Making the Case for Standardized Outcome Measures in Exercise and Physical Activity Research in Chronic Kidney Disease
Abstract
1. Introduction
2. Benefits of Exercise and Physical Activity in CKD
3. Diverse Heterogeneity in the Outcomes Used across Exercise and Physical Activity Research in CKD
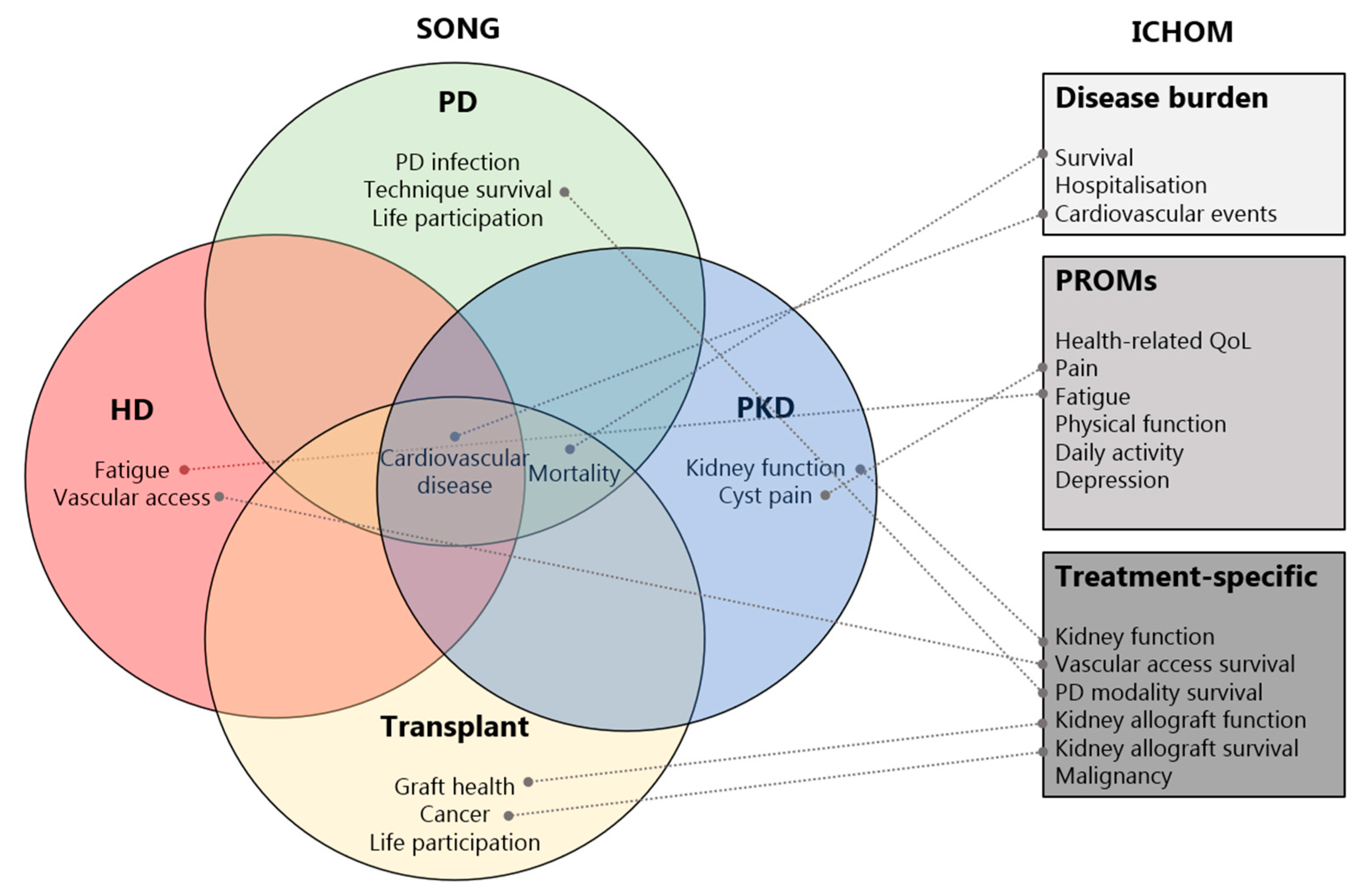
4. Core Outcome Sets in Nephrology
5. Core Outcome Sets in Exercise and Physical Activity Research
6. The Case for Standardized Outcomes in Exercise and Physical Activity Research in CKD
7. What Can We Do Next?
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Webster, A.C.; Nagler, E.V.; Morton, R.L.; Masson, P. Chronic kidney disease. Lancet 2017, 389, 1238–1252. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P. Epidemiology of chronic kidney disease: An update 2022. Kidney Int. Suppl. 2022, 12, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.; Weir, M.R. Defining, Treating, and Understanding Chronic Kidney Disease—A Complex Disorder. J. Clin. Hypertens. 2015, 17, 514–527. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Jafar, T.H.; Nitsch, D.; Neuen, B.L.; Perkovic, V. Chronic kidney disease. Lancet 2021, 398, 786–802. [Google Scholar] [CrossRef]
- Kelly, J.T.; Su, G.; Zhang, L.; Qin, X.; Marshall, S.; González-Ortiz, A.; Clase, C.M.; Campbell, K.L.; Xu, H.; Carrero, J.-J. Modifiable Lifestyle Factors for Primary Prevention of CKD: A Systematic Review and Meta-Analysis. J. Am. Soc. Nephrol. 2021, 32, 239–253. [Google Scholar] [CrossRef]
- Zelle, D.M.; Klaassen, G.; van Adrichem, E.; Bakker, S.J.; Corpeleijn, E.; Navis, G. Physical inactivity: A risk factor and target for intervention in renal care. Nat. Rev. Nephrol. 2017, 13, 152–168. [Google Scholar] [CrossRef]
- Wilkinson, T.J.; McAdams-DeMarco, M.; Bennett, P.N.; Wilund, K. Advances in exercise therapy in predialysis chronic kidney disease, hemodialysis, peritoneal dialysis, and kidney transplantation. Curr. Opin. Nephrol. Hypertens. 2020, 29, 471–479. [Google Scholar] [CrossRef]
- Wilkinson, T.J.; Clarke, A.L.; Nixon, D.G.D.; Hull, K.L.; Song, Y.; Burton, J.; Yates, T.; Smith, A.C. Prevalence and correlates of physical activity across kidney disease stages: An observational multicentre study. Nephrol. Dial. Transplant. 2019, 36, 641–649. [Google Scholar] [CrossRef]
- Zelle, D.M.; Kok, T.; Dontje, M.L.; Danchell, E.I.; Navis, G.; van Son, W.J.; Bakker, S.J.; Corpeleijn, E. The role of diet and physical activity in post-transplant weight gain after renal transplantation. Clin. Transplant. 2013, 27, E484–E490. [Google Scholar] [CrossRef]
- Dontje, M.L.; De Greef, M.H.G.; Krijnen, W.P.; Corpeleijn, E.; Kok, T.; Bakker, S.J.L.; Stolk, R.; Van Der Schans, C.P. Longitudinal measurement of physical activity following kidney transplantation. Clin. Transplant. 2014, 28, 394–402. [Google Scholar] [CrossRef]
