Abstract
A systematic review of the literature investigating the effects of the COVID-19 pandemic on psychological and psychosocial factors was completed. Published literature was examined using electronic databases to search psychosocial factors such as beliefs and media persuasion, social support, coping, risk perception, and compliance and social distancing; and psychological factors as anxiety, stress, depression, and other consequences of COVID-19 that impacted mental health among the pandemic. A total of 294 papers referring to the first wave of the COVID-19 pandemic (December 2019–June 2020) were selected for the review. The findings suggested a general deterioration of mental health, delineating a sort of “psychological COVID-19 syndrome”, characterized by increased anxiety, stress, and depression, and decreased well-being and sleep quality. The COVID-19 effect on the psychological dimensions of interest was not the same for everyone. Indeed, some socio-demographic variables exacerbated mental health repercussions that occurred due to the pandemic. In particular, healthcare workers and young women (especially those in postpartum condition) with low income and low levels of education have been shown to be the least resilient to the consequences of the pandemic.
1. Introduction
As of 21 February 2022, SARS-CoV-2 has infected more than 423 million individuals worldwide and caused more than 5.8 million deaths [1]. During the first months of 2020, the globe was under lockdown: the confinement measures which constituted an emergency protocol imposing restrictions on the free movement of persons [2]. These restrictive measures had various effects on people’s daily life, and physical and mental health. This review arose from the need to summarize and schematize the many psychological publications related to the first wave of COVID-19, as they appear to be very large. The authors aim to provide a complete review of the literature on the psychological impact that the first wave (December 2019–June 2020) of COVID-19 had on a global level, to identify which factors related to the pandemic were most impacting people’s mental health.
The results of the review regard the first wave of the pandemic (2019–2020). Therefore, this impact is unrepeatable in the future, also regarding resilience and transformative resilience. The findings could indicate a specific structure that could be attributed to a “psychological COVID-19 syndrome”, characterized by symptoms relatable to anxiety, depression, stress, less wellbeing and more sleep problems.
We chose to analyze different variables of mental health studied in previous pandemics (Ebola, SARS, MERS, Novel influenza A, Equine influenza, etc.), in addition to psychosocial dimensions which proved to be essential to mitigate the spread of Coronavirus [3,4,5,6,7,8,9,10]. The authors decided to build on the dimensions considered in previous pandemics to observe whether these variables were also present in the current COVID-19 pandemic. For easy reading of the review, we divided the work into two sections: (1) Psychosocial Variables, and (2) Observables related with Mental Health.
For this systematic review, 294 articles published between December 2019 and June 2020 were analyzed, resulting in a large, heterogeneous literature, with a total sample of 732,852 subjects from more than 30 countries. Although the collected works are often based on non-representative samples, their large number and the possibility of cross-referencing the results common to these studies allows on the one hand to overcome the possible problem of unrepresentativeness, and on the other to grasp the existence of an effect, assuming the heterogeneity of the samples used by these works.
The authors hypothesize that from this systematic review can be derived the psychosocial and psychopathological areas most affected by the COVID-19 pandemic, and likewise, that can be delineated a profile of the most vulnerable individual to these types of issues. So, in this perspective, this review can be useful both for future research and for the current management of the pandemic emergency.
2. Review Methodology
In this section, details about the systematic review approach are provided. We relied on an adapted version of the systematic qualitative review approach by Higgins and colleagues [11]. The authors searched all the papers that included the relationship between COVID-19 and psychological variables of interest.
As a first step, we asked academic information specialists to search for COVID-19 scientific papers that fulfilled our inclusion criteria. These were: written in English language; published between December, 2019 and June, 2020; being an empirical study, project report or review; published in a scholarly peer-reviewed journal and/or conference proceedings; those related to psychological dimensions and mental health (i.e., psychological disorders, risk perception, beliefs, coping, compliance, social support).
The specialists completed their task consulting the databases of PsycInfo, PsycArticles, PubMed, Science Direct, PsyArXiv, NCBI, medRxiv, and Elsevier repository. The authors on their part contributed to the search by consulting Google and Google Scholar to increase the chances of identifying the widest range of sources possible. The consultation took place between April and May 2020. A total of 7381 sources were considered. Subsequently, the authors’ results were compared with those of the experts, and duplicates were removed. To select the papers, search terms such as “COVID-19”, “Psychology”, “Psychological”, “Psychological effect”, “Mental health” were included in the research. For a more complete list of all the search terms, see Appendix A. Based on the inclusion criteria, only 480 sources were accessed as full-text: 303 papers were eligible since they met the inclusion criteria.
At the title review stage, sources were most commonly rejected because they fulfilled two or more of the following exclusion criteria: were only citations, commentary, or books; were papers published before 2019; those not related to the psychological dimensions and mental health (i.e., psychological disorders, risk perception, beliefs, coping, compliance, social support); articles not in English language. At the abstract and full paper review stages, papers were most commonly rejected for: demonstrating no inclusion of a psychological variable, having incomplete results, using qualitative measures and articles where data analysis was not suitable for the systematic review process (e.g., lack of descriptive statistics, no correlation coefficients provided for the variables of interest).
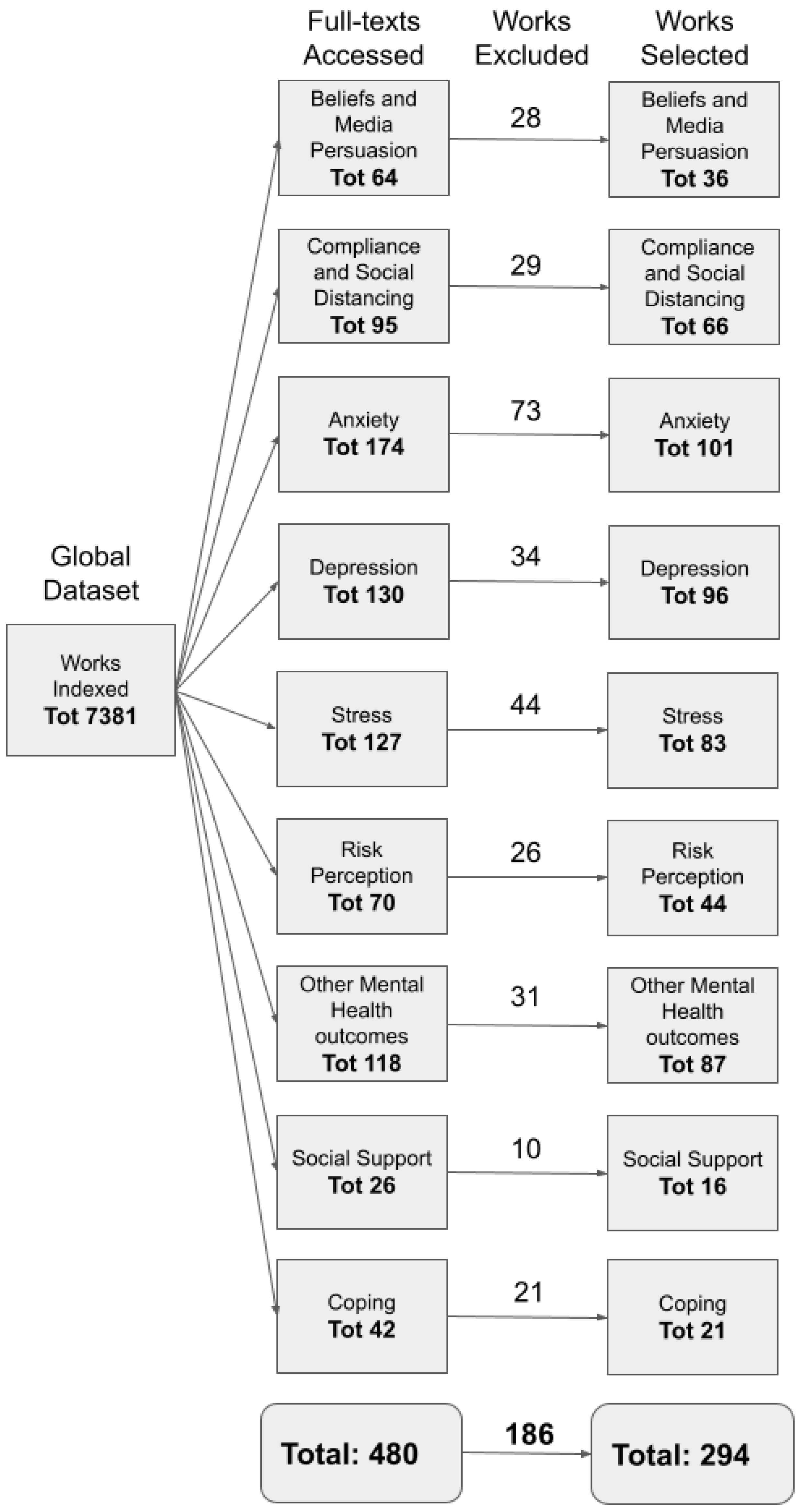
A flow diagram of the systematic search is shown in Figure 1.
Figure 1.
Diagram showing the information flow through the review: the number of works identified, included and excluded.
This review is divided into two main sections: (1) Psychosocial Variables, and (2) Observables related to Mental Health. The first section is in turn divided into different subsections: Beliefs and Media Persuasion, Social Support, Coping, Risk Perception, and Compliance and Social Distancing. The second section is in turn divided into different subsections: Anxiety, Stress, Depression, and Other consequences of COVID-19 on Mental Health. These are the dimensions that emerged most during the analysis of the literature about COVID-19. The subdivision in these paragraphs was formulated to make reading easier. Every subsection is divided into “Introduction ”, “Measures”, and “Results”.
Postponed to the “Discussion” paragraph is the possibility of connecting in a single design all the results emerging from the various sections, towards a definition of a psychological COVID-19 syndrome. For an easier reading, you can consult Table A1 (placed in the Appendix A) that contains the main information of the papers analyzed.
8. Mental Health Variables: Anxiety
8.1. Introduction
We chose to analyze anxiety because research on past epidemics, like SARS, MERS, swine flu and Ebola, revealed a wide range of negative psychosocial impacts, of which anxiety was one of the main outcomes [7,37,183,184,185,186]. In particular, the quarantine had a huge impact on people: when comparing quarantined versus non-quarantined individuals, the first were more likely to show psychological distress and to have a high prevalence of psychological symptomatology [187]. A recent study about the COVID-19 emergency indicated that “53.8% of respondents rated the psychological impact of the outbreak as moderate or severe; (…) 28.8% of respondents reported moderate to severe anxiety symptoms” [186].
Additionally, uncertainty may exacerbate the already existing detrimental effect of the pandemic on anxiety [188]. Anxiety is not just an outcome of the pandemic but could also have repercussions on behaviours implemented during the pandemic.
In the work of [185], it emerged that high and low anxiety individuals [189] behaved differently on some specific COVID-19 related conducts. High anxiety individuals may cause crowding (and thus increase the likelihood of infection), but at the same time they may be reluctant to seek medical assistance for fear of transmission, whereas individuals with low anxiety were found reluctant to comply with preventive measures [185].
8.2. Measures
The already validated questionnaires used to measure anxiety are reported in Table 11.

Table 11.
Validated tools to measure “Anxiety”. In the table are reported the psychological tools adopted by the studies taken into account, their internal consistency (reliability), and their frequency.
Only four papers decided to use ad hoc measures for anxiety [16,41,161,211].
8.3. Results for Anxiety
Fitzpatrick et al. (2020) [212] and Guo et al. (2020) [213] highlighted high and medium levels of anxiety in the USA and China populations. Pandemic related distress was associated with anxiety: specifically, perceiving symptoms of COVID-19 (fever, cough, etc.), loneliness and stress increased anxiety levels [214,215].
Following protective measures, like mask-wearing and handwashing, were related to lower anxiety levels [23,168,216]. Nonetheless, adopting these protections appeared as not enough for drastically lowering anxiety; instead, adhering to social isolation policies appeared as essentials to reduce anxiety levels [38].
Anxiety was also increased by social contexts. People who knew someone infected by COVID-19 [7,58,110,217,218,219,220] reported a higher level of anxiety. Anxiety was also higher in people with a positive COVID-19 diagnosis [201,221,222,223]. Unexpectedly, longer periods of lockdown did not lead to high anxiety levels [119,224,225].
Individuals with a higher level of COVID-19 knowledge were more likely to report a higher level of anxiety [16,23,41,157], but, despite this, up-to-date and accurate health information, along with being aware of the risks of the pandemic, were protective factors against the pandemic’s psychological burden [186,226]. The exposure time to COVID-19 information was associated with greater anxiety levels [211,216,226,227], as well as worries and concerns about COVID-19 [37,118,223,228,229].
Risk perception also played a role in shaping people’s anxiety in the pandemic scenario. Indeed, people who perceived a high risk and a realistic high threat reported higher levels of anxiety [6,96,122,133,230].
Anxiety was also studied and investigated in some specific populations, like medical-care workers. Several papers analyzed samples composed healthcare personnel (doctors, nurses, physical therapists etc.), finding a high prevalence of anxiety symptoms [70,157,220,222,231,232,233,234,235]. Although, according to [8], there was no significant difference in anxiety levels among doctors, nurses and pharmacists. Instead, the essential aspect that appeared to affect healthcare personnel anxiety levels is the time spent in the hospital [72]. In addition, healthcare workers who believed the virus was developed in a lab reported higher levels of anxiety [235].
In conclusion, several studies found that lower anxiety was associated with a higher life satisfaction [236,237], higher crisis management appraise [238], higher perceived level of health [7], a higher number of leisure activities [7], more physical activity and exercise [226,239,240] and resilience [24,133,229]. Instead, higher anxiety was associated with loneliness [24], bad distress tolerance [24], more significant changes in daily life [7], paralyzing worry [229], reduced appetite [229], and engagement in COVID-19 prosocial acts [64].
Anxiety levels during the pandemic were associated with age, gender, social condition, socio-demographic variables, culture and psychological variables. The results are shown below.
Age: 21 papers found a strong relation between anxiety and age [4,118,143,157,187,221,222,224,225,239,241,242,243,244,245,246,247,248,249,250,251,251]. Specifically, 16 reports claimed that younger age seems to be associated with higher anxiety [4,118,187,201,221,224,225,239,241,242,243,244,245,247,248,249,251,252,253]. Only three papers argued the opposite [222,246,254]. Instead, specific anxiety for COVID-19 was higher with older age [248].
Gender: There are numerous articles that have found a strong correlation between gender and anxiety [4,157,255,256,257]. In almost all articles, the female gender was associated with a higher level of anxiety than men [8,16,67,104,161,185,187,221,222,225,233,242,243,244,245,250,258,259,260,261,262,263]. Females reported being more influenced by anxiety and experiencing more negative emotion [161]. Just one article seems to find mixed results, reporting higher GAD-7 scores for males than females [263].
Social Condition: Several studies have shown that a higher level of education is correlated with an increased anxiety about COVID-19 [67,201], particularly individuals with a lower level of education than middle school are more anxious [224]. Other studies show that high levels of anxiety appear to be income-related: lower income leads to higher levels of anxiety [187,233,248,256].
Socio-demographic variables: Research shows that unemployment, self-employment, private sector employment, lack of formal education, family size, and paternity (>2 children) were associated with a higher likelihood of negative mental health [247]. The confidence in the physician’s ability to diagnose COVID-19 infection, the decrease in the probability of contracting it and the lower frequency of seeking information about it, because of satisfaction with the information received, have been protective factors against negative mental health, like anxiety [247]. Another protective factor against COVID-19 anxiety is living in urban areas and living with parents [58]. Instead, longer working time and more years of work increased the risk of anxiety [220,261]. Finally, living in heavily crowded areas, where the social distancing requirements are lacking, could lead to higher levels of anxiety [264]. Students, especially abroad ones [54], experienced relatively greater anxiety during the period of the epidemic [7,265], except if they considered themselves healthy [155]. Research has also observed that levels of anxiety among medical students have decreased with the introduction of distance learning [37].
Culture: Only Liu et al. [24] investigated and found significant differences possibly due to culture diversity. In their study, Asian Americans, Hispanic/Latinos reported lower anxiety levels than Whites [24].
Comorbidity: Anxiety measured during COVID-19 epidemic showed different comorbidity effects [55,56,58,67,70,221,229,262,266,267,268]. People with psychological anxiety disorders appeared more vulnerable to the impact of the COVID-19 epidemic on their mental health in terms of well-being and quality of life [220,221]. Anxiety during the COVID-19 epidemic was associated with negative affect [269], PTSD symptoms [268] and risk of postpartum depression [266,267]. The well known relationship between anxiety and sleep disorders [188] seemed to be confirmed also about Coronavirus specific anxiety. Indeed, Coronavirus anxiety levels were higher in people with sleep disorders (like insomnia) and poor sleep quality [70,99,188,227,270,271,272]. Only one article [273] found no significant correlation between anxiety and sleep disorders.
Table 12 shows information about the papers analyzed for the study of anxiety.

Table 12.
Anxiety. Summary of sources, with the number of papers analyzed, the total sample size, the provenance of the sample and the mediator variables. “MTurk” is used to indicate a sample extended worldwide.
9. Mental Health Variables: Stress
9.1. Introduction
The COVID-19 outbreak has caused public panic and mental health stress [10]. McEwen and colleagues [274] defined stress as an adaptive psycho-physical reaction in response to a physical, social or psychological stimulus, called a “stressor”. Stress-related responses are cognitive, emotional, behavioural and physiological [74,275]. During the first wave, the pandemic had an unprecedented impact on social lives around the world and can be viewed as a global stressor induced, beyond the risk for health, by the social isolation and distancing measures [276,277,278]. There is a lack of psychological literature related to epidemics (e.g., Ebola, Swine flu) or global pandemics; the last pandemic was the Spanish Flu of 1918, but there is not enough research about this [6]. The few recent studies about epidemics noted that there was increased stress due to the epidemic and quarantine [247]. Quarantine has been associated with high stress levels, depression, anxiety, irritability, insomnia, burnout, and physical symptoms [6,38,75,225,279]. Furthermore, being quarantined is associated with acute stress and trauma-related disorders, like Post Traumatic Stress Disorder (PTSD) [57,75,225,280,281,282,283]. In particular, during the first wave of COVID-19, PTSD appeared as characterized by involuntary memories of the trauma such as intrusions or nightmares, persistent avoidance of stimuli associated with the traumatic event, negative alterations in cognitions and mood that are associated with the trauma, as well as alterations in arousal and reactivity that are associated with the trauma [281,283]. Those populations who were more at risk, such as health workers, were more likely to develop this kind of disorder [10,57,225,284].
Moreover, the disruptive changes of the work market also led to higher general levels of stress [285]. For instance, many people had lost their jobs because of the pandemic, others had to work from home while taking care of the family (i.e., remote working) [7], especially teachers who were forced to rely on information and communication technology (ICT) despite their technological literacy and/or fluency [286]. In particular, this pandemic seemed to psychologically affect healthcare providers and other workers, since they were on the front line [284]. Additional factors that seem to exacerbate stress levels in the population during isolation or quarantine [287] were an incorrect perception about the transmission of the virus [288] and conspiratorial beliefs [46].
9.2. Measures
The validated questionnaires used to measure stress are reported in Table 13.

Table 13.
Validated tools to measure “Stress”. In the table are reported the psychological tools adopted by the studies taken into account, their internal consistency (reliability), and their frequency. 1: Modified version of PTSD Checklist for DSM-5 [289]; 2: adapted from the 14–item Perceived Stress Scale [290].
9.3. Results for Stress
The COVID-19 pandemic and the consequent lockdown period increased the level of stress in the population [5,7,78,259,307], and this was likely to increase as the number of lockdown days increased [287,308]. Higher levels of stress were associated with: loss of job/education [89,309], having to go out to work [187], having an acquaintance infected with COVID-19 [89,187,247], likelihood of contracting the virus [310], more hygiene behaviors [247,256,310], history of stressful situations [187], medical problems [74,187], risk perception and COVID-19 specific fear/worries [10,74,133,247,259,310], perception of changes in life [74], dysfunctional coping strategies (i.e., denial, substance use, behavioral disengagement) [55,74,245], loneliness [10], perceiving physical symptoms as COVID-19 [215], belief in conspiracy theories [46], low distress tolerance [10], low social support [10,55,276], and decreased sleep quality [271]. Protective factors for stress were associated with: resilience [259,311], greater social connectedness [276], seeking information on COVID-19 [74,89,183], up-to-date and accurate health information [186], functional coping styles (i.e., planning, religion) [74,245], internal locus of control [74], perception of being able to avoid the virus [74], satisfaction with life [237], personality traits (high agreeableness, high conscientiousness, high emotional stability and high extroversion) [74], less exposure to COVID-19 [233,273], and agreed/confidence with government measures [186,216,277]. Moreover, individuals who reported high levels of optimism, and reported that the lockdown situation also had positive aspects, had lower stress levels [277,312,313].
Interestingly, using the internet was positively associated with higher levels of stress [183,226,269,309]. For example, some studies showed that the use of social media (during the pandemic) was associated with symptoms of PTSD [183], because on these platforms there was information available that is not necessarily based on well-founded facts [226]. This could lead to confusion and uncertainty among individuals about the preventive measures taken to reduce the spread of the COVID-19 virus. The minimisation and unacceptability of the severity of the COVID-19 pandemic has been associated with stress [226]. When people reported more stress related to COVID-19, they felt less satisfied, less engaged, and more conflicted in their relationships [181]. For example, one study [7] saw how those who had a relationship without cohabitation perceived more individual and relational stress during lockdown [7].
The category of healthcare workers reported higher levels of stress [127,220,221,254,260,268,281,288]; and in particular, females reported to be more stressed than males [168,220,314]. According to [87], the main factors associated with stress were: concerns for personal safety, concerns for their families, and concerns for patient mortality; the factors that reduced stress were: correct guidance, and use of protective behaviors for prevention.
Furthermore, other studies showed correlations between stress and low social support [70], lack of psychological therapy [315], poor sleep quality [314], hyperarousal symptoms [314], risk perception [127], worries and knowledge about COVID-19 [127].
Finally, different studies showed that stress was strongly associated with symptoms of burnout (i.e., depersonalization, emotional exhaustion) [233,268,316]. In particular, females [279,284], those who were exposed to COVID-19 patients [285,316], and long-term workers [279,284] reported high levels of burnout.
Stress levels during the pandemic were associated with age, gender, social condition, culture and comorbidity. The results are shown below.
Age: results showed a significant impact of age on stress levels [74]. A lot of papers reported higher stress and PTSD levels among the younger individuals rather than the older one [7,75,118,187,243,247,258,260,277,308,317,318,319,320]. These results are not found within the medical staff sample [87].
Gender: numerous articles have reported a significant relation between gender and stress, with females reporting higher levels of stress and PTSD than males [10,74,186,187,220,221,225,237,242,243,247,252,259,260,277,281,282,309,317,319,320,321,322], in particular, women who have been in direct contact with a COVID-19 patient [260], or those who have a recent exposure history in Wuhan [282]. Accordingly to Newby and colleagues [310], not only women, but also those who identify as non-binary or with a different gender were associated with higher self-reported stress. Finally, Cai and colleagues [87] found that factors that could reduce stress (i.e., correct guidance and effective safeguards for prevention from disease transmission) had a larger impact on females than males.
Social Condition: people with lower education experienced higher levels of stress [74,252]. Regarding the difference between occupations, those who had undergone the greatest change in work, like medical staff and teachers, showed themselves as the most stressed [275,286,288]. Indeed, teachers and healthcare workers continued to work in emergency circumstances. Unemployment and discontinued working activity (working more) were also associated with higher stress [7,225,247,309]. Finally, lower incomes [56,233,247], student status [186,265,269,308,323], marital status [247,317], large families [74,317], and more years of working [220] were associated with more stress.
Culture: Geographical differences in the effect of the pandemic were few and fragmentary, but are reported below. Italian, Chinese, Nigerian and Aboriginal populations reported high prevalence of stress symptoms [231,280,310]. Australians were more stressed than the Chinese population, but less than Italians [256]. The Austrian population was less stressed than the Chinese population [226].
Comorbidity: During the COVID-19 pandemic, a significant positive correlation was observed between stress and depression [251,309,312], anxiety [251,312], sleep [283], physical illness [220,262,310,320,324], somatization [312], and history of mental disorders [220,259,310].
Table 14 shows information about the papers analyzed for the study of stress.

Table 14.
Stress. Summary of sources, with the number of papers analyzed, the total sample size, the provenance of the sample and the mediator variables. “MTurk” is used to indicate a sample extended worldwide.
10. Mental Health Variables: Depression
10.1. Introduction
Depressive disorder affects thoughts, emotions, and physical health to varying degrees [325], and it often manifests as low mood, slow thinking, decreased activity, and impaired cognitive function [253]. The consequences are quite serious, ranging from interruption of interpersonal relationships to lifelong mental illness and suicidal behavior [78,253,312,326]. Previous public health pandemics have been linked to an increase in mental health problems. For example, Ebola, SARS, MERS, novel influenza A, equine influenza outbreak seemed to be associated with higher levels of depression [4,6,157]. In line with previous epidemics, the COVID-19 pandemic showed a similar effect on depression [212,222,223,272,304]. In particular, quarantine and social isolation, but also the strict prevention and control requirements, and the patients’ lack of communication with the outside world, were associated with higher rates of psychological depressive symptoms [78,185,187,214,216,223,245,251,321,327].
The pandemic not only elicited symptoms of psychological distress in people with no previous history of depressive symptoms, but also worsened them in people with a history of psychiatric disorders such as depression [78,326]. Another source of depression symptoms was individuated by the literature in the constant exposure to information about COVID-19 [185,216], combined with the uncertainty of the situation [185,251,312]. Just one of 97 papers did not capture effects of the pandemic on depression levels [214].
10.2. Measures
The already validated questionnaires used to measure depression are reported in Table 15. Only two studies used ad hoc questionnaires to analyze depression [328,329].

