Research Staff COVID-19 Pandemic Survey-Results from the Prevention and Early Treatment of Acute Lung Injury (PETAL) Network
Abstract
:1. Introduction
2. Materials and Methods
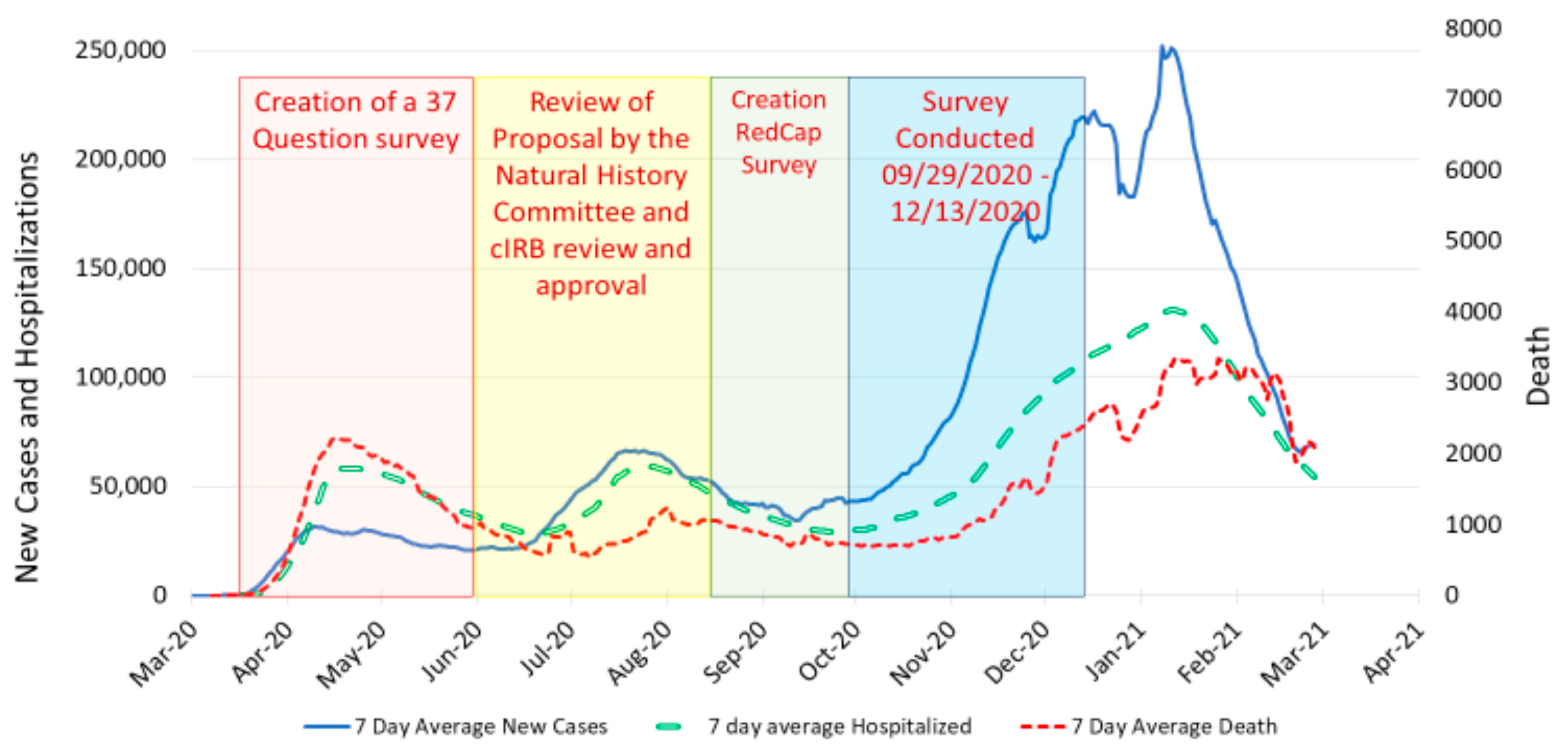
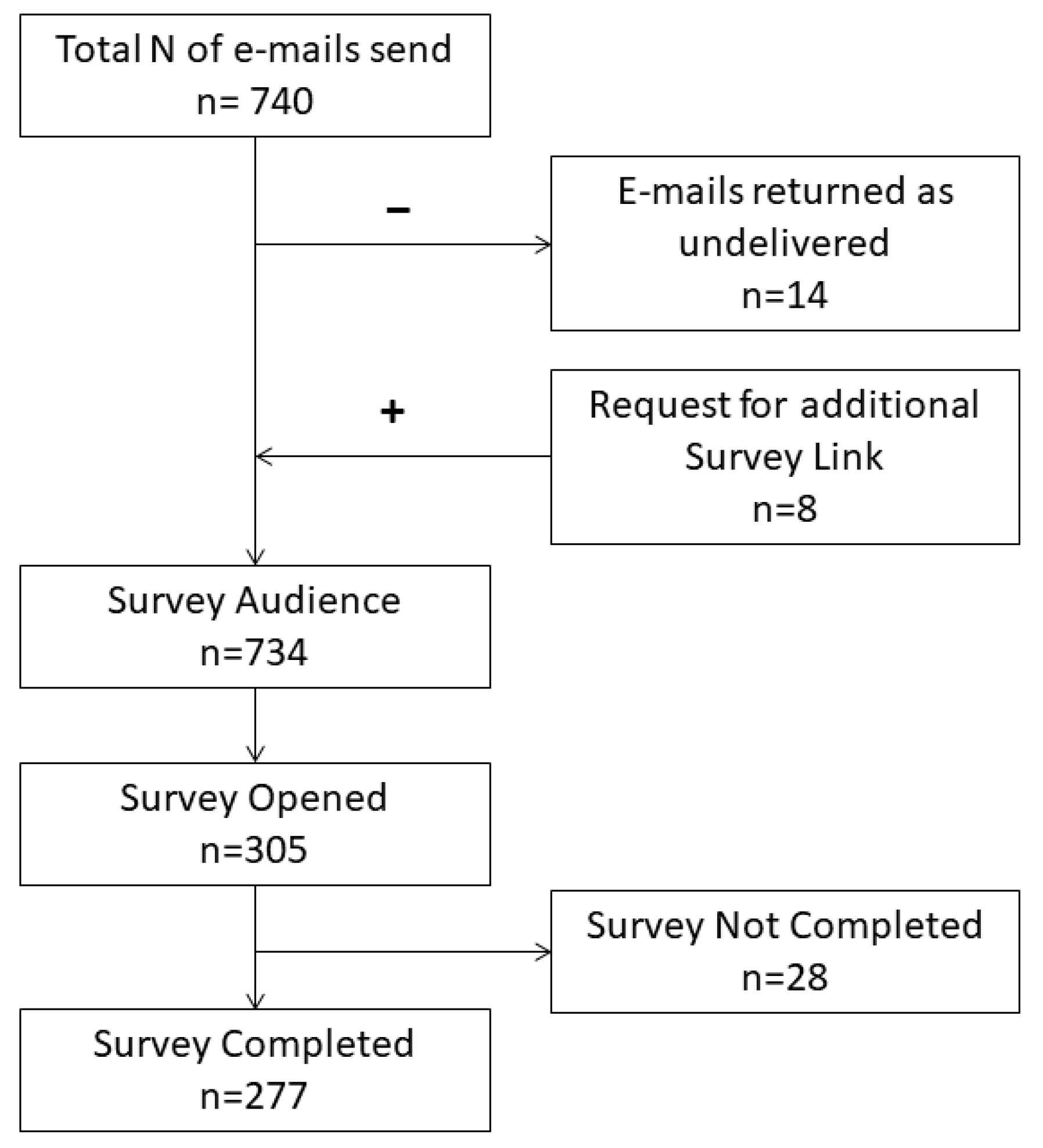
2.1. Study Design
2.2. Statistical Analysis
3. Results
3.1. Demographics
3.2. COVID-19 Impact on Research
3.3. Medical Supplies
3.4. Infection and Safety
4. Discussion
4.1. Limitations
4.2. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Del Rio, C.; Malani, P.N. COVID-19-new insights on a rapidly changing epidemic. JAMA 2020, 323, 1339–1340. [Google Scholar] [CrossRef] [PubMed]
- Fauci, A.S.; Lane, H.C.; Redfield, R.R. COVID-19—Navigating the uncharted. N. Engl. J. Med. 2020, 382, 1268–1269. [Google Scholar] [CrossRef] [PubMed]
- Mathews, K.S.; Seitz, K.P.; Vranas, K.C.; Duggal, A.; Valley, T.S.; Zhao, B.; Gundel, S.; Harhay, M.O.; Chang, S.Y.; Hough, C.L.; et al. Variation in initial U.S. hospital responses to the Coronavirus Disease 2019 pandemic. Crit. Care Med. 2021, 49, 1038–1048. [Google Scholar] [CrossRef]
- World Health Organization. Getting Your Workplace Ready for COVID-19: How COVID-19 Spreads, 19 March 2020. Available online: https://apps.who.int/iris/handle/10665/331584 (accessed on 18 January 2022).
- Centers for Disease Control and Prevention. Guidance for Businesses and Employers Responding to Coronavirus Disease 2019 (COVID-19). Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-business-response.html (accessed on 18 January 2022).
- Centers for Disease Control and Prevention. Public Health Activity Guidance. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-covid-19-client-interaction.html (accessed on 18 January 2022).
