Abstract
Objective: This study investigated emotional distress and associated factors among the general population in the aftermath of the COVID-19 lockdown in China. Design and sample: An online nationwide survey was conducted using a self-designed questionnaire, which included items related to demography, lifestyle, and experience of emotional distress during the previous month of the pandemic period. A total of 10,545 respondents completed the survey. Results: Over 30% of participants reported experiencing one or more symptoms of emotional distress to a moderate or higher degree. Increased emotional distress was associated with COVID-19-related impact on diet (β = −1.106, 95% CI: −1.187 to −1.026, p < 0.001), experiencing food shortage (β = 1.334, 95% CI: 1.117 to 1.551, p < 0.001), lack of physical exercise (β = −0.845, 95% CI: −1.024 to −0.667, p < 0.001), younger age (β = −0.050, 95% CI: −0.062 to −0.039, p < 0.001), being a smoker (β = 0.852, 95% CI: 0.604 to 1.100, p < 0.001), lower education level (β = −0.524, 95% CI: −0.702 to −0.346, p < 0.001), and lack of medical insurance (β = −0.742, 95% CI: −1.012 to −0.473, p < 0.001). Emotional distress was negatively associated time spent sleeping (β = −0.020, 95% CI: −0.027 to −0.013, p < 0.001). Conclusion: The levels of emotional distress are high in the aftermath of the lockdown and associated with a number of demographic and lifestyle factors.
1. Introduction
Coronavirus disease 2019 (COVID-19) rapidly spread worldwide and became a global pandemic after it was first reported in Wuhan City, Hubei Province, China, in late December 2019 [1,2]. In response to the pandemic, most of the affected countries implemented a lockdown policy, which suspended or restricted public transport, prohibited gatherings, and limited nonessential social interactions, in an attempt to reduce transmission of the virus [3,4]. This unprecedented global lockdown has been referred to as the largest quarantine in human history, and billions of people around the world were restricted to their homes. As a result, there is rising concern that the pandemic has had a significant influence on public mental health.
Previous studies have suggested that similar outbreaks of infectious diseases in recent years, including severe acute respiratory syndrome (SARS), H1N1 influenza, and Middle East respiratory syndrome (MERS), were associated with various mental health problems, such as anxiety, depression, post-traumatic stress symptoms (PTSS), stigmatization, abandonment, and isolation in the general population, which persisted over time [5,6,7]. The current COVID-19 pandemic appears to have had a similar impact on the mental health of the general population [8]. To better understand its impact, an increasing number of studies have been conducted to explore the prevalence of mental health concerns among the general population and identify its influencing factors. For instance, two cross-sectional studies during the COVID-19 outbreak in China showed high levels of psychological distress [9] and a sharp increase in the prevalence of anxiety and depression among the general population [10]. Another cross-sectional study during the initial stage of COVID-19 in Spain also revealed a high prevalence of depression, anxiety, and post-traumatic stress disorder (PTSD) among the general population and various specific groups [11].
Increased psychological distress was associated with the COVID-19 pandemic and lockdown measures [12]. An investigation in Belgium showed that half of the participants displayed psychological distress in the early stage of the COVID-19 lockdown, with women and young people displaying the highest levels of psychological distress [13]. A longitudinal study in Italy showed that individuals exhibited higher levels of anxiety throughout most of the lockdown period [14]. Several factors, such as socioeconomic and gender disparities, were found to be associated with psychological distress during the COVID-19 pandemic [15]. In a large national survey during the lockdown in China (January to March 2020), 35% of respondents were found to be suffering from emotional distress [16]. A key question is whether the levels of distress in Chinese people would be sustained in the aftermath of the immediate emergency and lockdown situation, and what factors might contribute to sustained levels of distress.
In addition, a growing body of evidence has documented the impact of the COVID-19 on sleep [17]. A systematic review estimated that the prevalence of sleep problems during the COVID-19 pandemic was high and affected approximately 40% of people from general and health care populations [18]. A longitudinal study observed longer sleep latency, worse sleep efficiency, and massive sleep medication use, but an increased sleep duration and better daytime functioning, in Italian participants during the COVID-19 lockdown [19,20]. Moreover, the increase in sleep difficulties was associated with higher levels of depression, anxiety, and stress among Italian adults during the lockdown [21].