Table 15.
Validated tools to measure “Depression”. In the table are reported the psychological tools adopted by the studies taken into account, their internal consistency (reliability), and their frequency.
10.3. Results for Depression
The influence of COVID-19 on depression levels is not solely attributable to the factors outlined in the introduction. There were a number of dynamics that still impact depression and were increased during the pandemic [6,212,259,310,328]. Among these factors were those related to aspects strictly connected with COVID-19 [24,111,133,157,214,215,220,225,240,243,269,345,346,347], risk perception and its reactions [96,111,129,133,143,216,247,256,309], low quality of life [55,157,214,243,259,312], and addictions [220,241].
Pregnancy was another area impacted by COVID-19, especially when it concerned depression, due to its nature as a special, but also critical, moment in womens’ lives [267]. In particular, WHO reported that about 10% of pregnant women experience a mental disorder, primarily depression [267], whose likelihood has increased during the COVID-19 pandemic [266,348,349]. Furthermore, for both pregnant women and their husbands, fear of COVID-19 was significantly associated with their depression level [191].
As for the COVID-19 pandemic effects on medical staff, there is some agreement between scholars. Some works highlighted that medical staff particularly suffered from the COVID-19 pandemic in terms of depression symptoms, due also to the increased work-related risks and workload [4,8,220,222,254]. In particular, medical staff members were more likely to have an impairment of their attention, cognitive functioning, and clinical decision-making [220]. Some others found that healthcare workers were at risk to develop depression [10,213,217,219,220,231,232,235,242,254,262,268,270,350]. However, other papers found the contrary [221,260], thus suggesting that the effect of the pandemic on the depression of health workers can be mediated by factors such as: longer average working time, more time in contact with COVID-19 patients, spending more time thinking about COVID-19, and spending more time searching for coronavirus information [217,219,270]. Some protective factors individuated specifically for healthcare workers were: maintaining contacts through social networks [265], individual resilience [281], distress tolerance [281], social support [65], and having a meaning in life [312].
Regarding the general population, literature identified a number of protective factors towards depression. In particular, resilience [24,133,259], sexual satisfaction [236], pandemic-related prosocial experiences [64], hope and zest [183], positive affect [96,243,351], confidence about overcoming COVID-19 pandemic [157,216,352], living farthest from the epidemic [273], high levels of family support [24,307], credibility of updates [216,247,352], home self-quarantine [269,352], having a garden [245], continuing to work [245], physical exercise [239,307], meaning in life [312], trust in medical staff [216,247], taking prevention measures [168], and optimism [307,312] were associated with lower depressive symptoms.
Depression levels during the pandemic were associated with age, gender, social condition, culture and psychological variables. The results are shown below.
Age: Age seemed to be significantly associated with depression [157]. Younger people reported a higher prevalence of depressive symptoms during the COVID-19 pandemic [4,7,184,221,225,235,239,242,243,245,247,248,249,258,347]. Conversely, older people showed lower depression levels [7].
Gender: The findings showed that women had higher levels of depression than men [4,8,10,67,157,186,187,220,221,222,225,239,242,243,247,254,255,258,259,260,262,272,307,321,347], in line with pre-COVID-19 literature [353,354]. A prolonged exposure to domestic hostility due to quarantine worsened the symptoms [259]. Just one research found the contrary [310].
Social Condition: An association between sociodemographic variables and depression was captured: lower levels of education, unemployment, lower income, living in urban areas, living in crowded areas where it is impossible to maintain social distance, not having a child, having an acquaintance infected with COVID-19 have been associated with higher levels of depression [6,8,67,185,187,226,233,245,247,248,253,264,347]. Remote working was associated with lower depressive symptoms [245], while being a student seemed to be significantly associated with higher levels of depression [4,8,186,254,265,310].
Culture: Some differences related to culture were found: during the COVID-19 pandemic, Chinese, Asian Americans, and Israeli Arabs were at low risk of present depressive symptoms, compared to Spanish, White Americans, and Israeli Jewish [7,24,355]. According to Gobbi and colleagues [326], Turkish had the lowest level of depression, compared to Canadians, Pakistanians, and Americans [326].
Comorbidity: Anxiety [38,96,223,345], stress [214,312], sleep difficulties [223,271], history of mental health issues and chronic illness [220,221,255,259,262,268,310,347,356] were consistent predictors of higher depression during COVID-19 pandemic. These results also are in line with pre-COVID-19 literature [353,354].
Table 16 shows information about the papers analyzed for the study of Depression.

Table 16.
Depression. Summary of sources, with the number of papers analyzed, the total sample size, the provenance of the sample and the mediator variables. “MTurk” is used to indicate a sample extended worldwide.
11. Mental Health Variables: Other Consequences of COVID-19 on Mental Health: Wellbeing, Psychological Distress, Fear of COVID-19 and Sleep
11.1. Introduction
The COVID-19 pandemic, as well as previous epidemics (such as SARS, H1N1, Ebola virus), have caused other psychological consequences with respect to those considered in the previous paragraphs, both on individuals affected by these diseases, as well as on the non-infected ones [3,5,8,9]. In particular, four constructs about Mental Health and Quality of Life domains will be examined below due to their connection with the COVID-19 outbreak.
Wellbeing: Living under the threat of the pandemic and its consequences represented a significant challenge to wellbeing [329,350,357]: indeed, the first wave of the COVID-19 pandemic was linked to worsening in wellbeing and mental health [9,329,358]. The sudden outbreak of COVID-19 and the preventive measures had a strong impact reducing the quality of life of the population [5,93]: forcing a drastic change in habits and routines [359], reducing social contact [329], and restricting freedom of movement as a consequence of social isolation [5]. Both the sudden outbreak of a new and unknown virus and the measures adopted to decrease its spread have had a strong impact on the mental health and the psychological well-being of the population [5].
Psychological Distress: Variables positively associated with psychological wellbeing were negatively associated with psychological distress [360]. APA defined psychological distress as a set of painful mental and physical symptoms that are associated with normal fluctuations of mood in most people [361]. Furthermore, Arvids Dotter and colleagues [362] defined psychological distress as a state of emotional suffering associated with stressors and demands that are difficult to cope with in daily life. When facing something new or unknown, such as the COVID-19 virus, a lack of effective treatment can lead to psychological distress in health care professionals as well as in patients [362]. The risk of getting infected, the lockdown scenario, and the consequent changes in habits may contribute to feelings of loneliness (connected to social isolation) and psychological distress [5,359,363].
Risk factors associated with greater distress were: not having an adequate supply (of food or goods of first need) [364], quarantine [364,365], low level of health perception [364], risk control [364], risk perception [364], low social support (family) [363], negative coping styles [75], delay in returning to work and school [365], negative thoughts [366], being close to potential risk groups [9], and work environment [3]. In the pandemic, healthcare workers are at high risk of psychological distress [357]: they were worried about overtime work, the stigma of the illness, and the health of their families and themselves [279]. While, protective factors associated with distress were: taking personal prevention/protection and clothing disinfection measures, clear communication of directives, and precautionary measures [364].
Fear of COVID-19: Fear is a negative emotion accompanied by excessive levels of emotive avoidance concerning particular stimuli, and it is an adaptive danger response [133,178,367]. It is associated with clinical phobias [178], social anxiety [178], risk perception [367], health anxiety [367], bad psychological and physical health [133], use of social media [367], high neuroticism and worries [366]. However, fear to some extent can be helpful for people in terms of leading them to comply in protective behaviours against COVID-19 [107,133,178].
In particular, it is also necessary to define the fear of COVID-19, that is based on four basic pillars: fear of the body, significant others, uncertainty, and action/inaction [9,368]. Especially the uncertainty led to changes in habits that are associated with decreased wellbeing and increased psychological distress [9,178].
Sleep: Finally, sleep is an indispensable physiological process in maintaining physical health [369] and sleep quality is a key indicator of health [70]. The stressful situations caused by the COVID-19 pandemic appeared to enhance symptoms such as sleep suppression, increased wakefulness, insomnia, difficulty falling asleep, maintaining sleep, waking up early, daytime sleepiness, nightmares and daytime dysfunction, and other sleep-related disorders [69,70,188,273,283,369]. On the other side, social support appeared to reduce stress and consequently improve sleep quality, and also enhance wellbeing [70].
11.2. Measures
Wellbeing: The validated questionnaires used to measure wellbeing are reported in Table 17.

Table 17.
Validated tools to measure “Wellbeing”. In the table are reported the psychological tools adopted by the studies taken into account, their internal consistency (reliability), and their frequency.
Different research used ad hoc questionnaires to analyze wellbeing [17,38,122,212,233,329].
Distress: The validated questionnaires used to measure distress are reported in Table 18.

Table 18.
Validated tools to measure “Distress”. In the table are reported the psychological tools adopted by the studies taken into account, their internal consistency (reliability), and their frequency.
Different research used ad hoc questionnaires to analyze distress [8,45,90,166,310,363,366].
Fear of COVID-19: The validated questionnaires used to measure the fear of COVID-19 are reported in Table 19.

Table 19.
Validated tools to measure “Fear of COVID-19”. In the table are reported the psychological tools adopted by the studies taken into account, their internal consistency (reliability), and their frequency.
Different research used ad hoc questionnaires to analyze fear [37,107,133,212,277,390].
Sleep: The already validated questionnaires used to measure sleep are reported in Table 20.

Table 20.
Validated tools to measure “Sleep”. In the table are reported the psychological tools adopted by the studies taken into account, their internal consistency (reliability), and their frequency.
Different research used ad hoc questionnaires to analyze sleep quality [69,188,256,269,395].
11.3. Results for Other Consequences of COVID-19 on Mental Health
The influence of COVID-19 on the levels of wellbeing, distress, fear, and sleep appeared as mediated by different factors that are reported below.
Wellbeing: The initial stages of the pandemic had minimal detrimental effects on wellbeing [68]. Several studies found that quarantine [310,359], living in regions with higher COVID-19 prevalence [309], loneliness [214,329,396,397], risk perception [3,122], conspiracy beliefs [45], suspected infection [71], spending time searching for information about COVID-19 [71], searching information on social media [3,359], not practicing prevention measures [3], fear of COVID-19 [9,17,397,398], intolerance of uncertainty [9], rumination [9], exhaustion [397], internet addiction [357], work overload [398], stressful life events [357], negative coping styles [71,86,93], and substance use [93] were associated with lower levels of mental wellbeing. On the contrary, physical exercise [239,399], positive coping strategies (e.g., emotional support, humor, religion) [8,71,77,93], optimistic attitude [35] (Imtiaz et al., 2020a), hope [106,183,329], resilience [106,329], perception of effective protective measures [397], satisfaction at work [397], good social support [71,357,398], and higher self-efficacy [3,398] were associated with an increase of wellbeing levels.
Regarding healthcare workers, it is demonstrated that their workload had a significant negative impact on their psychological wellbeing [279,400].
Distress: Greater mental distress was evident post lockdown [8,214]. The decrease in distress during the initial phase was attributed to preventive measures (including medical support and resources to stop the spread of the virus) [304]. Among the healthcare workers, high levels of distress were found [90,397,401,402], finding also that those who believed the virus was developed intentionally in a lab reported higher levels of distress [401].
Fear: Regarding the fear of COVID-19, it was associated with psychological distress and life satisfaction [170,228,403]: this was a mediating factor between intolerance of uncertainty and wellbeing [9]. According to Mertens and colleagues [367], there are four predictors of the fear of COVID-19: health anxiety, regular media use, social media use, and risks for loved ones [367]. Nevertheless, COVID-19 fear has been shown to predict positive changes in behavior (social distancing, hand hygiene) [107,170,178,390]. Furthermore, people who had higher levels of risk perception experienced more fear, and they were more inclined to develop a mental disorder [133,228]. Finally, between healthcare workers there was also a negative correlation between fear of COVID-19 and wellbeing [279,400,403,404].
Sleep: Reporting sleep-related functional problems was significantly associated with higher distress [397]. During quarantine, sleep timing markedly changed: people went to bed and woke up later, and spent more time in bed, but, paradoxically, also reported a lower sleep quality [271]. The difficulty in falling asleep was the result of an increase of “presleep cognitions”, which could probably lead to PTSD [283]. According to Di and colleagues, and Bai and colleagues [395,405], even children reported sleep difficulties during the COVID-19 pandemic [395,405]. In particular, sleep disorders were higher in COVID-19 confirmed cases [223], and those who had adversity experiences/worries [69], no exercise [65], and lower social support [65,69].
According to different studies [65,184,263], healthcare workers had the highest rate of poor sleep compared to other occupations [65,184,263]. They reported more difficulty in falling asleep [314], short sleep duration [314], and more sleep disturbance like insomnia [231,314].
Wellbeing, distress, fear and sleep levels during the pandemic were associated with age, gender, social condition, culture and comorbidity.
Age: Several studies have shown that being younger and having negative self-perceptions about ageing were associated with increased discomfort [5,75,309,319,359,363,364,406,407]. Thus, as a result, older people with positive self-perceptions of ageing seem to be more resistant during the COVID-19 outbreak [8,86,363,397]. In contrast with these findings, only Zhang and colleagues [365] argued that age was positively associated with psychological distress [365]. Nevertheless, an effect of the quarantine was found even on young people: children and adolescents in quarantine suffered greater psychological distress than children and adolescents not in quarantine [166]. Sleep disorders were more frequent in younger people [256,288,408]. In particular, as far as COVID-19 hospitalized patients are concerned, sleep disorders are greater in people aged 50 and over [223].
Gender: Several studies showed that being female was associated with higher levels of distress, and lower levels of psychological wellbeing [5,86,183,233,239,309,319,363,364,397,406,407,409,410]. Finally, fear of COVID-19 was more severe in females than in males [411]. Most of the papers found the prevalence of sleep disorders as insomnia [225,408] or poor sleep quality was higher among women [256]. Only Zhpu and colleagues [263] found conflicting results: in their paper, the sleep quality of men was worse than that of women [263].
Social Condition: People who were unemployed [309,407,409] or who had just lost their job reported higher psychological distress levels [406]. As for the workers, faculty, post-doctoral researchers and students showed lower levels of wellbeing than staff members [233,345]. Another significant association was found with marital status: those who were married had higher levels of wellbeing than those who were divorced because they had more social contacts and social support [318]. A relationship emerged between job loss, being single, and sleep disorders [69,256]. In particular, unemployed mothers or mothers who continued to work outside were more likely to suffer from sleep disorders than those who continued working at home or stopped working during lockdown [405].
Culture: Only one paper investigated cultural differences. According to Kimhi and colleagues [355], Arab respondents expressed a significantly higher level of COVID-19 distress compared with Jewish ones, who, on the contrary, reported higher levels of well-being and resilience [355].
Comorbidity: Having a background illness [239,310,324,398], depression [214,350], anxiety [214,329,350,412], stress [214], burnout [397], sleep problems [397], alcohol abuse [350], and OCD [38] were found to increase psychological distress. For what concerns fear, this was significantly related to depression [133,327], anxiety [133,234,327], specific phobias [327], stress [133,277], health anxiety [228], and general poor mental health [212]. PTSD [283,314], anxiety [70,188,223,256,269,271,272,408], physical dysfunctions [223], stress [70,256,269,271,369], depression [256,269,271], and general mental illness [69] were associated with sleep problems.
Table 21 shows information about the papers analyzed for the study of Wellbeing, Psychological Distress, Fear of COVID-19 and Sleep.

Table 21.
Other consequences of COVID-19. Summary of sources, with the number of papers analyzed, the total sample size, the provenance of the sample and the mediator variables. “MTurk” is used to indicate a sample extended worldwide.
12. Discussion
This review aimed to explore the impact of the first wave of COVID-19 on people, analyzing different psychological and psychosocial dimensions. To identify the domains impacted by COVID-19 we relied on previous pandemic literature (e.g., Ebola, SARS, MERS, Novel influenza A, Equine influenza), and chose to reanalyze them in the current one. The analysis of the results revealed that the dimensions most impacted by COVID-19 among psychosocial variables were: beliefs about COVID-19, coping strategies, risk perception, social support, and compliance and social distancing.
In particular, regarding the three fundamental moderators about beliefs and media persuasion (attitudes, knowledge, and finding news on social networks) the analysis of works showed that, although some attitudes were optimistic (e.g., the probability of being infected was perceived as low), most participants took precautionary measures to prevent infection [34]. On the contrary, higher levels of negative thoughts (e.g., fatalism toward the pandemic) were associated with lower behavioral intentions to comply with protective measures [36]. Furthermore, accurate knowledge about COVID-19 predicted more information-seeking behaviour, the ability to discern between true and false information, compliance with preventive measures, and showed lower panic reactions, a lower level of anxiety, and greater risk perception [25,41,126]. The major sources people used to seek information during the pandemic were TV and social media, but these also led to an increase in disinformation and a spread of fake news and conspiracy theories [16,17,43]. Regarding conspiracy theories about COVID-19, some studies showed that subjects who believed in them complied less with the suggested protective behaviours and were less likely to get vaccinated [18,51,52]. On the contrary, those whose core beliefs (beliefs that guide individuals in their identity) were less influenced by the pandemic reported to engage more in social isolation measures [38].
Beliefs about COVID-19, its transmission, and its protective measures, demonstrated to strongly influence compliance with them. In particular, low compliance was associated with belief in conspiracy theories, impulsivity, and self-centered behaviour [48,49]; instead, higher compliance with protective measures was associated with fear of COVID-19, trust in government and science, and higher risk perception [134,154,169,179].
The risk perception has shown a double effect: on the one hand, a higher risk perception induces higher levels of compliance, for example, in terms of compliance with social distancing [56]. On the other hand, however, it can lead to avoidant behaviors, such as being reluctant to seek medical assistance for fear of transmission, which can damage both the health of the individual and make the management of the pandemic more difficult, probably due to the sense of loss of control that is notoriously associated with high levels of risk perception [100,185].
Quarantine, and the COVID-19 pandemic in general, also had negative social consequences. For example, many social support networks have been interrupted: indeed, social distancing led to boredom, loneliness, social isolation fatigue, anxiety, and depression [54,135,159]. Nevertheless, social support proved to be crucial and had a positive impact on coping with the COVID-19 pandemic [56,59,66]. The results showed that positive coping strategies were correlated with less distress, fear, and general vulnerability, and higher wellbeing. In contrast, negative coping strategies (e.g., substance use, behavioral disengagement) were related to higher stress, distress, fear, and anger [77,79,88].
In addition, psychological dimensions regarding some areas of mental health, specifically anxiety, stress, depression, wellbeing, and sleep, were impacted due to the pandemic.
Restrictive measures had, in general, a protective effect on anxiety, whereas being more in contact with the virus resulted in higher levels of it. In particular, anxiety was negatively related to protective measures from COVID-19 [23,73,168], whereas it related positively to testing positive for COVID-19, being in an environment exposed to COVID-19 [58,110,219], knowing people who were COVID-19 positive [201,221,222], and having more knowledge about COVID-19 [16,23,41].
The COVID-19 pandemic was also associated with higher levels of depression, both in people with a history of psychiatric disorders and in others [78,326]. These results seemed to be due to quarantine and social isolation, but also to the constant exposure to information about COVID-19 [187,223,251].
Stress appeared to be positively related to the COVID-19 pandemic and the subsequent lockdown period [7,78,307]. This effect is buffered by some protective factors, such as lower exposure to COVID-19 [233,273] and some personality traits, such as emotional stability and conscientiousness [74].
The research has highlighted some risk and protection factors of wellbeing during the pandemic. Quarantine, living in areas with high virus prevalence, overexposure to COVID-19 information, and conspiracy theories seem to decrease wellbeing; while exercise, positive coping strategies, and greater social support seem to promote it [8,399].
The pandemic also impacted the distress experienced by people, particularly of those who were already physically and/or mentally ill. Indeed, poor sleep quality was positively correlated with stressful situations caused by the COVID-19 pandemic [69,273,369].
Overall, the COVID-19 experience may be useful to derive some evidence-based insights to be applied in case of future similar emergencies. Concerning compliance, promoting a correct risk perception in the population by disseminating correct information [17,19,20,39,46,169], and suggesting effective (and positive) coping strategies [71,77,87,91,93,94], would be helpful in increasing the degree of compliance with governmental measures [39,48,76,95,102,104,105,120,123,127,134,137,139,142,148,152,169,178]. Nonetheless, compliance is also affected by the perception of the effectiveness of such restrictions. For this reason, a better media campaign, focused not on fear but on efficiency (and self-efficacy), would be ideal, in the event that an extreme situation, such as the COVID-19 pandemic, should recur [21,24,40,41,46,49,169].
As highlighted by the literature, different management of the emergency would have also led to better psychosocial and psychological outcomes. In this regard, social support appeared to ease emergency management [55,66,67,69,70,71]. Greater social support was also useful in reducing the levels of anxiety, depression, stress, that ultimately contributed to people’s compliance with the rules, fear of contagion, and management of the emergency (both collectively and individually) [55,67,70,71]. Given the widespread increase in psychological/psychiatric symptoms (anxiety, depression, stress, insomnia, and psychological distress) [4,58,64,96,225,233,243,271,319,347], countries all over the world, especially those most affected by the virus, should envisage in such situations a prompter professional support to citizens, so to prevent the emerging or worsening of symptoms.
Finally, one of the factors identified in the scientific literature as key to countering the pandemic was resilience. Resilience resulted in stress [259,311], anxiety [24,57,133], and depression [157] protective factors, and has a positive relationship with wellbeing [329]. Resilience is fundamental in enabling people to change their behaviour in response to stressful events, like the COVID-19 pandemic, which in this specific case may prevent someone from getting sick or dying. For this reason, resilience appears to promote readiness to change, which is one of the factors that enable communities to respond adequately to emergencies such as a pandemic [12,13,14].
As described above, the pandemic affected several psychological dimensions. However, its effect appeared to be conditioned by a few factors that allowed us to qualitatively describe the psychological and socio-demographic profile of the most resilient people. The factors that more frequently had a significant influence on the previously analyzed variables are: age, gender, culture, social condition, healthcare workers and workload.
As for age, younger people appeared to be less resilient: they were more affected in terms of both psychosocial variables and mental health. Young people showed greater compliance with preventive measures, probably due to their greater risk perception and knowledge of the virus. Despite their major levels of compliance, young people suffered more from the effects of quarantine, implemented negative coping strategies more often, and suffered more from psychological distress and, in general, mental health problems (i.e., anxiety, depression, stress) [24,40,73,74,143,154,157,166,347].
Similarly, women were most affected by the pandemic: they tended to comply more with the rules because they were more worried and perceived greater risks, so they mainly used emotionally focused coping strategies. Again, despite showing higher compliance levels, women were more susceptible to anxiety, depression, stress, sleep disorders, and distress than men [89,114,139,187,223,363,408]. Furthermore, post-partum depression increased during the pandemic [266,348,349]. In light of this, young women appear to be the least resilient, especially under certain conditions such as postpartum.
An effect of culture was particularly evident on beliefs: collectivist societies seemed to have more accurate beliefs about COVID-19 than individualist societies [47,49]. However, the levels of risk perception, as well as people’s mental health, apart from possible cultural factors, appeared to be affected by the levels of contagion around the world. So, it was not possible to distinguish between the two causes which one influences more the results [78,127].
Lower levels of education were associated with more fear of dying by COVID-19, perception of susceptibility to the infection and worse overall knowledge about the pandemic [47], more anxiety [247], stress [258] and depression [347].
Lower income and unemployment were associated with higher levels of anxiety [247], stress [56], depression [347], higher levels of distress [406] and more sleep disorders [69,256]. The results about compliance and social distancing were conflicting regarding income [40,101,141,149].
Finally, healthcare workers experienced an increase in workload that led to several consequences, including higher risk perception [127], higher levels of anxiety [184], stress [288], depression [222], less wellbeing [232], worse sleep quality [184], and higher risk of psychological distress [357]. Healthcare workers implemented coping strategies like religious strategies, acceptance, planning, physical activity, virtual support groups, talk therapy, and positive framing [8,87,90]. Of these factors, some (e.g., age, gender) are known to be relevant to mental health even before the pandemic; nevertheless, the papers we analyzed did not distinguish the effects of these variables before and after the pandemic.
In conclusion, the aim of the paper was to research how the COVID-19 pandemic impacted the psychological health of the global population during the first wave. In particular, we investigated which psychosocial and psychological variables were most affected, delineating a first and preliminary picture of symptoms related to COVID-19 that could be called “psychological COVID-19 syndrome”. This syndrome appeared to be characterized by an increase in stress, depression, anxiety, sleep disturbance, and distress related symptoms. Healthcare workers were the most affected by the consequences of the COVID-19 pandemic, as they found themselves on the front lines facing the virus and experienced a sudden increase in workload. In addition to healthcare workers, the results showed that people who proved less resilient were young women, with low income and low education, particularly if they were in post-partum condition. In light of this, it would be hopeful to implement prevention and aid projects for these individuals, particularly affected by the pandemic.
The number of studies about the psychological effects of the COVID-19 pandemic is increasing. However, the literature available until June 2020 was still in the early stages of maturity. Therefore, thanks to the articles published since June 2020, the “psychological COVID-19 syndrome”, hypothesized in this review through the first wave studies, could be modified or expanded. Future research should investigate the second and third waves of the pandemic so that comparisons can be made with the present research.
Author Contributions
Conceptualization, A.G. and M.D.; methodology, A.G. and M.D.; investigation, V.F., C.P. and C.S.; data curation, V.F., C.P. and C.S.; writing—original draft preparation, V.F., C.P. and C.S. and M.D.; writing—review and editing, V.F., C.P., C.S., M.D. and A.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Search Strategy: PsycInfo, PsycArticles, PubMed, Science Direct, PsyArXiv, NCBI, medRxiv, and Elsevier repository.
Searched Terms:
COVID-19 AND Psychological (Search results: 1010)
COVID-19 AND Psychology (Search results: 2160)
COVID-19 AND Risk perception (Search results: 116)
COVID-19 AND Coping strategy (Search results: 17)
COVID-19 AND Coping strategies (Search results: 91)
COVID-19 AND Personality (Search results: 314)
COVID-19 AND Personality Traits (Search results: 177)
COVID-19 AND Risk Perception (Search results: 116)
COVID-19 AND Fear (Search results: 300)
COVID-19 AND Anxiety (Search results: 626)
COVID-19 AND Psychology learning (Search results: 87)
COVID-19 AND Psychology resilience (Search results: 129)
COVID-19 AND Psychology self-efficacy (Search results: 15)
COVID-19 AND Psychology motivation (Search results: 39)
COVID-19 AND Psychology self-esteem (Search results: 15)
COVID-19 AND Psychology communication (Search results: 124)
COVID-19 AND Psychology control (Search results: 264)
COVID-19 AND Psychology optimism (Search results: 21)
COVID-19 AND Psychology workplace (Search results: 31)
COVID-19 AND Psychology Psychological (Search results: 365)
COVID-19 AND Psychology employee (Search results: 337)
COVID-19 AND Psychology sleep (Search results: 106)
COVID-19 AND Psychology depression (Search results: 84)
COVID-19 AND Psychology mental health (Search results: 798)
COVID-19 AND Psychology panic (Search results: 98)
COVID-19 AND Social distancing
COVID-19 AND Messages
COVID-19 AND Media

