Hesitant Minds in Vulnerable Times: COVID-19 Vaccine Hesitancy Among University Students in Ukraine
Abstract
1. Introduction
2. Materials and Methods
2.1. Questionnaire
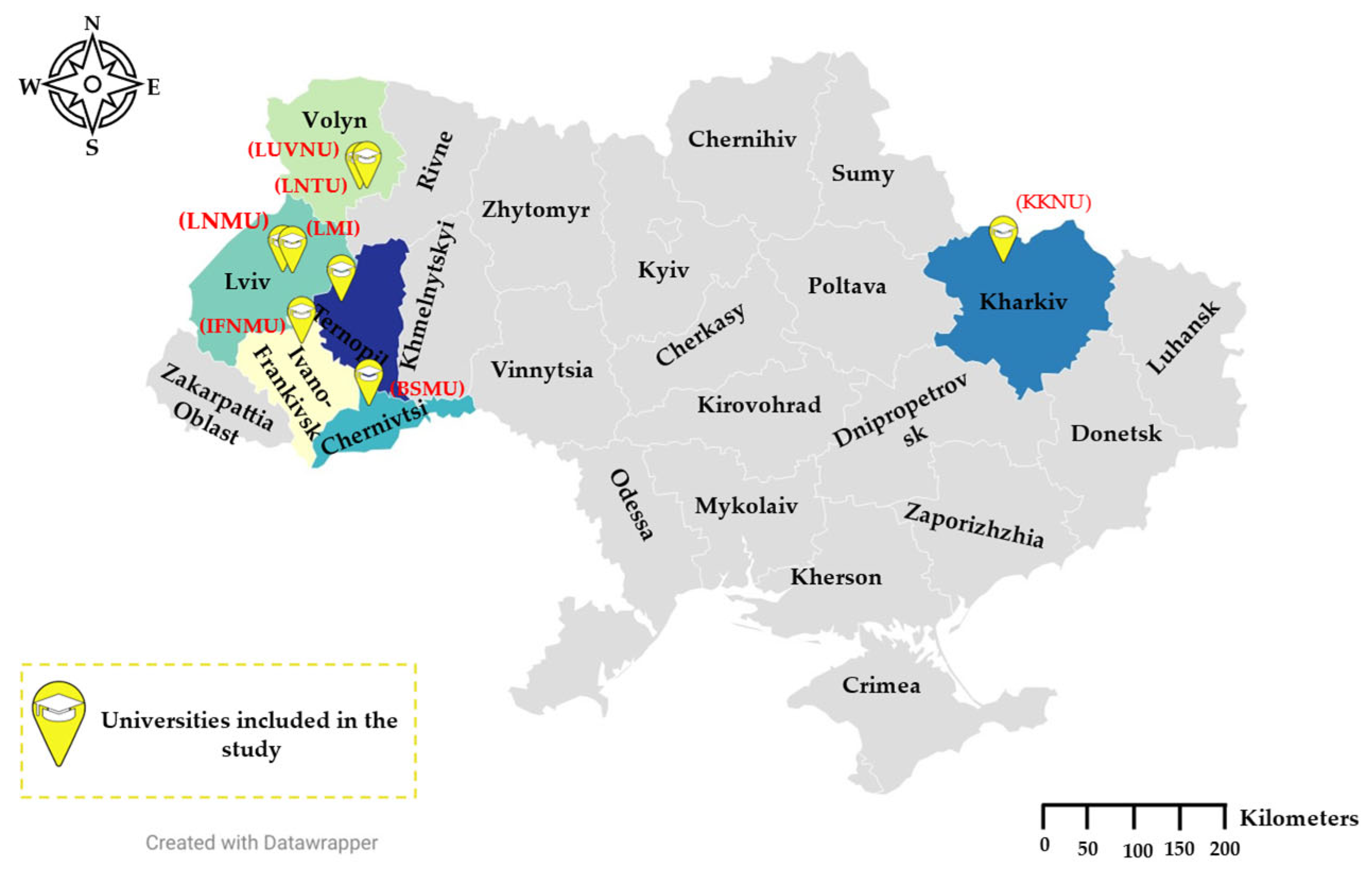
2.2. Study Design and Data Collection
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.1.1. Sociodemographic Indicators
3.1.2. The 5Cs Antecedents, Sources of Information, and Conspiracy Mentality
3.2. Inferential Statistics
3.2.1. Factors Influencing Hesitancy Toward COVID-19 Vaccination
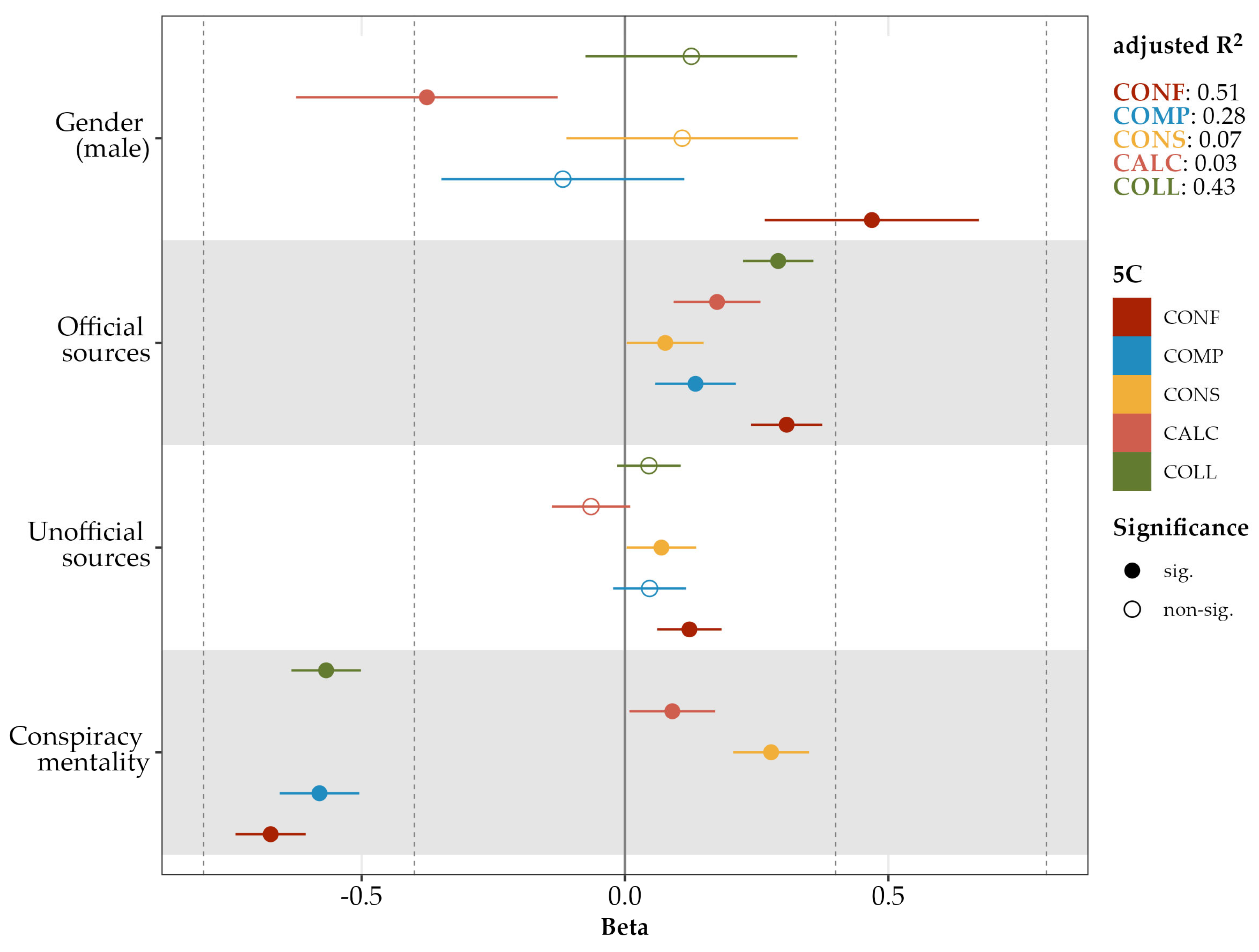
3.2.2. Factors Influencing the 5Cs Antecedents of Hesitancy Toward COVID-19 Vaccine
4. Discussion
Limitations of Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhao, S.; Hu, S.; Zhou, X.; Song, S.; Wang, Q.; Zheng, H.; Zhang, Y.; Hou, Z. The Prevalence, Features, Influencing Factors, and Solutions for COVID-19 Vaccine Misinformation: Systematic Review. JMIR Public Health Surveill. 2023, 9, e40201. [Google Scholar] [CrossRef]
- WHO Looks Back at 2024. Available online: https://www.who.int/news-room/spotlight/who-looks-back-at-2024 (accessed on 11 July 2025).
