Attachment and Coping in the Second Pandemic Year: The Impact on Loneliness and Emotional Distress
Abstract
:1. Introduction
- (1)
- Measuring the impact of attachment and coping on loneliness;
- (2)
- Measuring the impact of attachment and coping on emotional distress;
- (3)
- Measuring loneliness as a mediator between attachment and emotional distress. The secondary goals included measuring the impact of gender and age.
2. Study Design
2.1. Sample Demographics
2.2. Measurements
2.3. Statistical Analysis
3. Results
3.1. Gender Differences
3.2. Correlational Analyses
3.3. Regression Analysis
3.3.1. Attachment as Predictor of Loneliness and Emotional Distress
3.3.2. Coping Styles as Predictors of Loneliness and Emotional Distress
3.4. Mediation Analysis
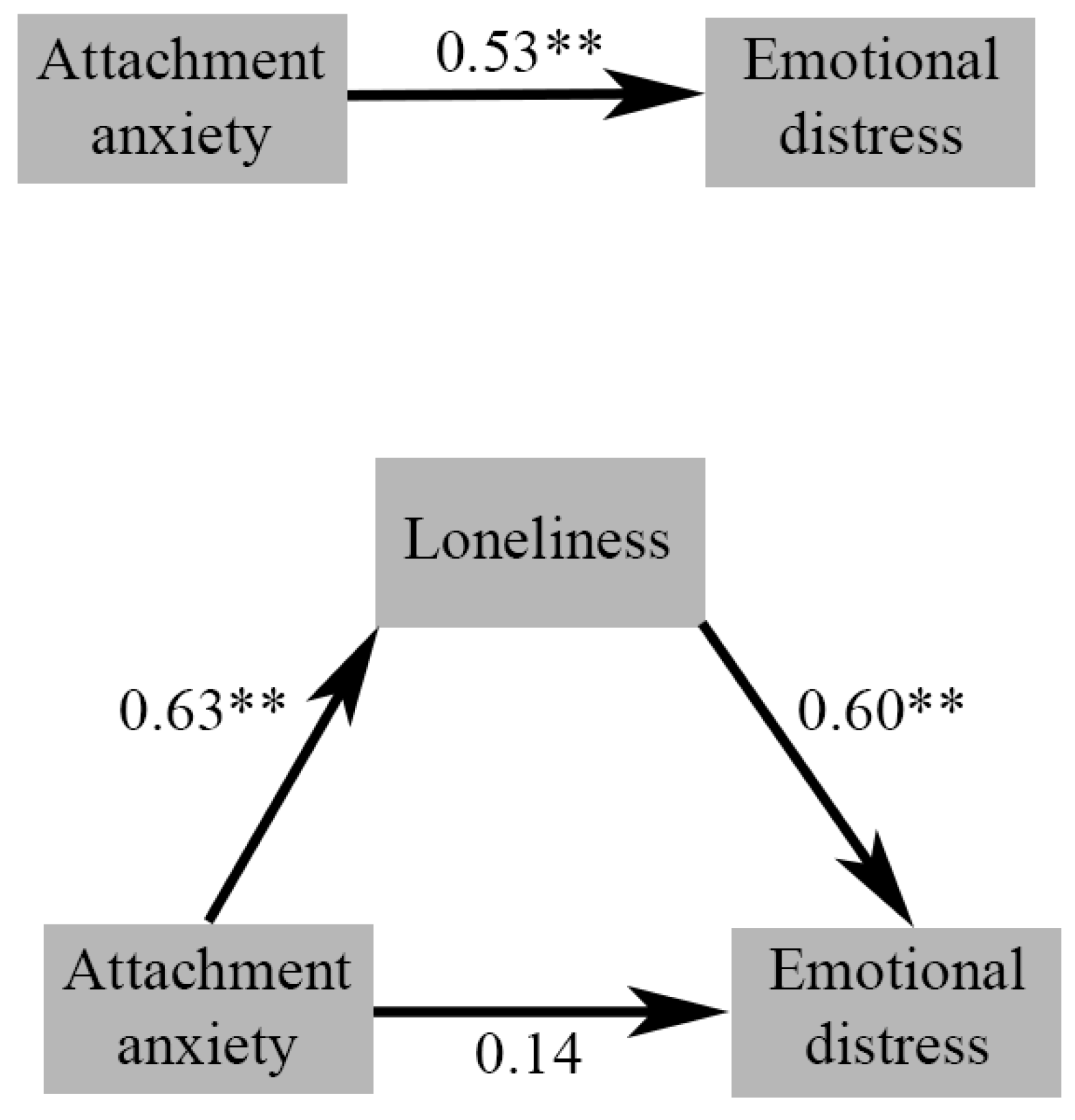
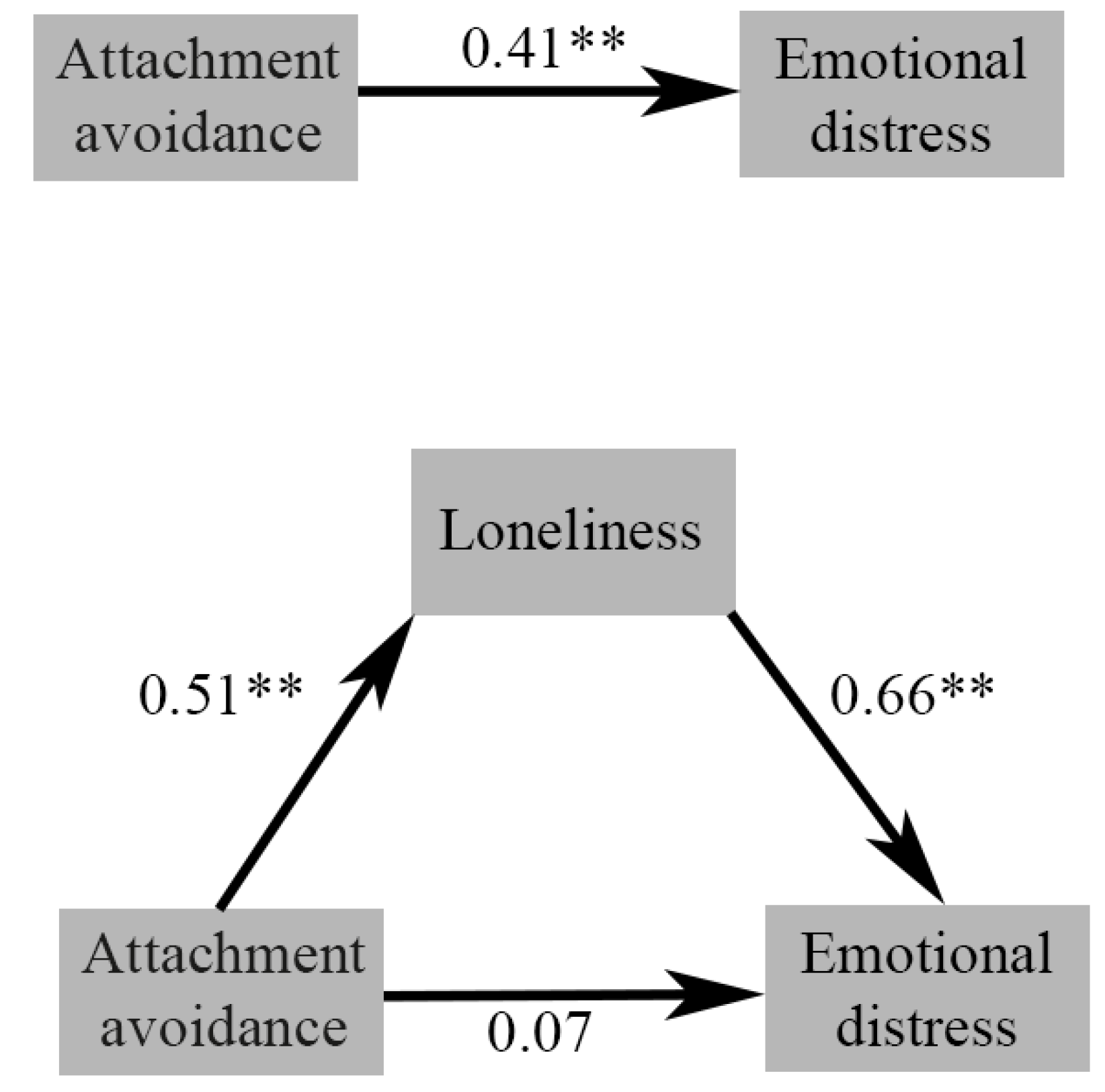
3.4.1. Path 1
3.4.2. Path 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dong, L.; Bouey, J. Public mental health crisis during COVID-19 pandemic, China. Emerg. Infect. Dis. 2020, 26, 1616. [Google Scholar] [CrossRef]
- Dascalu, S.; Geambasu, O.; Valentin Raiu, C.; Azoicai, D.; Damian Popovici, E.; Apetrei, C. COVID-19 in Romania: What went wrong? Front. Public Health 2021, 9, 813941. [Google Scholar] [CrossRef]
- Thorpe, N. COVID: Romania’s Health System Torn Apart by Pandemic. BBC. Available online: https://www.bbc.com/news/world-europe-58992090 (accessed on 23 October 2021).