Table A1.
Main characteristics of the studies reviewed: reference, country, sample size, impacted dimension, and main findings (n = 294). Main characteristics of the studies reviewed.
Table A1.
Main characteristics of the studies reviewed: reference, country, sample size, impacted dimension, and main findings (n = 294). Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [136] | Germany | 419 | Compliance | People use protective measures primarily to protect themselves and only secondarily to protect others. Social distancing and washing hands are the most implemented. |
| [135] | USA | 895 | Compliance | Those with higher levels of boredom perceived social distancing as more difficult and adhered less. |
| [158] | Ireland | 500 | Compliance | Evidence to support communications that inform people about recommended behaviors. |
| [19] | USA | 1022 | Beliefs/ | Up-to-date and accurate specific health information Media Persuasion and special precautionary measures have been associated with a lower psychological impact. |
| [178] | MTurk | 324 | Compliance | “COVID-19 fear” is a predictor of a positive change in behavior (social distancing, better hand hygiene). |
| [67] | China | 144 | Anxiety, Depression, | Presence of depressive and anxiety symptoms Social Support in patients with COVID-19. Lower perceived social support appears to be related to an increase of the symptoms. |
| [137] | Brazil, Colombia, | 2285 | Compliance | Preventive measures are perceived as Germany, Israel, more effective when control levels are Norway, USA higher and the perceived risk is lower. |
| [21] | MTurk | 2176 | Beliefs/ | self-interested framing isn’t more Media Persuasion effective than prosocial framing. |
| [105] | USA | 1591 | Risk | Subjects demonstrated a growing awareness Perception of the risk and reported engaging in protective behaviors with increasing frequency. |
| [76] | China | 4607 | Risk | People with low self-control are more Perception vulnerable and more in need of psychological help to maintain mental health. |
| [34] | China | 6910 | Beliefs/ | Although attitudes towards COVID-19 were optimistic, Media Persuasion most residents took precautions to prevent infection. |
| [134] | MTurk | 525 | Compliance | Those who perceive COVID-19 as a serious threat and those who have greater faith in science are more likely to act in accordance with guidelines. |
| [145] | Italy | 894 | Compliance | Respondents were more likely to reduce their self-isolation if the quarantine extension turned out to be longer than they expected. |
| [282] | China | 2091 | Stress | The prevalence of post-traumatic stress symptoms in China one month after the outbreak was 4.6%. |
| [43] | Poland, UK | 652 | Beliefs/ | The prejudice towards foreign nationalities was Media Persuasion sensitive to the epidemiological situation. |
| [155] | China | 4607 | Compliance | Emotional and behavioral reactions were slightly influenced by the outbreak of COVID-19. |
| [163] | Germany, | 2192 | Compliance | Inducing empathy for those most vulnerable to the virus UK, USA promotes motivation to adhere to social distancing. |
| [304] | China | 52,730 | Other Consequences | Over time, levels of distress have significantly decreased. It can be partly attributed to the effective prevention and control measures taken by the Chinese government. |
| [42] | USA | 1709 | Beliefs/ | Those who are least likely to rely on their Media Persuasion intuitions and who have lower basic scientific knowledge were the worst at discerning fake news. |
| [367] | Holland | 439 | Other Consequences | Four predictors of "COVID-19 fear" were found: intolerance to uncertainty, health anxiety, increased media exposure, and risks to loved ones. |
| [130] | Italy | 1573 | Risk perception | In line with international literature, for the Italian population, too, experimental data confirmed a decrease in risk propensity of around 17.4% during the lockdown. |

Table A2.
Main characteristics of the studies reviewed, pt.2. Main characteristics of the studies reviewed.
Table A2.
Main characteristics of the studies reviewed, pt.2. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [254] | China | 600 | Anxiety, | There were anxiety in 6.33% and Depression depression in 17.17% of the sample. |
| [231] | Nigeria | 884 | Anxiety, Stress, | Results revealed significant difference in Depression, the prevalence of depressive symptoms, insomnia symptoms, Other consequences post-traumatic stress symptoms and clinical anxiety symptoms with a higher prevalence reported by the healthcare personnel. |
| [65] | China | 7071 | Anxiety, Depression, | Doctors and nurses had more psychological Other Consequences, symptoms while defending against Social Support the outbreak than before. |
| [10] | China | 1315 | Anxiety, Depression, | A total of 1315 frontline HCWs were included, of which 49.1% Stress reported a moderate to severe stress 10.7% reported moderate anxiety to severe and 12.4% reported a major depression. |
| [92] | China | 30,077 | Beliefs/Media | The COVID-19 outbreak improves Chinese people’s Persuasion, Coping, ability to see the meaning of negative experiences. Risk Perception |
| [310] | Australia | 5071 | Stress, Depression, | More than three quarters of participants reported that Other consequences their mental health had been worse since the outbreak. A small proportion reported improvements in their mental health since the outbreak |
| [167] | UK | 520 | Compliance | There are significant associations between analytical thinking and compliance. Those who use slow cognitive styles are more likely to maintain social distance and reject COVID-19 conspiracy theories. |
| [144] | USA | 501 | Compliance | Greater conscientiousness was directly associated with adherence to guidelines, indirectly associated with greater self-efficacy. |
| [217] | China | 150 | Anxiety, Depression | The participants had severe anxiety and depression. |
| [267] | Turkey | 260 | Anxiety, Depression | the COVID-19 exerted statistically significant effects on psychology, social isolation, and BDI and BAI scores. |
| [224] | China | 992 | Anxiety | A clinical significance of anxiety symptoms was observed in 9.58% of the respondents. |
| [140] | Denmark | 799 | Compliance | People’s age (positively), levels of emotionality (positively), and the dark personality D factor (negatively) explain who is most willing to accept restrictions. |
| [142] | Switzerland | 705 | Compliance | The governmental rules were more effective and stronger among the older respondents, while having a lower risk perception. |
| [406] | Australia | 551 | Other consequences | 31% reported severe psychological distress, 35% in those with job loss and 28% in those still employed but working less. Those who had significantly greater odds of high psychological distress were younger, female, had lost their job and had lower social interactions. |
| [162] | USA | 789 | Compliance | Most teens reported not engaging in pure social distancing (70%), but were monitoring the news (75%) and performing disinfectant behavior(88%) |
| [56] | USA | 500 | Depression, Anxiety, | Findings highlight the importance of social connection to Other consequences mitigate negative psychological consequences. |
| [219] | China | 882 | Anxiety, Depression | The overall prevalence of GAD and depressive symptoms were 33.73%, and 29.35%, respectively. |
| [153] | USA | // | Compliance | Quarantine rules resulted in a significant flattening of the curve for Google searches for suicidal ideation, anxiety, negative thoughts and sleep disturbances. |
| [247] | India | 873 | Anxiety, Depression, | The prevalence of depression, anxiety and stress Stress were 18.56%, 25.66%, and 21.99%. |
| [258] | Brazil | 1460 | Anxiety, Depression, | Levels of stress, depression and anxiety were all Stress predicted by gender, food quality, psychotherapy frequency, exercise frequency, work outside, education level and age. |
| [18] | MTurk | 220 | Beliefs/ | Participants who believed that COVID-19 was a hoax or a Media Persuasion bio-weapon indicated less compliance with restrictive behaviors and greater commitment to self-centered preparedness behavior. |

Table A3.
Main characteristics of the studies reviewed, pt.3. Main characteristics of the studies reviewed.
Table A3.
Main characteristics of the studies reviewed, pt.3. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [369] | China | 26 | Stress, | ISI was positively correlated with total sleep time, Other Consequences and negatively correlated with deep sleep; patient SRQ scores were positively correlated with TST, sleep efficiency and REM. SRQ-20 and sex were risk factors for insomnia. |
| [171] | USA | 503 | Compliance | Agreeableness and conscientiousness predicted endorsement of social distancing, hygiene, and the appeal of health messages in general. Dark traits (psychopathy, meanness, and disinhibition) predicted low endorsement of health behaviors. |
| [169] | MTurk | 1665 | Compliance, Beliefs/ | Some indication was found that concern about COVID-19 Media Persuasion and beliefs about others’ behavior may predict behavior change. |
| [73] | China | 1600 | Coping | The general population with a history of visits to Wuhan, those with a history of epidemics, ant those who perceived more severe impacts of the COVID-19 epidemic on their lives, emotional control, and epidemic-related dreams had a higher level of psychological distress than those with none or little of these experiences. During the C-19 outbreak, the degree of concern about media reports influenced the general population’s level of psychological distress and coping style. Media reports could influence the perception of the disease and the preventive measures implemented. |
| [139] | Norway | 8676 | Risk Perception | Increased media exposure, perception of measures as effective, and of the epidemic as a serious endeavor lead to positive predictions for health protection behavior. |
| [25] | Perù | 225 | Risk Perception | Knowledge is highly correlated with education, occupation, and age. |
| [221] | Spain | 3550 | Anxiety, | A substantial portion of the sample analyzed Depression, exhibited symptoms of depression, anxiety, Stress stress, and PTSD as measured on validated scales. In addition, respondents showed high levels of concern for their own health and that of relatives such as their parents, as well as for the social and economic situation resulting from the COVID-19 crisis. |
| [20] | USA | 955 | Beliefs/ | The effectiveness of the fear intervention was less Media Persuasion dependent on the strength of the emotional response than the prosocial intervention. In contrast, the prosocial message was more effective in increasing the willingness to self-isolate if it produced a strong, positive, emotional response. Both fearful and prosocial messages were equally effective in stimulating engagement in protective behavior. |
| [91] | China | 97 | Coping | Mindfulness reduced daily anxiety. The sleep duration of participants in this condition was less affected by increased infections in the community than participants in the control condition. |
| [22] | MTurk | 210 | Beliefs/ | Social distancing is significantly influenced by situational awareness. Media Persuasion Information sources, formal and informal were found to be significantly related to perceived understanding. |
| [248] | England | 2025 | Anxiety, | Higher levels of anxiety, depression, and trauma symptoms Depression, were reported, but not dramatically so. Anxiety Stress and depression symptoms were predicted by low income, loss of income, and preexisting health conditions. C-19-specific anxiety was greater in older participants. |
| [109] | Vietnam | 391 | Risk Perception | 11% of respondents did not actively search for information on C-19, while over 80% admitted to searching at least 2 times per day. |

Table A4.
Main characteristics of the studies reviewed, pt.4. Main characteristics of the studies reviewed.
Table A4.
Main characteristics of the studies reviewed, pt.4. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [350] | China | 1074 | Anxiety, | A higher rate of anxiety, depression, hazardous Depression, and harmful alcohol use, and lower mental well-being Other Consequences in the Chinese population following the C-19 pandemic. The findings also revealed that young people are in a more vulnerable position in terms of mental health conditions and alcohol use. Young people are at higher risk for stress (despite lower mortality) as they take information from social media. |
| [58] | China | 7143 | Anxiety | 0.9% of respondents had severe anxiety, 2.7% moderate anxiety, and 21.3% mild anxiety. Living in urban areas, family income stability, and living with parents were protective factors against anxiety. Having relatives or acquaintances infected with COVID-19 was a risk factor for increased anxiety. Economic effects and effects on daily life, as well as delays in academic activities, were positively associated with anxiety symptoms, whereas social support was negatively correlated with anxiety level. |
| [109] | Vietnam | 391 | Risk Perception | 11% of respondents did not actively search for information on COVID-19, while over 80% admitted to searching at least 2 times per day. |
| [359] | Spain | 584 | Other consequences | Participants reported an important increase in negative affect and an important decrease in positive affect during the lockdown period, compared to before the lockdown. |
| [24] | China | 10,905 | Beliefs/Media Persuasion | In general, 74.1% of participants acknowledged the effectiveness of overall control measures and it was negatively correlated with regional number of existing cases. |
| [246] | China | 194 | Anxiety, | The overall prevalence of depressive symptoms, Depression, generalized anxiety and somatic symptoms were Stress 37.6%, 32.5% and 50%, respectively. |
| [147] | China | 1920 | Compliance | All studies together confirms that intentions to wear a face covering are higher in the priming reason condition compared to the priming emotion condition. |
| [280] | Italy | 2286 | Stress | Significant correlations were found among COVID-19-PTSD scores, general distress and sleep disturbance. |
| [44] | USA | 1034 | Other Consequences | Self-reported emotions showed that women were more worried, anxious, scared, and sad than men, and these results were supported by language differences. In addition, models showed that men wrote more frequently about concerns related to their health than women. |
| [164] | China | 1011 | Anxiety | The prevalence of moderate to severe anxiety was 4–5 times its normal level in urban China. The majority engaged in all six behaviors. Confusion about the reliability of information significantly fueled public anxiety levels. |
| [120] | Vietnam | 345 | Risk Perception | Those who use medical masks have a higher perception of risk than other people. This implies that people chose to wear a medical mask before the pandemic broke out perceive a higher risk than their counterpart. People tend to perceive greater risk as they age. |
| [47] | China | 1075 | Beliefs/ | The majority of respondents appear to take the risk of C-19 Media Persuasion (on themselves, their community, and their livelihood) very seriously and are aware of ways to reduce risk. Education was an important demographic determinant, and the impact of age is likely associated with both education and life experience. |
| [220] | China | 5062 | Anxiety, | Women and those with more than 10 years of employment, Depression, concomitant chronic illnesses, history of mental disorders, Stress and confirmed or suspected family members or relatives are prone to stress, depression, and anxiety among nurses during the COVID-19 pandemic. |
| [148] | MTurk | 1439 | Compliance | Greater concern and weaker endorsement of unfounded C-19 beliefs leads to more responsible behavior. |

Table A5.
Main characteristics of the studies reviewed, pt.5. Main characteristics of the studies reviewed.
Table A5.
Main characteristics of the studies reviewed, pt.5. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [156] | China, | 4505 | Compliance | Overall levels of anxiety and adoption of positive behaviors Italy were strongly influenced by the sufficiency of information in all three countries, demonstrating that population-level risk perception, self-efficacy, and response to an outbreak can be intensified or attenuated by the quantity and quality of information provided. |
| [126] | Canada, | 1975 | Risk Perception | Cognitive sophistication-that is, the quality of one’s reasoning UK, USA was associated with lower misperceptions in all three countries. In fact, in both the United States and the United Kingdom, cognitive sophistication was a stronger predictor of resistance to misperceptions than political ideology. |
| [127] | Italy | 353 | Risk Perception | Medical personnel in Northern Italy were more stressed and anxious than those in Central and Southern Italy. HCWs reported higher risk perception, level of concern and knowledge regarding C-19 infection than the general population. |
| [227] | USA | 303 | Anxiety, | 69.0% of the sample reported moderate to severe levels of anxiety. Other Consequences Changing behavioral factors were better predictors of anxiety than psychological, situational, or informational factors, but all were significant. |
| [186] | China | 1210 | Anxiety, | 53.8% of respondents rated the psychological impact Depression, of the outbreak as moderate to severe; Stress 16.5% reported moderate to severe depressive symptoms; 28.8% reported moderate to severe anxiety symptoms; and 8.1% reported moderate to severe stress levels. |
| [413] | China | 205 | Depression | A higher prevalence of depression was found primarily in patients who had C-19 infection. |
| [213] | China | 11,118 | Anxiety, | Approximately 4.98% of respondents reported medium Depression and high levels of anxiety, while 13.47% of respondents reported medium and high levels of depression. The level of perceived disaster-related risk was influenced by a person’s level of awareness and knowledge about the pandemic. |
| [363] | Spain | 1310 | Other Consequences | Being female, younger, having negative self-perceptions about ageing, more exposure to C-19 news, more contact with relatives other than those residing in the home, less positive emotions, less perceived self-efficacy, lower sleep quality, less positive emotions, and higher loneliness were associated with greater distress. |
| [159] | MTurk | Compliance | Confinement measures are associated with aversive experiences including boredom, so adherence is likely to require self-control. | |
| [404] | China | 2299 | Other Consequences | Compared with nonclinical staff, frontline medical personnel with close contact with infected patients showed higher scores on the Fear, HAMA, and HAMD scales, and were 1.4 times more likely to experience fear and 2 times more likely to experience anxiety and depression. |
| [216] | China | 1738 | Anxiety, | Statistically significant longitudinal reduction Depression, in mean IES-R scores after 4 weeks. Moderate Stress to severe stress, anxiety, and depression were observed during the initial assessment. Hand hygiene, mask use, and trust in physicians reduced psychological impact. |
| [410] | Denmark | 2458 | Other Consequences | The psychological well-being of the general Danish population is negatively affected by the COVID-19 pandemic. Females were more affected than males by the C-19 pandemic, in agreement with findings in other countries, reporting lower levels of well-being than their male counterparts. |
| [201] | USA | 775 | Anxiety | High CAS scores were associated with C-19 diagnosis. |

Table A6.
Main characteristics of the studies reviewed, pt.6. Main characteristics of the studies reviewed.
Table A6.
Main characteristics of the studies reviewed, pt.6. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [281] | China | 285 | Stress | The study showed a higher prevalence of symptoms in females. Finally, the study demonstrated the relationship between self-reported sleep conditions and the prevalence of PTSD, showing that participants with worse sleep quality had a higher prevalence of PTSD. |
| [5] | Italy | 1639 | Stress | Of 1639 respondents equally distributed in the Italian territory, Other Consequences 5.1% reported PTSD symptomatology, and 48.2% evidenced lower psychological well-being linked to COVID-19 diffusion. |
| [272] | China | 307 | Anxiety, | The prevalence of anxiety, depression symptoms Depression, were 18.6% and 13.4%, respectively. Other Consequences PSQI scores were significant positively associate with SAS scores and SDS scores (p < 0.05). |
| [327] | Italy | 250 | Anxiety, | Analysis of the data showed satisfactory psychometric characteristics Depression, and confirmed the scale’s unidimensional properties. Other Consequences Construct validity for the FCV-19S was supported by significant and positive correlations with the HADS and SMSP-A. |
| [240] | MTurk | 219 | Anxiety, | During the initial C-19 impacted academic term (Winter 2020), Depression, individuals were more sedentary and reported increased anxiety and depression symptoms, relative to the previous academic terms and subsequent academic breaks. |
| [347] | Mexico | 6023 | Depression, | Regarding indicators of psychological distress Stress mean values for severities of depression and anxiety reached the respective cutoff scores for mild degrees, and the mean score of the IES-6 was borderline. |
| [412] | Turkey | 126 | Other Consequences | The impact of the health anxiety on wellbeing levels among mothers with autistic children is stronger than it is among mothers with normotypic children. |
| [251] | China | 515 | Anxiety, | The results showed that prevalence of anxiety, Depression, depression and PTSD was 14.4, 29.7, and 5.6%, respectively. Stress There was a significantly positive correlation between anxiety and depression/ PTSD. |
| [59] | // | Anxiety, Stress, | A systematic review that investigate the impact of the Depression pandemic on mental health and the related implications. | |
| [241] | Mexico | 561 | Anxiety, | In the initial phase of the pandemic the prevalence for anxiety Depression and depression was 50% and 27.6%, but during the lockdown was incremented by 51% and 86% respectively. |
| [59] | // | Anxiety, Stress, | A systematic review that investigate the impact of the Depression pandemic on mental health and the related implications. | |
| [8] | Pakistan | 1134 | Anxiety, | The frequency of anxiety and depression was 34% and 45%. Depression, The main sources of distress were related to adverse effects of Other Consequences, ongoing pandemic on daily life. The main coping strategies Coping adopted were religious/spiritual coping and acceptance. |
| [226] | Austria | 4126 | Anxiety, | 43.3% of the sample rated the psychological impact Depression as moderate or severe. 26.5% reported depression, Stress 20.3% anxiety and 21.2% stress. |
| [182] | USA | 1159 | Compliance | Highlighted the critical role of working memory in social distancing compliance during the early stage of the pandemic. |
| [111] | UK | 501 | Depression, | News exposure was positively associated with depression; Risk Perception perceived vulnerability to C-19 mediated the relationship. |
| [55] | China | 41 | Anxiety, Stress, | Anxiety, depression and stress symptoms Depression, Coping, were associated with negative Social Support coping strategies and low social support |
| [244] | Iran | 1038 | Anxiety | The majority of healthcare workers(60.4%) had minimal to mild anxiety.The other 39.6% had moderate to severe anxiety. |
| [265] | Switzerland | 212 | Anxiety, | Students who participated in the Sept.2019 and Depression Apr.2020 surveys reported an average increase in Stress depressive symptoms, anxiety, stress, and loneliness. |
| [23] | Japan | 4000 | Anxiety, | 12% participants were unconcerned about the transmission, Beliefs/ 11% showed no worry about developing a serious Media Persuasion condition, 8% were not anxious about spreading infection. |

Table A7.
Main characteristics of the studies reviewed, pt.7. Main characteristics of the studies reviewed.
Table A7.
Main characteristics of the studies reviewed, pt.7. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [129] | Africa | 957 | Depression, | Higher perceived risk of COVID-19 infection Anxiety is associated with greater depressive symptoms among adults with histories of childhood trauma during the first 6 weeks of quarantine. |
| [407] | UK | 15,835 | Depression, Anxiety | Mean population GHQ-12 score increased from Stress, 11.5 (2018/19) to 12.6 (April 2020), Other consequences one month into lockdown. |
| [260] | Iran | 535 | Depression, | There was a significant relation between Stress, gender and variables of depression, anxiety, and stress. Anxiety There was also an inverse relationship between stress and variables of educational level and age. |
| [51] | France | 805 | Beliefs/ | Conspiracy beliefs positively predicted a pro-chloroquine Media Persuasion attitude. The same relations were found with vaccine attitudes, intention to be vaccinated, and pro-chloroquine attitudes. |
| [284] | Iran | 615 | Other consequences | 326 persons (53%) experienced high levels of burnout. |
| [38] | USA | 408 | Anxiety | Adhering to social isolation policies predicted lower levels of C-19 Anxiety. This effect was largely mediated by conservation of core beliefs and ability to make meaning of the pandemic. |
| [223] | China | 66 | Anxiety, Depression | The incidences of anxiety, depression, and sleep disorders Depression in the suspected case group were 18.2%, 18.2%, and 39.4%. The anxiety, depression and sleep disorder scores were significantly positively correlated (p < 0.05). |
| [183] | Italy | 944 | Anxiety, | 46% of participants presented moderate to extremely severe Depression, symptoms of depression, 40% presented moderate to extremely Stress, severe symptoms of stress, and 30% presented Other Consequences moderate to extremely severe symptoms of anxiety. People well-endowed with transcendence strengths (e.g., hope, zest, gratitude) scored higher for general mental health, lower for psychological distress (fewer symptoms of depression, anxiety and stress), and higher for self-efficacy in coping with the lockdown situation. |
| [3] | MTurk | 929 | Other Consequences | Of all respondents, 421(45.1%) had low psychological distress, 274(29.4%) had moderate psychological distress, 164 (17.6%) had high psychological distress, and 72 (7.3%) had very high psychological distress. |
| [397] | Arabic | 1006 | Other Consequences | Exhaustion, anxiety, depression, and sleep disturbances were reported (in past seven days) by approximately 34%, 34%, 19%, and 29% of subjects (respectively). |
| [401] | Ecuador | 252 | Anxiety, | Of the sample, 24.2% believed the virus was developed Other consequences intentionally in a lab; 20.6% believed the virus came about naturally; 13.9% believed it was made accidentally in a lab; and the remaining 41.3% were unsure where it originated. Almost one third (32.5%) of the healthcare workers surpassed the cutoff of distress disorder, and 28.2% of the healthcare workers had anxiety disorder. |
| [141] | USA | 2500 | Compliance | Even though 87.5% of the population had high levels of knowledge about social distancing, only 62.5% intended to always practice it, and only 46.2% always practiced it. |
| [285] | MTurk | 2707 | Other Consequences | Across all countries, reported burnout was associated with work impacting household activities, feeling pushed, exposure to COVID-19 patients, and making life prioritizing decisions. |
| [39] | China | 150 | Risk Perception, | The prevalence of the perceptions of high risk of contracting Beliefs/ COVID-19 and disease severity was 18.6% and 25.5%, respectively. Media Persuasion |
| [110] | China | 4991 | Risk Perception, | Over half of the respondents rated their risks of acquiring Anxiety COVID-19 as low. 14% of them reported mild to moderate anxiety level, 5.1% moderate to severe, only 1.5% reported severe anxiety. |

Table A8.
Main characteristics of the studies reviewed, pt.8. Main characteristics of the studies reviewed.
Table A8.
Main characteristics of the studies reviewed, pt.8. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [222] | Iran | 2045 | Anxiety, | 65.6% of the participants have moderate and severe anxiety Depression symptoms, 42.3% had moderate and severe depression symptoms. |
| [114] | USA | 146 | Risk Perception | Younger adults perceived a lower risk of C-19 than did elders, and men perceived lower risks than did women. |
| [357] | China | 1442 | Other Consequences | 26.63% of the participants demonstrated significant distress, and internet addiction was associated with it. |
| [52] | Serbia | 407 | Beliefs/ | 76.7% of the participants reported adhering to at least 3 health Media Persuasion, behaviors; participants moderately endorsed conspiracy theories, Compliance and only modestly overestimated their knowledge about C-19. |
| [279] | Italy | 273 | Other Consequences, | Women reported higher scores of fatigue and burnout than men. Stress COVID-19 fear levels and fatigue in HCWs decreased over the temporal trend, while satisfaction slightly increased. |
| [405] | Italy | 245 | Other Consequences | Mothers reported a worse sleep quality during lockdown, a decrease in time pressure and an increase in time expansion. |
| [316] | Italy | 1153 | Stress | More than 1 out of 3 HCWs showed Emotional Exhaustion, and 1 out of 4 reported Depersonalization. |
| [278] | China | 157 | Stress | 41.4% Non-COVID-19 patients worried about their disease conditions during the epidemic. The most common psychological problems was little interest or pleasure in doing things. |
| [268] | Norway | 1778 | Anxiety, | The levels of PTSD, anxiety, depression and health anxiety Stress, among health personnel and public service providers were Depression high: 27.7% had clinical or subclinical symptoms of PTSD. |
| [398] | Israel | 338 | Other Consequences | Risk of elevated psychological distress was found in 11.5% of the sample, particularly among those who had background illness, fear of contracting COVID-19, and higher subjective overload. |
| [102] | MTurk | 26,508 | Risk Perception | Perceived threat is positively correlated with protective behavior, so does Efficacy and Institutional trust. |
| [328] | MTurk | 324 | Depression | Amongst all the psychological effect, panic was the most agreed with, instead suicidal effect was the least agreed. |
| [98] | Germany | 661 | Compliance, | Participants reported that they adopted protective measures often. Risk Perception Shutdown and governmental restrictions were widely accepted. |
| [119] | USA | 1145 | Compliance, | Participants perceived their own likelihood of getting C-19 Risk Perception to be significantly lower than others; this relative private Anxiety optimism was strongly related to sense of agency and happiness. |
| [168] | China | 673 | Compliance, | Members of workforce reported a low prevalence of anxiety Anxiety, Stress, (3.8%), depression (3.7%), and stress (1.5%). Compliance with Depression safety measures was associated with less severe symptoms. |
| [234] | United Arab | 1485 | Anxiety, | Almost half of students reported anxiety levels from mild Emirates Other Consequences to severe, with females reporting higher anxiety scores, and medical students reporting lower anxiety than dental students. |
| [75] | China | 584 | Coping, | 40.4% of young sample were prone to psychological Stress, problems, as they reported PTSD symptoms and Other Consequences negative coping strategies. |
| [270] | Italy | 131 | Anxiety, | Those with moderate/severe depressive symptoms Depression reported more helplessness, spent more than 3 h searching for C-19 information, perceived less adequate PPE and visited more infected patients. |
| [273] | China | 5461 | Anxiety, Stress, | People who were farthest from the epidemic Depression, of COVID-19 had generally lower scores for each Other Consequences variable (anxiety, depression, stress and sleep). |
| [86] | Jordan | 381 | Coping, | There was a significant inverse relationship between Other Consequences severe psychological distress and motivation for distance. The most common coping strategy among students was spending more time on social media. |
| [261] | USA | 898 | Anxiety | Loneliness, C-19 specific worries, and distress tolerance were significantly associated with anxiety. |