- Williams, S.N. Vaccine Hesitancy Is One of the Greatest Threats to Global Health—and the Pandemic Has Made It Worse. Available online: http://theconversation.com/vaccine-hesitancy-is-one-of-the-greatest-threats-to-global-health-and-the-pandemic-has-made-it-worse-208227 (accessed on 11 July 2025).
- Jennings, W.; Valgarðsson, V.; McKay, L.; Stoker, G.; Mello, E.; Baniamin, H.M. Trust and Vaccine Hesitancy during the COVID-19 Pandemic: A Cross-National Analysis. Vaccine X 2023, 14, 100299. [Google Scholar] [CrossRef]
- Mamontova, T.V. An Analysis of COVID-19 Vaccination Campaign in Ukraine. Eur. J. Public Health 2024, 34, 156–162. [Google Scholar] [CrossRef]
- WHO Chief Declares End to COVID-19 as a Global Health Emergency|UN News. Available online: https://news.un.org/en/story/2023/05/1136367 (accessed on 30 June 2025).
- UNICEF Press Centre|Increasing Immunization Coverage Is Priority for Ukrainian Government—Vice Prime Minister of Ukraine|UNICEF. Available online: https://www.unicef.org/eca/press-releases/increasing-immunization-coverage-priority-ukraine (accessed on 30 June 2025).
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A Global Database of COVID-19 Vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Hotez, P.J. Global Vaccine Access Demands Combating Both Inequity And Hesitancy. Health Aff. 2023, 42, 1681–1688. [Google Scholar] [CrossRef]
- Malcolm, L.J.; McLean, K.E. COVID-19 Vaccine Anxieties: Exploring Social and Political Drivers of Vaccine Attitudes in Kono District, Sierra Leone. J. Biosoc. Sci. 2025, 57, 179–194. [Google Scholar] [CrossRef]
- Goodwin, R.; Nguyen Luu, L.A.; Wiwattanapantuwong, J.; Kovács, M.; Suttiwan, P.; Levin, Y. Two-Tailed Dogs, Social Unrest and COVID-19 Vaccination: Politics, Hesitancy and Vaccine Choice in Hungary and Thailand. Vaccines 2022, 10, 789. [Google Scholar] [CrossRef]
- Achore, M.; Braimah, J.A.; Dowou, R.K.; Kuuire, V.; Ayanore, M.A.; Bisung, E. Institutional Trust, Conspiracy Beliefs and Covid-19 Vaccine Uptake and Hesitancy among Adults in Ghana. PLOS Glob. Public Health 2024, 4, e00038. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Lee, W.; Lin, F. Infodemic, Institutional Trust, and COVID-19 Vaccine Hesitancy: A Cross-National Survey. Int. J. Environ. Res. Public Health 2022, 19, 8033. [Google Scholar] [CrossRef] [PubMed]
- Musa, S.; Cilovic-Lagarija, S.; Kavazovic, A.; Bosankic-Cmajcanin, N.; Stefanelli, A.; Scott, N.A.; Scherzer, M.; Kiss, Z.; Bach Habersaat, K. COVID-19 Risk Perception, Trust in Institutions and Negative Affect Drive Positive COVID-19 Vaccine Intentions. Int. J. Public Health 2022, 67, 1604231. [Google Scholar] [CrossRef]