- Avesani, C.M.; Trolonge, S.; Deleaval, P.; Baria, F.; Mafra, D.; Irving, G.F.; Chauveau, P.; Teta, D.; Kamimura, M.A.; Cuppari, L.; et al. Physical activity and energy expenditure in haemodialysis patients: An international survey. Nephrol. Dial. Transplant. 2012, 27, 2430–2434. [Google Scholar] [CrossRef] [PubMed]
- Fassett, R.G.; Robertson, I.K.; Geraghty, D.P.; Ball, M.J.; Burton, N.W.; Coombes, J.S. Physical Activity Levels in Patients with Chronic Kidney Disease Entering the LORD Trial. Med. Sci. Sports Exerc. 2009, 41, 985–991. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, H.J.; Wilkinson, T.J.; Clarke, A.L.; Gould, D.W.; O’sullivan, T.F.; Xenophontos, S.; Watson, E.L.; Singh, S.J.; Smith, A.C. The association of physical function and physical activity with all-cause mortality and adverse clinical outcomes in nondialysis chronic kidney disease: A systematic review. Ther. Adv. Chronic Dis. 2018, 9, 209–226. [Google Scholar] [CrossRef] [PubMed]
- Beddhu, S.; Wei, G.; Marcus, R.L.; Chonchol, M.; Greene, T. Light-Intensity Physical Activities and Mortality in the United States General Population and CKD Subpopulation. Clin. J. Am. Soc. Nephrol. 2015, 10, 1145–1153. [Google Scholar] [CrossRef] [PubMed]
- Chiba, I.; Lee, S.; Bae, S.; Makino, K.; Katayama, O.; Harada, K.; Tomida, K.; Morikawa, M.; Yamashiro, Y.; Takayanagi, N.; et al. Association of Daily Physical Activity with Disability in Community-Dwelling Older Adults With/Without Chronic Kidney Disease. J. Nutr. Health Aging 2022, 26, 521–528. [Google Scholar] [CrossRef]
- Robinson-Cohen, C. Physical Activity and Rapid Decline in Kidney Function Among Older Adults. Arch. Intern. Med. 2009, 169, 2116–2123. [Google Scholar] [CrossRef]
- Robinson-Cohen, C.; Littman, A.J.; Duncan, G.E.; Weiss, N.S.; Sachs, M.C.; Ruzinski, J.; Kundzins, J.; Rock, D.; de Boer, I.H.; Ikizler, T.A.; et al. Physical Activity and Change in Estimated GFR among Persons with CKD. J. Am. Soc. Nephrol. 2014, 25, 399–406. [Google Scholar] [CrossRef]
- Anand, S.; Johansen, K.L.; Grimes, B.; Kaysen, G.A.; Dalrymple, L.S.; Kutner, N.G.; Chertow, G.M. Physical activity and self-reported symptoms of insomnia, restless legs syndrome, and depression: The comprehensive dialysis study. Hemodial. Int. 2013, 17, 50–58. [Google Scholar] [CrossRef]
- Oh, T.R.; Choi, H.S.; Suh, S.H.; Kim, C.S.; Bae, E.H.; Sung, S.; Han, S.H.; Oh, K.H.; Ma, S.K.; Kim, S.W. The Association between Health-Enhancing Physical Activity and Quality of Life in Patients with Chronic Kidney Disease: Propensity Score Matching Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1318. [Google Scholar] [CrossRef]
- Pei, G.; Tang, Y.; Tan, L.; Tan, J.; Ge, L.; Qin, W. Aerobic exercise in adults with chronic kidney disease (CKD): A meta-analysis. Int. Urol. Nephrol. 2019, 51, 1787–1795. [Google Scholar] [CrossRef]
- Wilkinson, T.J.; Bishop, N.C.; Billany, R.E.; Lightfoot, C.J.; Castle, E.M.; Smith, A.C.; Greenwood, S.A. The effect of exercise training interventions in adult kidney transplant recipients: A systematic review and meta-analysis of randomised control trials. Phys. Ther. Rev. 2022, 27, 114–134. [Google Scholar] [CrossRef]