- Horwitz, A.V. Selecting outcomes for the sociology of mental health: Issues of measurement and dimensionality. J. Health Soc. Behav. 2002, 43, 130. [Google Scholar]
- Drapeau, A.; Marchand, A.; Beaulieu-Prevost, D. Epidemiology of psychological distress. Ment. Illnesses-Underst. Predict. Control. 2012, 69, 105–106. [Google Scholar]
- Wang, Y.; Kala, M.P.; Jafar, T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0244630. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Navarro, R.; Malonda, E.; Llorca-Mestre, A.; Cano-Vindel, A.; Fernández-Berrocal, P. Worry about COVID-19 contagion and general anxiety: Moderation and mediation effects of cognitive emotion regulation. J. Psychiatr. Res. 2021, 137, 311–318. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 1. [Google Scholar] [CrossRef]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.G.; Mukunzi, J.N.; McIntee, S.E.; Dalexis, R.D.; Goulet, M.A.; Labelle, P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef] [PubMed]
- Margetić, B.; Peraica, T.; Stojanović, K.; Ivanec, D. Predictors of emotional distress during the COVID-19 pandemic; a Croatian study. Personal. Individ. Differ. 2021, 175, 110691. [Google Scholar] [CrossRef]
- Sitarz, R.; Forma, A.; Karakuła, K.; Juchnowicz, D.; Baj, J.; Bogucki, J.; Karakuła-Juchnowicz, H. How do polish students manage emotional distress during the COVID-19 lockdown? A web-based cross-sectional study. J. Clin. Med. 2021, 10, 4964. [Google Scholar] [CrossRef]
- Taylor, S. The psychology of pandemics. Annu. Rev. Clin. Psychol. 2022, 18, 581–609. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Nguyen, T.V.T.; Zhong, J.; Liu, J. A COVID-19 descriptive study of life after lockdown in Wuhan, China. R. Soc. Open Sci. 2020, 7, 200705. [Google Scholar] [CrossRef] [PubMed]
- Ernst, M.; Niederer, D.; Werner, A.M.; Czaja, S.J.; Mikton, C.; Ong, A.D.; Rosen, T.; Brähler, E.; Beutel, M.E. Loneliness before and during the COVID-19 pandemic: A systematic review with meta-analysis. Am. Psychol. 2022, 77, 660. [Google Scholar] [CrossRef]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef]
- Perlman, D.; Peplau, L.A. Toward a social psychology of loneliness. Pers. Relatsh. 1981, 3, 31–56. [Google Scholar]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.E.; Braun, B. Loneliness and social isolation-a private problem, a public issue. J. Fam. Consum. Sci. 2019, 111, 7–14. [Google Scholar] [CrossRef]
- Jeste, D.V.; Lee, E.E.; Cacioppo, S. Battling the modern behavioral epidemic of loneliness: Suggestions for research and interventions. JAMA Psychiatry 2020, 77, 553–554. [Google Scholar] [CrossRef]
- Foti, S.A.; Khambaty, T.; Birnbaum-Weitzman, O.; Arguelles, W.; Penedo, F.; Espinoza Giacinto, R.A.; Gutierrez, A.P.; Gallo, L.C.; Giachello, A.L.; Schneiderman, N.; et al. Loneliness, cardiovascular disease, and diabetes prevalence in the hispanic community health study/study of latinos sociocultural ancillary study. J. Immigr. Minor. Health 2020, 22, 345–352. [Google Scholar] [CrossRef]
- Abdellaoui, A.; Sanchez-Roige, S.; Sealock, J.; Treur, J.L.; Dennis, J.; Fontanillas, P.; Elson, S.; 23andMe Research Team; Nivard, M.G.; Ip, H.F. Phenome-wide investigation of health outcomes associated with genetic predisposition to loneliness. Hum. Mol. Genet. 2019, 28, 3853–3865. [Google Scholar] [CrossRef]
- Buchman, A.S.; Boyle, P.A.; Wilson, R.S.; James, B.D.; Leurgans, S.E.; Arnold, S.E.; Bennett, D.A. Loneliness and the rate of motor decline in old age: The rush memory and aging project, a community-based cohort study. BMC Geriatr. 2010, 10, 77. [Google Scholar] [CrossRef]
- Yang, K.; Victor, C. Age and loneliness in 25 European nations. Ageing Soc. 2011, 31, 1368–1388. [Google Scholar] [CrossRef]
- Baarck, J.; d’Hombres, B.; Tintori, G. Loneliness in Europe before and during the COVID-19 pandemic. Health Policy 2022, 126, 1124–1129. [Google Scholar] [CrossRef] [PubMed]