- Waheed, A.; Abu Bakr Elsaid, N.M.; Ghweeba, M.; Elmaraghy, N.; Al-Touny, S.A.; Nemr, N.; Kishk, R.M.; Aly, H.M. Determinants of Coronavirus Disease 2019 Vaccine Acceptance, Hesitancy, and Barriers among Healthcare Workers in Ismailia, Egypt: A Mixed Methods Study. J. Egypt. Public Health Assoc. 2022, 97, 25. [Google Scholar] [CrossRef]
- Christodoulakis, A.; Bouloukaki, I.; Aravantinou-Karlatou, A.; Zografakis-Sfakianakis, M.; Tsiligianni, I. Vaccine Hesitancy and Associated Factors Amongst Health Professionals: A Scoping Review of the Published Literature. Vaccines 2024, 12, 1411. [Google Scholar] [CrossRef]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. ‘Vaccine Hesitancy’ among University Students in Italy during the COVID-19 Pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef]
- Patelarou, E.; Galanis, P.; Mechili, E.A.; Argyriadi, A.; Argyriadis, A.; Asimakopoulou, E.; Brokaj, S.; Bucaj, J.; Carmona-Torres, J.M.; Cobo-Cuenca, A.I.; et al. Factors Influencing Nursing Students’ Intention to Accept COVID-19 Vaccination: A Pooled Analysis of Seven European Countries. Nurse Educ. Today 2021, 104, 105010. [Google Scholar] [CrossRef]
- Rzymski, P.; Zeyland, J.; Poniedziałek, B.; Małecka, I.; Wysocki, J. The Perception and Attitudes toward COVID-19 Vaccines: A Cross-Sectional Study in Poland. Vaccines 2021, 9, 382. [Google Scholar] [CrossRef]
- Korolchuk, O.; Vasiuk, N.; Klymkova, I.; Shvets, D.; Piddubnyi, O. COVID-19 Vaccination under Conditions of War in Ukraine. Asian Bioeth. Rev. 2023, 15, 259–281. [Google Scholar] [CrossRef]
- Costantino, V.; MacIntyre, C.R. Impact of Vaccine Coverage and Disruption to Health Services on COVID-19 in Ukraine. Sci. Rep. 2024, 14, 14729. [Google Scholar] [CrossRef] [PubMed]
- Public Health and Immunization Efforts in Ukraine Bolstered by WHO amid the War. Available online: https://www.who.int/europe/news/item/11-04-2023-public-health-and-immunization-efforts-in-ukraine-bolstered-by-who-amid-the-war (accessed on 30 June 2025).
- Almost 114,000 Ukrainians Vaccinated Against COVID-19 Over Past Day. Available online: https://www.ukrinform.net/rubric-society/3374863-almost-114000-ukrainians-vaccinated-against-covid19-over-past-day.html (accessed on 30 June 2025).
- Park, A. Why Ukraine’s COVID-19 Problem Is Everyone’s Problem. Available online: https://time.com/6153254/ukraine-russia-war-covid-19/ (accessed on 10 April 2025).
- How Many People in Ukraine and the World Are Affected by the COVID-19 Pandemic: Incidence Statistics. Available online: https://visitukraine.today/blog/32/how-many-people-in-ukraine-and-the-world-are-affected-by-the-covid-19-pandemic-incidence-statistics (accessed on 11 July 2025).
- Wide Resistance to Vaccines Plagues Ukraine’s COVID-19 Fight. Available online: https://apnews.com/article/ukraine-wide-resistance-coronavirus-vaccines-9c59021f25140e990e03142f974501 (accessed on 30 June 2025).