- Huang, M.; Lv, A.; Wang, J.; Xu, N.; Ma, G.; Zhai, Z.; Zhang, B.; Gao, J.; Ni, C. Exercise Training and Outcomes in Hemodialysis Patients: Systematic Review and Meta-Analysis. Am. J. Nephrol. 2019, 50, 240–254. [Google Scholar] [CrossRef]
- Andrade, F.P.; Rezende, P.D.S.; Ferreira, T.D.S.; Borba, G.C.; Müller, A.M.; Rovedder, P.M.E. Effects of intradialytic exercise on cardiopulmonary capacity in chronic kidney disease: Systematic review and meta-analysis of randomized clinical trials. Sci. Rep. 2019, 9, 18470. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Bai, Y.; Zhao, X.; Huang, L.; Wang, W.; Zhou, W.; Zhang, H. Therapeutic effects of exercise interventions for patients with chronic kidney disease: An umbrella review of systematic reviews and meta-analyses. BMJ Open 2022, 12, e054887. [Google Scholar] [CrossRef]
- Ferreira, T.L.; Ribeiro, H.S.; Ribeiro, A.L.A.; Bonini-Rocha, A.C.; Lucena, J.M.S.; de Oliveira, P.A.; Amorim, F.R.S.; Ferreira, A.P.; Magno, L.A.V.; Martins, W.R. Exercise interventions improve depression and anxiety in chronic kidney disease patients: A systematic review and meta-analysis. Int. Urol. Nephrol. 2021, 53, 925–933. [Google Scholar] [CrossRef] [PubMed]
- Hargrove, N.; El Tobgy, N.; Zhou, O.; Pinder, M.; Plant, B.; Askin, N.; Bieber, L.; Collister, D.; Whitlock, R.; Tangri, N.; et al. Effect of Aerobic Exercise on Dialysis-Related Symptoms in Individuals Undergoing Maintenance Hemodialysis: A Systematic Review and Meta-Analysis of Clinical Trials. Clin. J. Am. Soc. Nephrol. 2021, 16, 560–574. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Wang, Y.; Xiong, L.; Luo, Y.; Huang, Z.; Bin Yi, B. Exercise therapy improves eGFR, and reduces blood pressure and BMI in non-dialysis CKD patients: Evidence from a meta-analysis. BMC Nephrol. 2019, 20, 398. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, M.J.; Bennett, P.N.; Fraser, S.F.; Warmington, S.A. Exercise interventions for improving objective physical function in patients with end-stage kidney disease on dialysis: A systematic review and meta-analysis. Am. J. Physiol. Physiol. 2019, 316, F856–F872. [Google Scholar] [CrossRef]
- Zhang, J.; Bhattacharyya, S.; Hickner, R.C.; Light, A.R.; Lambert, C.J.; Gale, B.K.; Fiehn, O.; Adams, S.H. Skeletal muscle interstitial fluid metabolomics at rest and associated with an exercise bout: Application in rats and humans. Am. J. Physiol. Endocrinol. Metab. 2019, 316, E43–E53. [Google Scholar] [CrossRef]
- Thompson, S.; Wiebe, N.; Padwal, R.S.; Gyenes, G.; Headley, S.A.E.; Radhakrishnan, J.; Graham, M. The effect of exercise on blood pressure in chronic kidney disease: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2019, 14, e0211032. [Google Scholar] [CrossRef]
