1. Introduction
The coronavirus disease (COVID-19) pandemic has afflicted over 40 million people worldwide, leading to more than 1.1 million deaths as of October 2020 [
1]. While Singapore was recently named by Bloomberg as “the world’s best place to be during COVID,” [
2] with the case fatality being one of the lowest in the world (below 0.05%), likely contributed by the disproportionately high number of younger migrant workers who were infected (about 95% of total cases), vigilance is still essential to prevent widespread community transmission, especially to the vulnerable population. As there is delay between infection and isolation as the incubation time of the virus can be up to two weeks, coupled with the asymptomatic nature of many patients (with asymptomatic patients still able to transmit the virus), emerging evidence internationally has highlighted early contact tracing and effective social distancing as imperative to reduce the risk of the spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [
3,
4,
5].
Successful contact tracing encompasses three key facets: contact identification, listing, and follow-up [
5,
6]. As the international response to the virus continues, governments across the globe have devised various strategies for tracing and quarantining carriers of the virus. From suppression, to mitigation, to herd-immunity strategies, countries across the world have adopted differentiated strategies to combat the pandemic. From aggressive and centralized suppression, to mitigation to herd-mentality strategies, success stories worldwide—South Korea, Denmark, New Zealand, Taiwan, Vietnam, and Singapore —showcase that a strong digital infrastructure and proactive containment based on comprehensive testing, tracing, and quarantining are key features that must work in conjunction with contact tracing technology [
7,
8,
9].
From using applications and platforms such as WeChat and Alipay, to permutations and combinations involving Bluetooth and other digital technologies, several solutions exist globally [
10]. However, the ability to retrieve the data and, more importantly, convert it into a beneficial format and/or dashboard is dependent on the design and efficacy of the software. In Singapore, the “TraceTogether” app adopts a similar approach. While this method removes the logging of a user’s location or their real name, it requires individuals to download the app and configure it to run in the foreground for the app to be effective. Moreover, this method is rendered altogether ineffective if individuals did not download and make use of the app [
11]. The implementation of “SafeEntry” subsequently by the Singapore government captures the data of individuals who have frequented public places at a particular day and time period, yet may not necessarily carry specific data on each individual’s interaction with people who eventually test positive for COVID-19 [
12]. Furthermore, there have been ethical concerns on privacy protection, equality, and fairness in digital contact tracing methods [
13].
All healthcare and other frontline workers are a critical demographic when it comes to contact tracing and the overall pandemic chain of transmission. This population is also one that faces a greater risk of contracting the virus: nurses, doctors, and other healthcare workers reported a median of 14,18, and 15 contact persons over a given shift, respectively, in a typical general ward in Singapore [
14]. Due to being in proximity of patients and their own coworkers for extended periods of time, failing to manage exposure and controlling contact could result in unsuccessful mitigation of risks in the healthcare work setting. In the hospital setting, conventional contact tracing methods, such as continuous direct observation, reliance on the individual’s memory of the encounter, and data extraction from electronic medical records demanding vast resources and data, are time consuming, and limit patient exposure to care providers who are adding to the database records. The gaps of these conventional methods alongside the pandemic have catalyzed the use of real-time locating systems in the healthcare space, with more and more healthcare institutions implementing wireless, Bluetooth, hardware, and mobile app mechanisms within the premises for contact tracing and social distancing [
15].
The creation of a standalone device by PwC Singapore intended to address these very concerns of personal data breach and location tracking, and the requirement of Bluetooth technology for effective contact tracing. We aimed to evaluate the use of a real-time standalone device created by PwC Singapore in the emergency department (ED) during its response to COVID-19. The pilot observational study was divided into two Phases.
The intention of Phase 1 was to monitor physical distancing amongst healthcare workers within various locations in the ED, namely doctors, nurses, and patient service associates (admin). Phase 2 assessed physical interactions—in terms of duration and distance—between patients who had received a swab to test for COVID-19 and healthcare workers assigned to evaluate and manage them within designated zones in the ED.
2. Materials and Methods
2.1. Setting and Participants
The pilot study was conducted in the ED of Singapore’s NUH from 1 June 2020 to 12 June 2020 (Phase 1) and from 29 June 2020 to 10 July 2020 (Phase 2). Participants involved included on-duty clinicians, nurses, and patient service associates within the department. Phase 2 of the study included ED patients. However, no personal data or patient identifiers were captured for the study. This study was thus exempted from formal institutional review board review as no identifiers were collected or stored.
The ED floor layout was studied to determine best strategic locations for placement of hardware to maintain optimal wireless signals between devices. Briefly, the ED comprised resuscitation areas (capacity of 6 standard resuscitation trolleys and 3 negative pressure resuscitation rooms), four distinct intermediate care areas (total capacity of 44 monitored trolleys), ambulatory area (3 triage counters, 5 main consultation rooms and 2 separate seated waiting areas), isolation zones (capacity of 15 monitored trolleys, 13 isolation rooms, 20 makeshift outdoor isolation cubicles and 20 temporary holding cubicles), and a staff pantry.
2.2. Study Design and Hardware
The study was designed to run for four weeks in total; Phases 1 and 2 lasted for two weeks each and ran sequentially but with a two-week break in between. The workflow processes of the Phase 1 were reviewed; improvisations were made, and the revisions were tested out in Phase 2.
