dimensions of social determinants of health: socio-economic advantage, limited mobility, urban core opportunity, and mixed immigrant cohesion and accessibility.
More than three thousand counties were enrolled in the search and about 500 were concentrated in the longitudinal-impact counties. Among the counties, 11.0% of the population was Black or African American, 6.3% was Hispanic or Latin, and in 1.1% was non-Hispanic White. Approximately half a million COVID-19-related deaths were registered. Concentrated longitudinal impact counties with a prevalent Black or African American community were in urban, suburban, and rural areas and faced a great number of disadvantages such as low income (85.6%) and preventable hospitalization (81.0%). Concentrated longitudinal-impact counties with a prevalent Hispanic or Latin community were located in urban areas (57.6%), and in about two thirds of these counties most of the people did not have health insurance. Concentrated longitudinal-impact counties with a prevalent non-Hispanic White population were in rural areas (69.7%) the most. These people were old (78.8%) and had limited access to quality health care (72.7%). In urban areas, the mixed immigrant cohesion and accessibility index proved to be inversely linked with the COVID-19 deaths rate, thus showing the association between the latter and the presence of immigrant communities, whose social model was a traditional family-oriented society with accessibility stressors and living in overcrowded buildings. Higher COVID-19 mortality rates were associated with preventable hospitalization in rural areas and higher socioeconomic status vulnerability in suburban areas. Across all communities, limited internet access was correlated with a higher number of deaths, mostly in urban areas.
On balance, the research showed a dramatic association between different social determinants of health measures and COVID-19 fatality rate, with some fluctuations across different racial and ethnic communities and geographical areas [
47].
Again, in another recent study, neighborhood conditions measured before the COVID-19 pandemic proved to have strong predictive power for subsequent incidence, with mobility-based disadvantages playing a pivotal role, even greater than residents’ socioeconomic features [
48].
However, it does not take a lot of research to see a connection between race and poor healthcare before and during the pandemic. This is exemplified by the case of Dr. Susan Moore, an African American physician from Indiana, a state in the United States, who was hospitalized for COVID-19. A physician herself, she immediately felt that her hospital and treatment were impacted by her race. She published her claims on Facebook Live and her story quickly gripped the African American community. This community was already experiencing a huge disparity in terms of infection rates versus the rest of the American population. Unfortunately, Dr. Moore died a few weeks after her initial complaint about denial of care. This has been mentioned in the book
Heart Disease: It Is All in Your Head [
49].
An example of ethnic inequalities detected during the first wave of COVID-19, which is also the phase of the disease with the largest number of examined data, is reported in
Table 1 [
50].
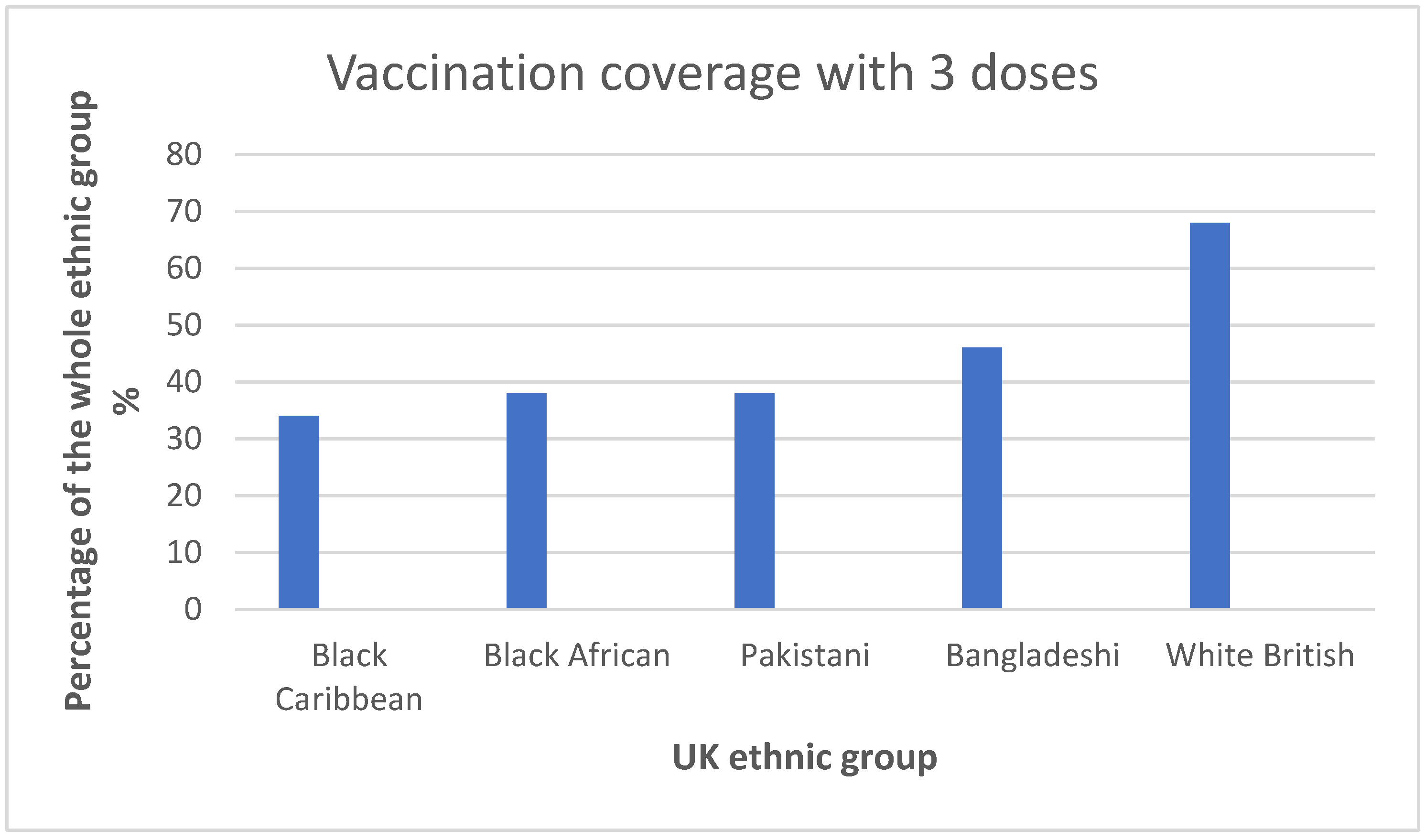
Some progress has been noted. Since its introduction in December 2020, the UK vaccination program has helped to decrease deaths from COVID-19 in the majority of ethnic minority groups. This is important, since the risk of death from COVID-19 is more than 90% lower for individuals who have received a third vaccine dose than for unvaccinated subjects. Nevertheless, vaccine roll-out remains the lowest in ethnic minority groups with the highest risk of COVID-19 death in all three pandemic waves [
51]. See
Figure 1.