- Moreland, A.; Herlihy, C.; Tynan, M.A.; Sunshine, G.; McCord, R.F.; Hilton, C.; Poovey, J.; Werner, A.K.; Jones, C.D.; Fulmer, E.B.; et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement—United States, March 1–May 31, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1198–1203. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Coronavirus(COVID-19) Statistics. Available online: https://www.bing.com/search?q=current+covid+-19+cases&form=ANNH02&refig=6dc3717b75ef48538f05e3682749da47 (accessed on 16 January 2022).
- Abati, E.; Nelva Stellio, L.; Manini, A.; Moroni, F.; Azzalini, L.; Vilca, L.M. A cross-sectional survey study of the impact of COVID-19 pandemic on the training and quality of life of Italian medical residents in the Lombardy region. Ann. Med. 2022, 54, 2326–2339. [Google Scholar] [CrossRef]
- Goldman, C.; Pradere, B.; Mete, M.; Talso, M.; Bernardino, R.; Campi, R.; Marchalik, D. A Multinational Study of The Impact of COVID-19 On Urologic Surgery Residency and Wellbeing. Urology 2022, 166, 87–94. [Google Scholar] [CrossRef]
- Khan, R.; Tandon, P.; Scaffidi, M.A.; Bishay, K.; Pawlak, K.M.; Kral, J.; Amin, S.; Bilal, M.; Lui, R.N.; Sandhu, D.S.; et al. COVID-19 and Canadian Gastroenterology Trainees. J. Can. Assoc. Gastroenterol. 2021, 4, 156–162. [Google Scholar] [CrossRef]
- Sathian, B.; Asim, M.; Banerjee, I.; Pizarro, A.B.; Roy, B.; van Teijlingen, E.R.; do Nascimento, I.J.B.; Alhamad, H.K. Impact of COVID-19 on clinical trials and clinical research: A systematic review. Nepal. J. Epidemiol. 2020, 10, 878–887. [Google Scholar] [CrossRef]
- Sarah, K.; Oceane, S.; Emily, F.; Carole, F. Learning from lockdown—Assessing the positive and negative experiences, and coping strategies of researchers during the COVID-19 pandemic. Appl. Anim. Behav. Sci. 2021, 236, 105269. [Google Scholar] [CrossRef]
- Dhont, J.; Di Tella, M.; Dubois, L.; Aznar, M.; Petit, S.; Spalek, M.; Boldrini, L.; Franco, P.; Bertholet, J. Conducting research in radiation oncology remotely during the COVID-19 pandemic: Coping with isolation. Clin. Transl. Radiat. Oncol. 2020, 24, 53–59. [Google Scholar] [CrossRef]
- Guintivano, J.; Dick, D.; Bulik, C.M. Psychiatric genomics research during the COVID-19 pandemic: A survey of Psychiatric Genomics Consortium researchers. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2021, 186, 40–49. [Google Scholar] [CrossRef]
- Gilmartin, H.M.; Connelly, B.; Hebbe, A.; Battaglia, C.; Kwan, B.M. Assessing the impact of remote work during COVID-19 on clinical and translational scientists and staff in Colorado. J. Clin. Transl. Sci. 2020, 5, e71. [Google Scholar] [CrossRef] [PubMed]
- Bratan, T.; Aichinger, H.; Brkic, N.; Rueter, J.; Apfelbacher, C.; Boyer, L.; Loss, J. Impact of the COVID-19 pandemic on ongoing health research: An ad hoc survey among investigators in Germany. BMJ Open 2021, 11, e049086. [Google Scholar] [CrossRef] [PubMed]
- Gerber, D.E.; Sheffield, T.Y.; Beg, M.S.; Williams, E.L.; Clark, V.L.; Xie, Y.; Holbein, M.E.B.; Skinner, C.S.; Lee, S.J.C. Experience, perceptions, and recommendations concerning COVID-19-related clinical research adjustments. J. Natl. Compr. Canc. Netw. 2021, 19, 505–512. [Google Scholar] [CrossRef] [PubMed]
- The PETAL Network. Available online: https://petalnet.org/general-public (accessed on 9 January 2023).