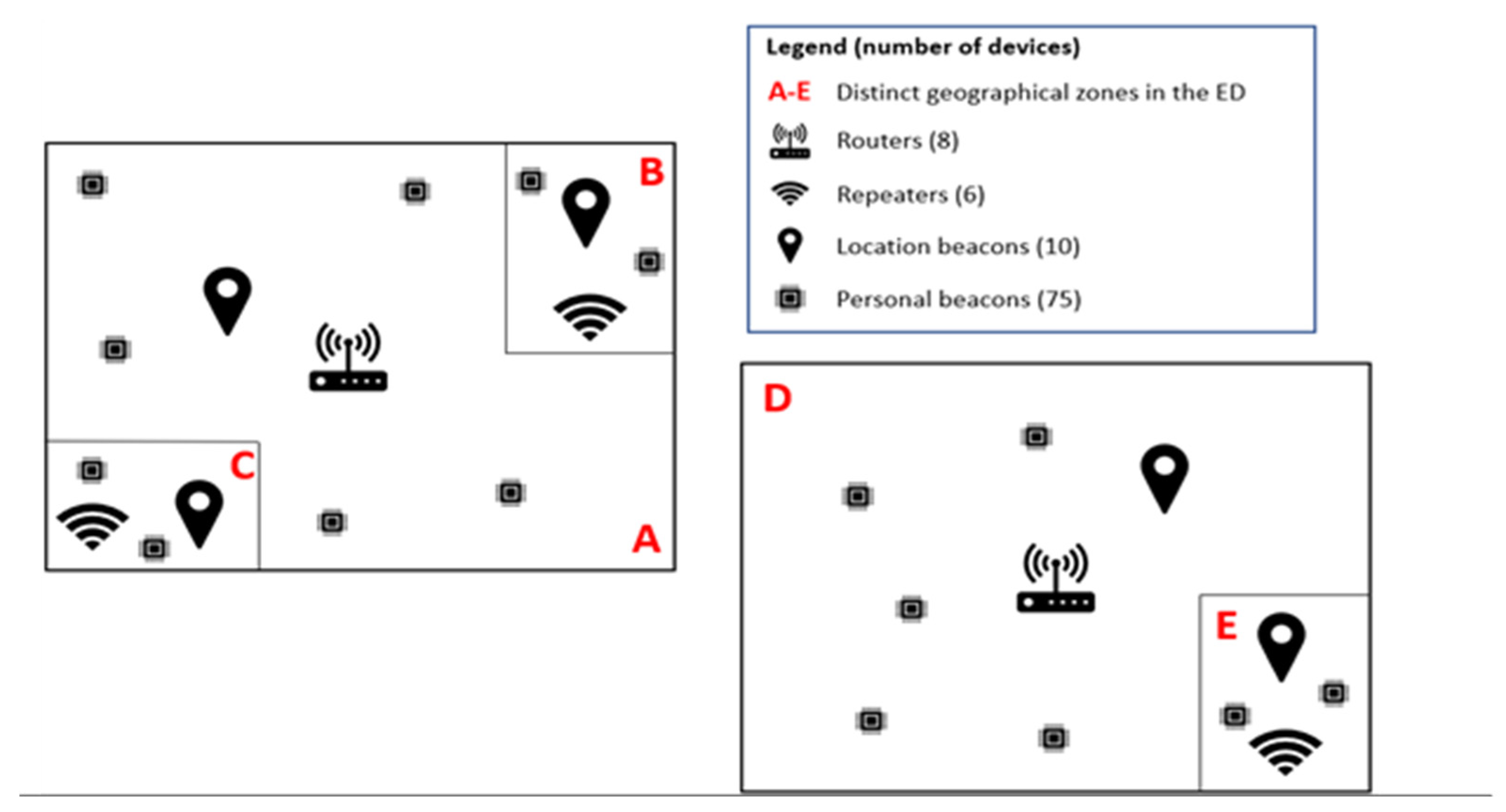
A total of 10 location beacons were placed at strategic locations within the ED. These location beacons did not track the exact geographical location of the areas within the ED but instead were used as markers to identify the relative distance or location of tagged individuals (
Figure 1). The internal components of location beacons include an nRF52810 SoC supporting Bluetooth Low Energy (BLE), powered by a single CR2032 battery.
A total of 75 personal beacons for individual use were prepared for healthcare workers and patients. The handling of the beacons for individual use is further highlighted in the workflow below. Beacon hardware features included in-built Bluetooth, Wi-Fi, 4 MB Flash Memory, 400mAH@3.7V battery and LCD Screen.
Additional routers (TP-Link Archer MR400 AC1200 Wireless 4G Router, ShenZhen, China) and repeaters (TP-Link 860re Range Extender, ShenZhen, China) were installed at various locations within the ED. These helped to capture data emitted from the location and personal beacons (
Figure 2) and reflected the data real-time onto the contact tracing portal and dashboard. The data were continually uploaded onto the server and analyzed to determine the interaction time and distance between individuals and the formation of clusters and areas of higher population density within the ED.
2.3. Administrative Workflow
In Phase 1, a designated administrative staff oversaw the distribution of the beacons at the start of each shift. Each beacon with its unique beacon number tag was pre-matched with each healthcare worker and subsequently distributed accordingly prior to the start of their shift. There was no linkage between the beacons and the individual’s mobile phone or any other device. At the back end, the unique beacon was tagged electronically to each of these healthcare workers’ randomly generated proxy ID onto the contact tracing portal. At the end of the shift, the staff sanitized and returned the beacon to the designated administrative staff, who untagged the beacon from the portal. The devices were then charged in a remote location at the end of the day to be ready for use the following day. Due to the limited number of beacons provided for the pilot study, Phase 1 was conducted on all day shifts during weekdays.
Phase 2 was conducted predominantly in the isolation zones of the ED where patients who presented with signs and symptoms suspicious of COVID-19 were isolated. This Phase was carried out on both day and evening shifts on weekdays. Phase 2 was intended to begin two weeks after the conclusion of Phase 1 to allow modifications and enhancements to be made, especially related to workflows and incorporation of patient movement data. Review of methods to tag and untag individuals to personal beacons was also conducted. After untagging, these beacons were also returned for charging, prior to their next use.
2.4. Tagging of COVID-19 Suspects
This additional workflow was part of Phase 2. Patients who required a COVID-19 swab after initial assessment by the doctors were identified for the study. COVID-19 suspects were issued a beacon to be kept physically with them for the duration of their stay within the ED. Each of these patients were given a unique beacon identification number, which was tagged onto the last four digits of their identity document. Only the last four digits of each individual was captured as data on the dashboard; in the event that a patient were to be identified as COVID-19 positive, we would be able to match their actual identity with these last four digits and extract the relevant data needed to contact trace the other potentially affected individuals.