- Cardoso, D.F.; Marques, E.A.; Leal, D.V.; Ferreira, A.; Baker, L.A.; Smith, A.C.; Viana, J.L. Impact of physical activity and exercise on bone health in patients with chronic kidney disease: A systematic review of observational and experimental studies. BMC Nephrol. 2020, 21, 334. [Google Scholar] [CrossRef] [PubMed]
- March, D.S.; Wilkinson, T.J.; Burnell, T.; Billany, R.E.; Jackson, K.; Baker, L.A.; Thomas, A.; Robinson, K.A.; Watson, E.L.; Graham-Brown, M.P.M.; et al. The Effect of Non-Pharmacological and Pharmacological Interventions on Measures Associated with Sarcopenia in End-Stage Kidney Disease: A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 1817. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.; Sandoo, A.; Macdonald, J. The Role of Exercise Training in Delaying Kidney Function Decline in Non-Dialysis-Dependent Chronic Kidney Disease. Kidney Dial. 2022, 2, 262–286. [Google Scholar] [CrossRef]
- Baker, L.A.; March, D.S.; Wilkinson, T.J.; Billany, R.E.; Bishop, N.C.; Castle, E.M.; Chilcot, J.; Davies, M.D.; Graham-Brown, M.P.M.; Greenwood, S.A.; et al. Clinical practice guideline exercise and lifestyle in chronic kidney disease. BMC Nephrol. 2022, 23, 75. [Google Scholar] [CrossRef] [PubMed]
- Yamagata, K.; Hoshino, J.; Sugiyama, H.; Hanafusa, N.; Shibagaki, Y.; Komatsu, Y.; Konta, T.; Fujii, N.; Kanda, E.; Sofue, T.; et al. Clinical practice guideline for renal rehabilitation: Systematic reviews and recommendations of exercise therapies in patients with kidney diseases. Ren. Replace. Ther. 2019, 5, 28. [Google Scholar] [CrossRef]
- Coster, W.J. Making the Best Match: Selecting Outcome Measures for Clinical Trials and Outcome Studies. Am. J. Occup. Ther. 2013, 67, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Manns, B.; Hemmelgarn, B.; Wheeler, D.C.; Evangelidis, N.; Tugwell, P.; Crowe, S.; Van Biesen, W.; Winkelmayer, W.C.; O’Donoghue, D.; et al. Establishing Core Outcome Domains in Hemodialysis: Report of the Standardized Outcomes in Nephrology–Hemodialysis (SONG-HD) Consensus Workshop. Am. J. Kidney Dis. 2017, 69, 97–107. [Google Scholar] [CrossRef]
- Tong, A.; Gill, J.; Budde, K.; Marson, L.; Reese, P.P.; Rosenbloom, D.; Rostaing, L.; Wong, G.; Josephson, M.A.; Pruett, T.L.; et al. Toward establishing core outcome domains for trials in kidney transplantation: Report of the standardized outcomes in nephrology–kidney transplantation (SONG-Tx) consensus workshops. Transplantation 2017, 101, 1887. [Google Scholar] [CrossRef]
- Bouchard, C.; Blair, S.N.; Haskell, W.L. Physical Activity and Health; Human Kinetics: Champaign, IL, USA, 2012. [Google Scholar]
- Fuhrmann, I.; Krause, R. Principles of exercising in patients with chronic kidney disease, on dialysis and for kidney transplant recipients. Clin. Nephrol. 2004, 61, S14–S25. [Google Scholar]
- Jegatheesan, D.K.; Modderman, R.; Krishnasamy, R.; Tong, A.; Coombes, J.S.; Viecelli, A.K.; Johnson, D.W.; Isbel, N. A Systematic Review of Scope and Consistency of Outcome Measures for Physical Fitness in Chronic Kidney Disease Trials. Kidney Int. Rep. 2021, 6, 1280–1288. [Google Scholar] [CrossRef]