- Bu, F.; Steptoe, A.; Fancourt, D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health 2020, 186, 31–34. [Google Scholar] [CrossRef]
- Palgi, Y.; Shrira, A.; Ring, L.; Bodner, E.; Avidor, S.; Bergman, Y.; Cohen-Fridel, S.; Keisari, S.; Hoffman, Y. The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020, 275, 109–111. [Google Scholar] [CrossRef]
- Ainsworth, M.S.; Bowlby, J. An ethological approach to personality development. Am. Psychol. 1991, 46, 333. [Google Scholar] [CrossRef]
- Shaver, P.; Hazan, C. Being lonely, falling in love. J. Soc. Behav. Personal. 1987, 2, 105. [Google Scholar]
- Larose, S.; Guay, F.; Boivin, M. Attachment, social support, and loneliness in young adulthood: A test of two models. Personal. Soc. Psychol. Bull. 2002, 28, 684–693. [Google Scholar] [CrossRef]
- Mallinckrodt, B. Attachment, social competencies, social support, and interpersonal process in psychotherapy. Psychother. Res. 2000, 10, 239–266. [Google Scholar] [CrossRef]
- Deniz, M.; Hamarta, E.; Ari, R. An investigation of social skills and loneliness levels of university students with respect to their attachment styles in a sample of Turkish students. Soc. Behav. Personal. Int. J. 2005, 33, 19–32. [Google Scholar] [CrossRef]
- Russell, D.; Cutrona, C.E.; Rose, J.; Yurko, K. Social and emotional loneliness: An examination of Weiss’s typology of loneliness. J. Personal. Soc. Psychol. 1984, 46, 1313. [Google Scholar] [CrossRef]
- Margalit, M.; Margalit, M. Loneliness Conceptualization. Lonely Children and Adolescents: Self-Perceptions, Social Exclusion, and Hope; Springer: New York, NY, USA, 2010; pp. 1–28. [Google Scholar]
- Bernardon, S.; Babb, K.A.; Hakim-Larson, J.; Gragg, M. Loneliness, attachment, and the perception and use of social support in university students. Can. J. Behav. Sci. /Rev. Can. Des Sci. Du Comport. 2011, 43, 40. [Google Scholar] [CrossRef]
- Pietromonaco, P.R.; Beck, L.A. Attachment processes in adult romantic relationships. In APA Handbook of Personality and Social Psychology, Volume 3: Interpersonal Relations; American Psychological Association: Washington, DC, USA, 2015; pp. 33–64. [Google Scholar]
- Bowlby, J. Separation, anxiety and anger. In Attachment and Loss; Basic Books: New York, NY, USA, 1973; Volume II, p. 429. [Google Scholar]
- Lewis, K.C.; Roche, M.J.; Brown, F.; Tillman, J.G. Attachment, loneliness, and social connection as prospective predictors of suicidal ideation during the COVID-19 pandemic: A relational diathesis-stress experience sampling study. Suicide Life-Threat. Behav. 2023, 53, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Rollè, L.; Trombetta, T.; Calabrese, C.; Vismara, L.; Sechi, C. Adult attachment, loneliness, COVID-19 risk perception and perceived stress during COVID-19 pandemic. Mediterr. J. Clin. Psychol. 2022, 10. [Google Scholar] [CrossRef]
- Vowels, L.M.; Vowels, M.J.; Carnelley, K.B.; Millings, A.; Gibson-Miller, J. Toward a causal link between attachment styles and mental health during the COVID-19 pandemic. Br. J. Clin. Psychol. 2023, 62, 605–620. [Google Scholar] [CrossRef]
- Lazarus, R.S. Psychological Stress and the Coping Process; McGraw-Hill: New York, NY, USA, 1984. [Google Scholar]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing coping strategies: A theoretically based approach. J. Personal. Soc. Psychol. 1989, 56, 267. [Google Scholar] [CrossRef] [PubMed]
- Park, C.L.; Armeli, S.; Tennen, H. Appraisal-coping goodness of fit: A daily internet study. Personal. Soc. Psychol. Bull. 2004, 30, 558–569. [Google Scholar] [CrossRef] [PubMed]
- Chew, Q.H.; Wei, K.C.; Vasoo, S.; Chua, H.C.; Sim, K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: Practical considerations for the COVID-19 pandemic. Singap. Med. J. 2020, 61, 350. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Havewala, M.; Zhu, Q. COVID-19 stressful life events and mental health: Personality and coping styles as moderators. J. Am. Coll. Health 2022, 1–10. [Google Scholar] [CrossRef]