2.5. Data Analysis
All data were captured real-time onto the Dashboard. All count, time, and distance measurements were summarized using mean. The data were subsequently summarized and displayed in Microsoft Power BI (Microsoft Corp, Redmond, WA, USA).
3. Results
3.1. Phase 1
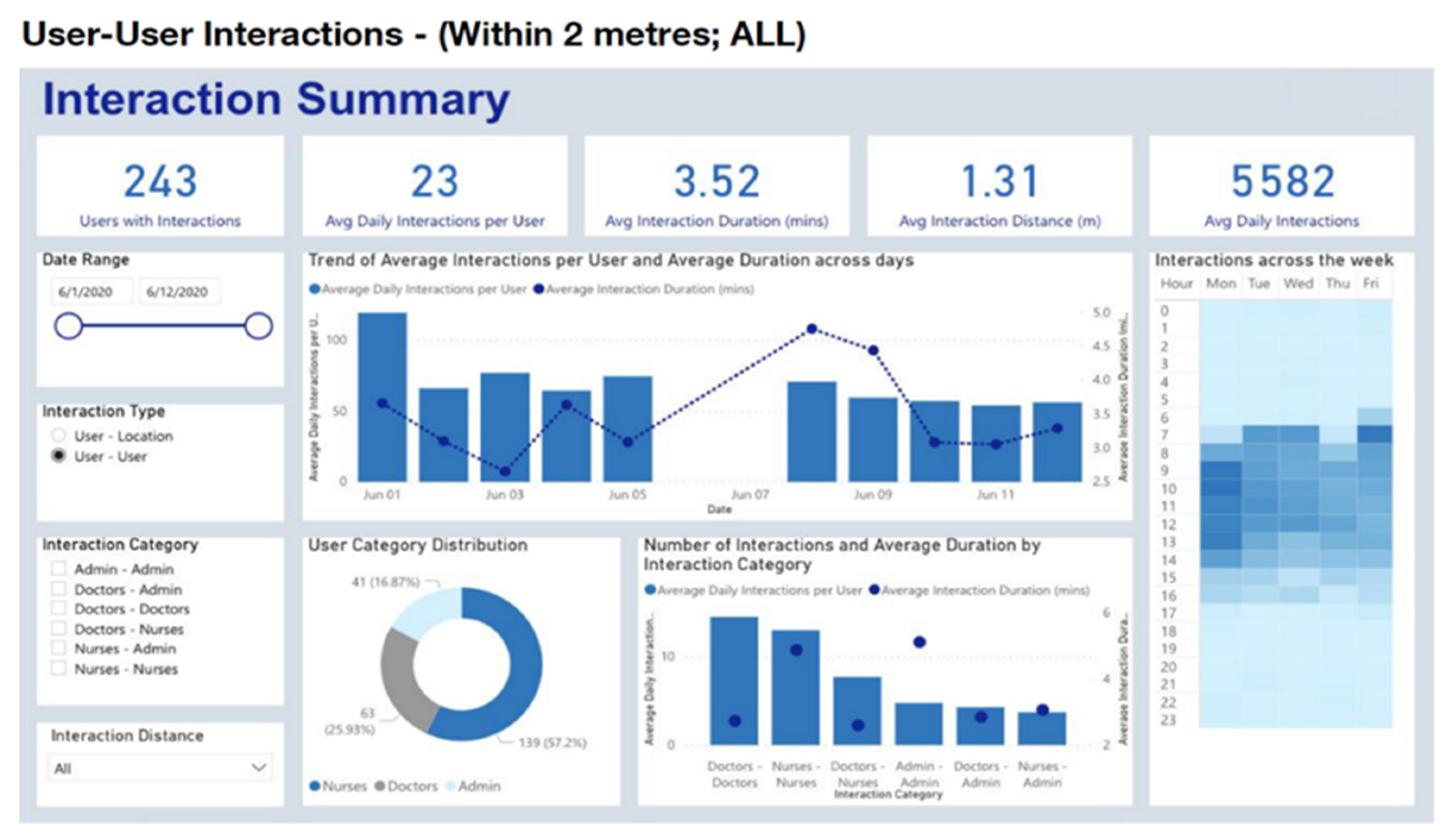
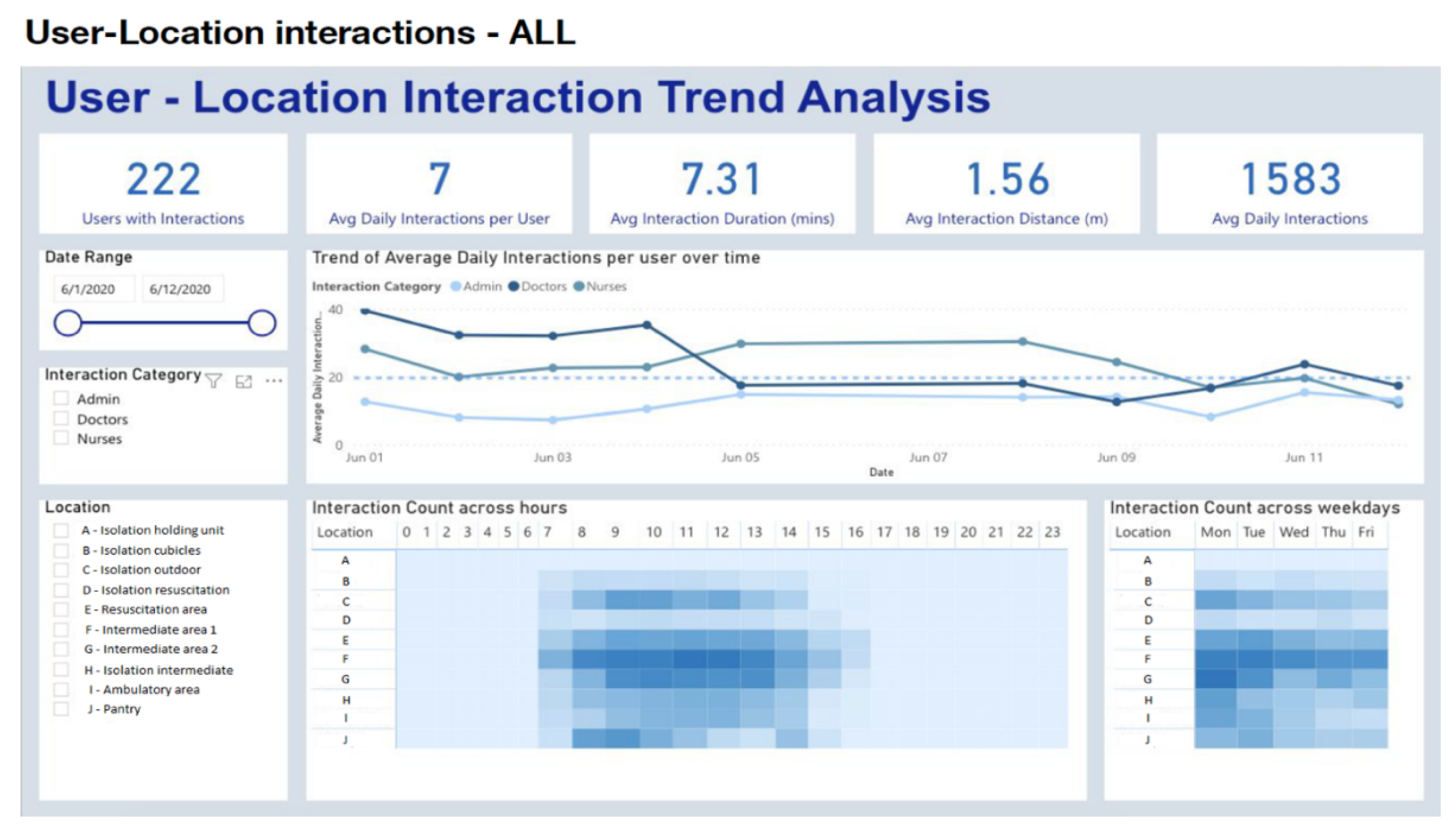
There was an average of 5582 daily interactions throughout the 10 days of Phase 1, at an average interaction distance of 1.31m, when a filter of 2 m [
15] was applied (
Figure 3). No staff members contracted COVID-19 during Phase 1. As a result, there was no scenario in which contact tracing was required. However, the ability to perform rapid contract tracing was made available to the contact tracing team should the need arise.
Based on the user–user interactions within a 2-m distance, the greatest time-periods of interaction among all staff occurred at 9:00 a.m. to 10:59 a.m. across the 10 days of Phase 1, with an average of 1444.8 interactions per day. The average daily interactions were additionally calculated by multiplying