- National Heart, L.; Blood Institute, P.C.T.N.; Moss, M.; Huang, D.T.; Brower, R.G.; Ferguson, N.D.; Ginde, A.A.; Gong, M.N.; Grissom, C.K.; Gundel, S.; et al. Early Neuromuscular Blockade in the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2019, 380, 1997–2008. [Google Scholar] [CrossRef]
- National Heart, L.; Blood Institute, P.C.T.N.; Ginde, A.A.; Brower, R.G.; Caterino, J.M.; Finck, L.; Banner-Goodspeed, V.M.; Grissom, C.K.; Hayden, D.; Hough, C.L.; et al. Early High-Dose Vitamin D3 for Critically Ill, Vitamin D-Deficient Patients. N. Engl. J. Med. 2019, 381, 2529–2540. [Google Scholar] [CrossRef]
- Casey, J.D.; Johnson, N.J.; Semler, M.W.; Collins, S.P.; Aggarwal, N.R.; Brower, R.G.; Chang, S.Y.; Eppensteiner, J.; Filbin, M.; Gibbs, K.W.; et al. Rationale and Design of ORCHID: A Randomized Placebo-controlled Clinical Trial of Hydroxychloroquine for Adults Hospitalized with COVID-19. Ann. Am. Thorac. Soc. 2020, 17, 1144–1153. [Google Scholar] [CrossRef]
- Self, W.H.; Semler, M.W.; Leither, L.M.; Casey, J.D.; Angus, D.C.; Brower, R.G.; Chang, S.Y.; Collins, S.P.; Eppensteiner, J.C.; Filbin, M.R.; et al. Effect of hydroxychloroquine on clinical status at 14 days in hospitalized patients with COVID-19: A randomized clinical trial. JAMA 2020, 324, 2165–2176. [Google Scholar] [CrossRef]
- Peltan, I.D.; Caldwell, E.; Admon, A.J.; Attia, E.F.; Gundel, S.J.; Mathews, K.S.; Nagrebetsky, A.; Sahetya, S.K.; Ulysse, C.; Brown, S.M.; et al. Characteristics and outcomes of US patients hospitalized with COVID-19. Am. J. Crit. Care 2022, 31, 146–157. [Google Scholar] [CrossRef]
- ACTIV-3/Therapeutics for Inpatients with COVID-19 Study Group. Efficacy and safety of two neutralising monoclonal antibody therapies, sotrovimab and BRII-196 plus BRII-198, for adults hospitalised with COVID-19 (TICO): A randomised controlled trial. Lancet Infect. Dis. 2022, 22, 622–635. [Google Scholar] [CrossRef]
- ACTIV-3/TICO LY-CoV555 Study Group; Lundgren, J.D.; Grund, B.; Barkauskas, C.E.; Holland, T.L.; Gottlieb, R.L.; Sandkovsky, U.; Brown, S.M.; Knowlton, K.U.; Self, W.H.; et al. A neutralizing monoclonal antibody for hospitalized patients with COVID-19. N. Engl. J. Med. 2021, 384, 905–914. [Google Scholar] [CrossRef]
- Group, A.-T.B.S.; Lundgren, J.D.; Grund, B.; Barkauskas, C.E.; Holland, T.L.; Gottlieb, R.L.; Sandkovsky, U.; Brown, S.M.; Knowlton, K.U.; Self, W.H.; et al. Responses to a Neutralizing Monoclonal Antibody for Hospitalized Patients With COVID-19 According to Baseline Antibody and Antigen Levels: A Randomized Controlled Trial. Ann. Intern. Med. 2022, 175, 234–243. [Google Scholar] [CrossRef]
- Group, A.-T.S.; Barkauskas, C.; Mylonakis, E.; Poulakou, G.; Young, B.E.; Vock, D.M.; Siegel, L.; Engen, N.; Grandits, G.; Mosaly, N.R.; et al. Efficacy and Safety of Ensovibep for Adults Hospitalized With COVID-19: A Randomized Controlled Trial. Ann. Intern. Med. 2022, 175, 1266–1274. [Google Scholar] [CrossRef]
- Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV). Available online: https://www.nih.gov/research-training/medical-research-initiatives/activ (accessed on 9 January 2023).
- Self, W.H.; Semler, M.W.; Bellomo, R.; Brown, S.M.; deBoisblanc, B.P.; Exline, M.C.; Ginde, A.A.; Grissom, C.K.; Janz, D.R.; Jones, A.E.; et al. Liberal Versus Restrictive Intravenous Fluid Therapy for Early Septic Shock: Rationale for a Randomized Trial. Ann. Emerg. Med. 2018, 72, 457–466. [Google Scholar] [CrossRef] [PubMed]
- National Heart, Lung, and Blood Institute Prevention and Early Treatment of Acute Lung Injury Clinical Trials Network; Shapiro, N.I.; Douglas, I.S.; Brower, R.G.; Brown, S.M.; Exline, M.C.; Ginde, A.A.; Gong, M.N.; Grissom, C.K.; Hayden, D.; et al. Early Restrictive or Liberal Fluid Management for Sepsis-Induced Hypotension. N. Engl. J. Med. 2023, 388, 499–510. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.T.; Angus, D.C.; Moss, M.; Thompson, B.T.; Ferguson, N.D.; Ginde, A.; Gong, M.N.; Gundel, S.; Hayden, D.L.; Hite, R.D.; et al. Design and rationale of the reevaluation of systemic early neuromuscular blockade trial for acute respiratory distress syndrome. Ann. Am. Thorac. Soc. 2017, 14, 124–133. [Google Scholar] [CrossRef]
- Prevention and Early Treatment of Acute Lung Injury Network. The PETAL Network. Available online: https://petalnet.org/locations (accessed on 4 February 2023).