- Moskova, M.; Zasheva, A.; Kunchev, M.; Popivanov, I.; Dimov, D.; Vaseva, V.; Kundurzhiev, T.; Tsachev, I.; Baymakova, M. Students’ Attitudes toward COVID-19 Vaccination: An Inter-University Study from Bulgaria. Int. J. Environ. Res. Public Health 2022, 19, 9779. [Google Scholar] [CrossRef]
- Popa, A.D.; Enache, A.I.; Popa, I.V.; Antoniu, S.A.; Dragomir, R.A.; Burlacu, A. Determinants of the Hesitancy toward COVID-19 Vaccination in Eastern European Countries and the Relationship with Health and Vaccine Literacy: A Literature Review. Vaccines 2022, 10, 672. [Google Scholar] [CrossRef] [PubMed]
- Holt, E. COVID-19 Vaccination in Ukraine. Lancet Infect. Dis. 2021, 21, 462. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, A.P.; Kiran, T.; Thakur, J.S.; Sharma, D.; Junaid, K.P.; Gupta, R.; Prajapati, A.; Amaljith, A.B. Validation of the 5C Questionnaire to Assess the Hesitancy towards Adult Vaccination among the Hindi Speaking Population of Northern India. Discov. Soc. Sci. Health 2024, 4, 2. [Google Scholar] [CrossRef]
- Nwachukwu, G.; Rihan, A.; Nwachukwu, E.; Uduma, N.; Elliott, K.S.; Tiruneh, Y.M. Understanding COVID-19 Vaccine Hesitancy in the United States: A Systematic Review. Vaccines 2024, 12, 747. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond Confidence: Development of a Measure Assessing the 5C Psychological Antecedents of Vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef] [PubMed]
- Danyliuk, I.; Kurapov, A.; Malysheva, K.; Lytvyn, S. Psychometric Properties of the Scale “5C Psychological Antecedents of Vaccination”: Ukrainian Sample. Insight Psychol. Dimens. Soc. 2023, 10, 13–39. [Google Scholar] [CrossRef] [PubMed]
- Davison, A.C.; Hinkley, D.V. Bootstrap Methods and Their Application; Cambridge Series in Statistical and Probabilistic Mathematics; Cambridge University Press: Cambridge, UK, 1997; ISBN 978-0-1-57471-6. [Google Scholar]
- Fox, J.; Weisberg, S. An R Companion to Applied Regression; Sage Publications: New York, NY, USA, 2018. [Google Scholar]
- Van Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Khongyot, T.; Takyi, A.; Ndzeshang, D.S.; Fai, K.G.N.; Win, T.Z.; Vorlasane, L.; Javes, G.O.; Kaneko, S.; Moriyasu, T. Mental Health and COVID-19 Vaccine Hesitancy among Health-Related University Students: A Cross-Sectional Multi-Center Study. Trop. Med. Health 2025, 53, 71. [Google Scholar] [CrossRef]
- Hunder, M. Russia vs Ukraine: The Biggest War of the Fake News Era. Reuters 2024. Available online: https://www.reuters.com/world/europe/russia-vs-ukraine-biggest-war-fake-news-era-2024-07-31/ (accessed on 20 May 2025).
- Bjork, A. Progress Toward Poliomyelitis Eradication—Afghanistan, January 2022–June 2023. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 1020–1026. [Google Scholar] [CrossRef]
- Collective Responsibility, Confidence in Immunizations Indicate Potential of Vaccine Refusal. Available online: https://www.pharmacytimes.com/view/collective-responsibility-confidence-in-immunizations-indicate-potential-of-vaccine-refusal (accessed on 30 June 2025).