- Gurvich, C.; Thomas, N.; Thomas, E.H.; Hudaib, A.R.; Sood, L.; Fabiatos, K.; Sutton, K.; Isaacs, A.; Arunogiri, S.; Sharp, G.; et al. Coping styles and mental health in response to societal changes during the COVID-19 pandemic. Int. J. Soc. Psychiatry 2021, 67, 540–549. [Google Scholar] [CrossRef] [PubMed]
- Garbóczy, S.; Szemán-Nagy, A.; Ahmad, M.S.; Harsányi, S.; Ocsenás, D.; Rekenyi, V.; Al-Tammemi, A.A.; Kolozsvári, L.R. Health anxiety, perceived stress, and coping styles in the shadow of the COVID-19. BMC Psychol. 2021, 9, 53. [Google Scholar] [CrossRef]
- Ciuhan, G.C.; Nicolau, R.G.; Iliescu, D. Perceived stress and wellbeing in Romanian teachers during the COVID-19 pandemic: The intervening effects of job crafting and problem-focused coping. Psychol. Sch. 2022, 59, 1844–1855. [Google Scholar] [CrossRef]
- Ding, Y.; Fu, X.; Liu, R.; Hwang, J.; Hong, W.; Wang, J. The impact of different coping styles on psychological distress during the COVID-19: The mediating role of perceived stress. Int. J. Environ. Res. Public Health 2021, 18, 10947. [Google Scholar] [CrossRef]
- Fluharty, M.; Bu, F.; Steptoe, A.; Fancourt, D. Coping strategies and mental health trajectories during the first 21 weeks of COVID-19 lockdown in the United Kingdom. Soc. Sci. Med. 2021, 279, 113958. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Russell, D.W. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J. Personal. Assess. 1996, 66, 20–40. [Google Scholar] [CrossRef]
- Collins, N.L. Revised adult attachment scale. In Behavior Therapy; American Psychological Association: Washington, DC, USA, 1996. [Google Scholar]
- Carver, C.S. You want to measure coping but your protocol’too long: Consider the brief cope. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Wong, T.W.; Yau, J.K.; Chan, C.L.; Kwong, R.S.; Ho, S.M.; Lau, C.C.; Lau, F.L.; Lit, C.H. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur. J. Emerg. Med. 2005, 12, 13–18. [Google Scholar] [CrossRef]
- Crasovan, D.I.; Sava, F.A. Translation, adaptation, and validation on Romanian population of COPE questionnaire for coping mechanisms analysis. Cogn. Brain Behav. 2013, 17, 61. [Google Scholar]
- Bose, C.N.; Bjorling, G.; Elfstrom, M.L.; Persson, H.; Saboonchi, F. Assessment of coping strategies and their associations with health related quality of life in patients with chronic heart failure: The Brief COPE restructured. Cardiol. Res. 2015, 6, 239. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Fritz, M.S.; MacKinnon, D.P. Required sample size to detect the mediated effect. Psychol. Sci. 2007, 18, 233–239. [Google Scholar] [CrossRef]
- Hayes, A.F.; Cai, L. Using heteroskedasticity-consistent standard error estimators in OLS regression: An introduction and software implementation. Behav. Res. Methods 2007, 39, 709–722. [Google Scholar] [CrossRef]
- Andersen, R. Modern methods for robust regression. In Quantitative Applications in the Social Sciences; Sage: Thousand Oaks, CA, USA, 2008; Volume 12. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford publications: New York, NY, USA, 2017. [Google Scholar]
- Pieh, C.; O’ Rourke, T.; Budimir, S.; Probst, T. Relationship quality and mental health during COVID-19 lockdown. PLoS ONE 2020, 15, e0238906. [Google Scholar] [CrossRef]
- Zaidi, A.; Ali, A.Z. Living under the shadow of a pandemic: The psychological challenges underlying social distancing and awareness raising. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 508. [Google Scholar] [CrossRef]
- Prati, G.; Mancini, A.D. Social and behavioral consequences of the COVID-19 pandemic: Validation of a Pandemic Disengagement Syndrome Scale (PDSS) in four national contexts. Psychol. Assess. 2023. [Google Scholar] [CrossRef]
- Kauhanen, L.; Wan Mohd Yunus, W.M.; Lempinen, L.; Peltonen, K.; Gyllenberg, D.; Mishina, K.; Gilbert, S.; Bastola, K.; Brown, J.S.; Sourander, A. A systematic review of the mental health changes of children and young people before and during the COVID-19 pandemic. Eur. Child Adolesc. Psychiatry 2023, 32, 995–1013. [Google Scholar] [CrossRef] [PubMed]