- Rothwell, E.; Brassil, D.; Barton-Baxter, M.; Brownley, K.A.; Dickert, N.W.; Ford, D.E.; Kraft, S.A.; McCormick, J.B.; Wilfond, B.S. Informed consent: Old and new challenges in the context of the COVID-19 pandemic. J. Clin. Transl. Sci. 2021, 5, e105. [Google Scholar] [CrossRef]
- Gomez-Ochoa, S.A.; Franco, O.H.; Rojas, L.Z.; Raguindin, P.F.; Roa-Diaz, Z.M.; Wyssmann, B.M.; Guevara, S.L.R.; Echeverria, L.E.; Glisic, M.; Muka, T. COVID-19 in health-care workers: A living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am. J. Epidemiol. 2021, 190, 161–175. [Google Scholar] [CrossRef]
- Alshamrani, M.M.; El-Saed, A.; Al Zunitan, M.; Almulhem, R.; Almohrij, S. Risk of COVID-19 morbidity and mortality among healthcare workers working in a large tertiary care hospital. Int. J. Infect. Dis. 2021, 109, 238–243. [Google Scholar] [CrossRef]
- Bandyopadhyay, S.; Baticulon, R.E.; Kadhum, M.; Alser, M.; Ojuka, D.K.; Badereddin, Y.; Kamath, A.; Parepalli, S.A.; Brown, G.; Iharchane, S.; et al. Infection and mortality of healthcare workers worldwide from COVID-19: A systematic review. BMJ Glob. Health 2020, 5, e003097. [Google Scholar] [CrossRef]
- World Health Organization. Health and Care Worker Deaths during COVID-19. Available online: https://www.who.int/news/item/20-10-2021-health-and-care-worker-deaths-during-covid-19 (accessed on 4 February 2023).
- Leo, C.G.; Sabina, S.; Tumolo, M.R.; Bodini, A.; Ponzini, G.; Sabato, E.; Mincarone, P. Burnout among healthcare workers in the COVID 19 era: A review of the existing literature. Front. Public Health 2021, 9, 750529. [Google Scholar] [CrossRef] [PubMed]
- Alsulimani, L.K.; Farhat, A.M.; Borah, R.A.; AlKhalifah, J.A.; Alyaseen, S.M.; Alghamdi, S.M.; Bajnaid, M.J. Health care worker burnout during the COVID-19 pandemic: A cross-sectional survey study in Saudi Arabia. Saudi Med. J. 2021, 42, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Iwashyna, T.J.; Kamphuis, L.A.; Gundel, S.J.; Hope, A.A.; Jolley, S.; Admon, A.J.; Caldwell, E.; Monahan, M.L.; Hauschildt, K.; Thompson, B.T.; et al. Continuing cardiopulmonary symptoms, disability, and financial toxicity 1 month after hospitalization for third-wave COVID-19: Early results from a US nationwide cohort. J. Hosp. Med. 2021, 16, 531–537. [Google Scholar] [CrossRef] [PubMed]
- REMAP-CAP Investigators; ACTIV-4a Investigators; ATTACC Investigators; Goligher, E.C.; Bradbury, C.A.; McVerry, B.J.; Lawler, P.R.; Berger, J.S.; Gong, M.N.; Carrier, M.; et al. Therapeutic anticoagulation with heparin in critically ill patients with COVID-19. N. Engl. J. Med. 2021, 385, 777–789. [Google Scholar] [CrossRef]
- ATTACC Investigators; ACTIV-4a Investigators; REMAP-CAP Investigators; Lawler, P.R.; Goligher, E.C.; Berger, J.S.; Neal, M.D.; McVerry, B.J.; Nicolau, J.C.; Gong, M.N.; et al. Therapeutic anticoagulation with heparin in noncritically ill patients with COVID-19. N. Engl. J. Med. 2021, 385, 790–802. [Google Scholar] [CrossRef]
- Sinsky, C.A.; Brown, R.L.; Stillman, M.J.; Linzer, M. COVID-related stress and work intentions in a sample of US health care workers. Mayo Clin. Proc. Innov. Qual. Outcomes 2021, 5, 1165–1173. [Google Scholar] [CrossRef]
- Rinaldi, M.; Bottani, E. How did COVID-19 affect logistics and supply chain processes? Immediate, short and medium-term evidence from some industrial fields of Italy. Int. J. Prod. Econ. 2023, 262, 108915. [Google Scholar] [CrossRef]
- Chowdhury, P.; Paul, S.K.; Kaisar, S.; Moktadir, M.A. COVID-19 pandemic related supply chain studies: A systematic review. Transp. Res. E Logist. Transp. Rev. 2021, 148, 102271. [Google Scholar] [CrossRef]
- Zondervan, N.A.; Tolentino-Zondervan, F.; Moeke, D. Logistics Trends and Innovations in Response to COVID-19 Pandemic: An Analysis Using Text Mining. Processes 2022, 10, 2667. [Google Scholar] [CrossRef]
- Armenakyan, N. New Survey Results Show Health Systems Starting to Recover from Pandemic. Available online: https://www.who.int/news/item/02-05-2023-new-survey-results-show-health-systems-starting-to-recover-from-pandemic (accessed on 9 January 2023).