the average daily interactions per user with the number of users who were actively using the device on a given day. The greatest average daily interactions occurred on Mondays with a total of 6989 interactions across Phase 1, and the fewest on Thursdays with a total of 4111 interactions across Phase 1.
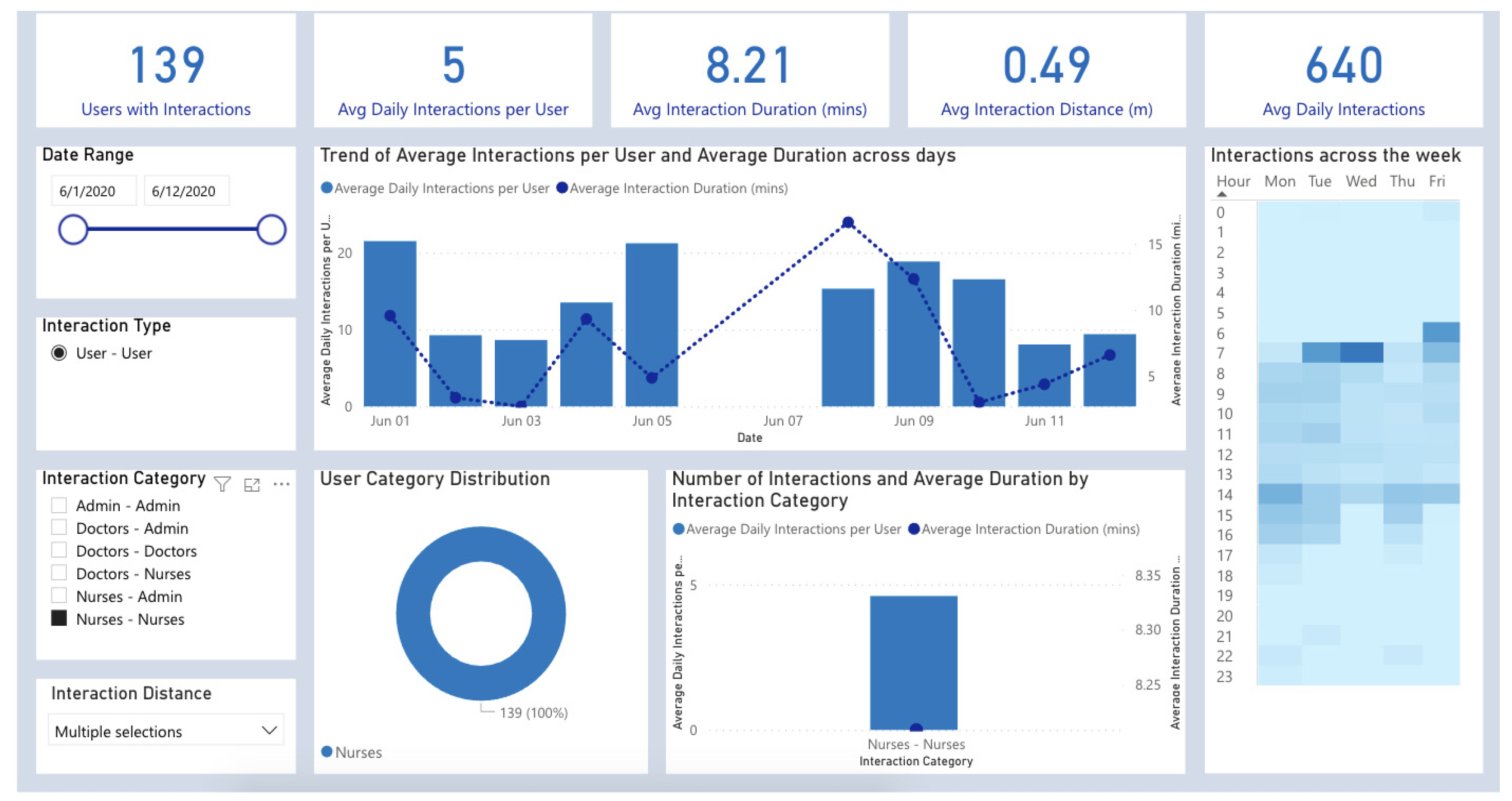
Among these interactions, social clusters were examined to determine physical distancing compliance among hospital workers by filtering for user–user interactions that occurred within 1 m [
16], for a duration of more than 1 min during Phase 1. User–user interactions were compared individually through the interaction category on the dashboard, displaying the largest average daily interactions occurring between nurses–nurses (640 interactions) over Phase 1 (
Figure 4). Fewer average interactions were found between doctors–doctors (388 average daily interactions), doctors–nurses (161 average daily interactions), admin–admin (118 average daily interactions) and doctors–admin (47 average daily interactions) over the course of Phase 1.