To fully understand the psychological effects of the current pandemic, it is critical to conduct surveys of emotional distress at the population level at various time points. In the present study, we aimed to conduct an online nationwide survey on the emotional distress and the associated factors among the general population in the aftermath of the lockdown due to the COVID-19 outbreak in China. We mainly hypothesized that a large proportion of the general population in China experienced emotional distress in the aftermath of the COVID-19 lockdown, and that was influenced by a variety of factors.
2. Materials and Methods
2.1. Study Design and Participants
An anonymous online survey was carried out nationally in mainland China from 25 April to 11 May 2020. Potential participants were recruited by sending the survey through WeChat, the most popular social media outlet in China. The final sample was obtained through both snowball and convenience sampling methods and included members of the general population living in mainland China during the COVID-19 outbreak. Researchers first disseminated the survey to their WeChat friends, and respondents were encouraged to invite new respondents from their contacts. The survey was anonymous and did not collect any personal information, such as names, to obtain honest responses. Each part of the questionnaire had a minimum time requirement to ensure that participants answered the questions carefully. The questionnaire could be submitted only after all the questions had been answered. This study was approved by the Ethical Committee of the Health Science Center, Xi’an Jiaotong University in July 2020 (Number: 2020-1172).
2.2. Measures
This study used a self-designed questionnaire consisting of the following parts: (1) general demographic characteristics, including gender, age, ethnicity, education, marital status, medical insurance, residence, and employment status; (2) lifestyle variables, including smoking and drinking, diet, and physical exercise; and (3) emotional distress and daily sleep duration. The primary outcome was emotional distress assessed by a 5-item scale measuring participants’ “stressful experiences” during the previous month of the pandemic period. It was adapted from the widely used and validated DSM-IV-based civilian version of the posttraumatic stress disorder checklist (PCL-C) [22]. The scale includes questions about how much participants experienced and were bothered by (1) losing interest in previously enjoyed activities; (2) repeated disturbing dreams related to COVID-19; (3) difficulty falling asleep or staying asleep or waking up frequently; (4) becoming irritable or angry easily; and (5) difficulty concentrating. Each question was answered by selecting from the following 5 options: not at all (1 point), a little bit (2 points), moderate (3 points), quite a bit (4 points), and extremely (5 points), using a 5-point Likert scale. The total score of emotional distress was the sum of the five items, ranging from 5 to 25. A higher score represented a great impact and worse emotional status.
2.3. Statistical Analyses
Descriptive statistics were calculated for the demographic characteristics, lifestyle, emotional distress, and daily sleep duration of the participants. Continuous variables are presented as means and standard deviation (SD), and categorical variables are presented as numbers with percentages. The independent-sample t-test and ANOVA were used to compare sleep duration and emotional distress among different groups according to demographic characteristics and lifestyle variables, as appropriate. A multivariate linear regression model was used to assess the associated factors of emotional distress among participants. In addition, Pearson’s correlation analysis and a multivariate linear regression model were used to explore the association between emotional distress and sleep duration. The statistical analyses were using SPSS Statistics software, version 19.0 (IBM, Chicago, IL, USA). A two-tailed p-value less than 0.05 was regarded as statistically significant for all tests.
3. Results
3.1. Basic Information of Participants
In total, 10,545 participants completed the online survey, and they were from all 31 provinces, autonomous regions, and municipalities in mainland China. By geographical regions, 1511 (14.3%) participants were in Western China, 3117 (29.6%) were in Central China, and 5917 (56.1%) were in Eastern China. The mean age of the participants was 31.8 ± 9.9 years; 43.7% were male and 56.3% were female. Detailed information on the demographic and lifestyle characteristics of the participants is presented in Table 1.

Table 1.
Basic characteristics of participants (n = 10,545).
3.2. Comparison of the Emotional Distress and Sleep Duration
Over 30% of participants reported experiencing at least one symptom of mental distress at a moderate level or higher (Figure 1). The average total score of emotional distress among all participants was 10.46 ± 4.90 points. As shown in Table 2, there were significant differences in emotional distress with respect to demographic and lifestyle variables (all p < 0.001). Emotional distress scores decreased with age and education. Men scored higher on emotional distress scores than women. Smokers and drinkers scored significantly higher than nonsmokers and non-drinkers, respectively. Participants who exercised during the pandemic had significantly lower emotional distress scores than those who did not.
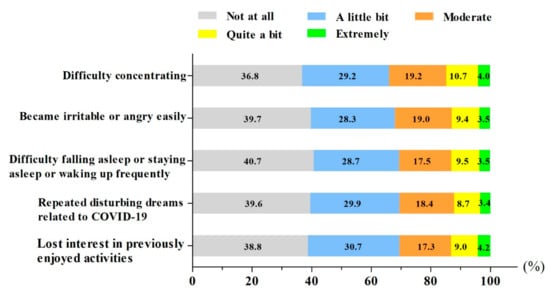
Figure 1.