| Characteristics of Survey Audience | n (%) |
|---|---|
| Research personal contacted | 734 |
| Number of complete responses | 277 (37.7) |
| Number of partial responses | 28 (0.03) |
| Female survey responders | 169 (58.9) |
| Male survey responders | 118 (41.1) |
| Age, years | |
| 18–25 | 27 (9.3) |
| 26–35 | 67 (23.2) |
| 36–45 | 75 (25.9) |
| 46–55 | 79 (27.3) |
| 56–65 | 31 (10.7) |
| 66–75 | 10 (3.5) |
| Ethnic groups | |
| Hispanic/Latino | 23 (8.1) |
| Non-Hispanic/Non-Latino | 260 (91.9) |
| Race | |
| White | 226 (79.9) |
| Black | 15 (5.3) |
| Hawaiian or Pacific Island | 2 (0.7) |
| Asian | 39 (13.8) |
| Others | 7 (2.5) |
| Highest education level | |
| High school graduate/GED | 1 (0.3) |
| Some college, no degree | 7 (2.4) |
| College degree | 91 (31.3) |
| Medical student | 4 (1.4) |
| Graduate/professional degree | 188 (64.6) |
| Hospital size | |
| 101 to 200 beds | 3 (1.1) |
| 210 to 500 beds | 59 (22.1) |
| More than 500 beds | 205 (76.8) |
| Hospital type | |
| Community hospital | 18 (6.1) |
| Public hospital | 32 (10.9) |
| Private-for-profit hospital | 7 (2.4) |
| Private non-profit hospital | 33 (11.3) |
| Rural hospital | 1 (0.3) |
| Urban hospital | 42 (14.3) |
| Teaching university hospital | 247 (84.3) |
| Teaching non-university hospital | 19 (6.5) |
| Research title | |
| Research assistant/research associate | 25 (8.5) |
| Research coordinator | 113 (38.6) |
| Investigators | 106 (36.2) |
| Other | 49 (16.7) |
| Clinical background | |
| EMT/paramedic | 14 (4.8) |
| Registered nurse | 45 (15.4) |
| Medical assistant | 8 (2.7) |
| Respiratory therapist | 2 (0.7) |
| Advanced practice practitioner | 5 (1.7) |
| Pharmacist | 28 (9.6) |
| Physician (MD/DO) | 109 (37.2) |
| Other | 82 (27.9) |
| Years working in the medical field, means ±SD | 16 ± 10.9 |
| Year working research trials, mean ± SD | 9.8 ± 8.1 |
| Survey Questions | Yes n (%) | No n (%) |
|---|---|---|
| Have COVID-19 research studies at your institution impacted non COVID-19 research studies? | 268 (91.5) | 25 (8.5) |
| At any point during the pandemic have you been redeployed or reassigned to another role at your institution in response to COVID-19? | 60 (20.5) | 233 (79.5) |
| Do you think your institution has provided adequate PPE1 to conduct research since the beginning of the COVID-19 pandemic? | 245 (84.2) | 46 (15.8) |
| Has PPE shortage affected your ability to conduct research? | 112 (38.5) | 179 (61.5) |
| Have you completed gowning/de-gowning training in the past 12 months? | ||
| Does your institution have standard operating procedures for bio-specimen processing of confirmed or suspected COVID-19 patients? | 265 (92.9) | 20 (7.0) |
| Does your institution have a designated negative pressure room or flow hood for research-related biological specimen processing? | 245 (86.3) | 39 (13.7) |
| Do you have access to the designated equipment for processing the biospecimens of suspected or confirmed COVID-19 patients? | 195 (79.6) | 50 (20.4) |
| If given the option, would you refuse to approach a suspected or confirmed COVID-19 patient for research enrollment? | 32 (11.6) | 245 (88.5) |
| Do you believe PPE should be budgeted for in research grants during the pandemic for studies that expose researchers to suspected or confirmed COVID-19 patients or their biological specimen? | 252 (90.9) | 25 (9.0) |
| Have you had any work-related exposure to COVID-19 patients? | ||
| Research related COVID-19 exposure | 54 (18.6) | 237 (81.4) |