- Rancher, C.; Moreland, A.D.; Smith, D.W.; Cornelison, V.; Schmidt, M.G.; Boyle, J.; Dayton, J.; Kilpatrick, D.G. Using the 5C Model to Understand COVID-19 Vaccine Hesitancy across a National and South Carolina Sample. J. Psychiatr. Res. 2023, 160, 180–186. [Google Scholar] [CrossRef]
- Yeboah, P.; Daliri, D.B.; Abdin, A.Y.; Appiah-Brempong, E.; Pitsch, W.; Panyin, A.B.; Adusei, E.B.A.; Razouk, A.; Nasim, M.J.; Jacob, C. Knowledge into the Practice against COVID-19: A Cross-Sectional Study from Ghana. Int. J. Environ. Res. Public Health 2021, 18, 12902. [Google Scholar] [CrossRef]
- Karlsson, L.C.; Lewandowsky, S.; Antfolk, J.; Salo, P.; Lindfelt, M.; Oksanen, T.; Kivimäki, M.; Soveri, A. The Association between Vaccination Confidence, Vaccination Behavior, and Willingness to Recommend Vaccines among Finnish Healthcare Workers. PLoS ONE 2019, 14, e0224330. [Google Scholar] [CrossRef]
- Eitze, S.; Felgendreff, L.; Horstkötter, N.; Seefeld, L.; Betsch, C. Exploring Pre-Pandemic Patterns of Vaccine Decision-Making with the 5C Model: Results from Representative Surveys in 2016 and 2018. BMC Public Health 2024, 24, 1205. [Google Scholar] [CrossRef]
- Parisi, A.; Regazzi, L.; Spanaus, E.S.; Valz Gris, A.; Cadeddu, C.; Moore, M.; Ricciardi, W.; Lomazzi, M. Impact of COVID-19 Pandemic on Vaccine Hesitancy and Sentiment Changes: A Survey of Healthcare Workers in 12 Countries. Public Health 2025, 238, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Krämer, W. Kahneman, D. (2011): Thinking, Fast and Slow. Stat. Pap. 2014, 55, 915. [Google Scholar] [CrossRef]
- Not All Skepticism Is Equal: Exploring the Ideological Antecedents of Science Acceptance and Rejection. Available online: https://journals.sagepub.com/doi/epub/10.1177/0146167217741314 (accessed on 30 June 2025).
- Martinelli, M.; Veltri, G.A. COVID-19 Vaccine Acceptance: A Comparative Longitudinal Analysis of the Association between Risk Perception, Confidence, and the Acceptance of a COVID-19 Vaccine. Risk Anal. 2024, 44, 802–816. [Google Scholar] [CrossRef] [PubMed]
- Habib, T.Z.; Ennab, F.; Matiashova, L.; Nawaz, F.A.; Volkova, A.; Trill, V.; Essar, M.Y. Double Trouble: COVID-19 Vaccine Misinformation amidst Conflict in Ukraine. Ann. Med. Surg. 2022, 80, 2. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Rabin, K.; Ratzan, S.C.; Parsons Leigh, J.; Hu, J.; El-Mohandes, A. Revisiting COVID-19 Vaccine Hesitancy around the World Using Data from 23 Countries in 2021. Nat. Commun. 2022, 13, 3801. [Google Scholar] [CrossRef]
- Amponsah-Tabi, S.; Djokoto, R.; Opoku, S.; Senu, E.; Boakye, D.K.; Azanu, W.K.; Ankobea-Kokroe, F.; Owusu-Asubonteng, G.; Ansah, R.O.; Owusu, E.; et al. Knowledge, Attitude and Acceptability of COVID-19 Vaccine among Residents in Rural Communities in Ghana: A Multi-Regional Study. BMC Infect. Dis. 2023, 23, 60. [Google Scholar] [CrossRef]
- Yeboah, P.; Abdin, A.Y.; Gyasi, T.O.; Anyimiah, P.; Osafo, N.; Skotzke, P.; Pitsch, W.; Brobbey, M.O.; Panyin, A.B.; Razouk, A. Informed but Unvaccinated: A Cross-Sectional Study Among University Students in Ghana. COVID 2025, 5, 47. [Google Scholar] [CrossRef]
- Al-Abdulla, O.; Alaref, M.; Kallström, A.; Kauhanen, J. Individual and Social Determinants of COVID-19 Vaccine Hesitancy and Uptake in Northwest Syria. BMC Health Serv. Res. 2024, 24, 265. [Google Scholar] [CrossRef]