Taking advantage of the fixed location beacons, we were able to determine the various levels of interaction among staff within specific areas of the ED. More specifically, user–location trends were analyzed to determine the locations that hosted greater crowding (average interaction distance), as well as greater interaction counts (average daily interactions) within the ED (
Figure 5). User–location interactions over the 10-day period uniquely identified the highest average daily interactions in intermediate care area 1 (345.3), intermediate care area 2 (265.4), the outdoor isolation zone (176.0) and the pantry (154.2) relative to other locations within the ED.
3.2. Phase 2
In Phase 2, we recognized that having an additional administrative staff to oversee the workflow of pre-assigning the beacons, then tagging beacons to the matched healthcare workers’ proxy ID onto the portal electronically would not be a feasible long-term solution, hence it was improvised into a self-tagging system using a QR code generated for the personal beacons as well as for each individual staff member. A QR code carrying each staff’s unique proxy ID had been distributed prior to the start of Phase 2. At the beginning of each shift, the healthcare worker was given a personal beacon with its unique QR code and proceeded to sign into the portal using their own QR code, then scanned the beacon’s QR code to tag themselves electronically to the beacon. At the end of the shift, the same process untagged the individual from the beacon.
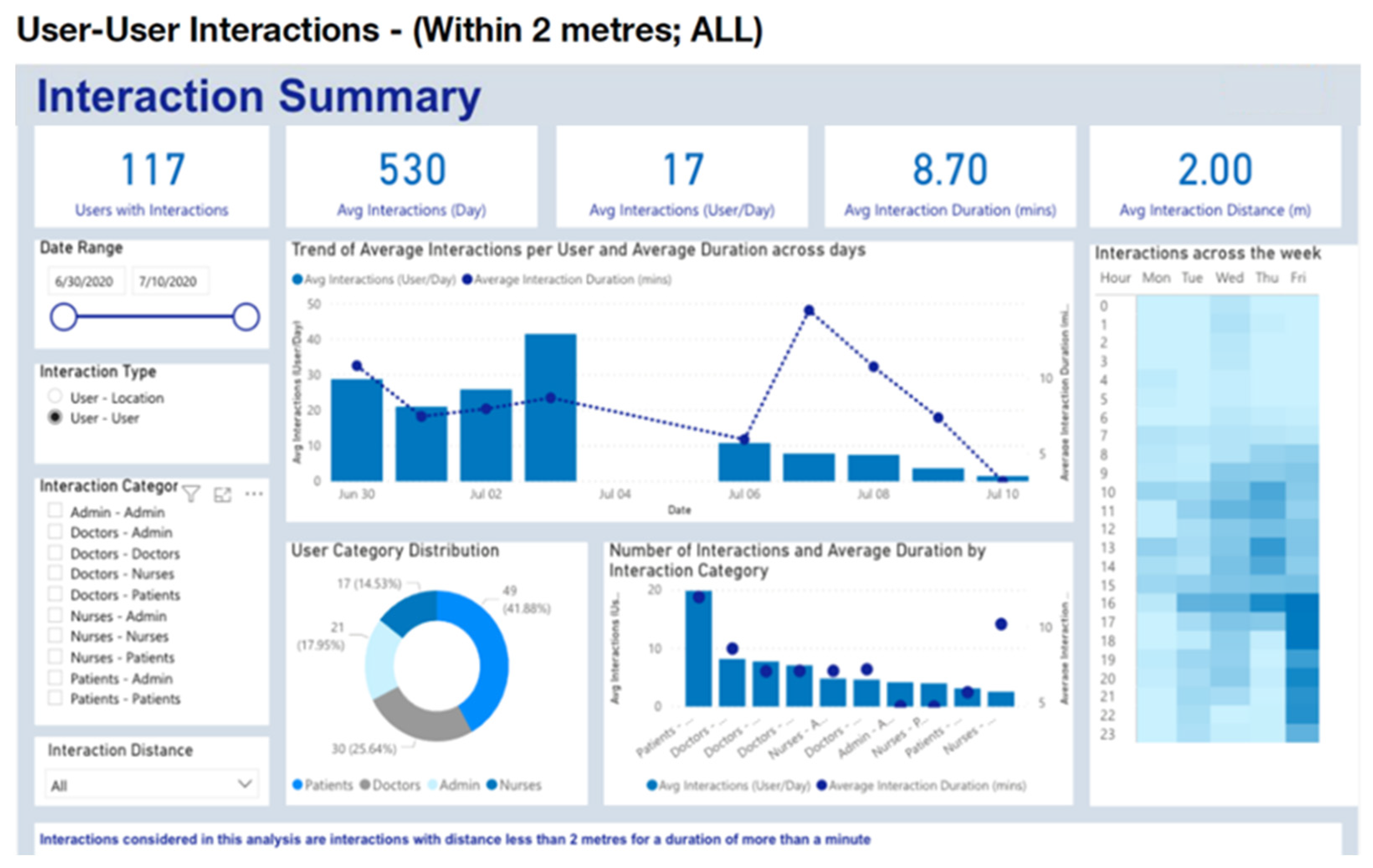
There was an average of 530 daily interactions throughout the 10 days of Phase 2, at an average interaction distance of 2 m, when a filter of 2 m [
15] was applied (
Figure 6). No staff members or patients contracted COVID-19 during Phase 2 as well. Thus, there was no scenario in which contact tracing was required in Phase 2 as well.