| Clinical work-related COVID-19 exposure | 40 (13.7) | 251 (86.3) |
| Both research and clinical work-related exposure | 70 (24.1) | 221 (75.9) |
| No work-related exposure | 127 (43.6) | 164 (56.4) |
| Have you been tested for COVID-19 at any time during the COVID-19 Pandemic? | 146 (50.2) | 145 (49.8) |
| Have you tested positive for COVID-19? | 12 (8.2) | 134 (91.8) |
| At any time during the pandemic have you or someone in your department: | ||
| Quarantined due to exposure to COVID-19 | 122 (42.9) | 162 (57.0) |
| Got infected and recovered from COVID-19 | 93 (32.8) | 191 (67.3) |
| Been hospitalized due to COVID-19 | 16 (5.6) | 268 (94.4) |
| Applied for disability benefits due to COVID-19 | 4 (1.4) | 280 (98.6) |
| Died from a COVID-19 infection | 1 (0.4) | 283 (99.7) |
| Research Position | |||||
|---|---|---|---|---|---|
| Investigators # (n = 106) | Research Staff € (n = 138) | Other $ (n = 49) | p-Value Investigators vs. Research Staff | ||
| Male gender | 71 (67.6%) | 33 (24.4%) | 14 (31.1%) | <0.001(C) * | |
| COVID-19 research at your institution has impacted non-COVID-19 studies. | 98 (92.5%) | 127 (92.0%) | 43 (87.8%) | 0.903 (C) | |
| You have been reassigned to another role due to COVID-19. | 29 (27.4%) | 25 (18.1%) | 6 (12.2%) | 0.085 (C) | |
| Primary clinical area of enrollment | Emergency department | 29 (27.4%) | 58 (42.6%) | 6 (12.8%) | <0.001(C) * |
| Intensive care unit | 66 (62.3%) | 59 (43.4%) | 17 (36.2%) | ||
| General practice unit | 10 (9.4%) | 7 (5.1%) | 6 (12.8%) | ||
| Other | 1 (0.9%) | 12 (8.8%) | 18 (38.3%) | ||
| Type of work-related COVID-19 | Research exposure | 0 (0.0%) | 49 (35.5%) | 5 (10.6%) | <0.001(C) * |
| Clinical exposure | 33 (31.1%) | 5 (3.6%) | 2 (4.3%) | ||
| Research and clinical exposure | 49 (46.2%) | 19 (13.8%) | 2 (4.3%) | ||
| No work-related COVID-19 exposure | 24 (22.6%) | 65 (47.1%) | 38 (80.9%) | ||
| You have been tested for COVID-19 at any time. | 69 (65.1%) | 61 (44.2%) | 16 (34.0%) | 0.001 (C) * | |
| If yes, a test result was positive. | 9 (13.0%) | 3 (4.9%) | 0 (0.0%) | 0.110 (C) | |
| Your institution has given you adequate PPE during the pandemic. | 92 (86.8%) | 114 (82.6%) | 39 (83.0%) | 0.372 (C) | |
| PPE shortages have affected your ability to conduct research. | 37 (34.9%) | 59 (42.8%) | 16 (34.0%) | 0.214 (C) | |
| You have completed gowning/de-gowning training in the past 12 months. | 100 (94.3%) | 85 (61.6%) | 27 (57.4%) | <0.001 (C) * | |
| Scrubs are not provided. | 8 (7.5%) | 10 (7.2%) | 1 (2.0%) | 0.929 (C) | |
| Gloves are not provided. | 4 (3.8%) | 6 (4.3%) | 1 (2.0%) | 1.000 (F) | |
| Surgical masks are not provided. | 2 (1.9%) | 11 (8.0%) | 2 (4.1%) | 0.036 (C) * | |
| N95 masks are not provided. | 23 (21.7%) | 44 (31.9%) | 11 (22.4%) | 0.077 (C) | |
| Rate your highest fear of infection at work prior to the pandemic. | 3.4 ± 2.7 2.5 (1–5) | 3.0 ± 2.5 2(1–5) | 2.8 ± 2.5 2(1–5) | 0.247 (W) | |
| Rate your highest fear of infection at work since the pandemic. | 6.1 ± 3.0 7 (4–8) | 5.8 ± 2.8 6 (4–8) | 5.9 ± 3.0 7 (3–8) | 0.407 (W) | |
| Rate how comfortable you feel in the lab while processing possible COVID-19 samples. | 6.8 ± 2.9 8 (5–9) | 6.4 ± 3.0 7 (4–9) | 5.6 ± 3.4 6 (2.5–8.5) | 0.355 (W) | |
| Someone in your department was hospitalized due to COVID-19. | 11 (10.5%) | 2 (1.5%) | 3 (6.7%) | 0.002 (C) * | |
| Someone in your department was disabled due to COVID-19. | 2 (1.9%) | 2 (1.5%) | 0 (0.0%) | 1.000 (F) | |