- Na, L.; Yang, L.; Mezo, P.G.; Liu, R. Age disparities in mental health during the COVID19 pandemic: The roles of resilience and coping. Soc. Sci. Med. 2022, 305, 115031. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry 2021, 218, 326–333. [Google Scholar]
- Okely, J.A.; Corley, J.; Welstead, M.; Taylor, A.M.; Page, D.; Skarabela, B.; Redmond, P.; Cox, S.R.; Russ, T.C. Change in physical activity, sleep quality, and psychosocial variables during COVID-19 lockdown: Evidence from the Lothian Birth Cohort 1936. Int. J. Environ. Res. Public Health 2021, 18, 210. [Google Scholar] [CrossRef] [PubMed]
- Shaver, P.R.; Mikulincer, M. An overview of adult attachment theory. In Attachment Theory and Research in Clinical Work with Adults; The Guilford Press: New York, NY, USA, 2009; pp. 17–45. [Google Scholar]
- Turton, H.; Berry, K.; Danquah, A.; Green, J.; Pratt, D. An investigation of whether emotion regulation mediates the relationship between attachment insecurity and suicidal ideation and behaviour. Clin. Psychol. Psychother. 2022, 29, 1587–1598. [Google Scholar] [CrossRef] [PubMed]
- Davila, J.; Burge, D.; Hammen, C. Why does attachment style change? J. Personal. Soc. Psychol. 1997, 73, 826. [Google Scholar] [CrossRef]
- Thompson, R.A.; Simpson, J.A.; Berlin, L.J. Taking perspective on attachment theory and research: Nine fundamental questions. Attach. Hum. Dev. 2022, 24, 543–560. [Google Scholar] [CrossRef]
- Pinquart, M.; Feußner, C.; Ahnert, L. Meta-analytic evidence for stability in attachments from infancy to early adulthood. Attach. Hum. Dev. 2013, 15, 189–218. [Google Scholar] [CrossRef] [PubMed]
- Bakermans-Kranenburg, M.J.; Van Ijzendoorn, M.H. No reliable gender differences in attachment across the lifespan. Behav. Brain Sci. 2009, 32, 22–23. [Google Scholar] [CrossRef]
- Hasson-Ohayon, I.; Goldzweig, G.; Sela-Oren, T.; Pizem, N.; Bar-Sela, G.; Wolf, I. Attachment style, social support and finding meaning among spouses of colorectal cancer patients: Gender differences. Palliat. Support. Care 2015, 13, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Beutel, M.E.; Hettich, N.; Ernst, M.; Schmutzer, G.; Tibubos, A.N.; Braehler, E. Mental health and loneliness in the German general population during the COVID-19 pandemic compared to a representative pre-pandemic assessment. Sci. Rep. 2021, 11, 14946. [Google Scholar] [CrossRef] [PubMed]
- Fernández, R.S.; Crivelli, L.; Guimet, N.M.; Allegri, R.F.; Pedreira, M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. J. Affect. Disord. 2020, 277, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Shaver, P.R.; Mikulincer, M.; Sahdra, B.; Gross, J. Attachment security as a foundation for kindness toward self and others. In The Oxford Handbook of Hypo-Egoic Phenomena; Oxford University Press: Oxford, UK, 2016; p. 10. [Google Scholar]
- Powers, S.I.; Pietromonaco, P.R.; Gunlicks, M.; Sayer, A. Dating couples’ attachment styles and patterns of cortisol reactivity and recovery in response to a relationship conflict. J. Personal. Soc. Psychol. 2006, 90, 613. [Google Scholar] [CrossRef]
- Diamond, L.M.; Fagundes, C.P. Psychobiological research on attachment. J. Soc. Pers. Relatsh. 2010, 27, 218–225. [Google Scholar] [CrossRef]
- Carter, C.S. Neuroendocrine perspectives on social attachment and love. Psychoneuroendocrinology 1998, 23, 779–818. [Google Scholar] [CrossRef] [PubMed]
- Pietromonaco, P.R.; Beck, L.A. Adult attachment and physical health. Curr. Opin. Psychol. 2019, 25, 115–120. [Google Scholar] [CrossRef]
- Mikulincer, M.; Shaver, P.R. The attachment behavioral system in adulthood: Activation, psychodynamics, and interpersonal processes. Adv. Exp. Soc. Psychol. 2003, 35, 56–152. [Google Scholar]
- Lopez, F.G.; Brennan, K.A. Dynamic processes underlying adult attachment organization: Toward an attachment theoretical perspective on the healthy and effective self. J. Couns. Psychol. 2000, 47, 283. [Google Scholar] [CrossRef]