Based on the user–user interactions within a 2m distance during Phase 2, the greatest time-periods of interaction among all staff over the 10-day period occurred between 4:00 p.m.–4:59 p.m., with an average of 37.8 average interactions per day of Phase 2. The average daily interactions were not computed for Phase 2 due to logistical issues that resulted in a lack of hardware usage and accompanied data gaps.
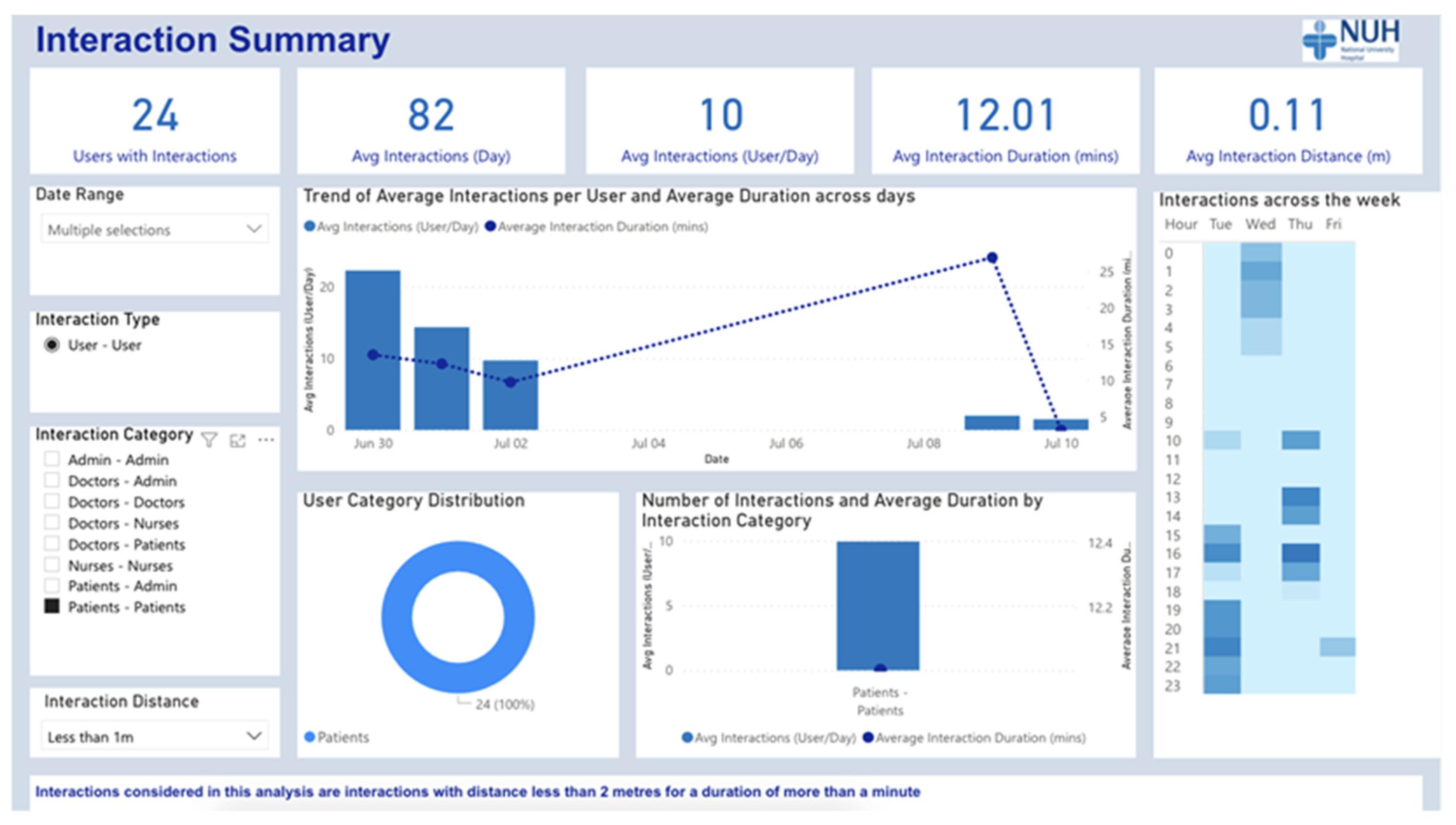
Among these interactions, social clusters were further examined within Phase 2 as well, in order to understand physical distancing compliance among hospital workers as well as their respective patients. User–user interactions that occurred within 1 m [
16] of each other were filtered and compared by interaction category (
Figure 7), uniquely identifying the greatest average daily interactions between patients–patients (82 average daily interactions), and doctors–doctors (31 average daily interactions). There were fewer average daily interactions found between doctors–patients (12), admin–admin (10) and doctors–admin (10), nurses–nurses (7), patients–admin (6), and doctors–nurses (3) within the ED.
Taking advantage of the fixed location beacons once again, we were able to determine user-location trends among both staff and patients within Phase 2 of the ED (
Figure 8). Intermediate care area 2 was uniquely identified once again for having one of the largest average daily interactions over the 10-day period (86.8), other than the Isolation holding unit which hosted 173.8 average daily interactions, relative to all other locations listed within the ED.