There are many stories about inequities in the distribution of COVID-19 vaccines. According to a report by the Centers for Disease Control and Prevention in February 2022, “of 42 million people receiving at least the first vaccine dose, only 6.3% were African Americans” [
52].
Emerging statistics have proved without any doubt that COVID-19 disproportionately affects African Americans the most. The effects of COVID-19 on this specific population are inextricably related with four areas of systemic oppression and weakness, which are further exacerbated by COVID-19 itself: (1) healthcare inequality; (2) segregation, overall health, and food insecurity; (3) underrepresentation in government and the medical profession; and (4) inequalities in participatory democracy and public engagement. To overcome this no longer acceptable lack of equity, specific planned interventions are needed; for example, the development of a national, standardized database to monitor the demographic backgrounds of people suffering from COVID-19 with the aim of helping the American government to equitably and efficiently distribute the available human, economic, and medical resources; creating a partnership with nonprofit organizations, those run by African Americans and/or serving mostly African American people included; and developing specific strategies to safeguard the ability of African Americans to vote. This includes, but it is not limited to, expanding opportunities for them to register and vote remotely, as well as adopting and extending paid time off for voting for those involved in low-skill professions; addressing digital inequality to allow African Americans to gain access to potentially life-saving information, which is needed to mitigate the spread of COVID-19 [
53].
9. Mental Health Issues as a Part of the Syndemic
The COVID-19 syndemic is accompanied and exacerbated by mental health issues in patients, family members, and healthcare workers themselves [
54]. These mental health issues include anxiety, depression, and suicide. Mental health problems may arise from direct infection and inflammation of the brain from COVID-19 and/or concomitant vasculitis and thrombosis of blood vessels in the central nervous system. Psychological problems can also result from fear of the disease, proximity to death and dying, confinement in small spaces, and isolation. People who suffer from a mental health disease seem to have worse outcomes after COVID-19 infection compared to non-affected populations. There is a need for more studies in this area and for clinical trials to lessen and prevent the impact of these conditions, especially in the setting of long COVID-19 infection and in children [
54]. Nonetheless, there is no doubt that the tighter the COVID-19-related restrictions, the poorer the mental health. The likelihood of mental issues related to the situation of emergency, such as anxiety, depression, post-traumatic stress disorder, and sleep disorders, is significantly increased in healthcare workers, mostly frontline workers, migrant workers, and workers in contact with the public. On the other hand, the risk of losing their job, long periods of quarantine, and uncertainty concerning the future make psychological conditions worse, especially in the youth and in people with a higher level of education [
55].
10. Conclusions
The current COVID-19 syndemic/pandemic has highlighted chronic disparity in healthcare systems. Historically the highest rates of infection and mortality have been among the poorest and socially disadvantaged people around the world. COVID-19 morbidity and mortality are no exception. COVID-19 has revealed already existing social/economic/political discriminations in access to healthcare, vaccine administration, and monoclonal antibodies therapies, particularly in individuals affected by non-communicable diseases such as cancer and cardiovascular disease. COVID-19 has already dramatically reduced life expectancy in this subset of subjects [
56].
The COVID-19 pandemic has made previous inequities clearer than ever. Three population groups, based on their historical inequities, can be identified: “The last” low- and middle-income countries whose healthcare systems run the risk of collapsing under the pressures of the pandemic; “The lost” refugees and migrants who have been left in even more precarious position than before the pandemic; and “The least” minority populations, who are further prone to new detrimental socioeconomic consequences as a result of COVID-19 exacerbating the pattern of inequalities [
57]
In addition, culture is crucial since it shapes how people react to crises such as the current COVID-19 pandemic. Understanding cultural differences not only provides a better understanding of the current pandemic, but also helps in preparing for future crises [
19].
Without a strategic plan and a new anthropological
syndemic approach to future pandemics, more and more people worldwide will unnecessarily suffer, health inequities will widen, and the world economies will slow down [
58]. As a take home message learned from this global crisis, we should try our best to make it easier for everyone to access vaccines and other officially accepted therapies, and health in general. The distribution of limited and, at the same time, life-saving resources, such as vaccines, intensive care beds, and ventilators, should be global, equal, and fair. Any derogation from that is no longer acceptable in terms of ethics [
59].