Experience of emotional distress among the general population during the COVID-19 pandemic in China (n = 10,545).

Table 2.
Comparison of emotional distress and daily sleeping time according to demographic and lifestyle characteristics (n = 10,545).
The average daily sleep duration for all participants was 7.6 ± 1.7 h. There were significant differences in sleep duration with respect to age, gender, education, marital status, residence, employment status, and all lifestyle variables (all p < 0.001), but there were no significant differences with respect to ethnicity (p = 0.188) or medical insurance (p = 0.316) (Table 2). The average daily sleep duration reduced with age but increased with education. The daily sleep duration of smokers and drinkers was significantly lower than that of non-smokers and non-drinkers, respectively. Those who experienced food shortages had significantly higher emotional distress scores and a lower daily sleep duration than those who did not experience food shortages during the pandemic.
3.3. Multivariate Linear Regression Analyses of Influencing Factors of Emotional Distress
Table 3 shows the stepwise multivariate linear regression analyses of emotional distress. The independent variable codes are shown in Table A1 in Appendix A. The results revealed that increased emotional distress scores were associated with increased levels of the pandemic’s impact on diet (β = −1.106, 95% CI: −1.187 to −1.026, p < 0.001), food shortages (β = 1.334, 95% CI: 1.117 to 1.551, p < 0.001), not participating in physical exercise (β = −0.845, 95% CI: −1.024 to −0.667, p < 0.001), younger age (β = −0.050, 95% CI: −0.062 to −0.039, p < 0.001), being a smoker (β = 0.852, 95% CI: 0.604 to 1.100, p < 0.001), lower education level (β = −0.524, 95% CI: −0.702 to −0.346, p < 0.001), and not having medical insurance (β = −0.742, 95% CI: −1.012 to −0.473, p < 0.001). Compared with participants who were married, those who were unmarried (β = 0.404, 95% CI: 0.146 to 0.663, p = 0.002) or cohabiting (β = 1.881, 95% CI: 1.389 to 2.372, p < 0.001) had higher emotional distress scores. Students had lower emotional distress scores (β = −0.535, 95% CI: −0.821 to −0.250, p < 0.001) than participants who were employed.

Table 3.
Multivariate linear regression analyses of influencing factors of emotional distress.
3.4. Association between Emotional Distress and Daily Sleep Duration
Pearson’s correlation analysis showed that the correlation coefficient between the emotional distress score and daily sleep duration was −0.065 (p < 0.001). As shown in Table 4, multivariate linear model analyses revealed that the emotional distress scores were significantly negatively associated with daily sleep duration (β = −0.023, 95% CI: −0.029 to −0.016, p < 0.001). The results remained statistically significant after adjustment for age, gender, ethnicity, education, marital status, medical insurance, residence, and employment status (Model 1) (β = −0.024, 95% CI: −0.030 to −0.017, p < 0.001) and remained statistically significant after further adjustment for smoking, drinking, the pandemic’s impact on diet, food shortages, and physical exercise (Model 2) (β = −0.020, 95% CI: −0.027 to −0.013, p < 0.001).

Table 4.
Multivariate association analyses of emotional distress and daily sleeping time.
4. Discussion
The public suffered varying degrees of psychological stress during the public health emergency due to COVID-19. In February and March of 2020, all healthy Chinese residents throughout the nation were required to stay at home and maintain strict social distancing [23]. This strict lockdown policy resulted in cognitive distress, negative emotions, and reduced sleep quality in the general population [24]. The quarantine has proved to be associated with psychological distress and a high prevalence of mental health symptoms [25]. The present nationwide survey enrolled 10,545 participants from 25 April to 11 May 2020, in the immediate aftermath of the strict lockdown. Our main findings were that levels of emotional distress remained high and were associated with a number of demographic and lifestyle factors.