3.3. Dashboard for Contact Tracing
While no patient or staff member contracted COVID-19 in either Phase 1 or 2, the dashboard can be activated to allow for individual-level visualization and contact tracing in the event of a positive contraction (
Figure S1). Contact tracing via the Contra platform can be visualized and performed by the following four steps:
Step 1: Notify: Staff or patients who tested COVID-19 positive must notify relevant authorities within the hospital. Staff can also notify on behalf of patients after their testing results are received.
Step 2: Flag: After confirmation that a particular staff/patient has been tested positive, Contra dashboard administrator logs into the Contra dashboard. He/she then selects the appropriate filters (contact distance, contact time, days) and searches for the user and clicks on ‘Flag as Infected’.
Step 3: Assess: After the person has been flagged, the system then calculates risk level for people in contact based on their contact duration and distance with the infected person. At this point, the administrator selects the infected person in the dashboard and clicks on ‘View Cluster Info’ for information on all other people at risk.
Step 4: Communicate: The administrator and other relevant hospital departments then can reach out (outside the Contra platform) to people at risk providing them with the necessary advisory and next steps.
4. Discussion
4.1. Principal Findings
This hardware solution uniquely captures and visualizes clusters, count, time, and distance measurements in a user-friendly manner through the Contra dashboard without any privacy or security concerns.
The key findings were the time-day trends of interaction, social cluster trends within a 1-m distance, and location data that displayed the areas of high traffic within the ED throughout Phases 1 and 2. Time-day trend findings were key in identifying when frequent and lengthy close contact was occurring among individuals on a day-to-day basis. The findings from Phase 1 suggested that the greatest amount of daily interaction times over the 10-day period among all staff members typically occurred in the mornings (9:00 a.m.–10:59 a.m.), with Monday hosting the greatest interaction counts relative to any other weekday. Phase 2 time-day trends included hardware usage by patients as well as staff within the ED, uniquely highlighted evenings (16:00–16:59) as hosting the greatest counts of human traffic. While no day analysis was computed for Phase 2 due to a lack of hardware usage that created gaps within the data,
Figure 6 suggests that Fridays were most crowded within the ED, with an emphasis on evening-times where patients were most likely being discharged. However, the information gathered ultimately lacks data on the weekends and night shifts, which resulted in an underestimated recorded number of healthcare staff on shift and ED attendance; hence, it is important to note that the Phase 2 findings may not be entirely representative of the time and days of high traffic throughout the study.
Based on the social cluster trends displaying physical distance incompliance (<1 m), the largest average daily interactions seemed to occur between nurses–nurses and doctors–doctors in Phase 1, and patients–patients in Phase 2. While social cluster information was not actionable within the context of the study as no staff member or patient contracted COVID-19 during either Phase 1 or 2, these trends are critical in the event that contact tracing is required within the ED. In the event that an individual becomes positive, the Contra dashboard would allow the user to rapidly identify social clusters and points of contact within the ED, easily alerting and notifying necessary individuals. Furthermore, it should be noted that the dashboard (
Figure 8) allows various parameters to be adjusted (e.g., distance of 50 cm, 1 m, 2 m, etc., time) to meet with any change in the Ministry of Health (MOH) guidelines.
Finally, the location interaction feature identified the highest traffic locations, uniquely identifying intermediate areas (both 1 and 2), the outdoor isolation zone, and the pantry as having the highest recorded number of interactions per day during Phase 1, with Intermediate area 2 (and the Isolation holding area) additionally highlighted as high-traffic regions within Phase 2. However, it is important to consider that this information seems appropriate given the natural structure of the ED; both doctors and nurses frequently need to congregate around intermediate areas in order to work together and attend to patients on a normal day-to-day shift. For instance, when a sick patient presents to a given resuscitation area, many doctors and nurses are required to be in close proximity to properly attend to a sick patient for a prolonged period of time. Hence, social distancing may not be entirely possible due to the nature of the work itself, emphasizing a need for strict compliance to mask wearing, hand hygiene, and personal protective equipment among health care workers within the ED that may circumvent the issue of proximity.
4.2. Implications and Effected Change
While some of the findings could not be acted upon given the nature of ED work that necessitates proximity (resuscitation and intermediate areas), the findings were contextualized and considered, resulting in some amendments to improve social distancing within the ED. For example, as the pantry was identified as high risk, mitigating steps were taken to limit access to a maximum of 8 people at any given time.
Based on the social cluster trends coupled with the aforementioned location data explored on the dashboard, the ED additionally dedicated new areas for doctors and nurses within the ED that promoted dining separately and limited the number of individuals gathering in a closed and confined space. This implementation facilitated the separation of social interaction between different groups of health workers further (doctors, nurses, admin).
Finally, due to the proximity information gathered on the Contra dashboard, transparent plexiglass was installed within the ED to separate diners at each table from each other: spacing out tables at a bare minimum of 2 m away from each other to circumvent the issue of proximity in regions where PPE and masks may be removed.
4.3. Strengths
This observational study highlighted and addressed multiple concerns that earlier contract tracing devices and applications had faced within an outbreak setting. For instance, the hardware solution resolved many of the personal data collection and privacy concerns around GPS location trackers. The standalone hardware device requires no linkage to any other mobile device and carries no personal user data onto the portal. Additionally, it does not include any GPS location around the user in order to track the users every move, eliminating some key user privacy concerns.
Additionally, multiple contact tracing applications available on the phone such as COVIDSafe in Australia and TraceTogether in Singapore require Bluetooth energy consumption. While these Bluetooth signals allow for the capturing of contacts within the vicinity without any recall biases, they force the application to continuously run in the foreground in order to effectively work. This hardware solution circumvents this issue by relying on stand-alone beacons instead of the limitations of the phone itself.
Furthermore, where the elderly who often are not technology-savvy form a substantial proportion of presentations to the ED, the device itself is user friendly, which is critical within this population, as it requires no additional steps to activate it, or power it off. The device automatically switches on after it has been tagged to the end-user and does not require any manual navigation on the user’s end.