| Someone in your department was quarantined due to COVID-19. | 46 (43.8%) | 62 (46.3%) | 14 (31.1%) | 0.705 (C) | |
| Someone in your department got infected by and recovered from COVID. | 37 (35.2%) | 42 (31.3%) | 14 (31.1%) | 0.525 (C) | |
| Someone in your department died from COVID-19. | 1 (1.0%) | 0 (0.0%) | 0 (0.0%) | 0.439 (F) | |
| Rate how obligated you feel to enroll suspected/confirmed COVID-19 patients in trials. | 7.2 ± 3.0 8 (5–10) | 7.5 ± 3.1 9 (6–10) | 6.2 ± 4.1 8 (1–10) | 0.137 (W) | |
| Rate how comfortable you feel enrolling suspected/confirmed COVID-19 patients in studies. | 8.6 ± 2.1 9 (8–10) | 8.0 ± 1.9 8 (7–10) | 7.4 ± 2.7 8.5 (7–9) | 0.001 (W) * | |
| Rate how willing your co-workers are to share workload on possible COVID-19 patients. | 7.4 ± 2.4 8 (6–10) | 7.6 ± 2.5 8 (6–10) | 8.2 ± 2.4 9 (7.5–10) | 0.513 (W) | |
| You would refuse to approach a possible COVID-19 patient for enrollment. | 4 (3.9%) | 19 (14.4%) | 9 (21.4%) | 0.007 (C) * | |
| Available emotional support | 73 (70.9%) | 71 (53.8%) | 37 (88.1%) | 0.008 (C) * | |
| Available work from home support | 86 (83.5%) | 112 (84.8%) | 39 (92.9%) | 0.777 (C) | |
| Available time-off support | 76 (73.8%) | 92 (69.7%) | 35 (83.3%) | 0.491 (C) | |
| Available pay incentive support | 23 (22.3%) | 18 (13.6%) | 0 (0.0%) | 0.081 (C) | |
| Available quarantine support | 46 (44.7%) | 39 (29.5%) | 16 (38.1%) | 0.017 (C) * | |
| Other available support | 0 (0.0%) | 1 (0.8%) | 0 (0.0%) | 1.000 (F) | |
| Rate the clinical response to COVID-19 by your organization. | 74.8 ± 18.9 77 (64–88) | 77.4 ± 19.6 81 (68–95) | 77.5 ± 15.6 79 (70–90) | 0.242 (W) | |
| Rate the research response to COVID-19 by your organization. | 64.9 ± 27.5 72 (50–86) | 68.3 ± 26.7 76 (50–92) | 75.6 ± 20.7 81.5 (61–92) | 0.293 (W) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gill, J.K.; Bissonette, A.; Cook, A.A.; Jaehne, A.K.; Day, J.; Renaud, S.; Jacobsen, G.; Nelson, K.; Kozikowski, L.-A.; Jayaprakash, N.; et al. Research Staff COVID-19 Pandemic Survey-Results from the Prevention and Early Treatment of Acute Lung Injury (PETAL) Network. COVID 2023, 3, 1528-1543. https://doi.org/10.3390/covid3100104
Gill JK, Bissonette A, Cook AA, Jaehne AK, Day J, Renaud S, Jacobsen G, Nelson K, Kozikowski L-A, Jayaprakash N, et al. Research Staff COVID-19 Pandemic Survey-Results from the Prevention and Early Treatment of Acute Lung Injury (PETAL) Network. COVID. 2023; 3(10):1528-1543. https://doi.org/10.3390/covid3100104
Chicago/Turabian StyleGill, Jasreen Kaur, Andrew Bissonette, Aaron A. Cook, Anja Kathrin Jaehne, Jacqueline Day, Sheri Renaud, Gordon Jacobsen, Kristine Nelson, Lori-Ann Kozikowski, Namita Jayaprakash, and et al. 2023. "Research Staff COVID-19 Pandemic Survey-Results from the Prevention and Early Treatment of Acute Lung Injury (PETAL) Network" COVID 3, no. 10: 1528-1543. https://doi.org/10.3390/covid3100104
APA StyleGill, J. K., Bissonette, A., Cook, A. A., Jaehne, A. K., Day, J., Renaud, S., Jacobsen, G., Nelson, K., Kozikowski, L.-A., Jayaprakash, N., Gardner-Gray, J., Swiderek, J., Oldmixon, C. F., Ringwood, N. J., Sherwin, R. L., Williams, M. D., Gupta, A. H., Johnson, N. J., Hyzy, R. C., ... on behalf of the National Heart, Lung and Blood Institute PETAL Clinical Trials Network. (2023). Research Staff COVID-19 Pandemic Survey-Results from the Prevention and Early Treatment of Acute Lung Injury (PETAL) Network. COVID, 3(10), 1528-1543. https://doi.org/10.3390/covid3100104