- Green, J.; Berry, K.; Danquah, A.; Pratt, D. The role of psychological and social factors in the relationship between attachment and suicide: A systematic review. Clin. Psychol. Psychother. 2020, 27, 463–488. [Google Scholar] [CrossRef]
- Levi-Belz, Y.; Gvion, Y.; Horesh, N.; Apter, A. Attachment patterns in medically serious suicide attempts: The mediating role of self-disclosure and loneliness. Suicide Life-Threat. Behav. 2013, 43, 511–522. [Google Scholar] [CrossRef] [PubMed]
- Campbell, L.; Marshall, T. Anxious attachment and relationship processes: An interactionist perspective. J. Personal. 2011, 79, 1219–1250. [Google Scholar] [CrossRef] [PubMed]
- Marazziti, D.; Dell’Osso, B.; Dell’Osso, M.C.; Consoli, G.; Del Debbio, A.; Mungai, F.; Vivarelli, L.; Albanese, F.; Piccinni, A.; Rucci, P.; et al. Romantic attachment in patients with mood and anxiety disorders. CNS Spectr. 2007, 12, 751–756. [Google Scholar] [CrossRef]
- Eng, W.; Heimberg, R.G.; Hart, T.A.; Schneier, F.R.; Liebowitz, M.R. Attachment in individuals with social anxiety disorder: The relationship among adult attachment styles, social anxiety, and depression. Emotion 2001, 1, 365. [Google Scholar] [CrossRef]
- Woodhouse, S.; Ayers, S.; Field, A.P. The relationship between adult attachment style and post-traumatic stress symptoms: A meta-analysis. J. Anxiety Disord. 2015, 35, 103–117. [Google Scholar] [CrossRef]
- Ostacoli, L.; Cosma, S.; Bevilacqua, F.; Berchialla, P.; Bovetti, M.; Carosso, A.R.; Malandrone, F.; Carletto, S.; Benedetto, C. Psychosocial factors associated with postpartum psychological distress during the COVID-19 pandemic: A cross-sectional study. BMC Pregnancy Childbirth 2020, 20, 703. [Google Scholar] [CrossRef] [PubMed]
- Warfa, N.; Harper, M.; Nicolais, G.; Bhui, K. Adult attachment style as a risk factor for maternal postnatal depression: A systematic review. BMC Psychol. 2014, 2, 56. [Google Scholar] [CrossRef] [PubMed]
- Shaver, P.R.; Schachner, D.A.; Mikulincer, M. Attachment style, excessive reassurance seeking, relationship processes, and depression. Personal. Soc. Psychol. Bull. 2005, 31, 343–359. [Google Scholar] [CrossRef]
- Vowels, L.M.; Carnelley, K.B. Attachment styles, negotiation of goal conflict, and perceived partner support during COVID-19. Personal. Individ. Differ. 2021, 171, 110505. [Google Scholar] [CrossRef]
- Grunebaum, M.F.; Galfalvy, H.C.; Mortenson, L.Y.; Burke, A.K.; Oquendo, M.A.; Mann, J.J. Attachment and social adjustment: Relationships to suicide attempt and major depressive episode in a prospective study. J. Affect. Disord. 2020, 123, 123–130. [Google Scholar] [CrossRef]
- Bartholomew, K.; Horowitz, L.M. Attachment styles among young adults: A test of a four-category model. J. Personal. Soc. Psychol. 1991, 61, 226. [Google Scholar] [CrossRef]
- Main, M.; Solomon, J. Procedures for identifying infants as disorganized/disoriented during the Ainsworth Strange Situation. Attach. Presch. Years Theory Res. Interv. 1990, 1, 121–160. [Google Scholar]
- Briere, J.; Runtz, M.; Eadie, E.M.; Bigras, N.; Godbout, N. The Disorganized Response Scale: Construct validity of a potential self-report measure of disorganized attachment. Psychol. Trauma Theory Res. Pract. Policy 2019, 11, 486. [Google Scholar] [CrossRef] [PubMed]
- Paetzold, R.L.; Rholes, W.S.; Kohn, J.L. Disorganized attachment in adulthood: Theory, measurement, and implications for romantic relationships. Rev. Gen. Psychol. 2015, 19, 146–156. [Google Scholar] [CrossRef]
- Beeney, J.E.; Wright, A.G.; Stepp, S.D.; Hallquist, M.N.; Lazarus, S.A.; Beeney, J.R.; Scott, L.N.; Pilkonis, P.A. Disorganized attachment and personality functioning in adults: A latent class analysis. Personal. Disord. Theory Res. Treat. 2017, 8, 206. [Google Scholar] [CrossRef] [PubMed]
- Dumont, M.; Provost, M.A. Resilience in adolescents: Protective role of social support, coping strategies, self-esteem, and social activities on experience of stress and depression. J. Youth Adolesc. 1999, 28, 343–363. [Google Scholar] [CrossRef]