Table A9.
Main characteristics of the studies reviewed, pt.9. Main characteristics of the studies reviewed.
Table A9.
Main characteristics of the studies reviewed, pt.9. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [259] | India | 159 | Anxiety, | An increase in anxiety and stress scores Depression, during the two months of follow-up was found, Stress and also an increase in depressive symptoms. |
| [90] | USA | 657 | Compliance, | Positive screens for psychological symptoms were common; Other consequences 57% for acute stress, 48% for depressive, and 33% for anxiety symptoms. For each, a higher percent of nurses/advanced practice providers screened positive vs. attending physicians, though housestaff’s rates for acute stress and depression did not differ from either. |
| [45] | Cyprus, Greece | 100 | Beliefs/ | The findings showed conspiracy theories are widely Media Persuasion, believed even among highly educated individuals. Compliance, Conspiracy theory beliefs predicted science mistrust Other Consequences and unwillingness to adhere to public health measures. Psychological distress increased conspiracy beliefs. |
| [276] | Austria | 902 | Stress | Greater social connectedness during the lockdown was associated with lower levels of perceived stress, as well as general and COVID-19 specific worries. A negative relationship between fatigue and social connectedness was found (mediated by feelings of stress, general worries, and C-19 specific worries). |
| [49] | MTurk | 704 | Beliefs/ | Social distancing intentions were positively Media Persuasion, predicted by horizontal collectivism, but only Compliance indirectly through lower feelings of powerlessness. Vertical individualism negatively predicted intentions to engage in social distancing, directly and indirectly through belief in C-19 conspiracy theories. |
| [46] | MTurk | 660 | Beliefs/ | Participants perceived themselves and their loved ones Media Persuasion, as moderately/high at risk of contracting a serious illness. Stress C-19 conspiracy beliefs were strongly related to other measures of conspiracy belief; respondent’s level of stress was unrelated to any of the conspiracy belief scales. |
| [113] | Iran | 3727 | Risk Perception | 56.4% of participants were engaging in danger control processes and 43.6% in fear control processes. |
| [262] | Turkey | 771 | Anxiety, | 86% patients with RD were unwilling to go to the Depression, hospital, while 22% discontinued their medications. Stress The frequency of anxiety (20%), depression (43%) and stress (28%) among patients with RD were found to be comparable to that among the teachers/academic staff, whereas significantly less than that among HCWs. |
| [70] | China | 180 | Anxiety, Stress, | Levels of social support for medical staff were Social Support, significantly associated with self-efficacy and sleep quality Other Consequences and negatively associated with the degree of anxiety and stress. Anxiety was significantly associated with stress, which negatively impacted self-efficacy and sleep quality. Anxiety, stress, and self-efficacy were mediating variables associated with social support and sleep quality. |
| [99] | South Korea | 973 | Beliefs/ | Respondents’ perceived risk of COVID-19 infection. Media Persuasion, The average perceived severity score was higher than Compliance, perceived susceptibility. Precautionary behaviors were Risk Perception associated with perceived risk and efficacy. |
| [315] | Spain | 3109 | Stress | Of the 1671 physicians who completed the survey, the highest psychosocial impact was perceived in Respiratory medicine and Geriatrics. Higher distress levels were found in the areas with the highest incidence of COVID-19. |
| [187] | Italy | 2766 | Anxiety, | There is an associations between sociodemographic variables, Depression, depression, anxiety, and stress levels during the C-19 outbreak. Stress Higher levels of negative affect and detachment were associated with higher levels of depression and anxiety. |

Table A10.
Main characteristics of the studies reviewed, pt.10. Main characteristics of the studies reviewed.
Table A10.
Main characteristics of the studies reviewed, pt.10. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [326] | MTurk | 2734 | Depression | Canada: 80.89% proportion of patients reporting worsening of their psychiatric condition; Pakistan: 72.41%; USA: 67.5%. Turkey had the lowest percentage: 28.57%. All scores were significantly (p < 0.05) higher in patients reporting worsening of psychiatric conditions. |
| [264] | Saudi Arabia | 2081 | Anxiety, | The prevalence of depression and anxiety among the Depression participants was 9.4% and 7.3%, respectively. |
| [288] | China | 939 | Stress, | Difference between occupations: teachers reported that Other Consequences their mental state improved for the specific question regarding fidgeting and not knowing what to do; after 2 weeks, medical staff and business managers reported increased anxiety, officials showed more anxiety and fear regarding the epidemic when compared with people with other occupations. |
| [309] | France | 1771 | Depression, Stress, | In total, 38.06% of the respondents had psychological distress. Other Consequences Sex, unemployment and depression were associated with it. |
| [9] | Turkey | 1772 | Other Consequences | Mental wellbeing was negatively associated with intolerance of uncertainty, rumination, and fear of C-19. |
| [103] | France | 991 | Compliance, | Conspiracy was positively correlated with the adoption Risk Perception of non-normative prevention behaviours, in contrast, no association was observed with the adoption of normative prevention behaviours. Furthermore, conspiracy was associated with a greater perception of risk of contamination of the French population, personal contamination, and risk of death. |
| [349] | Italy | 192 | Depression | The COVID-19 study group had significantly higher mean EPDS scores compared with the control group. Analysis of three EPDS subscales revealed significantly higher scores among the COVID-19 group compared with the control group for anhedonia and depression. |
| [229] | Poland | 356 | Anxiety | Persistent thinking about C-19 was associated with increased coronavirus anxiety and negative trauma effects. Anxiety served as a partial mediator in the link between persistent thinking about C-19 and negative trauma effects. |
| [121] | Nigeria | 1500 | Risk Perception | Higher risk perception was related to greater precautionary behaviour. |
| [215] | Bangladesh | 505 | Anxiety, | 28.5% of the respondents had stress, 33.3% anxiety, Depression, 46.92% depression from mild to extremely severe, Stress according to DASS 21 and 69.31% had event-specific distress from mild to severe in terms of severity according to IES. Perceiving physical symptoms as COVID-19 was significantly associated with DASS stress, anxiety and depression subscales. |
| [100] | Germany | 1055 | Risk Perception | Individuals showed biases in their risk perception concerning overconfidence and the underestimation of exponential growth of infection cases in the early phase of the pandemic. Risk perceptions increased with perceived dread and tended to increase with perceived control over infection, the evaluation of scientific and own knowledge about the pandemic. |
| [314] | China | 371 | Stress, | 1 month after the outbreak, the prevalence of PTSSs was Other Consequences 3.8% in HCWs. HCWs with higher exposure level also rated more hyperarousal symptoms. In summary, targeted interventions on sleep contribute to the mental recovery during the outbreak of COVID-19. |

Table A11.
Main characteristics of the studies reviewed, pt.11. Main characteristics of the studies reviewed.
Table A11.
Main characteristics of the studies reviewed, pt.11. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [125] | Poland | 621 | Compliance, | Loneliness was correlated with MHS and with affective response Risk Perception to COVID-19’s threat to health. However, increased worry about the social isolation and heightened risk perception for financial problems was observed in lonelier individuals. |
| [157] | China | 608 | Compliance, Anxiety, | More respondents had state anxiety than trait anxiety. Depression was found among 27.1% of respondents. About 10.1% of respondents suffered from phobia. The three most commonly used prevention measures were making fewer trips outside and avoiding contact, wearing a mask, and hand hygiene. |
| [242] | India | 291 | Anxiety, | Of total sample analyzed, the overall prevalence of Depression, acute stress reaction, GAD and depressive symptoms Stress were 1.37%, 11.34%, 42.61% respectively. |
| [277] | Switzerland | 1565 | Stress, | The shows that worries about the individual, social, and Other Consequences economic consequences of the crisis, strongly boost stress. The infection rate in the zone of residence also contributes to stress. Positive thinking and perceived support mitigate worries and stress. |
| [257] | China | 3611 | Anxiety | The mean SAS score was significantly higher than that of the national norm, and there were still 557 students identified as anxious of different levels with the max score of 100, whom were from different provinces and at different grades with different majors. |
| [365] | China | 3248 | Other Consequences | 3248 individuals were enrolled, and the score of psychological distress scale was 15 × 93 ± 6 × 99, the score of psychological help seeking was 82 × 34 ± 13 × 04. |
| [66] | France | 4003 | Social Support, | The effects of sociocultural variables on compliance are Compliance not mediated by psychosocial variables, but by cognitive ones. |
| [322] | China | 3088 | Stress | Using psychological stress as the dependent variable, authors found several predictors, including being female. |
| [312] | Turkey | 451 | Depression, | Having high level of stress or being pessimistic was Stress associated with more maladaptive psychological constructs. |
| [166] | India | 121 | Compliance, | Most of the children and adolescents were non-compliant, Other consequences quarantined ones experienced greater psychological distress. |
| [243] | UK | 3097 | Anxiety, | Mean scores for depression, stress and anxiety, and significantly Depression, exceeded population norms. Being younger and female, Stress was associated with all outcomes. |
| [320] | India | 1106 | Stress | One third of respondents had IES-R > 24. |
| [346] | China | 500 | Depression | The prevalence rate of mild depression was 29%, 12.8% for moderate, 6.2% for moderately severe, and 0.8% for severe. |
| [50] | UK, | 950 | Beliefs/ | Participants high in national narcissism agreed USA Media Persuasion more strongly with COVID-19 conspiracy theories. |
| [311] | China | 600 | Stress | There was a significant negative correlation between perceived stress and resilience. |
| [228] | Pakistan | 347 | Anxiety, | Fear of C-19 was related to disgust sensitivity, Other Consequences anxiety sensitivity-related physical concerns, body vigilance, contamination cognitions and general distress. |
| [235] | South Korea | 65 | Anxiety, | 32.3% of physical therapists had GAD-7 ≥ 5, indicating Depression presence of anxiety; 18.5% had PHQ-9 ≥ 10, indicating presence of depression. |
| [318] | Spain | 878 | Stress, | No significant group differences emerged in older adults’ Other Consequences appraisals or COVID stress-related variables. Older adults experienced more gratitude and resilience. |
| [123] | USA | 100 | Risk Perception | Participants rated both the USA and European governments as somewhat unprepared for future outbreaks, they were less concerned with personally being infected but they perceived the disease as quite severe, they were very likely to get vaccinated. |
| [154] | USA | 302 | Compliance | Perceived norms were lower than individuals’ own beliefs. |

Table A12.
Main characteristics of the studies reviewed, pt.12. Main characteristics of the studies reviewed.
Table A12.
Main characteristics of the studies reviewed, pt.12. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [181] | MTurk | 3593 | Compliance, | People with more social isolation or stress reported Stress more problems in relationships with their partner. |
| [253] | China | 1620 | Depression | 279 students had social anxiety, and 102 students had depression. The following variables were found to be significant risk factors for social anxiety during home quarantine: deterioration of the parent-child relationship, increased conflicts with parents, irregular work and rest, and worrying more about being infected. |
| [57] | Poland | 515 | Stress, | Ego-resiliency and social support had a Social Support significant impact on the level of C-19 anxiety. |
| [53] | MTurk | 404 | Beliefs/ | The sample was mildly inclined towards conspiracy ideation and Media Persuasion indicated a slight inclination towards rejecting science. |
| [366] | Germany | 1609 | Other Consequences | Neuroticism was associated with negative affect in daily life, paying more attention to information, and worrying more about one’s own health. |
| [409] | Italy | 1569 | Other Consequences | Lower media exposure, higher worry, lower coping efficacy, lower trust in institutions, and negative attitudes toward quarantine measures predicted more mental health symptoms. |
| [402] | China | 98 | Other Consequences | Mental distress among participants was not very serious in general. C-19 survivors presented a highest score. |
| [64] | USA | 437 | Anxiety, | Greater negative C-19 experiences were associated with Depression, higher depressive symptoms, higher anxiety, Social Support and lower belongingness. |
| [151] | USA | 3101 | Compliance | Greater self-reported social distancing was linked to reporting that one can control C-19 via one’s own behavior and greater self-reported hygiene practices. |
| [211] | China | 631 | Anxiety | Anxiety was correlated with the frequency of receiving negative news, current health situation and time spent on receiving information related to C-19. |
| [116] | MTurk | 1657 | Risk Perception, | As the pandemic evolved, people’s perceived infection Compliance increased and they tended to respect social distance more. |
| [115] | Italy | 1751 | Risk Perception, | For psychological distance factors, a positive effect of risk Compliance perception emerged and was modulated by the type of humor. |
| [143] | UK | 202 | Anxiety, | Depression and anxiety were highly correlated with Depression, fight–flight–freeze system, and behavioural inhibition and system. Compliance. |
| [48] | Turkey | 1088 | Risk Perception, | Those who are less tolerant of uncertain situations were more Compliance, Beliefs/ likely to believe in conspiracy theories; these were positively Media Persuasion correlated with perceived risk, but negatively with compliance. |
| [236] | Italy | 67 | Anxiety, | No worsening of anxiety and depression Depression levels was found in MS patients. |
| [88] | MTurk | 487 | Coping | The increase of the adaptive coping strategies was associated with lower levels of fear, restlessness, and trouble relaxing. |
| [8] | Pakistan | 398 | Anxiety, Coping, | Most frequently coping strategies adopted by HCWs were Depression, religious coping, acceptance and coping planning. The Other Consequences prevalence of anxiety and depression were 21.4% and 21.9%. |
| [212] | USA | 10,368 | Anxiety, | Fear appears to be concentrated in regions with the highest Depression, reported COVID-19 cases. Greater fear correlates Other Consequences with anxiety and depression. |
| [188] | Turkey | 451 | Anxiety, | Individuals who were experiencing sleep problems during the Other Consequences COVİD-19 pandemic had higher levels of anxiety. |
| [348] | China | 845 | Depression | The prevalence of postpartum depression among women was 30%. Significant factors as concerns about contracting COVID-19 and certain precautionary measures were relevant. |
| [104] | Italy | 932 | Anxiety, | The mean compliance scores follow a hyperbolic-like curve, Risk Perception, decreasing over time for the lowest level of risk. Higher Compliance levels of anxiety and perceived risk were reported by women. |

Table A13.
Main characteristics of the studies reviewed, pt.13. Main characteristics of the studies reviewed.
Table A13.
Main characteristics of the studies reviewed, pt.13. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [287] | Lebanon | 950 | Stress | Quarantine started to cause PTSD symptoms during the second week, worsening in the fourth. |
| [364] | Spain | 4180 | Other Consequences | Results showed a high level of psychological distress, with a higher percentage in women and people of middle age. |
| [358] | Australia | 673 | Other Consequences | Results showed more presence of mental health outcomes for participants measured during C-19, compared to before C-19. |
| [286] | Slovenia | 964 | Stress | Educators’ stress was negatively related to their ICT self-efficacy, attitudes about online education, and perceived support. |
| [4] | UK | 12,090 | Anxiety, | People showed statistically significant increases in mental Depression health problems (anxious and depressive symptoms). |
| [149] | Brazil | 2056 | Compliance | There was a significant difference among political partisan groups when it comes to attitudes toward social distancing. |
| [106] | Turkey | 220 | Other Consequences | Dispositional hope was negatively and moderately correlated with psychological health of adults. Psychological health was negatively associated with resilience and subjective well-being, and resilience had positive correlation with subjective wellbeing and preventive behaviours. |
| [36] | MTurk | 851 | Beliefs/ | Higher levels of fatalism were associated with Media Persuasion lower behavioral intentions to support mitigation efforts; the optimistic message increased support for mitigation efforts relative to no message. |
| [112] | Italy | 580 | Risk Perception | The risk infection perception is higher in those regions where the number of confirmed cases is higher. C-19 outbreak emergency negatively affected psychological state and symptoms (separation distress, psychological symptoms), as well as the ability to cope with challenging times. |
| [74] | Italy | 2053 | Coping, Stress | The results suggest a characterization of people who are more vulnerable to experiencing high levels of stress during the COVID-19 pandemic. |
| [107] | Turkey | 4536 | Risk Perception, | Vulnerability, perceived risk, and fear can increase Other Consequences engagement in preventive behaviours during the pandemic. |
| [269] | Bangladesh | 555 | Anxiety, Stress, | Prevalence estimates of depression, anxiety and stress were Depression, 76.1%, 71.5% and 70.1% for at least mild symptoms, Other Consequences 62.9%, 63.6% and 58.6% for at least moderate symptoms. |
| [355] | Israel | 761 | Depression, | The Israeli Arabs reported a higher level of distress Other Consequences and a lower level of resilience and well-being. |
| [238] | China | 846 | Compliance, | Results demonstrated reciprocal negative associations Anxiety between anxiety and crisis management appraise. |
| [396] | China | 803 | Other Consequences | Exploratory analyses suggested that relatively extroverted individuals exhibited larger declines in social connection. |
| [232] | Pakistan | 389 | Anxiety, | A 43% prevalence of anxiety/depression among Depression frontline physicians of Pakistan was reported. Almost all the doctors had moderate/high knowledge score. |
| [323] | China | 415 | Stress | Overall, analysis of data on perceived stress and professional identity pandemic suggests that stress levels are inversely proportional to knowledge in effective ways of handling the pandemic. |
| [266] | China | 1160 | Anxiety, | Compared with general adults in some regions of China, Depression the scores of SAS and SDS were both significantly higher in pregnant women during the outbreak of COVID-19. |
| [345] | Pakistan | 500 | Depression, | Results specified a normal (65.9%), mild (9.10%), Other Consequences moderate (9.12%), and severe (15.90%) depression prevalence, and findings stipulated that anxiety disorder prevalence was higher than the depression disorder. |
| [128] | USA | 1153 | Risk Perception, | Differences in reported social distancing were mediated Compliance by divergent perceptions of health risk, explained by differences in self-reported knowledge of C-19 and perceived media accuracy in covering the pandemic. |
| [68] | New Zealand | 1103 | Social Support, | Broadly speaking, levels of trust, and Other Consequences attitudes toward the nation and government changed following lockdown. |

Table A14.
Main characteristics of the studies reviewed, pt.14. Main characteristics of the studies reviewed.
Table A14.
Main characteristics of the studies reviewed, pt.14. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [329] | MTurk | 29,744 | Depression, | The results show that participants’ emotional Other Consequences experiences were characterized by love and hope, as well as feelings of anxiety and sadness. |
| [101] | China | 1022 | Depression, | Findings show that government emergency public information, Other Consequences detailed pandemic information, and positive risk communication had greater impact on protective behaviors. |
| [275] | China | 4268 | Stress | Results revealed that in all provinces of China, medical staffs scored significantly higher on all items of psychological stress than college students. |
| [160] | Switzerland | 737 | Compliance | Non-compliance, especially with hygiene-related measures, was more prevalent in males and in individuals with higher education, higher SES, and a non-migrant background. |
| [117] | MTurk | 996 | Risk Perception | Who felt more threatened by C-19 stockpiled more toilet paper. A predisposition towards Emotionality predicted the perceived threat and affected stockpiling behavior. |
| [146] | Brazil | 715 | Compliance | Results show a trend towards lower extroversion scores in the social distance group, and lower conscientiousness scores for the groups that considered that the containment measures were not essential. |
| [122] | MTurk | 1142 | Risk Perception, Anxiety, | Studies reveal that both realistic and symbolic threats Other Consequences predict higher distress and lower well-being. |
| [41] | USA | 1182 | Beliefs/ | 3 distinct clusters of psychological responses: Media Persuasion, informed, panic, and ignorant. Clusters Anxiety differed regarding their knowledge about the virus, C-19-related anxiety (i.e., worry and emotionality), and evaluation of the C-19 crisis’s severity. |
| [230] | USA | 474 | Anxiety | Those in threat condition reported a higher likelihood that the prevalence of C-19 would increase in the future and also reported greater harm to the US from C-19. |
| [351] | China | 5115 | Depression | Participants who reported greater flow also reported more positive emotion, less severe depressive symptoms, less loneliness, and more healthy behaviors. Interactions with quarantine length were more consistent. |
| [96] | China | 1346 | Anxiety, | Significant correlations were found between anxiety Risk Perception, and perceived risk, positive affect and negative affect; Depression depression correlated with perceived risk, positive affect, negative affect and anxiety symptoms. |
| [399] | Brazil | 592 | Other Consequences | Wellbeing related to physical activity during quarantine was linked to an established routine of physical activity before the social isolation period. |
| [79] | China | 117 | Compliance | Psychological distress during the pandemic Risk Perception was associated with greater C-19-related catastrophizing, increased general health anxiety, greater support-seeking coping, but less use of problem-focused coping. |
| [185] | Turkey | 318 | Anxiety, | Female gender, living in urban areas and previous psychiatric Depression illness were found as risk factors for anxiety and depression. |
| [271] | Italy | 1310 | Anxiety, | During lockdown, sleep timing changed (people going to Depression, bed and waking up later), but also reporting a lower Stress, sleep quality, especially for those with a higher Other Consequences level of depression, anxiety and stress symptomatology. |
| [78] | Italy | 1163 | Coping, Stress, | The perceived impact on health was significantly higher Depression, in HCWs and in people living in northern Italy. A significant Risk Perception indirect effect of problem-oriented coping was found. |
| [184] | China | 7236 | Anxiety, | The prevalence of anxiety symptoms, depressive symptoms, Depression, and poor sleep quality were 35.1%, 20.1%, Other Consequences and 18.2%, respectively. |

Table A15.
Main characteristics of the studies reviewed, pt.15. Main characteristics of the studies reviewed.
Table A15.
Main characteristics of the studies reviewed, pt.15. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [69] | UK | 45,109 | Social Support, | Individuals with diagnosed mental illness, lower social Other Consequences support, and more worries had worse sleep quality. |
| [408] | China | 484 | Other Consequences | Females, young people, and those with higher fatigue and anxiety severity were more likely to experience insomnia. |
| [54] | China | 182 | Anxiety, | Chinese overseas students experienced a Social Support higher level of anxiety than the Chinese population. |
| [356] | USA | 374 | Depression | Factors associated with depression included: degree of C-19 interference with the treatment of cancer, and concern that patients will not receive the level of care needed. |
| [321] | India | 100 | Stress, | Female college students are severely affected by PTSD, Depression and present a correlation between depression and avoidance. |
| [390] | Japan | 1148 | Other Consequences | The number of workplace measures correlated positively with respondents’ fear and worry, negatively with distress. |
| [89] | USA | 1015 | Coping, | The most common stressor is reading about the severity of Stress, C-19, uncertainty about length of quarantine and social Compliance distancing requirements. Most common coping strategies: distraction, active coping, and seeking emotional social support. |
| [95] | Qatar | 405 | Compliance, | 87.3% of participants reported that they stay at home, Risk Perception 60.3% said that they maintain an adequate distance, and 73.5% believed that COVID-19 is a dangerous disease. |
| [16] | USA | 464 | Anxiety, Compliance, | Most of the people received information through TV, social Risk Perception, media, family and friends. Only 35.1% stated that they were Beliefs/ likely to contract C-19; nearly 38% did not consider Media Persuasion C-19 serious for themselves; 47.8% had high levels of anxiety. |
| [245] | Portugal | 1280 | Anxiety, | Severe depression and anxiety symptoms existed in 7.6% Depression and 9.1% of the sample. |
| [77] | USA | 269 | Coping, | Active coping, denial, use of emotional support, humor, Other Consequences religion, and self-blame were associated with wellbeing. |
| [94] | China | 2640 | Coping | Behavioral coping showed the highest level, and emotional coping the lowest. |
| [93] | Poland | 353 | Coping, | Most used strategies for coping with the stress generated Other Consequences by C-19 are: emotional support, planning, acceptance. |
| [71] | China | 1588 | Coping, | Suspected cases of C-19 had high psychological distress, Other Consequences, spent more time searching for information, they rarely Social Support used any coping style to deal with the stressor, and had less social support. |
| [138] | Norway | 10,084 | Compliance | Social distance may lead to self-isolation, that could cause severe consequences (feeling loneliness). |
| [133] | Turkey | 204 | Anxiety, Stress, | Perceived risk was significantly and positively correlated Depression, with coronavirus fear, depression, stress, and anxiety, Other Consequences and negatively associated with resilience. |
| [87] | China | 534 | Coping, | Coping strategies, strict protective measures, knowledge of Stress prevention and transmission, social isolation, and positive self-attitude resulted in less stress. |
| [313] | Turkey | 475 | Stress | C-19 stress had negative correlations with meaning in life and optimism, as well as positive associations with pessimism and depressive symptoms. |
| [308] | Ethiopia | 374 | Stress | 3/4 of the sample rated their stress as moderate to high. |
| [256] | Australia | 1491 | Stress, Depression, | Negative changes in physical activity, sleep, smoking Anxiety, and alcohol intake were associated with higher Other consequences depression, anxiety and stress symptoms. |
| [263] | China | 210 | Stress, Depression, | The average score of the GAD-7 of all subjects was Anxiety at the level of moderate anxiety, while the average score of the PHQ-9 of them was at the level of mild depression. |
| [255] | Canada, USA | 616 | Anxiety, Depression | For depression, there were significant main effects of gender and health status.For anxiety, there were significant main effects of gender and health status. |
| [357] | China | 232 | Stress | 22.4% HD patients and 13.4% PD patients had moderate or severe PTSS, which need psychological support. Both groups considered psychological support necessary. |