- Williamson, P.R.; Altman, D.G.; Blazeby, J.M.; Clarke, M.; DeVane, D.; Gargon, E.; Tugwell, P. Developing core outcome sets for clinical trials: Issues to consider. Trials 2012, 13, 132. [Google Scholar] [CrossRef] [PubMed]
- Prinsen, C.A.C.; Vohra, S.; Rose, M.R.; King-Jones, S.; Ishaque, S.; Bhaloo, Z.; Adams, D.; Terwee, C.B. Core Outcome Measures in Effectiveness Trials (COMET) initiative: Protocol for an international Delphi study to achieve consensus on how to select outcome measurement instruments for outcomes included in a ‘core outcome set’. Trials 2014, 15, 247. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Manns, B.; Wang, A.Y.M.; Hemmelgarn, B.; Wheeler, D.C.; Gill, J.; Tugwell, P.; Pecoits-Filho, R.; Crowe, S.; Harris, T.; et al. Implementing core outcomes in kidney disease: Report of the Standardized Outcomes in Nephrology (SONG) implementation workshop. Kidney Int. 2018, 94, 1053–1068. [Google Scholar] [CrossRef] [PubMed]
- Webbe, J.; Sinha, I.; Gale, C. Core Outcome Sets. Arch. Dis. Child. Educ. Pract. 2018, 103, 163–166. [Google Scholar] [CrossRef] [PubMed]
- Tugwell, P.; Boers, M. OMERACT conference on outcome measures in rheumatoid arthritis clinical trials: Introduction. J. Rheumatol. 1993, 20, 528–530. [Google Scholar] [PubMed]
- Verberne, W.R.; Das-Gupta, Z.; Allegretti, A.S.; Bart, H.A.; van Biesen, W.; García-García, G.; Gibbons, E.; Parra, E.; Hemmelder, M.H.; Jager, K.J.; et al. Development of an International Standard Set of Value-Based Outcome Measures for Patients with Chronic Kidney Disease: A Report of the International Consortium for Health Outcomes Measurement (ICHOM) CKD Working Group. Am. J. Kidney Dis. 2019, 73, 372–384. [Google Scholar] [CrossRef] [PubMed]
- Martin-Kerry, J.; Taylor, J.; Scott, S.; Patel, M.; Wright, D.; Clark, A.; Turner, D.; Alldred, D.P.; Murphy, K.; Keevil, V.; et al. Developing a core outcome set for hospital deprescribing trials for older people under the care of a geriatrician. Age Ageing 2022, 51, afac241. [Google Scholar] [CrossRef] [PubMed]
- Crocker, H.; Peters, M.; Foster, C.; Black, N.; Fitzpatrick, R. A core outcome set for randomised controlled trials of physical activity interventions: Development and challenges. BMC Public Health 2022, 22, 389. [Google Scholar] [CrossRef]
- Ramdharry, G.; Buscemi, V.; Boaz, A.; Dawes, H.; Jaki, T.; Jones, F.; Marsden, J.; Paul, L.; Playle, R.; Randell, E.; et al. Proposing a Core Outcome Set for Physical Activity and Exercise Interventions in People with Rare Neurological Conditions. Front. Rehabil. Sci. 2021, 2, 705474. [Google Scholar] [CrossRef]
- Gonçalves, A.-C.; Samuel, D.; Ramsay, M.; Demain, S.; Marques, A. A Core Outcome Set to Evaluate Physical Activity Interventions for People Living with Dementia. Gerontologist 2020, 60, 682–692. [Google Scholar] [CrossRef]