Anxiety and depressive symptoms were the most common mental problems experienced during this pandemic [9,10,26,27,28,29]. A longitudinal survey in the initial stage of the COVID-19 outbreak in China (31 January to 2 February 2020) showed that more than half of the respondents from the general population rated the psychological impact of the pandemic as moderate or severe, 28.8% of participants reported moderate to severe anxiety symptoms, 16.5% reported moderate to severe depressive symptoms, and 8.1% reported moderate to severe stress levels [27]. No significant changes in anxiety, depression, or stress levels were found in the second survey during the peak (28 February to 1 March 2020) of the COVID-19 outbreak in China [28]. Similar findings were observed in the initial stage of the COVID-19 outbreak in Spain, with 18.7% of the general population reporting depressive symptoms, 21.6% reporting anxiety, and 15.8% reporting PTSD symptoms [11]. All these findings suggest that a significant proportion of the general population experienced psychological distress during the pandemic. Therefore, promoting appropriate support is crucial to reduce emotional distress and promote the psychological well-being of the general population.
We found that emotional distress scores in the general population varied by the demographic and lifestyle factors measured. Multivariate analyses showed that participants with younger age, lower education level, and no medical insurance had increased emotional distress. A study showed that young adults were more vulnerable to being impacted by the COVID-19 lockdown [30]. Younger people tended to have increased emotional distress, potentially because of greater exposure to social media, which could easily trigger stress [16,31]. In this study, a higher education level was negatively associated with emotional distress. The opposite result was found in a previous study, in which people with higher education tended to report more distress in earlier surveys [16]. Thus, the role of education in modulating emotional distress is unclear. It is easier to understand that participants without medical insurance would show increased emotional distress due to the potential financial burden from illness. Married people showed less emotional distress than those who were unmarried and cohabiting, which was in line with the results of a previous study [9]. In unmarried people, the lack of a major social support system was suggested to mediate psychological distress [32]. In addition, a systematic review showed that living in rural areas and having a lower socioeconomic status was associated with higher anxiety odds [15]. However, our results showed that there was no urban/rural difference regarding emotional distress.
The implementation of lockdowns caused shortages of some kinds of food in markets because of panic buying and disruptions to the food supply. In this study, 26.9% of participants experienced food shortages during the COVID-19 outbreak. Moreover, being forced to stay indoors for a long time caused dramatic changes in people’s daily lifestyles and behaviors. Some studies have suggested that dietary habits have changed considerably during the pandemic in Spanish and Italian populations [33,34]. Our multivariate analyses revealed that experiencing a higher level of COVID-19’s impact on diet and food shortages during the pandemic were associated with increased emotional distress. In addition, participants who were smokers and did not participate in physical exercise showed higher levels of emotional distress. Recommendations for better dietary habits, exercise, and sleep were proposed in response to pandemic situations [35].
Stress from the COVID-19 situation has a negative impact on sleep. Recent studies have shown that 18.2% of the general population reported poor sleep quality, and 34.0% of health care workers reported symptoms of insomnia during the pandemic [29,36]. A systematic review showed that the global pooled prevalence of sleep problems among all populations was 35.7% during the pandemic [18]. Sleep plays an important role in emotion regulation, and sleep disturbances can negatively affect both physical and mental health. Lower quality sleep and insomnia were correlated with depressive symptoms, feelings of loneliness and anxiety, and a more negative mood during the pandemic and quarantines [17]. A study also showed that participants with better sleep quality and fewer early morning awakenings reported fewer PTSD symptoms during the COVID-19 outbreak [37]. Our results showed that emotional distress was negatively associated with daily sleep duration, suggesting that daytime emotional status can also affect nighttime sleep. Thus, paying attention to sleep is vital for the well-being of the general population during the COVID-19 pandemic.
Our study has several limitations. One is that this study was designed as a web-based survey through social media using the non-random snowball sampling method, and the participants needed to have a smartphone and be able to use WeChat. As with many internet surveys, the results are also limited by a lack of information about response rates and differences between respondents and nonrespondents [38]. As a result, our results may be subject to potential selection bias. Another limitation is that this study used a self-designed questionnaire to assess the impact of COVID-19 on the public’s emotional status. As a result, we cannot estimate the prevalence of emotional distress, and the findings need to be verified by questionnaires with proven validity. In addition, this is an observational study, and observed differences may be still subject to unobserved confounding factors that we could not control for in the analyses.
Despite some methodological limitations, this study was able to determine the huge emotional impact of COVID-19 on the general population in China. Addressing mental health in public health emergencies is important. Mental health professionals have vital responsibilities in providing mental support to the population [39]. The World Health Organization (WHO) and others have proposed a series of strategies to strengthen mental health care in countries experiencing and recovering from COVID-19 [40]. In addition, it is important for all countries to develop mid- to long-term support plans to respond to the mental health consequences of the pandemic [41].