Table A16.
Main characteristics of the studies reviewed, pt.16. Main characteristics of the studies reviewed.
Table A16.
Main characteristics of the studies reviewed, pt.16. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [35] | Bangladesh | 700 | Beliefs/ | Psychologically distressed participants showed more Media Persuasion negative attitudes toward winning over C-19 Other Consequences than participants with good mental health. |
| [72] | China | 802 | Coping | It was found that nurses’ anxiety, fear, sadness, and anger was significantly higher than the emotional level of nursing college students. |
| [161] | USA | 1070 | Compliance, | Women adhere more to preventive behaviors than men. Anxiety During pandemics, policymakers may benefit from disseminating preventive health messages purposely tuned to motivate adherence by men. |
| [218] | Philippines | 538 | Anxiety | Respondents are suffering from moderate illness anxiety: symptoms of hypochondriasis, attitude on acquiring COVID-19, avoidance, and reassurance seeking behavior. |
| [254] | China | 702 | Depression, | Risk of severe depression in rst-line Stress staff was 6.63 fold; the risk of severe panic disorder was 2.62 fold higher than non-rst line group. |
| [152] | Bangladesh | 350 | Compliance | Better self-control ability, higher education and good mental health emerged as factors that significantly shaped the precautionary behaviors of young adults in this study. |
| [317] | MTurk | 54,245 | Stress | Higher levels of stress are associated with younger age, being women, being single, staying with more children, and living in collectivist cultures. |
| [124] | USA | 2135 | Risk Perception | US adult residents severely underestimated their absolute and relative fatality risk. |
| [150] | UK | 2025 | Compliance | All three COM-B components significantly predicted good hygienic practices, with motivation having the greatest influence on behaviour. |
| [40] | Serbia | 975 | Compliance, Beliefs/ | Significant association was found between Media Persuasion, educational level, gender, age and different variables Risk Perception of preparedness and various information variables. |
| [66] | France | 2000 | Compliance | Results show a high rate of compliance with the behavioral recommendations. |
| [6] | USA, Canada, | 2065 | Anxiety, Stress, | Cross-sectional findings indicated elevated anxiety Europe Depression and depressive symptoms associated with COVID-19 concern more strongly than epidemiological objective risk. |
| [352] | China | 1951 | Depression | Credibility of real-time updates and confidence in the epidemic control are associated with a decline in depression but an increase in happiness. |
| [25] | South America | 600 | Beliefs/ | Our study identified that, although people reported Media Persuasion adequate knowledge by identifying expected symptoms and coronavirus transmission process. |
| [180] | Croatia | 1854 | Compliance | Parents, mothers especially, represent the most concerned group, regardless of age. People with chronic health conditions also expressed greater concern and safety behaviour than healthy participants. |
| [249] | Turkey | 103 | Anxiety, | Anxiety, hostility, and phobic anxiety were higher Depression in participants over the age of 29 years. |
| [37] | United Arab | 2200 | Beliefs/Media Persuasion, | Females, those who felt public fear as justifiable, Emirates Risk Perception, worried about C-19, intended to take the vaccine, Other Consequences, and smokers were all associated with anxiety. Anxiety |
| [403] | Mexico | 2860 | Other Consequences | There was a significantly higher level of fear in nursing and administrative personnel. |
| [239] | China | 474 | Anxiety, Depression, | Age had a curvilinear relationship with Other Consequences nonsomatic pain, depression, and anxiety. |