In addition to being technologically user-friendly, the hardware is small and simplistic by design (
Figure 8,
Appendix A Figure A2), easily carried in the pockets or scrubs of healthcare workers or clipped on a ring and worn on lanyard (
Figure 9,
Appendix A Figure A1). Hence, the device is hassle-free: easy to sanitize and charge before and after use.
Lastly, from a cost perspective, the total solution cost is under 10 dollars per user per month, inclusive of all software and hardware, if mass deployed at scale.
4.4. Limitations
There were several limitations of the study, which served as learning points for the team.
- 1.
Battery/Charging Issues
The battery life of the device lasted up to a maximum of 10 h; effective data would have been lost if these devices were used past 10 h. In addition, it was not possible to charge the device while it was being used. Enhancements to the battery and use of low-energy solutions may be able to prolong the battery life of the devices.
- 2.
Lack of Prompts
The lack of visual, audio, or tactile notifications from the device reduced the ability of prompts for the individual carrying it to be aware of potential breach of social distancing measures. Future iterations could consider adding useful vibratory, light, and sound features to enable the prevention of prolonged close contact time, rather than needing to remedy the situation later.
- 3.
Device Tagging and Untagging Issues
During Phase 1 of the pilot study, the handling of the device—issuing at the start of each shift, collection of the device at the end of shift, accounting for each device and recharging the devices—was outsourced to an administrative staff. To ensure that the process of issuing the devices personally to a large number of staff at the start of each shift was not time consuming, the device allocation was planned out beforehand by the administrative staff, and then tagged backend onto the portal. This put a strain on the administrative staff to run the process. Specific improvements were thus made to address administrative strain in Phase 2. The introduction of the QR code method for signing in, self-tagging, and untagging of the devices improved the end-user experience and ensured more accurate data to be reflected in real time as well.
- 4.
Compliance Issues
Inability to manage the devices during peak hours
In Phase 1, the additional steps required for doctors to manually tag the patients onto the portal following a COVID-19 swab test was relatively time-consuming during peak periods where patient load was high and there were more urgent issues to attend to while on clinical duty. This could have led to a loss of movement and contact data as the doctors were unable to practically comply with entering the details onto the portal and issuing the device to the patient. However, this was resolved within Phase 2 as previously described.
- 5.
End-User Behaviour and Attitudes
The self-service method of assigning and revoking the devices (Phase 2) led to multiple occasions whereby the end-users either forgot to tag themselves despite being handed the device at the start of shift or forgot to untag the devices before returning them. This resulted in inaccurate real-time data being collected and represented. However, we were able to filter by end-time to allow such inaccuracies to be removed from the summary display.
4.5. Recommendations
If the device were to be mass produced, there could potentially be an option for every staff member to be responsible for each of their own devices that they bring to work every shift, and to self-assign or revoke them when necessary.
In addition, the device could also have better battery life, with simple power on/off buttons and indicators for when a device is faulty and requires troubleshooting. There could also be an alarm indicator for distance alerts to remind users to be wary of physical distancing, or to alert when the battery is running low or is fully charged.
The bigger challenge remains in bringing about behavioral change amongst end-users with regard to using the device, especially for tagging of patients suspected of COVID-19. If a practical and fuss-free solution can be rolled out for the execution of the patient tagging process, perhaps it would improve the compliance rate of the end-users involved. Issuing and tagging of the device during the initial patient administration process may be a feasible solution.
In a hectic work environment such as the ED, there are a myriad of situations in which congregation is both inevitable such as when more attention is required for sicker patients and where medical interventions are time sensitive. In these cases, social proximity is necessary and unavoidable. Hence, the role of the beacon in prompting physical distancing may be less appropriate yet may still be a good reminder for individuals interacting in time-periods after their respective shifts.
4.6. Future Enhancements
- (1)
Battery Life
Future enhancements could consider streamlining the end-to-end assignment of devices further as well as improving the battery-life of the hardware itself to obtain more accurate data within the ED. While Phase 2 introduced the process of self-tagging instead of manual administrative delegation, which simplified and improved the accuracy of data, there is still more potential to streamline the method of device delegation further to the point of having no issues at all. This could be done by improving the recharging process of the hardware, which is manual at the present moment, involving extra time for admin staff in Phase 1, and individual users in Phase 2. In addition, reducing the limited battery life of the hardware would remove several of anomalies in the data with respect to the time and clusters of interaction discussed previously.
- (2)
Visual, Audio, and Tactile Cues
Future enhancements to the hardware solution itself could incorporate visual, audio, or tactile cues to notify and alert individuals directly on possible social distance violations. For example, if an individual is within 1 m of another individual, the hardware could take the extra step of notifying the individuals in a discrete manner so that social distancing compliance may be achieved instead of merely tracked in the event of a COVID-positive case. However, as mentioned previously, proximity may be unavoidable in intermediate care and resuscitation areas, and these cues may be a source of distraction to patient care. Hence, future enhancements could consider the “activation” of cues in only specific areas that elicit high traffic and may not require it, such as the pantry within the ED.
5. Conclusions
The study was key in evaluating the effectiveness of this “real-time” standalone solution in a real-world outbreak setting. In addition to resolving numerous issues experienced with alternative solutions such as data privacy and security, and Bluetooth discrepancies, the key features of the hardware include a contact tracer platform, real-time time-day trends, as well as location trends within the ED. Despite some technical, usability, and logistical issues, the study suggests that this hardware solution is a robust and effective location tracking, contract tracing, and safe distancing tool within the ED setting that must be explored further.
As no patients or staff that were tracked were identified as COVID positive throughout the study, there was no case in which the contact tracer platform needed to be used for contact tracing: identifying healthcare workers or other patients who were in proximity or spent a long time interacting with a given positive patient. While in the context of this study, this may have been a potentially useful and efficient contact tracing tool, and it proved to be useful and clinically validated in a separate study on foreign workers in a dormitory setting in Singapore that is in the process of being reported [
17].