- Folkman, S.; Lazarus, R.S. Coping and emotion. In Stress and Coping: An Anthology; Columbia University Press: New York, NY, USA, 1991; pp. 207–227. [Google Scholar]
- Rettie, H.; Daniels, J. Coping and tolerance of uncertainty: Predictors and mediators of mental health during the COVID-19 pandemic. Am. Psychol. 2021, 76, 427. [Google Scholar] [CrossRef] [PubMed]
- Edjolo, A.; Dorey, J.M.; Herrmann, M.; Perrot, C.; Lebrun-Givois, C.; Buisson, A.; El Haouari, H.; Laurent, B.; Pongan, E.; Rouch, I. Stress, personality, attachment, and coping strategies during the COVID-19 pandemic: The STERACOVID prospective cohort study protocol. Front. Psychiatry 2022, 13, 918428. [Google Scholar] [CrossRef] [PubMed]
| Male (N = 30) | Female (N = 111) | t-Test | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p | |
| Age | 35.22 | 10.80 | 35.03 | 10.23 | 0.00 |
| Loneliness | 21 | 13.69 | 22.81 | 13.32 | 0.513 |
| Emotional distress | 17.9 | 13.40 | 17.89 | 12.86 | 0.998 |
| Attachment anxiety | 13.43 | 5.32 | 14.18 | 6.59 | 0.568 |
| Attachment avoidance | 33.56 | 7.36 | 33.06 | 8.74 | 0.773 |
| Problem-focused | 8.06 | 4.05 | 10.23 | 4.35 | 0.015 |
| Emotion-focused | 33.33 | 14.94 | 41.08 | 14.31 | 0.001 |
| Avoidant | 22.50 | 9.21 | 27.37 | 10.61 | 0.023 |
| Socially supported | 15.50 | 7.47 | 19.43 | 9.94 | 0.046 |
| N = 141 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | - | ||||||||
| 2. Loneliness | −0.13 | - | |||||||
| 3. Emotional distress | −0.20 * | 0.70 *** | - | ||||||
| 4. Attachment anxiety | −0.19 * | 0.63 *** | 0.53 *** | - | |||||
| 5. Attachment avoidance | −0.15 | 0.51 *** | 0.41 *** | 0.61 *** | - | ||||
| 6. Problem-focused coping | −0.17 * | 0.21 * | 0.24 ** | 0.05 | 0.11 | - | |||
| 7. Avoidant coping | −0.22 ** | 0.10 | 0.22 | 0.16 | −0.03 | 0.47 *** | - | ||
| 8. Emotion-focused coping | −17 * | 0.08 | 0.13 | 0.17 | 0.00 | 0.73 *** | 0.71 *** | - | |
| 9. Socially supported coping | −0.00 | 0.20 * | 0.26 ** | −0.02 | 0.09 | 0.42 *** | 0.69 *** | 0.62 *** | - |
| Loneliness R.sq = 0.42, p < 0.001 | Emotional Distress R.sq = 0.30, p < 0.001 | |||||
|---|---|---|---|---|---|---|
| β | T | p | β | T | p | |
| Attachment anxiety | 0.503 | 6.13 | 0.000 | 0.428 | 4.71 | 0.000 |
| Attachment avoidance | 0.205 | 2.46 | 0.015 | 0.142 | 1.59 | 0.113 |
| Age | −0.005 | −0.08 | 0.935 | −0.102 | −1.41 | 0.160 |
| Gender | −0.036 | −0.55 | 0.57 | 0.017 | 0.23 | 0.81 |
| Loneliness R.sq = 0.11, p < 0.01 | Emotional distress R.sq = 0.18, p < 0.001 | |||||
|---|---|---|---|---|---|---|
| β | T | p | β | T | p | |
| Problem-focused | 0.335 | 2.75 | 0.007 | 0.313 | 2.69 | 0.008 |
| Emotion-focused | −0.382 | −2.47 | 0.015 | −0.253 | −1.70 | 0.083 |
| Avoidant | 0.014 | 0.10 | 0.915 | −0.231 | −1.78 | 0.070 |
| Socially supported | 0.286 | 2.37 | 0.019 | 0.454 | 3.93 | 0.000 |
| Age | −0.136 | −1.57 | 0.117 | −0.24 | −2.96 | 0.003 |
| Gender | −0.020 | −0.23 | 0.81 | 0.04 | 0.50 | 0.61 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hopulele-Petri, A.; Fadgyas-Stănculete, M.; Manea, M. Attachment and Coping in the Second Pandemic Year: The Impact on Loneliness and Emotional Distress. COVID 2023, 3, 1322-1335. https://doi.org/10.3390/covid3090092
Hopulele-Petri A, Fadgyas-Stănculete M, Manea M. Attachment and Coping in the Second Pandemic Year: The Impact on Loneliness and Emotional Distress. COVID. 2023; 3(9):1322-1335. https://doi.org/10.3390/covid3090092
Chicago/Turabian StyleHopulele-Petri, Andrei, Mihaela Fadgyas-Stănculete, and Mirela Manea. 2023. "Attachment and Coping in the Second Pandemic Year: The Impact on Loneliness and Emotional Distress" COVID 3, no. 9: 1322-1335. https://doi.org/10.3390/covid3090092
APA StyleHopulele-Petri, A., Fadgyas-Stănculete, M., & Manea, M. (2023). Attachment and Coping in the Second Pandemic Year: The Impact on Loneliness and Emotional Distress. COVID, 3(9), 1322-1335. https://doi.org/10.3390/covid3090092