Table A17.
Main characteristics of the studies reviewed, pt.17. Main characteristics of the studies reviewed.
Table A17.
Main characteristics of the studies reviewed, pt.17. Main characteristics of the studies reviewed.
| Ref | Country | Sample Size | Impacted Dimension | Main Findings |
|---|---|---|---|---|
| [411] | Cuba | 772 | Other Consequences | In the sample, on average, female participants experienced significantly greater fear of COVID-19 than men. |
| [214] | USA, UK, | 218 | Anxiety, Depression, | Contrary to expectations, depression, rumination, Canada Other Consequences and distress intolerance were at equivalent levels during the pandemic as they were at baseline. |
| [395] | China | 30,861 | Other Consequences | The results showed that there were significant differences in children’s behavior scores in variables such as age, whether or not an only child and place of residence. |
| [170] | Iran | 290 | Compliance, Anxiety, | Fear of COVID-19 among pregnant women was significantly Depression, and positively associated with their psychological problems, Other Consequences with their husbands’ psychological problems, with their and their husband’s preventive COVID-19 behaviour. |
| [400] | Pakistan | 250 | Other Consequences | The psychological impact of quarantine ward on healthcare professionals has identified through six dimensions of PGWB, i.e., psychology effect; depression; negative well-being; lack of self-control; general health; vitality. |
| [233] | USA | 5550 | Anxiety, Stress, | Among all workers, anxiety, depression, Depression, and high work exhaustion were independently Other Consequences associated with community or clinical exposure to COVID-19. |
| [319] | India | 586 | Stress, | During the lockdown due to COVID-19, 1-in-2 Indian endodontists Other Consequences had distress, as measured by CPDI and 4-in-5 of them had perceived stress, as indicated by PSS. |
| [225] | Italy | 18,147 | Anxiety, Stress, | Quarantine was associated with PTSS, anxiety and ADS. Depression, Any recent COVID-related stressful life event Other Consequences was associated with all the selected outcomes. |
| [7] | Spain | 3055 | Anxiety, Stress, | Spanish consider the current COVID-19 health crisis Depression as fairly severe, and the majority felt that the COVID-19 crisis had greatly impacted on their daily life, including changes in their daily routines and cancellation of important activities. |
| [17] | Kurdistan | 516 | Beliefs/ | Participants reported that social media has a significant impact Media Persuasion, on spreading fear and panic related to the COVID-19 outbreak Other Consequences in Iraqi Kurdistan, with a potential negative influence on people’s mental health and psychological well-being. |
| [237] | Poland | 317 | Stress, Anxiety, | Analyses indicated that stronger basic hope and Beliefs/ higher levels of meaning in life and life satisfaction Media Persuasion correlate with lower state anxiety and stress. |
| [307] | MTurk | 12,817 | Depression, | Female gender, pre-existing psychiatric condition, Stress and prior exposure to trauma were identified as risk factors, whereas optimism, ability to share concerns with family and friends, positive prediction about COVID-19, and daily exercise predicted fewer psychological symptoms. |
| [283] | China | 2027 | Stress | The results showed rapid growth in the first 4 days, Other Consequences and then decreased in the last days, both in PTSD and in sleep-related problems. |
References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2021. Available online: https://covid19.who.int/ (accessed on 21 February 2022).
- World Health Organization. 2020. Available online: https://www.who.int/ (accessed on 1 September 2021).
- Ambelu, A.; Birhanu, Z.; Yitayih, Y.; Kebede, Y.; Mecha, M.; Abafita, J.; Belay, A.; Fufa, D. Psychological distress during the COVID-19 pandemic in Ethiopia: An online cross-sectional study to identify the need for equal attention of intervention. Ann. Gen. Psychiatry 2021, 20, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.; Sutin, A.R.; Robinson, E. Longitudinal changes in mental health and the COVID-19 pandemic: Evidence from the UK Household Longitudinal Study. Psychol. Med. 2020, 13, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Favieri, F.; Forte, G.; Tambelli, R.; Casagrande, M. The Italians in the time of coronavirus: Psychosocial aspects of the unexpected COVID-19 pandemic. Front. Psychiatry 2021, 12, 551924. [Google Scholar] [CrossRef] [PubMed]
- Nelson, B.W.; Pettitt, A.; Flannery, J.E.; Allen, N.B. Psychological and Epidemiological Predictors of COVID-19 Concern and Health-Related. Int. J. Methods Psychiatr. Res. 2021, 21, 169–184. [Google Scholar]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front. Psychol. 2020, 11, 1540. [Google Scholar] [CrossRef]
- Salman, M.; Asif, N.; Mustafa, Z.U.; Khan, T.M.; Shehzadi, N.; Hussain, K.; Tahir, H.; Raza, M.H.; Khan, M.T. Psychological impact of COVID-19 on Pakistani university students and how they are coping. medRxiv 2020. [Google Scholar] [CrossRef]
- Satici, B.; Saricali, M.; Satici, S.A.; Griffiths, M.D. Intolerance of uncertainty and mental wellbeing: Serial mediation by rumination and fear of COVID-19. Int. J. Ment. Health Addict. 2020, 15, 1–12. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, X.; Gao, B. Mental Distress among Frontline Healthcare Workers outside the Central Epidemic Area during the Novel Coronavirus Disease (COVID-19) Outbreak in China: A Cross-Sectional Study. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-26633/v1 (accessed on 1 September 2021).
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Fenichel, E.P.; Wang, X. The mechanism and phenomena of adaptive human behavior during an epidemic and the role of information. In Modeling the Interplay between Human Behavior and the Spread of Infectious Diseases; Springer: Berlin/Heidelberg, Germany, 2013; pp. 153–168. [Google Scholar]
- Fenichel, E.P.; Castillo-Chavez, C.; Ceddia, M.G.; Chowell, G.; Parra, P.A.G.; Hickling, G.J.; Holloway, G.; Horan, R.; Morin, B.; Perrings, C.; et al. Adaptive human behavior in epidemiological models. Proc. Natl. Acad. Sci. USA 2011, 108, 6306–6311. [Google Scholar] [CrossRef]
- Funk, S.; Salathé, M.; Jansen, V.A. Modelling the influence of human behaviour on the spread of infectious diseases: A review. J. R. Soc. Interface 2010, 7, 1247–1256. [Google Scholar] [CrossRef]
- Teasdale, E.; Yardley, L.; Schlotz, W.; Michie, S. The importance of coping appraisal in behavioural responses to pandemic flu. Br. J. Health Psychol. 2012, 17, 44–59. [Google Scholar] [CrossRef]
- Ha, T.; Schensul, S.; Lewis, J.; Brown, S. Early assessment of knowledge, attitudes, anxiety and behavioral adaptations of Connecticut residents to COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Ahmad, A.R.; Murad, H.R. The impact of social media on panic during the COVID-19 pandemic in Iraqi Kurdistan: Online questionnaire study. J. Med. Internet Res. 2020, 22, e19556. [Google Scholar] [CrossRef] [PubMed]
- Imhoff, R.; Lamberty, P. A bioweapon or a hoax? The link between distinct conspiracy beliefs about the Coronavirus disease (COVID-19) outbreak and pandemic behavior. Soc. Psychol. Personal. Sci. 2020, 11, 1110–1118. [Google Scholar] [CrossRef]
- Everett, J.A.; Colombatto, C.; Chituc, V.; Brady, W.J.; Crockett, M. The Effectiveness of Moral Messages on Public Health Behavioral Intentions during the COVID-19 Pandemic. 2020, Psyarxiv. Available online: https://psyarxiv.com/9yqs8/ (accessed on 1 September 2021).
- Heffner, J.; Vives, M.L.; FeldmanHall, O. Emotional responses to prosocial messages increase willingness to self-isolate during the COVID-19 pandemic. Personal. Individ. Differ. 2021, 170, 110420. [Google Scholar] [CrossRef] [PubMed]
- Jordan, J.; Yoeli, E.; Rand, D. Don’t get it or don’t spread it? Comparing self-interested versus prosocially framed COVID-19 prevention messaging. Sci. Rep. 2021, 11, 1–7. [Google Scholar]
- Qazi, A.; Qazi, J.; Naseer, K.; Zeeshan, M.; Hardaker, G.; Maitama, J.Z.; Haruna, K. Analyzing situational awareness through public opinion to predict adoption of social distancing amid pandemic COVID-19. J. Med. Virol. 2020, 92, 849–855. [Google Scholar] [CrossRef]
- Shiina, A.; Niitsu, T.; Kobori, O.; Idemoto, K.; Hashimoto, T.; Sasaki, T.; Igarashi, Y.; Shimizu, E.; Nakazato, M.; Hashimoto, K.; et al. Perception of and anxiety about COVID-19 infection and risk behaviors for spreading infection: An international comparison. Ann. Gen. Psychiatry 2021, 20, 1–11. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, D.; Xu, H.; Xiao, Y.; Chen, C.; Chen, R.N.; Hu, L.H.; Li, Z.S. Public Knowledge of Novel Coronavirus Diseases 2019: A Web-Based National Survey. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-28163/v1 (accessed on 1 September 2021).
- Zegarra-Valdivia, J.; Vilca, B.N.C.; Guerrero, R.J.A. Knowledge, Attitudes, and Perception Susceptibility towards the COVID-19 Pandemic in Latin American Region. 2020, Psyarxiv. Available online: https://psyarxiv.com/w9y6z/ (accessed on 1 September 2021).
- Goodman, R. The Strengths and Difficulties Questionnaire: A research note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Swami, V.; Chamorro-Premuzic, T.; Furnham, A. Unanswered questions: A preliminary investigation of personality and individual difference predictors of 9/11 conspiracist beliefs. Appl. Cogn. Psychol. 2010, 24, 749–761. [Google Scholar] [CrossRef]
- Brotherton, R.; French, C.C.; Pickering, A.D. Measuring belief in conspiracy theories: The generic conspiracist beliefs scale. Front. Psychol. 2013, 4, 279. [Google Scholar] [CrossRef]
- Cann, A.; Calhoun, L.G.; Tedeschi, R.G.; Kilmer, R.P.; Gil-Rivas, V.; Vishnevsky, T.; Danhauer, S.C. The Core Beliefs Inventory: A brief measure of disruption in the assumptive world. Anxiety Stress Coping 2010, 23, 19–34. [Google Scholar] [CrossRef] [PubMed]
- Frederick, S. Cognitive reflection and decision making. J. Econ. Perspect. 2005, 19, 25–42. [Google Scholar] [CrossRef]
- Jolley, D.; Douglas, K.M. Prevention is better than cure: Addressing anti-vaccine conspiracy theories. J. Appl. Soc. Psychol. 2017, 47, 459–469. [Google Scholar] [CrossRef]
- Bruder, M.; Haffke, P.; Neave, N.; Nouripanah, N.; Imhoff, R. Measuring individual differences in generic beliefs in conspiracy theories across cultures: Conspiracy Mentality Questionnaire. Front. Psychol. 2013, 4, 225. [Google Scholar] [CrossRef] [PubMed]
- Lewandowsky, S.; Gignac, G.E.; Oberauer, K. The role of conspiracist ideation and worldviews in predicting rejection of science. PLoS ONE 2013, 8, e75637. [Google Scholar] [CrossRef] [PubMed]
- Zhong, B.L.; Luo, W.; Li, H.M.; Zhang, Q.Q.; Liu, X.G.; Li, W.T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745. [Google Scholar] [CrossRef]
- Imtiaz, A.; Hasan, M.E.; Hossain, M.A.; Khan, N.M. Attitudes Toward COVID-19 among Young Adults: Role of Psychological Distress. 2020, Psyarxiv. Available online: https://psyarxiv.com/futpk/ (accessed on 1 September 2021).
- Hayes, J.; Clerk, L. Fatalism in the Fight against COVID-19: Implications for Mitigation and Mental Health. 2020, OSFPreprints. Available online: https://osf.io/t6zmv (accessed on 1 September 2021).
- Saddik, B.; Hussein, A.; Albanna, A.; Elbarazi, I.; Al-Shujairi, A.; Sharif-Askari, F.S.; Temsah, M.H.; Stip, E.; Hamid, Q.; Halwani, R. Assessing the influence of parental anxiety on childhood anxiety during the COVID-19 pandemic in the United Arab Emirates. medRxiv 2020. [Google Scholar] [CrossRef]
- Milman, E.; Lee, S.A.; Neimeyer, R.A. Social isolation and the mitigation of coronavirus anxiety: The mediating role of meaning. Death Stud. 2020, 46, 1–13. [Google Scholar] [CrossRef]
- Yang, X.Y.; Yang, T.; Rockett, I.R. Changing trends of excess self-protective behavior, and association with belief in prevention myths during the COVID-19 epidemic in China: A panel study. medRxiv 2020. [Google Scholar] [CrossRef]
- Cvetković, V.M.; Nikolić, N.; Radovanović Nenadić, U.; Öcal, A.; K Noji, E.; Zečević, M. Preparedness and preventive behaviors for a pandemic disaster caused by COVID-19 in Serbia. Int. J. Environ. Res. Public Health 2020, 17, 4124. [Google Scholar] [CrossRef]
- Stadler, M.; Niepel, C.; Botes, E.; Dörendahl, J.; Krieger, F.; Greiff, S. Individual Psychological Responses to the SARS-CoV-2 Pandemic: Different Clusters and Their Relation to Risk-Reducing Behavior. 2020, Psyarxiv. Available online: https://psyarxiv.com/k8unc/ (accessed on 1 September 2021).
- Pennycook, G.; McPhetres, J.; Zhang, Y.; Lu, J.G.; Rand, D.G. Fighting COVID-19 misinformation on social media: Experimental evidence for a scalable accuracy-nudge intervention. Psychol. Sci. 2020, 31, 770–780. [Google Scholar] [CrossRef] [PubMed]
- Sorokowski, P.; Groyecka, A.; Kowal, M.; Sorokowska, A.; Białek, M.; Lebuda, I.; Dobrowolska, M.; Zdybek, P.; Karwowski, M. Can information about pandemics increase negative attitudes toward foreign groups? A case of COVID-19 outbreak. Sustainability 2020, 12, 4912. [Google Scholar] [CrossRef]
- Clements, J.M. Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic: Cross-sectional online questionnaire. JMIR Public Health Surveill. 2020, 6, e19161. [Google Scholar] [CrossRef] [PubMed]
- Constantinou, M.; Kagialis, A.; Karekla, M. COVID-19 Scientific Facts vs. Conspiracy Theories: 0–1: Science Fails to Convince Even Highly Educated Individuals. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-33972/v1 (accessed on 1 September 2021).
- Georgiou, N.; Delfabbro, P.; Balzan, R. COVID-19-related conspiracy beliefs and their relationship with perceived stress and pre-existing conspiracy beliefs. Personal. Individ. Differ. 2020, 166, 110201. [Google Scholar] [CrossRef]
- Mohd Hanafiah, K.; Wan, C.D. Public Knowledge, Perception and Communication Behavior Surrounding COVID-19 in Malaysia. 2020, Advance: A SAGE Preprints Community. Available online: https://advance.sagepub.com/articles/preprint/Public_knowledge_perception_and_communication_behavior_surrounding_COVID-19_in_Malaysia/12102816 (accessed on 1 September 2021).
- Alper, S.; Bayrak, F.; Yilmaz, O. Psychological correlates of COVID-19 conspiracy beliefs and preventive measures: Evidence from Turkey. Curr. Psychol. 2020, 40, 5708–5717. [Google Scholar] [CrossRef]
- Biddlestone, M.; Green, R.; Douglas, K.M. Cultural orientation, power, belief in conspiracy theories, and intentions to reduce the spread of COVID-19. Br. J. Soc. Psychol. 2020, 59, 663–673. [Google Scholar] [CrossRef]
- Sternisko, A.; Cichocka, A.; Cislak, A.; Van Bavel, J.J. Collective Narcissism Predicts the Belief and Dissemination of Conspiracy Theories during the COVID-19 Pandemic. 2020, Psyarxiv. Available online: https://psyarxiv.com/4c6av/ (accessed on 1 September 2021).
- Bertin, P.; Nera, K.; Delouvée, S. Conspiracy beliefs, chloroquine, and the rejection of vaccination: A conceptual replication-extension in the COVID-19 pandemic context. PsyArXiv Prepr. 2020. [Google Scholar] [CrossRef]
- Teovanović, P.; Lukić, P.; Zupan, Z.; Lazić, A.; Ninković, M.; Žeželj, I. Irrational beliefs differentially predict adherence to guidelines and pseudoscientific practices during the COVID-19 pandemic. Appl. Cogn. Psychol. 2021, 35, 486–496. [Google Scholar] [CrossRef]
- Lobato, E.J.; Powell, M.; Padilla, L.M.; Holbrook, C. Factors predicting willingness to share COVID-19 misinformation. Front. Psychol. 2020, 11, 2413. [Google Scholar] [CrossRef]
- Ma, H.; Miller, C. Trapped in a double bind: Chinese overseas student anxiety during the COVID-19 pandemic. Health Commun. 2021, 36, 1598–1605. [Google Scholar] [CrossRef]
- Qi, R.; Chen, W.; Liu, S.; Thompson, P.M.; Zhang, L.J.; Xia, F.; Cheng, F.; Hong, A.; Surento, W.; Luo, S.; et al. Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: Prevalence and associated biopsychosocial risk factors. medRxiv 2020. [Google Scholar] [CrossRef]
- Tull, M.; Edmonds, K.; Scamaldo, K.; Richmond, J.; Rose, J.; Gratz, K. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020, 289, 113098. [Google Scholar] [CrossRef] [PubMed]
- Skalski, S.; Uram, P.; Dobrakowski, P.; Kwiatkowska, A. The link between ego-resiliency, social support, SARS-CoV-2 anxiety and trauma effects. Polish adaptation of the Coronavirus Anxiety Scale. Personal. Individ. Differ. 2021, 171, 110540. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Nobles, J.; Martin, F.; Dawson, S.; Moran, P.; Savovic, J. The Potential Impact of COVID-19 on Mental Health Outcomes and the Implications for Service Solutions; National Institute for Health Research, University of Bristol: Bristol, UK, 2020. [Google Scholar]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The multidimensional scale of perceived social support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Shuiyuan, X. The Social Support Rating Scale. In Handbook of Psychological Health Rating Scales; Mental Health Publishing House: Beijing, China, 1999; pp. 127–130. [Google Scholar]
- Sarason, I.G.; Levine, H.M.; Basham, R.B.; Sarason, B.R. Assessing social support: The social support questionnaire. J. Personal. Soc. Psychol. 1983, 44, 127. [Google Scholar] [CrossRef]
- Cutrona, C.E.; Russell, D.W. The provisions of social relationships and adaptation to stress. Adv. Pers. Relatsh. 1987, 1, 37–67. [Google Scholar]
- Alvis, L.; Shook, N.; Oosterhoff, B. Adolescents’ prosocial experiences during the covid-19 pandemic: Associations with mental health and community attachments. Curr. Psychol. 2022. [Google Scholar] [CrossRef]
- Lv, Y.; Yao, H.; Xi, Y.; Zhang, Z.; Zhang, Y.; Chen, J.; Li, J.; Li, J.; Wang, X.; Luo, G. Social Support Protects Chinese Medical Staff from Suffering Psychological Symptoms in COVID-19 Defense. 2020, SSRN. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3557996 (accessed on 1 September 2021).
- Raude, J.; Lecrique, J.M.; Lasbeur, L.; Leon, C.; Guignard, R.; Roscoät, E.D.; Arwidson, P. Determinants of preventive behaviors in response to the COVID-19 pandemic in France: Comparing the sociocultural, psychosocial and social cognitive explanations. Front. Psychol. 2020, 11, 3345. [Google Scholar] [CrossRef]
- Kong, X.; Zheng, K.; Tang, M.; Kong, F.; Zhou, J.; Diao, L.; Wu, S.; Jiao, P.; Su, T.; Dong, Y. Prevalence and factors associated with depression and anxiety of hospitalized patients with COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Sibley, C.G.; Greaves, L.M.; Satherley, N.; Wilson, M.S.; Overall, N.C.; Lee, C.H.; Milojev, P.; Bulbulia, J.; Osborne, D.; Milfont, T.L.; et al. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am. Psychol. 2020, 75, 618. [Google Scholar] [CrossRef] [PubMed]
- Wright, L.; Steptoe, A.; Fancourt, D. Are adversities and worries during the COVID-19 pandemic related to sleep quality? Longitudinal analyses of 46,000 UK adults. PLoS ONE 2021, 16, e0248919. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020, 26, e923549-1. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Li, M.; Li, Z.; Xiang, W.; Yuan, Y.; Liu, Y.; Li, Z.; Xiong, Z. Coping style, social support and psychological distress in the general Chinese population in the early stages of the COVID-19 epidemic. BMC Psychiatry 2020, 20, 426. [Google Scholar] [CrossRef]
- Huang, L.; Xu, F.; Liu, H. Emotional responses and coping strategies of nurses and nursing college students during COVID-19 outbreak. medRxiv 2020. [Google Scholar] [CrossRef]
- Wang, H.; Xia, Q.; Xiong, Z.; Li, Z.; Xiang, W.; Yuan, Y.; Liu, Y.; Li, Z. The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: A web-based survey. PLoS ONE 2020, 15, e0233410. [Google Scholar] [CrossRef]
- Flesia, L.; Monaro, M.; Mazza, C.; Fietta, V.; Colicino, E.; Segatto, B.; Roma, P. Predicting perceived stress related to the COVID-19 outbreak through stable psychological traits and machine learning models. J. Clin. Med. 2020, 9, 3350. [Google Scholar] [CrossRef]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The effect of COVID-19 on youth mental health. Psychiatr. Q. 2020, 91, 841–852. [Google Scholar] [CrossRef]
- Li, J.B.; Yang, A.; Dou, K.; Cheung, R.Y. Self-control moderates the association between perceived severity of coronavirus disease 2019 (COVID-19) and mental health problems among the Chinese public. Int. J. Environ. Res. Public Health 2020, 17, 4820. [Google Scholar] [CrossRef]
- Umucu, E.; Lee, B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil. Psychol. 2020, 65, 193. [Google Scholar] [CrossRef]
- Cerami, C.; Santi, G.C.; Galandra, C.; Dodich, A.; Cappa, S.F.; Vecchi, T.; Crespi, C. COVID-19 outbreak in Italy: Are we ready for the psychosocial and the economic crisis? Baseline findings from the PsyCovid study. Front. Psychiatry 2020, 11, 556. [Google Scholar] [CrossRef] [PubMed]
- Ng, D.W.; Chan, F.H.; Barry, T.J.; Lam, C.; Chong, C.Y.; Kok, H.C.; Liao, Q.; Fielding, R.; Lam, W.W. Psychological distress during the 2019 coronavirus disease (COVID-19) pandemic among cancer survivors and healthy controls. Psych. Oncolog. 2020, 29. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.; Seligman, M.E. Character Strengths and Virtues: A Handbook and Classification; American Psychological Association & Oxford University Press: New York, NY, USA, 2004. [Google Scholar]
- Carver, C.S. You want to measure coping but your protocol’too long: Consider the brief cope. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Foà, C.; Tonarelli, A.; Caricati, L.; Fruggeri, L. COPE-NVI-25: Validazione italiana della versione ridotta della Coping Orientation to the Problems Experienced (COPE-NVI). Psicol. Della Salut. 2015, 2, 123–140. [Google Scholar]
- Rosenstiel, A.K.; Keefe, F.J. The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain 1983, 17, 33–44. [Google Scholar] [CrossRef]
- Xie, Y. Reliability and validity of the simplified coping style questionnaire. Chin. J. Clin. Psychol. 1998, 6, 114–115. [Google Scholar]
- Li, M.; Wang, M.C.; Shou, Y.; Zhong, C.; Ren, F.; Zhang, X.; Yang, W. Psychometric properties and measurement invariance of the brief symptom inventory-18 among chinese insurance employees. Front. Psychol. 2018, 9, 519. [Google Scholar] [CrossRef]
- Ala’a, B.; Akour, A.; Alfalah, L. Is it just about physical health? An internet-based cross-sectional study exploring the psychological impacts of COVID-19 pandemic on university students in Jordan using Kessler Psychological Distress Scale. medRxiv 2020. [Google Scholar] [CrossRef]
- Cai, H.; Tu, B.; Ma, J.; Chen, L.; Fu, L.; Jiang, Y.; Zhuang, Q. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020, 26, e924171-1. [Google Scholar]
- Papini, S.; Dainer-Best, J.; Rubin, M.; Zaizar, E.D.; Telch, M.J.; Smits, J.A. Psychological Networks Can Identify Potential Pathways to Specific Intervention Targets for Anxiety in Response to Coronavirus Disease 2019 (COVID-19). 2020, Psyarxiv. Available online: https://psyarxiv.com/4zr25/ (accessed on 1 September 2021).
- Park, C.L.; Russell, B.S.; Fendrich, M.; Finkelstein-Fox, L.; Hutchison, M.; Becker, J. Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. J. Gen. Intern. Med. 2020, 35, 2296–2303. [Google Scholar] [CrossRef]
- Shechter, A.; Diaz, F.; Moise, N.; Anstey, D.E.; Ye, S.; Agarwal, S.; Birk, J.L.; Brodie, D.; Cannone, D.E.; Chang, B.; et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry 2020, 66, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Yao, J.; Narayanan, J. Mindfulness Buffers the Impact of COVID-19 Outbreak Information on Sleep Duration. 2020, Psyarxiv. Available online: https://psyarxiv.com/wuh94/ (accessed on 1 September 2021).
- Yang, Z.; Ji, L.J.; Yang, Y.; Wang, X.; Zhang, M.; Xie, Y.; Su, Z.; Zhou, W.; Chen, J.; Jing, Y.; et al. COVID-19 Outbreak Enhances Making Meaning in Negative Experiences: Evidence from China. 2020, Psyarxiv. Available online: https://psyarxiv.com/9twhb/ (accessed on 1 September 2021).
- Chwaszcz, J.; Palacz-Chrisidis, A.; Wiechetek, M.; Bartczuk, R.P.; Niewiadomska, I.; Wośko, P.; Sławska-Jaroszewska, P. The quality of life, resources, and coping during the first weeks of the COVID-19 pandemic in people seeking psychological counselling before the pandemic. Int. J. Occup. Med. Environ. Health 2021, 34, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Peng, J. Coping Strategies as Predictors of Anxiety: Exploring positive experience of Chinese university in health education in COVID-19 pandemic. Creat. Educ. 2020, 11, 735–750. [Google Scholar] [CrossRef]
- Abdelrahman, M. Personality traits, risk perception, and protective behaviors of Arab residents of Qatar during the COVID-19 pandemic. Int. J. Ment. Health Addict. 2020, 20, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Zong, M.; Yang, Z.; Gu, W.; Dong, D.; Qiao, Z. When altruists cannot help: The influence of altruism on the mental health of university students during the COVID-19 pandemic. Glob. Health 2020, 16, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Slovic, P.; Fischhoff, B.; Lichtenstein, S. Why study risk perception? Risk Anal. 1982, 2, 83–93. [Google Scholar] [CrossRef]
- Dohle, S.; Wingen, T.; Schreiber, M. Acceptance and adoption of protective measures during the COVID-19 pandemic: The role of trust in politics and trust in science. Soc. Psychol. Bull. 2020, 15, 1–23. [Google Scholar] [CrossRef]
- Lee, M.; You, M. Psychological and behavioral responses in South Korea during the early stages of coronavirus disease 2019 (COVID-19). Int. J. Environ. Res. Public Health 2020, 17, 2977. [Google Scholar] [CrossRef]
- Glöckner, A.; Dorrough, A.R.; Wingen, T.; Dohle, S. The Perception of Infection Risks during the Early and Later Outbreak of COVID-19 in Germany: Consequences and Recommendations. 2020, Psyarxiv. Available online: https://psyarxiv.com/wdbgc/ (accessed on 1 September 2021).
- Dai, B.; Fu, D.; Meng, G.; Liu, B.; Li, Q.; Liu, X. The effects of governmental and individual predictors on COVID-19 protective behaviors in China: A path analysis model. Public Adm. Rev. 2020, 80, 797–804. [Google Scholar] [CrossRef]
- Jørgensen, F.J.; Bor, A.; Petersen, M.B. Compliance without fear: Predictors of protective behavior during the first wave of the COVID-19 pandemic. PsyArXiv 2020, 26, 679–696. [Google Scholar] [CrossRef]
- Marinthe, G.; Brown, G.; Delouvée, S.; Jolley, D. Looking out for myself: Exploring the relationship between conspiracy mentality, perceived personal risk, and COVID-19 prevention measures. Br. J. Health Psychol. 2020, 25, 957–980. [Google Scholar] [CrossRef] [PubMed]
- Nese, M.; Riboli, G.; Brighetti, G.; Sassi, V.; Camela, E.; Caselli, G.; Sassaroli, S.; Borlimi, R. Delay discounting of compliance with containment measures during the COVID-19 outbreak: A survey of the Italian population. J. Public Health 2020, 30, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Wise, T.; Zbozinek, T.D.; Michelini, G.; Hagan, C.C.; Mobbs, D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. R. Soc. Open Sci. 2020, 7, 200742. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, M.; Arslan, G. Exploring the associations between resilience, dispositional hope, preventive behaviours, subjective well-being, and psychological health among adults during early stage of COVID-19. Curr. Psychol. 2020, 14, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, M.; Geçer, E.; Akgül, Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychol. Health Med. 2021, 26, 35–43. [Google Scholar] [CrossRef]
- Witte, K. Fear control and danger control: A test of the extended parallel process model (EPPM). Commun. Monogr. 1994, 61, 113–134. [Google Scholar] [CrossRef]
- Huynh, T.L. The COVID-19 risk perception: A survey on socioeconomics and media attention. Econ. Bull 2020, 40, 758–764. [Google Scholar]
- Liu, M.; Zhang, H.; Huang, H. Media exposure to COVID-19 information, risk perception, social and geographical proximity, and self-rated anxiety in China. BMC Public Health 2020, 20, 1649. [Google Scholar] [CrossRef]
- Olagoke, A.A.; Olagoke, O.O.; Hughes, A.M. Exposure to coronavirus news on mainstream media: The role of risk perceptions and depression. Br. J. Health Psychol. 2020, 25, 865–874. [Google Scholar] [CrossRef]
- Bettinsoli, M.; Di Riso, D.; Napier, J.; Moretti, L.; Bettinsoli, P.; Delmedico, M.; Piazzolla, A.; Moretti, B. Psychological impact and contextual factors associated with physical and mental health conditions of Italian Healthcare Professionals during the COVID-19 disease outbreak. Appl. Psychol. Health Well-Being 2020, 12, 1054–1073. [Google Scholar] [CrossRef]
- Jahangiry, L.; Bakhtari, F.; Sohrabi, Z.; Reihani, P.; Samei, S.; Ponnet, K.; Montazeri, A. Risk perception related to COVID-19 among the Iranian general population: An application of the extended parallel process model. BMC Public Health 2020, 20, 1571. [Google Scholar] [CrossRef] [PubMed]
- Barber, S.J.; Kim, H. COVID-19 worries and behavior changes in older and younger men and women. J. Gerontol. Ser. B 2021, 76, e17–e23. [Google Scholar] [CrossRef] [PubMed]
- Bischetti, L.; Canal, P.; Bambini, V. Funny but aversive: A large-scale survey of the emotional response to COVID-19 humor in the Italian population during the lockdown. Lingua 2021, 249, 102963. [Google Scholar] [CrossRef]
- De Neys, W.; Raoelison, M.; Boissin, E.; Voudouri, A.; Bago, B.; Białek, M. Moral Outrage and Social Distancing: Bad or Badly Informed Citizens? 2020, Psyarxiv. Available online: https://psyarxiv.com/j9h76/ (accessed on 1 September 2021).
- Garbe, L.; Rau, R.; Toppe, T. Influence of perceived threat of COVID-19 and HEXACO personality traits on toilet paper stockpiling. PLoS ONE 2020, 15, e0234232. [Google Scholar] [CrossRef] [PubMed]
- Germani, A.; Buratta, L.; Delvecchio, E.; Mazzeschi, C. Emerging adults and COVID-19: The role of individualism-collectivism on perceived risks and psychological maladjustment. Int. J. Environ. Res. Public Health 2020, 17, 3497. [Google Scholar] [CrossRef]
- Globig, L.K.; Blain, B.; Sharot, T. When Private Optimism Meets Public Despair: Dissociable Effects on Behavior and Well-Being. 2020, Psyarxiv. Available online: https://psyarxiv.com/gbdn8/ (accessed on 1 September 2021).
- Huynh, T.D. The more I fear about COVID-19, the more I wear medical masks: A survey on risk perception and medical masks uses. medRxiv 2020. [Google Scholar] [CrossRef]
- Iorfa, S.K.; Ottu, I.F.; Oguntayo, R.; Ayandele, O.; Kolawole, S.O.; Gandi, J.C.; Dangiwa, A.L.; Olapegba, P.O. COVID-19 knowledge, risk perception, and precautionary behavior among nigerians: A moderated mediation approach. Front. Psychol. 2020, 11, 3292. [Google Scholar] [CrossRef]
- Kachanoff, F.; Bigman, Y.; Kapsaskis, K.; Gray, K. Measuring two distinct psychological threats of covid-19 and their unique impacts on wellbeing and adherence to public health behaviors. Soc. Psychol. Personal. Sci. 2021, 12, 603–616. [Google Scholar] [CrossRef]
- Martin, C.C. HEXACO Traits, Big Five Traits, and COVID-19. 2020, Psyarxiv. Available online: https://psyarxiv.com/c9gxe/ (accessed on 1 September 2021).
- Niepel, C.; Kranz, D.; Borgonovi, F.; Emslander, V.; Greiff, S. The coronavirus (COVID-19) fatality risk perception of US adult residents in March and April 2020. Br. J. Health Psychol. 2020, 25, 883–888. [Google Scholar] [CrossRef]