- Ahmed, A.; Al-Aghbari, A.A.; Hassan, O.E.-H.; McGowan, M.; Al-Qadasi, Y.; Dureab, F. The COVID-19 Infodemic as a Major Driver for Vaccine Hesitancy in Conflict Settings: A Mixed-Method Study. Discov. Health Syst. 2024, 3, 60. [Google Scholar] [CrossRef]
- Feng, B. Gaming with Health Misinformation: A Social Capital-Based Study of Corrective Information Sharing Factors in Social Media. Front. Public Health 2024, 12, 1351820. [Google Scholar] [CrossRef]
- Enria, L.; Dwyer, H.; Marchant, M.; Beckmann, N.; Schmidt-Sane, M.; Conteh, A.; Mansaray, A.; N’Jai, A. Political Dimensions of Misinformation, Trust, and Vaccine Confidence in a Digital Age. BMJ 2024, 385, e079940. [Google Scholar] [CrossRef] [PubMed]
- Ugarte, D.A.; Young, S. Effects of an Online Community Peer-Support Intervention on COVID-19 Vaccine Misinformation Among Essential Workers: Mixed-Methods Analysis. West. J. Emerg. Med. Integr. Emerg. Care Popul. Health 2023, 24, 264. [Google Scholar] [CrossRef]
- Zimdars, M.; Cullinan, M.E.; Na, K. Alternative Health Groups on Social Media, Misinformation, and the (de)Stabilization of Ontological Security. New Media Soc. 2024, 26, 6059–6076. [Google Scholar] [CrossRef]
- Skulmowski, A.; Standl, B. COVID-19 Information Fatigue? A Case Study of a German University Website during Two Waves of the Pandemic. Hum. Behav. Emerg. Technol. 2021, 3, 350–356. [Google Scholar] [CrossRef]
- Sun, J.; Lee, S.K. “No More COVID-19 Messages via Social Media, Please”: The Mediating Role of COVID-19 Message Fatigue between Information Overload, Message Avoidance, and Behavioral Intention. Curr. Psychol. 2023, 42, 20347–20361. [Google Scholar] [CrossRef] [PubMed]
- Kisa, A.; Kisa, S. Health Conspiracy Theories: A Scoping Review of Drivers, Impacts, and Countermeasures. Int. J. Equity Health 2025, 24, 93. [Google Scholar] [CrossRef]
- Roozenbeek, J.; Schneider, C.R.; Dryhurst, S.; Kerr, J.; Freeman, A.L.J.; Recchia, G.; van der Bles, A.M.; van der Linden, S. Susceptibility to Misinformation about COVID-19 around the World. R. Soc. Open Sci. 2020, 7, 201199. [Google Scholar] [CrossRef] [PubMed]
- Winter, K.; Pummerer, L.; Hornsey, M.J.; Sassenberg, K. Pro-Vaccination Subjective Norms Moderate the Relationship between Conspiracy Mentality and Vaccination Intentions. Br. J. Health Psychol. 2022, 27, 390–405. [Google Scholar] [CrossRef]
- McNaghten, A.D. COVID-19 Vaccination Coverage and Vaccine Confidence by Sexual Orientation and Gender Identity—United States, August 29–October 30, 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 171–176. [Google Scholar] [CrossRef]
- Jayawardana, S.; Esquivel, M.; Orešković, T.; Mossialos, E. Gender Differences in COVID-19 Preventative Measures and Vaccination Rates in the United States: A Longitudinal Survey Analysis. Vaccine 2024, 42, 126044. [Google Scholar] [CrossRef]
- Heidari, S.; Palmer-Ross, A.; Goodman, T. A Systematic Review of the Sex and Gender Reporting in COVID-19 Clinical Trials. Vaccines 2021, 9, 1322. [Google Scholar] [CrossRef] [PubMed]
- Grygarová, D.; Kožený, J.; Tišanská, L.; Havlík, M.; Horáček, J. Trust in Official Information as a Key Predictor of COVID-19 Vaccine Acceptance: Evidence from a Czech Longitudinal Survey Study. BMC Public Health 2025, 25, 770. [Google Scholar] [CrossRef] [PubMed]
- The Correlation between Conspiracy Mentality and Vaccine Misinformation Acceptance: Strategies for Mitigation|DISA 2025.