- Paul, L.; Coote, S.; Crosbie, J.; Dixon, D.; Hale, L.; Holloway, E.; McCrone, P.; Miller, L.; Saxton, J.; Sincock, C.; et al. Core outcome measures for exercise studies in people with multiple sclerosis: Recommendations from a multidisciplinary consensus meeting. Mult. Scler. J. 2014, 20, 1641–1650. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.; Mallett, R.; Harrop, D.; McLean, S. Development of a core set of outcomes for exercise and physical activity schemes. Physiotherapy 2019, 105, e22–e23. [Google Scholar] [CrossRef]
- Taryana, A.A.; Krishnasamy, R.; Bohm, C.; Palmer, S.C.; Wiebe, N.; Boudville, N.; MacRae, J.; Coombes, J.S.; Hawley, C.; Isbel, N.; et al. Physical activity for people with chronic kidney disease: An international survey of nephrologist practice patterns and research priorities. BMJ Open 2019, 9, e032322. [Google Scholar] [CrossRef] [PubMed]
- Hughes, K.L.; Williamson, P.R.; Young, B. In-depth qualitative interviews identified barriers and facilitators that influenced chief investigators’ use of core outcome sets in randomised controlled trials. J. Clin. Epidemiol. 2022, 144, 111–120. [Google Scholar] [CrossRef] [PubMed]
| Study | Population | Outcomes | Outcome Measures |
|---|---|---|---|
| Ramdharry et al., 2021 [50] | Rare neurological conditions |
|
|
|
| ||
| Gonçalves et al., 2020 [51] | Dementia |
| Not identified as part of the study |
| |||
| |||
| |||
| |||
| |||
| |||
| Paul et al., 2014 [52] | Multiple sclerosis |
|
|
|
| ||
|
| ||
|
| ||
|
| ||
| Crocker et al., 2022 [49] | General adult population |
|
|
|
| ||
| Thompson et al., 2019 [53] | Musculoskeletal disorders |
| Not identified as part of the study |
| |||
| |||
| |||
| |||
| |||
| |||
| |||
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilkinson, T.J.; MacRae, J.M.; Thompson, S.; Bohm, C., on behalf of the Global Renal Exercise Network (GREX). Making the Case for Standardized Outcome Measures in Exercise and Physical Activity Research in Chronic Kidney Disease. Kidney Dial. 2023, 3, 219-228. https://doi.org/10.3390/kidneydial3020020
Wilkinson TJ, MacRae JM, Thompson S, Bohm C on behalf of the Global Renal Exercise Network (GREX). Making the Case for Standardized Outcome Measures in Exercise and Physical Activity Research in Chronic Kidney Disease. Kidney and Dialysis. 2023; 3(2):219-228. https://doi.org/10.3390/kidneydial3020020
Chicago/Turabian StyleWilkinson, Thomas J., Jennifer M. MacRae, Stephanie Thompson, and Clara Bohm on behalf of the Global Renal Exercise Network (GREX). 2023. "Making the Case for Standardized Outcome Measures in Exercise and Physical Activity Research in Chronic Kidney Disease" Kidney and Dialysis 3, no. 2: 219-228. https://doi.org/10.3390/kidneydial3020020
APA StyleWilkinson, T. J., MacRae, J. M., Thompson, S., & Bohm, C., on behalf of the Global Renal Exercise Network (GREX). (2023). Making the Case for Standardized Outcome Measures in Exercise and Physical Activity Research in Chronic Kidney Disease. Kidney and Dialysis, 3(2), 219-228. https://doi.org/10.3390/kidneydial3020020