- Okruszek, L.; Aniszewska-Stańczuk, A.; Piejka, A.; Wiśniewska, M.; Żurek, K. Safe But lonely? Loneliness, Mental Health Symptoms and COVID-19; 2020, Psyarxiv. Available online: https://psyarxiv.com/9njps/ (accessed on 1 September 2021).
- Pennycook, G.; McPhetres, J.; Bago, B.; Rand, D.G. Predictors of attitudes and misperceptions about COVID-19 in Canada, the UK, and the USA. PsyArXiv 2020, 10, 1–25. [Google Scholar]
- Simione, L.; Gnagnarella, C. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. Front. Psychol. 2020, 11, 2166. [Google Scholar] [CrossRef] [PubMed]
- Rothgerber, H.; Wilson, T.; Whaley, D.; Rosenfeld, D.L.; Humphrey, M.; Moore, A.; Bihl, A. Politicizing the COVID-19 Pandemic: Ideological Differences in Adherence to Social Distancing. 2020, Psyarxiv. Available online: https://psyarxiv.com/k23cv/ (accessed on 1 September 2021).
- Kim, A.W.; Nyengerai, T.; Mendenhall, E. Evaluating the mental health impacts of the COVID-19 pandemic: Perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms in urban South Africa. Psychol. Med. 2020, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Marotta, L.; Pesce, A.; Guazzini, A. Before and after the Quarantine: An Approximate Study on the Psychological Impact of COVID-19 on the Italian Population during the Lockdown Period. Future Internet 2020, 12, 229. [Google Scholar] [CrossRef]
- Gainforth, H.L.; Cao, W.; Latimer-Cheung, A.E. Determinants of human papillomavirus (HPV) vaccination intent among three Canadian target groups. J. Cancer Educ. 2012, 27, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.C.; Highhouse, S.; Nye, C.D. Development and validation of the general risk propensity scale (GRiPS). J. Behav. Decis. Mak. 2019, 32, 152–167. [Google Scholar] [CrossRef]
- Yıldırım, M.; Arslan, G.; Özaslan, A. Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: Exploring the mediating effects of resilience and coronavirus fear. Int. J. Ment. Health Addict. 2020, 16, 1–11. [Google Scholar] [CrossRef]
- Plohl, N.; Musil, B. Modeling compliance with COVID-19 prevention guidelines: The critical role of trust in science. Psychol. Health Med. 2021, 26, 1–12. [Google Scholar] [CrossRef]
- Wolff, W.; Martarelli, C.S.; Schüler, J.; Bieleke, M. High boredom proneness and low trait self-control impair adherence to social distancing guidelines during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5420. [Google Scholar] [CrossRef]
- Leder, J.; Pastukhov, A.S.; Schütz, A. Even Prosocially Oriented Individuals Save Themselves First: Social Value Orientation, Subjective Effectiveness and the Usage of Protective Measures during the COVID-19 Pandemic in Germany. 2020, Psyarxiv. Available online: https://psyarxiv.com/nugcr/ (accessed on 1 September 2021).
- Mækelæ, M.J.; Reggev, N.; Dutra, N.; Tamayo, R.M.; Silva-Sobrinho, R.A.; Klevjer, K.; Pfuhl, G. Perceived efficacy of COVID-19 restrictions, reactions and their impact on mental health during the early phase of the outbreak in six countries. R. Soc. Open Sci. 2020, 7, 200644. [Google Scholar] [CrossRef]
- Hoffart, A.; Johnson, S.U.; Ebrahimi, O.V. Loneliness and social distancing during the COVID-19 pandemic: Risk factors and associations with psychopathology. Front. Psychiatry 2020, 11, 1297. [Google Scholar] [CrossRef]
- Zickfeld, J.; Schubert, T.; Herting, A.; Grahe, J.; Faasse, K. Predictors of health-protective behavior and changes over time during the outbreak of the COVID-19 pandemic in Norway. Front Psychol. 2020, 11, 564083. [Google Scholar] [CrossRef] [PubMed]
- Zettler, I.; Schild, C.; Lilleholt, L.; Böhm, R. Individual differences in accepting personal restrictions to fight the COVID-19 pandemic: Results from a Danish adult sample. PsyArXiv Prepr. 2020, 10. [Google Scholar] [CrossRef]
- Charles, G.; Jain, M.; Caplan, Y.; Kemp, H.; Keisler, A.; Huang, V.; Sgaier, S.K. Increasing Uptake of Social Distancing during COVID-19: Machine Learning Strategies for Targeted Interventions. SSRN 2020. [Google Scholar] [CrossRef]
- Abu-Akel, A.; Spitz, A.; West, R. Who is listening? Spokesperson effect on communicating social and physical distancing measures during the COVID-19 pandemic. Front. Psychol. 2020, 11, 564434. [Google Scholar] [CrossRef] [PubMed]
- Bacon, A.M.; Corr, P.J. Coronavirus (COVID-19) in the United Kingdom: A personality-based perspective on concerns and intention to self-isolate. Br. J. Health Psychol. 2020, 25, 839–848. [Google Scholar] [CrossRef] [PubMed]
- Bogg, T.; Milad, E. Slowing the spread of COVID-19: Demographic, personality, and social cognition predictors of guideline adherence in a representative US sample. PsyArXiv 2020. [Google Scholar] [CrossRef]
- Briscese, G.; Lacetera, N.; Macis, M.; Tonin, M. Compliance with COVID-19 Social-Distancing Measures in Italy: The Role of Expectations and Duration; National Bureau of Economic Research Cambridge: Cambridge, MA, USA, 2020. [Google Scholar]
- Carvalho, L.d.F.; Pianowski, G.; Gonçalves, A.P. Personality differences and COVID-19: Are extroversion and conscientiousness personality traits associated with engagement with containment measures? Trends Psychiatry Psychother. 2020, 42, 179–184. [Google Scholar] [CrossRef]
- Capraro, V.; Barcelo, H. Priming reasoning increases intentions to wear a face covering to slow down COVID-19 transmission. arXiv 2020, arXiv:2006.11273. [Google Scholar]
- Erceg, N.; Ružojčić, M.; Galić, Z. Misbehaving in the corona crisis: The role of anxiety and unfounded beliefs. Curr. Psychol. 2020, 1–10. [Google Scholar] [CrossRef]
- Farias, J.E.M.; Pilati, R. Violating Social Distancing Amid the COVID-19 Pandemic: Psychological Factors to Improve Compliance. J. Appl. Soc. Psychol. 2020. [Google Scholar] [CrossRef]
- Gibson Miller, J.; Hartman, T.K.; Levita, L.; Martinez, A.P.; Mason, L.; McBride, O.; McKay, R.; Murphy, J.; Shevlin, M.; Stocks, T.V.; et al. Capability, opportunity, and motivation to enact hygienic practices in the early stages of the COVID-19 outbreak in the United Kingdom. Br. J. Health Psychol. 2020, 25, 856–864. [Google Scholar] [CrossRef] [PubMed]
- Gollwitzer, A.; McLoughlin, K.; Martel, C.; Marshall, J.; Höhs, J.M.; Bargh, J.A. Connecting Self-Reported Social Distancing to Real-World Behavior During the COVID-19 Pandemic. 2020, Psyraxiv. Available online: https://psyarxiv.com/kvnwp/ (accessed on 1 September 2021).
- Imtiaz, A.; Khan, N.M.; Hossain, M.A. COVID-19 in Bangladesh: Measuring differences in individual precautionary behaviors among young adults. J. Public Health 2021, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, N.C.; Lekkas, D.; Price, G.; Heinz, M.V.; Song, M.; O’Malley, A.J.; Barr, P.J. Flattening the mental health curve: COVID-19 stay-at-home orders are associated with alterations in mental health search behavior in the United States. JMIR Ment. Health 2020, 7, e19347. [Google Scholar] [CrossRef] [PubMed]
- Lees, J.; Cetron, J.S.; Vollberg, M.C.; Reggev, N.; Cikara, M. Intentions to Comply with COVID-19 Preventive Behaviors Are Associated with Personal BELIEFS, independent of Perceived Social Norms. 2020, Psyarxiv. Available online: https://psyarxiv.com/97jry/ (accessed on 1 September 2021).
- Li, J.B.; Yang, A.; Dou, K.; Wang, L.X.; Zhang, M.C.; Lin, X.Q. Chinese public’s knowledge, perceived severity, and perceived controllability of COVID-19 and their associations with emotional and behavioural reactions, social participation, and precautionary behaviour: A national survey. BMC Public Health 2020, 20, 1589. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.M.; Tun, Z.M.; Kumar, V.; Quaye, S.E.D.; Offeddu, V.; Cook, A.R.; Lwin, M.O.; Jiang, S.; Tam, C.C. Population anxiety and positive behaviour change during the COVID-19 epidemic: Cross-sectional surveys in Singapore, China and Italy. Influenza Other Respir. Viruses 2021, 15, 45–55. [Google Scholar] [CrossRef]
- Liu, X.; Luo, W.T.; Li, Y.; Li, C.N.; Hong, Z.S.; Chen, H.L.; Xiao, F.; Xia, J.Y. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect. Dis. Poverty 2020, 9, 1–11. [Google Scholar] [CrossRef]
- Lunn, P.D.; Timmons, S.; Belton, C.A.; Barjaková, M.; Julienne, H.; Lavin, C. Motivating social distancing during the COVID-19 pandemic: An online experiment. Soc. Sci. Med. 2020, 265, 113478. [Google Scholar] [CrossRef]
- Martarelli, C.S.; Wolff, W. Too bored to bother? Boredom as a potential threat to the efficacy of pandemic containment measures. Humanit. Soc. Sci. Commun. 2020, 7, 1–5. [Google Scholar] [CrossRef]
- Nivette, A.; Ribeaud, D.; Murray, A.; Steinhoff, A.; Bechtiger, L.; Hepp, U.; Shanahan, L.; Eisner, M. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Soc. Sci. Med. 2021, 268, 113370. [Google Scholar] [CrossRef]
- Okten, I.O.; Gollwitzer, A.; Oettingen, G. Gender Differences in Preventing the Spread of Coronavirus. Behav. Sci. Policy 2020, 6, 109–122. [Google Scholar] [CrossRef]
- Oosterhoff, B.; Palmer, C.A. Psychological Correlates of News Monitoring, Social Distancing, Disinfecting, and Hoarding Behaviors among US Adolescents during the COVID-19 Pandemic. 2020, Psyarxiv. Available online: https://psyarxiv.com/rpcy4/ (accessed on 1 September 2021).
- Pfattheicher, S.; Nockur, L.; Böhm, R.; Sassenrath, C.; Petersen, M.B. The emotional path to action: Empathy promotes physical distancing and wearing of face masks during the COVID-19 pandemic. Psychol. Sci. 2020, 31, 1363–1373. [Google Scholar] [CrossRef] [PubMed]
- Qian, M.; Wu, Q.; Wu, P.; Hou, Z.; Liang, Y.; Cowling, B.J.; Yu, H. Psychological responses, behavioral changes and public perceptions during the early phase of the COVID-19 outbreak in China: A population based cross-sectional survey. medRxiv 2020. [Google Scholar] [CrossRef]
- Sarkar, A.; Liu, G.; Jin, Y.; Xie, Z.; Zheng, Z.J. Public health preparedness and responses to the coronavirus disease 2019 (COVID-19) pandemic in South Asia: A situation and policy analysis. Glob. Health J. 2020, 4, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Saurabh, K.; Ranjan, S. Compliance and psychological impact of quarantine in children and adolescents due to COVID-19 pandemic. Indian J. Pediatrics 2020, 87, 532–536. [Google Scholar] [CrossRef]
- Swami, V.; Barron, D. Analytic Thinking, Rejection of Coronavirus (COVID-19) Conspiracy Theories, and Compliance with Mandated Social-Distancing: Direct and Indirect Relationships in a Nationally Representative Sample of Adults in the United Kingdom. 2020 OSFPreprint. Available online: https://osf.io/nmx9w (accessed on 1 September 2021).
- Tan, W.; Hao, F.; McIntyre, R.S.; Jiang, L.; Jiang, X.; Zhang, L.; Zhao, X.; Zou, Y.; Hu, Y.; Luo, X.; et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 2020, 87, 84–92. [Google Scholar] [CrossRef]
- van Holm, E.J.; Monaghan, J.; Shahar, D.C.; Messina, J.; Surprenant, C. The impact of political ideology on concern and behavior during COVID-19. SSRN 2020. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Imani, V.; Lin, C.Y.; Timpka, T.; Broström, A.; Updegraff, J.A.; Årestedt, K.; Griffiths, M.D.; Pakpour, A.H. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: An actor-partner interdependence modelling. Int. J. Ment. Health Addict. 2020, 20, 68–82. [Google Scholar] [CrossRef]
- Blagov, P.S. Adaptive and dark personality in the COVID-19 pandemic: Predicting health-behavior endorsement and the appeal of public-health messages. Soc. Psychol. Personal. Sci. 2021, 12, 697–707. [Google Scholar] [CrossRef]
- Hays, R.D.; DiMatteo, M.R. A short-form measure of loneliness. J. Personal. Assess. 1987, 51, 69–81. [Google Scholar] [CrossRef]
- Kwiatkowska, M.M.; Rogoza, R.; Kwiatkowska, K. Analysis of the Psychometric Properties of the Revised UCLA Loneliness Scale in the Polish Adolescent Sample. 2018, Psyarxiv. Available online: https://psyarxiv.com/m6udc/ (accessed on 1 September 2021).
- Blakey, S.M.; Reuman, L.; Jacoby, R.J.; Abramowitz, J.S. Tracing “Fearbola”: Psychological predictors of anxious responding to the threat of ebola. Cogn. Ther. Res. 2015, 39, 816–825. [Google Scholar] [CrossRef]
- Kuiper, M.E.; de Bruijn, A.L.; Reinders Folmer, C.; Olthuis, E.; Brownlee, M.; Kooistra, E.B.; Fine, A.; Van Rooij, B. The intelligent lockdown: Compliance with COVID-19 mitigation measures in the Netherlands. Amst. Law Sch. Res. Pap. 2020. [Google Scholar] [CrossRef]
- Michie, S.; Atkins, L.; West, R. The behaviour change wheel. In A Guide to Designing Interventions, 1st ed.; Silverback Publishing: Sutton, UK, 2014; pp. 1003–1010. [Google Scholar]
- Bello-Pardo, E.D.; Nayak, M.; Ray, J. New Coronavirus Polling Shows Americans Are Responding to the Threat Unevenly. 2020. Available online: https://yougovblue.medium.com/new-coronavirus-polling-shows-americans-are-responding-to-the-threat-unevenly-641026301516 (accessed on 1 September 2021).
- Harper, C.A.; Satchell, L.P.; Fido, D.; Latzman, R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addict. 2020, 19, 1875–1888. [Google Scholar] [CrossRef] [PubMed]
- Folmer, C.R.; Kuiper, M.; Olthuis, E.; Kooistra, E.B.; de Bruijn, A.L.; Brownlee, M.; Fine, A.; van Rooij, B. Compliance in the 1.5 Meter Society: Longitudinal Analysis of Citizens’ Adherence to COVID-19 Mitigation Measures in a Representative Sample in the Netherlands. 2020, Psyarxiv. Available online: https://psyarxiv.com/dr9q3/ (accessed on 1 September 2021).
- Lauri Korajlija, A.; Jokic-Begic, N. COVID-19: Concerns and behaviours in Croatia. Br. J. Health Psychol. 2020, 25, 849–855. [Google Scholar] [CrossRef]
- Balzarini, R.N.; Muise, A.; Zoppolat, G.; Di Bartolomeo, A.; Rodrigues, D.L.; Alonso-Ferres, M.; Urganci, B.; Debrot, A.; Pichayayothin, N.B.; Dharma, C.; et al. Love in the Time of COVID: Perceived Partner Responsiveness Buffers People from Lower Relationship Quality Associated with COVID-Related Stressors. 2020, Psyarxiv. Available online: https://psyarxiv.com/e3fh4/ (accessed on 1 September 2021).
- Xie, W.; Campbell, S.; Zhang, W. Working memory capacity predicts individual differences in social-distancing compliance during the COVID-19 pandemic in the United States. Proc. Natl. Acad. Sci. USA 2020, 117, 17667–17674. [Google Scholar] [CrossRef] [PubMed]
- Casali, N.; Feraco, T.; Ghisi, M.; Meneghetti, C. “Andrà Tutto Bene”. The Effect of Character Strengths on Psychological Distress and Self-Efficacy during COVID-19 Lockdown. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-35332/v1 (accessed on 1 September 2021).
- Huang, Y.; Zhao, N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychol. Health Med. 2021, 26, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Özdin, S.; Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- ÇITAK, Ş.; Pekdemir, Ü. An analysis on sleep habits and generalized anxiety levels of individuals during the COVID-19 pandemic. J. Fam. Couns. Educ. 2020, 5, 60–73. [Google Scholar] [CrossRef]
- Taylor, S. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease; Cambridge Scholars Publishing: Cambridge, UK, 2019. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The fear of COVID-19 scale: Development and initial validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.R.; Henry, J.D. The Depression Anxiety Stress Scales (DASS): Normative data and latent structure in a large non-clinical sample. Br. J. Clin. Psychol. 2003, 42, 111–131. [Google Scholar] [CrossRef] [PubMed]
- Si, C.; Pan, Y. A study on the correlation between the Hamilton depression and anxiety scales and the positive and negative affect schedule. Gen. Care 2019, 17, 140–142. [Google Scholar]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893. [Google Scholar] [CrossRef] [PubMed]
- Salkovskis, P.M.; Rimes, K.A.; Warwick, H.; Clark, D.M. The Health Anxiety Inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol. Med. 2002, 32, 843–853. [Google Scholar] [CrossRef]
- Giang, K.B.; Allebeck, P.; Kullgren, G.; Van Tuan, N. The Vietnamese version of the Self Reporting Questionnaire 20 (SRQ-20) in detecting mental disorders in rural Vietnam: A validation study. Int. J. Soc. Psychiatry 2006, 52, 175–184. [Google Scholar] [CrossRef]
- Wheaton, M.G.; Abramowitz, J.S.; Berman, N.C.; Fabricant, L.E.; Olatunji, B.O. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cogn. Ther. Res. 2012, 36, 210–218. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Gater, R.; Sartorius, N.; Ustun, T.B.; Piccinelli, M.; Gureje, O.; Rutter, C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef]
- Quinn, H.; Thissen, D.; Liu, Y.; Magnus, B.; Lai, J.S.; Amtmann, D.; Varni, J.W.; Gross, H.E.; DeWalt, D.A. Using item response theory to enrich and expand the PROMIS® pediatric self report banks. Health Qual. Life Outcomes 2014, 12, 1–10. [Google Scholar] [CrossRef]
- Lee, S.A. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud. 2020, 44, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Zung, W.W. A rating instrument for anxiety disorders. Psychosom. J. Consult. Liaison Psychiatry 1971, 12, 371–379. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Schalet, B.D.; Pilkonis, P.A.; Yu, L.; Dodds, N.; Johnston, K.L.; Yount, S.; Riley, W.; Cella, D. Clinical validity of PROMIS depression, anxiety, and anger across diverse clinical samples. J. Clin. Epidemiol. 2016, 73, 119–127. [Google Scholar] [CrossRef]
- Spielberger, C.D. State-Trait anxiety inventory. Corsini Encycl. Psychol. 2010, 1. [Google Scholar] [CrossRef]
- Derogatis, L.R.; Savitz, K.L. The SCL-90-R, Brief Symptom Inventory, and Matching Clinical Rating Scales; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 1999. [Google Scholar]
- Shiffman, S.; Stone, A.A.; Hufford, M.R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 2008, 4, 1–32. [Google Scholar] [CrossRef]
- Marteau, T.M.; Bekker, H. The development of a six-item short-form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI). Br. J. Clin. Psychol. 1992, 31, 301–306. [Google Scholar] [CrossRef]
- La Greca, A.M.; Dandes, S.K.; Wick, P.; Shaw, K.; Stone, W.L. Development of the Social Anxiety Scale for Children: Reliability and concurrent validity. J. Clin. Child Psychol. 1988, 17, 84–91. [Google Scholar] [CrossRef]
- Kroenke, K.; Strine, T.W.; Spitzer, R.L.; Williams, J.B.; Berry, J.T.; Mokdad, A.H. The PHQ-8 as a measure of current depression in the general population. J. Affect. Disord. 2009, 114, 163–173. [Google Scholar] [CrossRef]
- Qiao, C.H.; Wang, L.Z.; Lin, J.R.; Yao, X.T.; Chen, G.; Yao, Y. A Survey Analysis of Psychological Impact on Chinese during Quarantine against COVID-19. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-24664/v1 (accessed on 1 September 2021).
- Fitzpatrick, K.M.; Harris, C.; Drawve, G. Fear of COVID-19 and the mental health consequences in America. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S17. [Google Scholar] [CrossRef]
- Gu, Y.; Guo, J.; Liao, L.; Wang, B.; Li, X.; Guo, L.; Tong, Z.; Guan, Q.; Zhou, M.; Wu, Y.; et al. Psychological effects of COVID-19 on hospital staff: A national cross-sectional survey in mainland China. Vasc. Investig. Ther. 2021, 4, 6. [Google Scholar] [CrossRef]
- Katz, B.; Cognition, P. Mood Symptoms Predict COVID-19 Pandemic Distress but not Vice Versa: An 18-Month Longitudinal Study. 2020, Psyraxiv. Available online: https://psyarxiv.com/6qske/ (accessed on 1 September 2021).
- Khan, A.H.; Sultana, M.S.; Hossain, S.; Hasan, M.T.; Ahmed, H.U.; Sikder, M.T. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study. J. Affect. Disord. 2020, 277, 121–128. [Google Scholar] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Laiyou, L.; Shuangqin, C.; Shuang, Y.; Xiufen, L. Status of and Factors Influencing the Anxiety and Depression of Front-Line Medical Staff Supporting Wuhan in Containing COVID-19. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-19665/v1 (accessed on 1 September 2021).
- Nicomedes, C.; Avila, R. An analysis on the panic of Filipinos during COVID-19 pandemic in the Philippines. J. Affect Disord. 2020, 276, 14–22. [Google Scholar] [CrossRef]
- Ying, Y.; Ruan, L.; Kong, F.; Zhu, B.; Ji, Y.; Lou, Z. Mental health status among family members of health care workers in Ningbo, China, during the coronavirus disease 2019 (COVID-19) outbreak: A cross-sectional study. BMC Psychiatry 2020, 20, 379. [Google Scholar] [CrossRef]
- Zhu, Z.; Xu, S.; Wang, H.; Liu, Z.; Wu, J.; Li, G.; Miao, J.; Zhang, C.; Yang, Y.; Sun, W.; et al. COVID-19 in Wuhan: Immediate psychological impact on 5062 health workers. medRxiv 2020. [Google Scholar] [CrossRef]
- Odriozola-González, P.; Planchuelo-Gómez, Á.; Irurtia, M.J.; de Luis-García, R. Psychological symptoms of the outbreak of the COVID-19 confinement in Spain. J. Health Psychol. 2020, 27, 825–835. [Google Scholar] [CrossRef]
- Hassannia, L.; Taghizadeh, F.; Moosazadeh, M.; Zarghami, M.; Taghizadeh, H.; Dooki, A.F.; Fathi, M.; Navaei, R.A.; Hedayatizadeh-Omran, A. Anxiety and depression in health workers and general population during COVID-19 epidemic in Iran: A web-based cross-sectional study. medRxiv 2020. [Google Scholar] [CrossRef]
- Mai, M.; Wang, J.; Xia, D.; Guo, X.; Li, F.; Chen, Y.; Gong, X.; Li, Z.; Zhang, H. Survey of Anxiety and Depression in Patients with Suspected and Confirmed Cases of COVID-19 During Hospitalization and Isolation. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-17959/v1 (accessed on 1 September 2021).
- Hu, W.; Su, L.; Qiao, J.; Zhu, J.; Zhou, Y. Countrywide quarantine only mildly increased anxiety level during COVID-19 outbreak in China. medRxiv 2020. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef]
- Traunmüller, C.; Stefitz, R.; Gaisbachgrabner, K.; Schwerdtfeger, A. Psychological correlates of COVID-19 pandemic in the Austrian population. BMC Public Health 2020, 20, 1395. [Google Scholar] [CrossRef] [PubMed]
- Rosen, Z.; Weinberger-Litman, S.L.; Rosenzweig, C.; Rosmarin, D.H.; Muennig, P.; Carmody, E.R.; Rao, S.T.; Litman, L. Anxiety and Distress among the First Community Quarantined in the US Due to COVID-19: Psychological Implications for the Unfolding Crisis. 2020, Psyraxiv. Available online: https://psyarxiv.com/7eq8c/ (accessed on 1 September 2021).
- Hania, A.; Hongbo, L. Psychological Predictors of Anxiety in Response to the COVID-19 Pandemic: Evidence from Pakistan. 2020, Psyraxiv. Available online: https://psyarxiv.com/gk6mt/ (accessed on 1 September 2021).
- Skalski, S.; Uram, P.; Dobrakowski, P.; Kwiatkowska, A. Thinking too much about the novel coronavirus. The link between persistent thinking about COVID-19, SARS-CoV-2 anxiety and trauma effects. Curr. Issues Personal. Psychol. 2020, 8, 169–174. [Google Scholar] [CrossRef]
- Tabri, N.; Hollingshead, S.; Wohl, M. Framing COVID-19 as an Existential Threat Predicts Anxious Arousal and Prejudice towards Chinese People. 2020, Psyarxiv. Available online: https://psyarxiv.com/mpbtr/ (accessed on 1 September 2021).
- Agberotimi, S.F.; Akinsola, O.S.; Oguntayo, R.; Olaseni, A.O. Interactions between socioeconomic status and mental health outcomes in the nigerian context amid COVID-19 pandemic: A comparative study. Front. Psychol. 2020, 11, 2655. [Google Scholar] [CrossRef] [PubMed]
- Amin, F.; Sharif, S.; Saeed, R.; Durrani, N.; Jilani, D. COVID-19 pandemic-knowledge, perception, anxiety and depression among frontline doctors of Pakistan. BMC Psychiatry 2020, 20, 459. [Google Scholar] [CrossRef] [PubMed]
- Evanoff, B.A.; Strickland, J.R.; Dale, A.M.; Hayibor, L.; Page, E.; Duncan, J.G.; Kannampallil, T.; Gray, D.L. Work-related and personal factors associated with mental well-being during the COVID-19 response: Survey of health care and other workers. J. Med. Internet Res. 2020, 22, e21366. [Google Scholar] [CrossRef]
- Saddik, B.; Hussein, A.; Sharif-Askari, F.S.; Kheder, W.; Temsah, M.H.; Koutaich, R.A.; Haddad, E.S.; Al-Roub, N.M.; Marhoon, F.A.; Hamid, Q.; et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. Risk Manag. Healthc. Policy 2020, 13, 2395. [Google Scholar] [CrossRef]
- Yang, S.; Kwak, S.G.; Ko, E.J.; Chang, M.C. The mental health burden of the covid-19 pandemic on physical therapists. Int. J. Environ. Res. Public Health 2020, 17, 3723. [Google Scholar] [CrossRef]
- Capuano, R.; Altieri, M.; Bisecco, A.; d’Ambrosio, A.; Docimo, R.; Buonanno, D.; Matrone, F.; Giuliano, F.; Tedeschi, G.; Santangelo, G.; et al. Psychological consequences of COVID-19 pandemic in Italian MS patients: Signs of resilience? J. Neurol. 2021, 268, 743–750. [Google Scholar] [CrossRef]
- Trzebiński, J.; Cabański, M.; Czarnecka, J.Z. Reaction to the COVID-19 pandemic: The influence of meaning in life, life satisfaction, and assumptions on world orderliness and positivity. J. Loss Trauma 2020, 25, 544–557. [Google Scholar] [CrossRef]
- Jin, Z.; Zhao, K.; Xia, Y.; Chen, R.; Yu, H.; Tamutana, T.T.; Sherman, J.; Bermeitinger, C.; Baess, P. Psychological responses to the Coronavirus Disease (COVID-19) outbreak. China 2020, 14, 1. [Google Scholar]
- Chen, J.; Zhang, S.X.; Wang, Y.; Jahanshahi, A.A.; Dinani, M.M.; Madavani, A.N.; Nawaser, K. The curvilinear relationship between the age of adults and their mental health in Iran after its peak of COVID-19 cases. medRxiv 2020. [Google Scholar] [CrossRef]
- Mack, D.L.; DaSilva, A.W.; Rogers, C.; Hedlund, E.; Murphy, E.I.; Vojdanovski, V.; Plomp, J.; Wang, W.; Nepal, S.K.; Holtzheimer, P.E.; et al. Mental Health and Behavior of College Students During the COVID-19 Pandemic: Longitudinal Mobile Smartphone and Ecological Momentary Assessment Study, Part II. J. Med. Internet Res. 2021, 23, e28892. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Priego, B.A.; Triana-Romero, A.; Pinto-Galvez, S.M.; Duran-Ramos, C.; Salas-Nolasco, O.; Reyes, M.M.; de la Medina, A.R.; Troche, J.M.R. Anxiety, depression, attitudes, and internet addiction during the initial phase of the 2019 coronavirus disease (COVID-19) epidemic: A cross-sectional study in México. medRxiv 2020. [Google Scholar] [CrossRef]
- Gupta, P.; Rai, P.; Dang, K. Acute stress disorder, generalized anxiety disorderand major depressive disorder during COVID-19 epidemic in India: Online questionnaire-based cross-sectional survey. J. Dent. Med. Sci. 2020, 19, 50–59. [Google Scholar]
- Jia, R.; Ayling, K.; Chalder, T.; Massey, A.; Broadbent, E.; Coupland, C.; Vedhara, K. Mental health in the UK during the COVID-19 pandemic: Cross-sectional analyses from a community cohort study. BMJ Open 2020, 10, e040620. [Google Scholar] [CrossRef]
- Kaveh, M.; Davari-tanha, F.; Varaei, S.; Shirali, E.; Shokouhi, N.; Nazemi, P.; Ghajarzadeh, M.; Feizabad, E.; Ashraf, M.A. Anxiety levels among Iranian health care workers during the COVID-19 surge: A cross-sectional study. medRxiv 2020. [Google Scholar] [CrossRef]
- Silva Moreira, P.; Ferreira, S.; Couto, B.; Machado-Sousa, M.; Fernández, M.; Raposo-Lima, C.; Sousa, N.; Picó-Pérez, M.; Morgado, P. Protective elements of mental health status during the COVID-19 outbreak in the Portuguese population. Int. J. Environ. Res. Public Health 2021, 18, 1910. [Google Scholar] [CrossRef]
- Pan, X.; Xiao, Y.; Ren, D.; Xu, Z.M.; Zhang, Q.; Yang, L.Y.; Liu, F.; Hao, Y.S.; Zhao, F.; Bai, Y.H. Prevalence of mental health problems and associated risk factors among military healthcare workers in specialized COVID-19 hospitals in Wuhan, China: A cross-sectional survey. Asia-Pac. Psychiatry 2020, 14, e12427. [Google Scholar] [CrossRef]
- Saikarthik, J.; Saraswathi, I.; Siva, T. Assessment of impact of COVID-19 outbreak & lockdown on mental health status & its associated risk and protective factors in adult Indian population. 2020, medRxiv. Available online: https://www.medrxiv.org/content/10.1101/2020.06.13.20130153v1 (accessed on 1 September 2021).
- Shevlin, M.; McBride, O.; Murphy, J.; Miller, J.G.; Hartman, T.K.; Levita, L.; Mason, L.; Martinez, A.P.; McKay, R.; Stocks, T.V.; et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open 2020, 6, e125. [Google Scholar] [CrossRef]
- Uzun, N.D.; Tekin, M.; Sertel, E.; Tuncar, A. Psychological and social effects of COVID-19 pandemic on obstetrics and gynecology employees. J. Surg. Med. 2020, 4, 355–358. [Google Scholar] [CrossRef]
- Wang, Y.; Di, Y.; Ye, J.; Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2021, 26, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; An, Y.; Tan, X.; Li, X. Mental health and its influencing factors among self-isolating ordinary citizens during the beginning epidemic of COVID-19. J. Loss Trauma 2020, 25, 580–593. [Google Scholar] [CrossRef]
- Filgueiras, A.; Hora, G.; Fioravanti-Bastos, A.C.M.; Santana, C.M.; Pires, P.; de Oliveira Galvão, B.; Landeira-Fernandez, J. Development and psychometric properties of a novel depression measure. Temas Em Psicol. 2014, 22, 249–269. [Google Scholar] [CrossRef]
- Zheng, Y.; Li, J.; Zhang, M.; Jin, B.; Li, X.; Cao, Z.; Wu, N.; Jin, C. A survey of the psychological status of primary school students who were quarantined at home during the coronavirus disease 2019 epidemic in Hangzhou China. medRxiv 2020. [Google Scholar] [CrossRef]
- Wang, B.; Sun, J.; Gao, F.; Chen, J.; Shi, L.; Li, L.; Tang, Y.; Wang, K.; Lu, H. A Study on Mental Health Status among the Staff in a Designated Hospital for COVID-19. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-23224/v1 (accessed on 1 September 2021).
- Alonzi, S.; La Torre, A.; Silverstein, M.W. The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S236. [Google Scholar] [CrossRef]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Wang, C.; Zhao, H. The impact of COVID-19 on anxiety in Chinese university students. Front. Psychol. 2020, 11, 1168. [Google Scholar] [CrossRef]
- Filgueiras, A.; Stults-Kolehmainen, M. The relationship between behavioural and psychosocial factors among brazilians in quarantine due to COVID-19. SSRN 2020. [Google Scholar] [CrossRef]
- Gopal, A.; Sharma, A.J.; Subramanyam, M.A. Dynamics of psychological responses to COVID-19 in India: A longitudinal study. PLoS ONE 2020, 15, e0240650. [Google Scholar] [CrossRef]
- Hosseinzadeh-Shanjani, Z.; Hajimiri, K.; Rostami, B.; Ramazani, S.; Dadashi, M. Stress, anxiety, and depression levels among healthcare staff during the COVID-19 epidemic. Basic Clin. Neurosci. 2020, 11, 163. [Google Scholar] [CrossRef]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for US young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef] [PubMed]
- Seyahi, E.; Poyraz, B.C.; Sut, N.; Akdogan, S.; Hamuryudan, V. The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: A web-based cross-sectional survey. Rheumatol. Int. 2020, 40, 1229–1238. [Google Scholar] [CrossRef] [PubMed]
- Zhpu, P.; Du, N.; OuYang, Y. Investigation on the Mental Health of Healthcare Workers for Aid in Hu Bei Province During the Outbreak of COVID-19 Based on the Network Survey. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-34118/v1 (accessed on 1 September 2021).
- Alyami, H.S.; Naser, A.Y.; Dahmash, E.Z.; Alyami, M.H.; Al, O.T.; Meanazel, A.T.; Al Meanazel, O.T. Depression and anxiety during 2019 coronavirus disease pandemic in Saudi Arabia: A cross-sectional study. 2021, medrxiv. Available online: https://www.medrxiv.org/content/10.1101/2020.05.09.20096677v2 (accessed on 1 September 2021).
- Elmer, T.; Mepham, K.; Stadtfeld, C. Students under Lockdown: Assessing Change in Students’ Social Networks and Mental Health during the COVID-19 Crisis in Switzerland. PLoS ONE 2020, 15, e023633. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Zhuang, J.; Chen, Q.; Tan, X. Psychological Investigation on Pregnant Women during the Outbreak of COVID-19. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-28455/v1 (accessed on 1 September 2021).