- Atad, E. Health Decisions Under Uncertainty: The Roles of Conspiracy Beliefs and Institutional Trust. Behav. Sci. 2025, 15, 524. [Google Scholar] [CrossRef] [PubMed]
- Hassan Raza, S.; Yousaf, M.; Zaman, U.; Waheed Khan, S.; Core, R.; Malik, A. Unlocking Infodemics and Mysteries in COVID-19 Vaccine Hesitancy: Nexus of Conspiracy Beliefs, Digital Informational Support, Psychological Well-Being, and Religious Fatalism. Vaccine 2023, 41, 1703–1715. [Google Scholar] [CrossRef]


| Characteristic | COVID-19 Status | |||
|---|---|---|---|---|
| Overall | Acceptant | Hesitant | Resistant | |
| N = 936 | n = 600 | n = 101 | n = 235 | |
| Confidence | 4.37 (1.59) | 4.81 (1.40) | 4.79 (1.21) | 3.05 (1.43) |
| Complacency | 4.67 (1.49) | 5.05 (1.37) | 4.89 (1.20) | 3.58 (1.36) |
| Constraints | 2.25 (1.24) | 2.12 (1.16) | 2.80 (1.35) | 2.35 (1.33) |
| Calculation | 5.66 (1.37) | 5.57 (1.41) | 5.65 (1.34) | 5.91 (1.27) |
| Collective responsibility | 4.95 (1.45) | 5.42 (1.23) | 5.09 (1.26) | 3.68 (1.27) |
| Official vaccine information sources | 4.76 (1.37) | 5.04 (1.23) | 4.95 (1.21) | 3.98 (1.47) |
| Unofficial vaccine information sources | 3.94 (1.39) | 4.06 (1.39) | 4.15 (1.07) | 3.53 (1.45) |
| Misinformation (conspiracy mentality) | 2.62 (1.19) | 2.35 (1.01) | 2.39 (1.09) | 3.43 (1.29) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeboah, P.; Razouk, A.; Skotzke, P.; Pitsch, W.; Chubuchna, O.; Serhiyenko, V.; Slyvka, N.; Holota, S.; Nasim, M.J.; Abdin, A.Y.; et al. Hesitant Minds in Vulnerable Times: COVID-19 Vaccine Hesitancy Among University Students in Ukraine. COVID 2025, 5, 122. https://doi.org/10.3390/covid5080122
Yeboah P, Razouk A, Skotzke P, Pitsch W, Chubuchna O, Serhiyenko V, Slyvka N, Holota S, Nasim MJ, Abdin AY, et al. Hesitant Minds in Vulnerable Times: COVID-19 Vaccine Hesitancy Among University Students in Ukraine. COVID. 2025; 5(8):122. https://doi.org/10.3390/covid5080122
Chicago/Turabian StyleYeboah, Prince, Afraa Razouk, Philip Skotzke, Werner Pitsch, Olena Chubuchna, Victoria Serhiyenko, Nataliia Slyvka, Serhii Holota, Muhammad Jawad Nasim, Ahmad Yaman Abdin, and et al. 2025. "Hesitant Minds in Vulnerable Times: COVID-19 Vaccine Hesitancy Among University Students in Ukraine" COVID 5, no. 8: 122. https://doi.org/10.3390/covid5080122
APA StyleYeboah, P., Razouk, A., Skotzke, P., Pitsch, W., Chubuchna, O., Serhiyenko, V., Slyvka, N., Holota, S., Nasim, M. J., Abdin, A. Y., & Jacob, C. (2025). Hesitant Minds in Vulnerable Times: COVID-19 Vaccine Hesitancy Among University Students in Ukraine. COVID, 5(8), 122. https://doi.org/10.3390/covid5080122