- Durankuş, F. Effects of the COVID-19 Pandemic on Anxiety and Depressive Symptoms in School-Age Children. Cerrahpas A Med. J. 2021, 45, 87–94. [Google Scholar] [CrossRef]
- Johnson, S.U.; Ebrahimi, O.V.; Hoffart, A. PTSD symptoms among health workers and public service providers during the COVID-19 outbreak. PLoS ONE 2020, 15, e0241032. [Google Scholar] [CrossRef]
- Islam, M.S.; Sujan, M.S.H.; Tasnim, R.; Sikder, M.T.; Potenza, M.N.; Van Os, J. Psychological responses during the COVID-19 outbreak among university students in Bangladesh. PLoS ONE 2020, 15, e0245083. [Google Scholar] [CrossRef]
- Amerio, A.; Bianchi, D.; Santi, F.; Costantini, L.; Odone, A.; Signorelli, C.; Costanza, A.; Serafini, G.; Amore, M.; Aguglia, A. COVID-19 pandemic impact on mental health: A web-based cross-sectional survey on a sample of Italian general practitioners. Acta Bio Med. Atenei Parm. 2020, 91, 83. [Google Scholar]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef]
- Dai, L.L.; Wang, X.; Jiang, T.C.; Li, P.F.; Wang, Y.; Wu, S.J.; Jia, L.Q.; Liu, M.; An, L.; Cheng, Z. Anxiety and Depression Symptoms of Patients in Fangcang Shelter Hospital During the COVID-19 Outbreak in China: A Web-Based Cross-Sectional Study. PLoS ONE 2020. [Google Scholar] [CrossRef]
- Lin, L.Y.; Wang, J.; Ou-Yang, X.Y.; Miao, Q.; Chen, R.; Liang, F.X.; Zhang, Y.P.; Tang, Q.; Wang, T. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2021, 77, 348–354. [Google Scholar] [CrossRef]
- McEwen, B.S. Neurobiological and systemic effects of chronic stress. Chronic Stress 2017, 1, 2470547017692328. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Zhang, Y.; Wang, P.; Zhang, L.; Wang, G.; Lei, G.; Xiao, Q.; Cao, X.; Bian, Y.; Xie, S.; et al. Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. J. Med. Virol. 2020, 92, 1962–1970. [Google Scholar] [CrossRef] [PubMed]
- Nitschke, J.P.; Forbes, P.A.; Ali, N.; Cutler, J.; Apps, M.A.; Lockwood, P.L.; Lamm, C. Resilience during uncertainty? Greater social connectedness during COVID-19 lockdown is associated with reduced distress and fatigue. Br. J. Health Psychol. 2021, 26, 553–569. [Google Scholar] [CrossRef]
- Wissmath, B.; Mast, F.W.; Kraus, F.; Weibel, D. Understanding the psychological impact of the COVID-19 pandemic and containment measures: An empirical model of stress. PLoS ONE 2021, 16, e0254883. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Lu, X.; Cao, Y.; Li, Y.; Li, C.; Zhang, W. Concerns about disease management and psychological stress in SAPHO patients during the COVID-19 epidemic. medRxiv 2020. [Google Scholar] [CrossRef]
- Ramaci, T.; Barattucci, M.; Ledda, C.; Rapisarda, V. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustainability 2020, 12, 3834. [Google Scholar] [CrossRef]
- Forte, G.; Favieri, F.; Tambelli, R.; Casagrande, M. COVID-19 pandemic in the Italian population: Validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int. J. Environ. Res. Public Health 2020, 17, 4151. [Google Scholar] [CrossRef]
- Liu, N.; Zhang, F.; Wei, C.; Jia, Y.; Shang, Z.; Sun, L.; Wu, L.; Sun, Z.; Zhou, Y.; Wang, Y.; et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020, 287, 112921. [Google Scholar] [CrossRef]
- Sun, L.; Sun, Z.; Wu, L.; Zhu, Z.; Zhang, F.; Shang, Z.; Jia, Y.; Gu, J.; Zhou, Y.; Wang, Y.; et al. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. medRxiv 2020. [Google Scholar] [CrossRef]
- Zhang, F.; Shang, Z.; Ma, H.; Jia, Y.; Sun, L.; Guo, X.; Wu, L.; Sun, Z.; Zhou, Y.; Wang, Y.; et al. High risk of infection caused posttraumatic stress symptoms in individuals with poor sleep quality: A study on influence of coronavirus disease (COVID-19) in China. medRxiv 2020. [Google Scholar] [CrossRef]
- Jalili, M.; Niroomand, M.; Hadavand, F.; Zeinali, K.; Fotouhi, A. Burnout among healthcare professionals during COVID-19 pandemic: A cross-sectional study. Int. Arch. Occup. Environ. Health 2021, 94, 1345–1352. [Google Scholar] [CrossRef] [PubMed]
- Morgantini, L.A.; Naha, U.; Wang, H.; Francavilla, S.; Acar, Ö.; Flores, J.M.; Crivellaro, S.; Moreira, D.; Abern, M.; Eklund, M.; et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLoS ONE 2020, 15, e0238217. [Google Scholar] [CrossRef] [PubMed]
- Košir, K.; Dugonik, Š.; Huskić, A.; Gračner, J.; Kokol, Z.; Krajnc, Ž. Predictors of perceived teachers’ and school counsellors’ work stress in the transition period of online education in schools during the COVID-19 pandemic. Educ. Stud. 2020, 1–5. [Google Scholar] [CrossRef]
- Fawaz, M.; Samaha, A. COVID-19 quarantine: Post-traumatic stress symptomatology among Lebanese citizens. Int. J. Soc. Psychiatry 2020, 66, 666–674. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Liao, Z.; Huang, H.; Jiang, B.; Zhang, X.; Wang, Y.; Zhao, M. Comparison of the indicators of psychological stress in the population of Hubei province and non-endemic provinces in China during two weeks during the coronavirus disease 2019 (COVID-19) outbreak in February 2020. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020, 26, e923767-1. [Google Scholar] [CrossRef]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. Perceived stress scale. Meas. Stress: A Guide Health Soc. Sci. 1994, 10, 1–2. [Google Scholar]
- Beck, J.G.; Grant, D.M.; Read, J.P.; Clapp, J.D.; Coffey, S.F.; Miller, L.M.; Palyo, S.A. The impact of event scale-revised: Psychometric properties in a sample of motor vehicle accident survivors. J. Anxiety Disord. 2008, 22, 187–198. [Google Scholar] [CrossRef]
- Joseph, S.; Linley, P.A.; Andrews, L.; Harris, G.; Howle, B.; Woodward, C.; Shevlin, M. Assessing positive and negative changes in the aftermath of adversity: Psychometric evaluation of the changes in outlook questionnaire. Psychol. Assess. 2005, 17, 70. [Google Scholar] [CrossRef]
- Olff, M.; Bakker, A.; Frewen, P.; Aakvaag, H.; Ajdukovic, D.; Brewer, D.; Elmore Borbon, D.L.; Cloitre, M.; Hyland, P.; Kassam-Adams, N.; et al. Screening for consequences of trauma–an update on the global collaboration on traumatic stress. Eur. J. Psychotraumatology 2020, 11, 1752504. [Google Scholar] [CrossRef]
- Bryant, R.A.; Moulds, M.L.; Guthrie, R.M. Acute Stress Disorder Scale: A self-report measure of acute stress disorder. Psychol. Assess. 2000, 12, 61. [Google Scholar] [CrossRef] [PubMed]
- Brunet, A.; Weiss, D.S.; Metzler, T.J.; Best, S.R.; Neylan, T.C.; Rogers, C.; Fagan, J.; Marmar, C.R. The Peritraumatic Distress Inventory: A proposed measure of PTSD criterion A2. Am. J. Psychiatry 2001, 158, 1480–1485. [Google Scholar] [CrossRef] [PubMed]
- Cardeña, E.; Koopman, C.; Classen, C.; Waelde, L.C.; Spiegel, D. Psychometric properties of the Stanford Acute Stress Reaction Questionnaire (SASRQ): A valid and reliable measure of acute stress. J. Trauma. Stress 2000, 13, 719–734. [Google Scholar] [CrossRef] [PubMed]
- Evren, C.; Dalbudak, E.; Umut, G.; Bozkurt, M.; Evren, B.; Agachanli, R.; Teksin-Unal, G. Psychometric properties of the Turkish version of the National Stressful Events Survey for PTSD-Short Scale in a sample of inpatients with Alcohol Use Disorder. Heroin Addict. Relat. Clin. Probl. 2016, 18, 19–26. [Google Scholar]
- Palestini, L.; Prati, G.; Pietrantoni, L.; Cicognani, E. La qualità della vita professionale nel lavoro di soccorso: Un contributo alla validazione italiana della Professional Quality of Life Scale (ProQOL). Psicoter. Cogn. E Comport. 2009, 15, 205–227. [Google Scholar]
- Prasad, K.; Vaidya, R.; Kumar, V.A. Teacher’s Performance as a Function of Occupational Stress and Coping with Reference to CBSE Affiliated School Teachers in and around Hyderabad: A Multinomial Regression Approach. Psychology 2016, 7, 1700–1718. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. MBI: Maslach Burnout Inventory; CPP Incorporated: Sunnyvale, CA, USA, 1996. [Google Scholar]
- Warttig, S.L.; Forshaw, M.J.; South, J.; White, A.K. New, normative, English-sample data for the short form perceived stress scale (PSS-4). J. Health Psychol. 2013, 18, 1617–1628. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.T.; Herman, D.S.; Huska, J.A.; Keane, T.M. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. In Proceedings of the Annual Convention of the International Society for Traumatic Stress Studies, San Antonio, TX, USA, 25 October 1993; Volume 462. [Google Scholar]
- Lu, W.; Bian, Q.; Wang, W.; Wu, X.; Wang, Z.; Zhao, M. Chinese version of the Perceived Stress Scale-10: A psychometric study in Chinese university students. PLoS ONE 2017, 12, e0189543. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef]
- Thoresen, S.; Tambs, K.; Hussain, A.; Heir, T.; Johansen, V.A.; Bisson, J.I. Brief measure of posttraumatic stress reactions: Impact of Event Scale-6. Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 405–412. [Google Scholar] [CrossRef]
- Umucu, E.; Iwanaga, K.; Wu, J.R.; Brooks, J.M.; Ditchman, N.; Flowers-Benton, S.; Chan, F. Preliminary validation of a short form of the Perceived Stress Questionnaire for use in clinical rehabilitation counseling research and practice. Rehabil. Res. Policy Educ. 2018, 32, 232–243. [Google Scholar] [CrossRef]
- Plomecka, M.B.; Gobbi, S.; Neckels, R.; Radziński, P.; Skórko, B.; Lazerri, S.; Almazidou, K.; Dedić, A.; Bakalović, A.; Hrustić, L.; et al. Mental Health Impact of COVID-19: A global study of risk and resilience factors. medRxiv 2020. [Google Scholar] [CrossRef]
- Samadarshi, S.C.A.; Sharma, S.; Bhatta, J. An online survey of factors associated with self-perceived stress during the initial stage of the COVID-19 outbreak in Nepal. Ethiop. J. Health Dev. 2020, 34, 2. [Google Scholar]
- Chaix, B.; Delamon, G.; Guillemassé, A.; Brouard, B.; Bibault, J.E. Psychological distress during the COVID-19 pandemic in France: A national assessment of at-risk populations. Gen. Psychiatry 2020, 33, e100349. [Google Scholar] [CrossRef]
- Newby, J.M.; O’Moore, K.; Tang, S.; Christensen, H.; Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE 2020, 15, e0236562. [Google Scholar] [CrossRef]
- Huang, L.; Wang, Y.; Liu, J.; Ye, P.; Cheng, B.; Xu, H.; Qu, H.; Ning, G. Factors associated with resilience among medical staff in radiology departments during the outbreak of 2019 novel coronavirus disease (COVID-19): A cross-sectional study. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020, 26, e925669-1. [Google Scholar] [CrossRef]
- Arslan, G.; Yıldırım, M.; Tanhan, A.; Buluş, M.; Allen, K.A. Coronavirus stress, optimism-pessimism, psychological inflexibility, and psychological health: Psychometric properties of the Coronavirus Stress Measure. Int. J. Ment. Health Addict. 2021, 19, 2423–2439. [Google Scholar] [CrossRef]
- Arslan, G.; Yıldırım, M. Coronavirus stress, meaningful living, optimism, and depressive symptoms: A study of moderated mediation model. Aust. J. Psychol. 2021, 73, 113–124. [Google Scholar] [CrossRef]
- Yin, Q.; Sun, Z.; Liu, T.; Ni, X.; Deng, X.; Jia, Y.; Shang, Z.; Zhou, Y.; Liu, W. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin. Psychol. Psychother. 2020, 27, 384–395. [Google Scholar] [CrossRef]
- Romero, C.S.; Delgado, C.; Catalá, J.; Ferrer, C.; Errando, C.; Iftimi, A.; Benito, A.; De Andres, J.; Otero, M. COVID-19 psychological impact in 3109 healthcare workers in Spain: The PSIMCOV group. Psychol. Med. 2020, 52, 188–194. [Google Scholar] [CrossRef]
- Barello, S.; Palamenghi, L.; Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020, 290, 113129. [Google Scholar] [CrossRef] [PubMed]
- Kowal, M.; Coll-Martín, T.; Ikizer, G.; Rasmussen, J.; Eichel, K.; Studzinska, A.; Koszałkowska, K.; Karwowski, M.; Najmussaqib, A.; Pankowski, D.; et al. Who Is the Most Stressed during COVID-19 Isolation? Data from 27 Countries. 2020, Psyarxiv. Available online: https://psyarxiv.com/qv5t7/ (accessed on 1 September 2021).
- López, J.; Perez-Rojo, G.; Noriega, C.; Carretero, I.; Velasco, C.; Martinez-Huertas, J.; López-Frutos, P.; Galarraga, L. Psychological well-being among older adults during the COVID-19 outbreak: A comparative study of the young–old and the old–old adults. Int. Psychogeriatr. 2020, 32, 1365–1370. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.K.R.; Chellaswamy, K.S.; Kattula, D.; Thavarajah, R.; Mohandoss, A.A. Perceived stress and psychological (dis) stress among Indian endodontists during COVID19 pandemic lock down. medRxiv 2020. [Google Scholar] [CrossRef]
- Varshney, M.; Parel, J.T.; Raizada, N.; Sarin, S.K. Initial psychological impact of COVID-19 and its correlates in Indian Community: An online (FEEL-COVID) survey. PLoS ONE 2020, 15, e0233874. [Google Scholar] [CrossRef]
- Sinha, D.; Manna, P. The effect of Lockdown due to COVID-19 on Post-traumatic Stress and Depression among College Students of Kolkata, hotspot district of West Bengal, India. J. Humanit. Soc. Sci. 2020, 25, 58–64. [Google Scholar]
- Song, K.; Xu, R.; Stratton, T.D.; Kavcic, V.; Luo, D.; Hou, F.; Bi, F.; Jiao, R.; Yan, S.; Jiang, Y. Sex Differences and Psychological Stress: Responses to the COVID-19 epidemic in China. 2020, medrxiv. Available online: https://www.medrxiv.org/content/10.1101/2020.04.29.20084061v3 (accessed on 21 September 2021).
- Zhi, X.; Lu, L.; Pu, Y.; Meng, A.; Zhao, Y.; Cheng, F.; Jiang, J.; Xu, J.L.; Zeng, Y. Investigation and Analysis of Psychological Stress and Professional Identity of Nursing Students during COVID-19 Pandemic. Indian J. Exp. Biol. 2020, 58, 426–432. [Google Scholar]
- Xia, X.; Wu, X.; Zhou, X.; Zang, Z.; Pu, L.; Li, Z. Comparison of psychological distress and demand induced by COVID-19 during the lockdown period in patients undergoing peritoneal dialysis and hemodialysis: A cross-section study in a tertiary hospital. Blood Purif. 2021, 50, 315–323. [Google Scholar] [CrossRef]
- Cui, R. A systematic review of depression. Curr. Neuropharmacol. 2015, 13, 480. [Google Scholar] [CrossRef]
- Gobbi, S.; Płomecka, M.B.; Ashraf, Z.; Radziński, P.; Neckels, R.; Lazzeri, S.; Dedić, A.; Bakalović, A.; Hrustić, L.; Skórko, B.; et al. Worsening of preexisting psychiatric conditions during the COVID-19 pandemic. Front. Psychiatry 2020, 11, 1407. [Google Scholar] [CrossRef]
- Soraci, P.; Ferrari, A.; Abbiati, F.A.; Del Fante, E.; De Pace, R.; Urso, A.; Griffiths, M.D. Validation and psychometric evaluation of the Italian version of the Fear of COVID-19 Scale. Int. J. Ment. Health Addict. 2020, 4, 1–10. [Google Scholar] [CrossRef]
- Amakiri, P.C.; Chude, C.F.; Oradiegwu, S.; Primanik, I.; Anoka, K.C.; Ezeoke, Q. Psychological effect of pandemic COVID-19 on families of health care professionals. Br. J. Psychol. Res. 2020, 8, 1–7. [Google Scholar]
- Sun, R.; Balabanova, A.; Bajada, C.J.; Liu, Y.; Kriuchok, M.; Voolma, S.R.; Đurić, M.; Mayer, C.H.; Constantinou, M.; Chichua, M.; et al. Psychological Wellbeing during the Global COVID-19 Outbreak. 2020. Available online: https://www.researchgate.net/publication/341838488_Psychological_wellbeing_during_the_global_COVID-19_outbreak (accessed on 1 September 2021).
- Snaith, R.; Zigmond, A. The hospital anxiety and depression scale. Br. Med. J. 1986, 292, 344. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A. Beck Depression Inventory (BDI-II); Pearson: London, UK, 1996; Volume 10. [Google Scholar]
- Zung, W.W. A self-rating depression scale. Arch. Gen. Psychiatry 1965, 12, 63–70. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med. Care 2003, 2003, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
- Birleson, P. The validity of depressive disorder in childhood and the development of a self-rating scale: A research report. J. Child Psychol. Psychiatry 1981, 22, 73–88. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.; Williams, J. The Patient Health Questionnaire (PHQ-9)–overview. J. Gen. Intern. Med 2001, 16, 606–616. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. An ultra-brief screening scale for anxiety and depression: The PHQ–4. Psychosomatics 2009, 50, 613–621. [Google Scholar]
- Trapnell, P.D.; Campbell, J.D. Private self-consciousness and the five-factor model of personality: Distinguishing rumination from reflection. J. Personal. Soc. Psychol. 1999, 76, 284. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Hillier, V. A scaled version of the General Health Questionnaire. Psychol. Med. 1979, 9, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Derogatis, L.R.; Savitz, K.L. The SCL-90-R and Brief Symptom Inventory (BSI) in Primary Care; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2000. [Google Scholar]
- Netsereab, T.B.; Kifle, M.M.; Tesfagiorgis, R.B.; Habteab, S.G.; Weldeabzgi, Y.K.; Tesfamariam, O.Z. Validation of the WHO self-reporting questionnaire-20 (SRQ-20) item in primary health care settings in Eritrea. Int. J. Ment. Health Syst. 2018, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Soykan, Ç. Institutional Differences and Case Typicality as Diagnosis System Severity, Prognosis and Treatment. Master’s Thesis, Orta Doğu Teknik Üniversitesi, Ankara, Turkey, 1990. [Google Scholar]
- Aqeel, M.; Abbas, J.; Shuja, K.H.; Rehna, T.; Ziapour, A.; Yousaf, I.; Karamat, T. The influence of illness perception, anxiety and depression disorders on students mental health during COVID-19 outbreak in Pakistan: A web-based cross-sectional survey. Int. J. Hum. Rights Healthc. 2021, 15, 17–30. [Google Scholar] [CrossRef]
- Choi, E.P.H.; Hui, B.P.H.; Wan, E.Y.F. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3740. [Google Scholar] [CrossRef]
- Toledo-Fernández, A.; Betancourt-Ocampo, D.; Romo-Parra, H.; Reyes-Zamorano, E.; Gongález-González, A. A Cross-Sectional Survey of Psychological Distress in a Mexican Sample during the Second Phase of the COVID-19 Pandemic. 2000, OSFPreprints. Available online: https://osf.io/wzqkh (accessed on 1 September 2021).
- Liang, P.; Wang, Y.; Shi, S.; Liu, Y.; Xiong, R. Prevalence and factors associated with postpartum depression during the COVID-19 pandemic among women in Guangzhou, China: A cross-sectional study. BMC Psychiatry 2020, 20, 557. [Google Scholar] [CrossRef]
- Zanardo, V.; Manghina, V.; Giliberti, L.; Vettore, M.; Severino, L.; Straface, G. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int. J. Gynecol. Obstet. 2020, 150, 184–188. [Google Scholar] [CrossRef]
- Ahmed, M.Z.; Ahmed, O.; Aibao, Z.; Hanbin, S.; Siyu, L.; Ahmad, A. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatry 2020, 51, 102092. [Google Scholar] [CrossRef]
- Sweeny, K.; Rankin, K.; Cheng, X.; Hou, L.; Long, F.; Meng, Y.; Azer, L.; Zhou, R.; Zhang, W. Flow in the time of COVID-19: Findings from China. PLoS ONE 2020, 15, e0242043. [Google Scholar] [CrossRef]
- Lu, H.; Nie, P.; Qian, L. Do quarantine experiences and attitudes towards COVID-19 affect the distribution of mental health in China? A quantile regression analysis. Appl. Res. Qual. Life 2020, 16, 1925–1942. [Google Scholar] [CrossRef]
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Walters, E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Association, A.P. Depression Guideline. 2019. Available online: https://www.apa.org/depression-guideline/guideline.pdf (accessed on 1 September 2021).
- Kimhi, S.; Eshel, Y.; Marciano, H.; Adini, B. Distress and resilience in the days of COVID-19: Comparing two ethnicities. Int. J. Environ. Res. Public Health 2020, 17, 3956. [Google Scholar] [CrossRef] [PubMed]
- Thomaier, L.; Teoh, D.; Jewett, P.; Beckwith, H.; Parsons, H.; Yuan, J.; Blaes, A.H.; Lou, E.; Hui, J.Y.C.; Vogel, R.I. Emotional health concerns of oncology physicians in the United States: Fallout during the COVID-19 pandemic. PLoS ONE 2020, 15, e0242767. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, Y.; Jiang, J.; Valdimarsdóttir, U.A.; Fall, K.; Fang, F.; Song, H.; Lu, D.; Zhang, W. Psychological distress among health professional students during the COVID-19 outbreak. Psychol. Med. 2021, 51, 1952–1954. [Google Scholar] [CrossRef]
- Van Agteren, J.; Bartholomaeus, J.; Fassnacht, D.B.; Iasiello, M.; Ali, K.; Lo, L.; Kyrios, M. Using internet-based psychological measurement to capture the deteriorating community mental health profile during COVID-19: Observational study. JMIR Ment. Health 2020, 7, e20696. [Google Scholar] [CrossRef]
- Aymerich-Franch, L. COVID-19 Lockdown: IMPACT on Psychological Well-Being and Relationship to Habit and Routine Modifications. 2020, Psyarxiv. Available online: https://psyarxiv.com/9vm7r/ (accessed on 1 September 2021).
- Winefield, H.R.; Gill, T.K.; Taylor, A.W.; Pilkington, R.M. Psychological well-being and psychological distress: Is it necessary to measure both? Psychol. Well-Being Theory Res. Pract. 2012, 2, 1–14. [Google Scholar] [CrossRef]
- Association, A.P. Psychological Distress. 2020. Available online: https://dictionary.apa.org/psychological-distress (accessed on 1 September 2021).
- Arvidsdotter, T.; Marklund, B.; Kylén, S.; Taft, C.; Ekman, I. Understanding persons with psychological distress in primary health care. Scand. J. Caring Sci. 2016, 30, 687–694. [Google Scholar] [CrossRef]
- Losada-Baltar, A.; Jiménez-Gonzalo, L.; Gallego-Alberto, L.; Pedroso-Chaparro, M.d.S.; Fernandes-Pires, J.; Márquez-González, M. “We are staying at home.” Association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. J. Gerontol. Ser. B 2021, 76, e10–e16. [Google Scholar] [CrossRef]
- Gómez-Salgado, J.; Andrés-Villas, M.; Domínguez-Salas, S.; Díaz-Milanés, D.; Ruiz-Frutos, C. Related health factors of psychological distress during the COVID-19 pandemic in Spain. Int. J. Environ. Res. Public Health 2020, 17, 3947. [Google Scholar] [CrossRef]
- Zhang, H.; Su, H.; Wang, D.; Wang, L.; Cai, Y.; Zhou, Y. COVID-19: Are you Ready to Seek Psychological Help during Home Quarantine? 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-21747/v1 (accessed on 1 September 2021).
- Kroencke, L.; Geukes, K.; Utesch, T.; Kuper, N.; Back, M. Neuroticism and emotional risk during the COVID-19 pandemic. J. Res. Personal. 2020, 89, 104038. [Google Scholar] [CrossRef]
- Mertens, G.; Gerritsen, L.; Duijndam, S.; Salemink, E.; Engelhard, I.M. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J. Anxiety Disord. 2020, 74, 102258. [Google Scholar] [CrossRef] [PubMed]
- Schimmenti, A.; Billieux, J.; Starcevic, V. The four horsemen of fear: An integrated model of understanding fear experiences during the COVID-19 pandemic. Clin. Neuropsychiatry 2020, 17, 41–45. [Google Scholar] [PubMed]
- Zhuo, K.; Gao, C.; Wang, X.; Zhang, C.; Wang, Z. Stress and sleep: A survey based on wearable sleep trackers among medical and nursing staff in Wuhan during the COVID-19 pandemic. Gen. Psychiatry 2020, 33, e100260. [Google Scholar] [CrossRef]
- Ryff, C.D. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Personal. Soc. Psychol. 1989, 57, 1069. [Google Scholar] [CrossRef]
- Stamm, B.H. The ProQOL Manual: The professional Quality of Life Scale: Compassion Satisfaction, Burnout & Compassion Fatigue/Secondary Trauma Scales; Sidran: Baltimore, MD, USA, 2005. [Google Scholar]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh mental well-being scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Wirtz, D.; Biswas-Diener, R.; Tov, W.; Kim-Prieto, C.; Choi, D.W.; Oishi, S. New measures of well-being. In Assessing Well-Being; Springer: Berlin/Heidelberg, Germany, 2009; pp. 247–266. [Google Scholar]
- Grossi, E.; Compare, A.; Pgwbi, S.F. Psychological General Well-Being Index (PGWB). Encyclopedia of Quality of Life and Well-Being Research; Michalos, A.C., Ed.; Springer: Dordrecht, The Netherlands, 2014; pp. 224–311. [Google Scholar]
- WHO. Introduction, Administration, Scoring and Generic Version of the Assessment, Field Trial Version; World Health Organization: Geneva, Switzerland, 1996. [Google Scholar]
- Moss-Morris, R.; Weinman, J.; Petrie, K.; Horne, R.; Cameron, L.; Buick, D. The revised illness perception questionnaire (IPQ-R). Psychol. Health 2002, 17, 1–16. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Personal. Soc. Psychol. 1988, 54, 1063. [Google Scholar] [CrossRef]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The satisfaction with life scale. J. Personal. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Nielsen, L.; Hinrichsen, C.; Santini, Z.; Koushede, V. The Danish Mental Health and Well-Being Survey 2016; Statens Institut for Folkesundhed: Copenhagen, Denmark, 2017. [Google Scholar]
- Keyes, C.L.; Wissing, M.; Potgieter, J.P.; Temane, M.; Kruger, A.; Van Rooy, S. Evaluation of the mental health continuum–short form (MHC–SF) in setswana-speaking South Africans. Clin. Psychol. Psychother. 2008, 15, 181–192. [Google Scholar] [CrossRef]
- Schmitz, N.; DaviesOsterkamp, S. Clinical and statistical significance using the symptom check list 90 R (SCL-90-R). Diagnostica 1997, 43, 80–96. [Google Scholar]
- Kimhi, S.; Shamai, M. Community resilience and the impact of stress: Adult response to Israel’s withdrawal from Lebanon. J. Community Psychol. 2004, 32, 439–451. [Google Scholar] [CrossRef]
- Butler, J.; Kern, M.L. The PERMA-Profiler: A brief multidimensional measure of flourishing. Int. J. Wellbeing 2016, 6, 1–48. [Google Scholar] [CrossRef]
- Tanner, B.A. Validity of global physical and emotional SUDS. Appl. Psychophysiol. Biofeedback 2012, 37, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- Simons, J.S.; Gaher, R.M. The Distress Tolerance Scale: Development and validation of a self-report measure. Motiv. Emot. 2005, 29, 83–102. [Google Scholar] [CrossRef]
- Goldberg, D.; Williams, P. General Health Questionnaire (GHQ); NferNelson: Swindon, Wiltshire, UK, 2000. [Google Scholar]
- Horowitz, M.; Wilner, N.; Alvarez, W. Impact of Event Scale: A measure of subjective stress. Psychosom. Med. 1979, 41, 209–218. [Google Scholar] [CrossRef]
- Becker, S.; Fuchs, X.; Schakib-Ekbatan, K.; Schweiker, M. What does “moderate pain” mean? Subgroups holding different conceptions of rating scales evaluate experimental pain differently. Eur. J. Pain 2020, 24, 625–638. [Google Scholar] [CrossRef]
- Sasaki, N.; Kuroda, R.; Tsuno, K.; Kawakami, N. Workplace responses to COVID-19 associated with mental health and work performance of employees in Japan. J. Occup. Health 2020, 62, e12134. [Google Scholar] [CrossRef]
- Morin, C.M.; Belleville, G.; Bélanger, L.; Ivers, H. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011, 34, 601–608. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds III, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Li, J. Seff-rating scale of sleep (SRSS). China J. Health Psychol. 2012, 20, 1851. [Google Scholar]
- Cella, D.; Riley, W.; Stone, A.; Rothrock, N.; Reeve, B.; Yount, S.; Amtmann, D.; Bode, R.; Buysse, D.; Choi, S.; et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J. Clin. Epidemiol. 2010, 63, 1179–1194. [Google Scholar] [CrossRef] [PubMed]
- Bai, R.; Wang, Z.; Liang, J.; Qi, J.; He, X. The Effect of the COVID-19 Outbreak on Children’s Behavior and Parents’ mental HEALTH in China: A Research Study. 2020, Researchsquare. Available online: https://www.researchsquare.com/article/rs-22686/v1 (accessed on 1 September 2021).
- Folk, D.; Okabe-Miyamoto, K.; Dunn, E.; Lyubomirsky, S. Have introverts or extraverts declined in social connection during the first wave of COVID-19. Retrieved Sept. 2020, 14, 2020. [Google Scholar]
- Hawari, F.I.; Obeidat, N.A.; Dodin, Y.I.; Albtoosh, A.S.; Manasrah, R.M.; Alaqeel, I.O.; Mansour, A.H. The inevitability of COVID-19 related distress among healthcare workers: Findings from a low caseload country under lockdown. PLoS ONE 2021, 16, e0248741. [Google Scholar] [CrossRef] [PubMed]
- Shacham, M.; Hamama-Raz, Y.; Kolerman, R.; Mijiritsky, O.; Ben-Ezra, M.; Mijiritsky, E. COVID-19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. Int. J. Environ. Res. Public Health 2020, 17, 2900. [Google Scholar] [CrossRef] [PubMed]
- de Abreu, J.M.; de Souza, R.A.; Viana-Meireles, L.G.; Landeira-Fernandez, J.; Filgueiras, A. Effects of physical activity and exercise on well-being in the context of the COVID-19 pandemic. PLoS ONE 2022, 17, e0260465. [Google Scholar] [CrossRef]
- Amin, S. The psychology of coronavirus fear: Are healthcare professionals suffering from corona-phobia? Int. J. Healthc. Manag. 2020, 13, 249–256. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, S.X.; Jahanshahi, A.A.; Alvarez-Risco, A.; Dai, H.; Li, J.; Ibarra, V.G. Belief in Conspiracy Theory about COVID-19 Predicts Mental Health and Well-being—A Study of Healthcare Staff in Ecuador. medRxiv 2020. [Google Scholar] [CrossRef]
- Chen, B.; Wang, Y.; Yang, T.; Li, C.; Xu, C.; Shen, Y.; Qin, Q.; Chen, F.; Xu, B.; Hou, J.; et al. Mental health among COVID-19 survivors and healthcare workers exposed to COVID-19 in Wuhan, China: A cross-sectional study. Authorea Prepr. 2020. [Google Scholar] [CrossRef]
- García-Reyna, B.; Castillo-García, G.D.; Barbosa-Camacho, F.J.; Cervantes-Cardona, G.A.; Cervantes-Pérez, E.; Torres-Mendoza, B.M.; Fuentes-Orozco, C.; Pintor-Belmontes, K.J.; Guzmán-Ramírez, B.G.; Bernal-Hernández, A.; et al. Fear of COVID-19 scale for hospital staff in regional hospitals in Mexico: A brief report. Int. J. Ment. Health Addict. 2020, 1–12. [Google Scholar] [CrossRef]
- Lu, W.; Wang, H.; Lin, Y.; Li, L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020, 288, 112936. [Google Scholar] [CrossRef] [PubMed]
- Di Giorgio, E.; Di Riso, D.; Mioni, G.; Cellini, N. The interplay between mothers’ and children behavioral and psychological factors during COVID-19: An Italian study. Eur. Child Adolesc. Psychiatry 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Collie, A.; Sheehan, L.; van Vreden, C.; Grant, G.; Whiteford, P.; Petrie, D.; Sim, M.R. Psychological distress among people losing work during the COVID-19 pandemic in Australia. medRxiv 2020. [Google Scholar] [CrossRef]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Wang, Y.; Zhu, L.Y.; Ma, Y.F.; Bo, H.X.; Deng, H.B.; Cao, J.; Wang, Y.; Wang, X.J.; Xu, Y.; Lu, Q.D.; et al. Association of insomnia disorder with sociodemographic factors and poor mental health in COVID-19 inpatients in China. Sleep Med. 2020, 75, 282–286. [Google Scholar] [CrossRef]
- Prati, G. Mental health and its psychosocial predictors during national quarantine in Italy against the coronavirus disease 2019 (COVID-19). Anxiety Stress Coping 2021, 34, 145–156. [Google Scholar] [CrossRef]
- Sønderskov, K.M.; Dinesen, P.T.; Santini, Z.I.; Østergaard, S.D. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr. 2020, 32, 226–228. [Google Scholar] [CrossRef]
- Broche-Pérez, Y.; Fernández-Fleites, Z.; Jiménez-Puig, E.; Fernández-Castillo, E.; Rodríguez-Martin, B.C. Gender and fear of COVID-19 in a Cuban population sample. Int. J. Ment. Health Addict. 2020, 20, 83–91. [Google Scholar] [CrossRef]
- Ersoy, K.; Altin, B.; Sarikaya, B.B.; Özkardas, O.G. The comparison of impact of health anxiety on dispositional hope and psychological well-being of mothers who have children diagnosed with autism and mothers who have normal children, in COVID-19 pandemic. Sosyal Bilimler Araştırma Dergisi 2020, 9, 117–126. [Google Scholar]
- Zhang, J.; Lu, H.; Zeng, H.; Zhang, S.; Du, Q.; Jiang, T.; Du, B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020, 87, 49. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).