5. Conclusions
In conclusion, this study revealed a great emotional impact among the general population caused by the COVID-19 outbreak and associated lockdown in China. Marriage status, employment status, COVID-19’s impact on diet, food shortages, participation in physical exercise, age, smoking, education, and medical insurance were the influencing factors of emotional distress among the general population. In addition, the public’s emotional distress was negatively associated with daily sleep duration. Our findings suggest that the emotional status of the general population needs further attention during the COVID-19 pandemic. Further research is needed to evaluate the long-term mental consequences of COVID-19 and the lockdown, taking into account the severity of COVID-19 prevalence and varying suppression measures in different countries.
Author Contributions
L.Y.: study conception and design, data collection, data analysis and interpretation, drafting of the article; J.S.: data collection, data analysis and interpretation; D.W.: study conception and design, data collection, data analysis and interpretation, critical revision of the article; A.R.: critical revision of the article; Z.S.: critical revision of the article; Y.W.: study conception and design, funding acquisition; X.L.: study conception and design, validation. All authors have read and agreed to the published version of the manuscript.
Funding
The project was supported in part by research grants from the China Medical Board (Grant Number: 16-262), the University Alliance of the Silk Road (Grant Number: 2020LMZX002), and Xi’an Jiaotong University Global Health Institute.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethical Committee of Health Science Center, Xi’an Jiaotong University in July 2020 (Number: 2020-1172).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Acknowledgments
The authors thank all participants in this study for their participation and cooperation. We thank Guorui Ruan, Lihua Yan, and Bingtong Zhao for their special assistance in supporting this project.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
The independent variable codes in the stepwise multiple linear regression model.
Table A1.
The independent variable codes in the stepwise multiple linear regression model.
| Variables | Value Codes |
|---|---|
| Age | Numerical variable (year) |
| Gender | Dummy variable: Male = 1; Female = 0 |
| Ethnicity | Dummy variable: Han Chinese = 1; others = 0 |
| Education | Numerical variable: Primary school or below = 1; Middle–high school = 2; University or above = 3 |
| Marital status | Categorical variable: Married = 1; Unmarried = 2; Cohabiting = 3; Widowed = 4; Divorced or separated = 5 |
| Medical insurance | Dummy variable: Yes = 1; No = 0 |
| Residence | Categorical variable: City = 1; Town = 2; Rural = 3 |
| Employment status | Categorical variable: Employed = 1; Student = 2; Unemployed = 3; Retired = 4 |
| Smoking | Dummy variable: Yes = 1; No (including those who quit smoking) = 0 |
| Drinking | Dummy variable: Yes = 1; No (including those who quit drinking) = 0 |
| COVID-19 impact on diet | Numerical variable: Great impact = 1; Some impact = 2; General = 3; Minimal impact = 4: Not at all = 5 |
| Experienced food shortage | Dummy variable: Yes = 1; No = 0 |
| Participated in physical exercise | Dummy variable: Yes = 1; No = 0 |
| Daily sleeping time | Numerical variable (hours) |
References
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Bio Med. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Lewnard, J.A.; Lo, N.C. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect. Dis. 2020, 20, 631–633. [Google Scholar] [CrossRef] [Green Version]
- Lau, H.; Khosrawipour, V.; Kocbach, P.; Mikolajczyk, A.; Schubert, J.; Bania, J.; Khosrawipour, T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Travel Med. 2020, 27, 37. [Google Scholar] [CrossRef] [Green Version]
- Chew, Q.; Wei, K.; Vasoo, S.; Chua, H.; Sim, K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: Practical considerations for the COVID-19 pandemic. Singap. Med. J. 2020, 61, 350–356. [Google Scholar] [CrossRef]
- Peng, E.Y.-C.; Lee, M.-B.; Tsai, S.-T.; Yang, C.-C.; Morisky, D.E.; Tsai, L.-T.; Weng, Y.-L.; Lyu, S.-Y. Population-based Post-crisis Psychological Distress: An Example from the SARS Outbreak in Taiwan. J. Formos. Med Assoc. 2010, 109, 524–532. [Google Scholar] [CrossRef] [Green Version]
- Jeong, H.; Yim, H.W.; Song, Y.-J.; Ki, M.; Min, J.-A.; Cho, J.; Chae, J.-H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol. Health 2016, 38, e2016048. [Google Scholar] [CrossRef]
- Vigo, D.; Patten, S.; Pajer, K.; Krausz, M.; Taylor, S.; Rush, B.; Raviola, G.; Saxena, S.; Thornicroft, G.; Yatham, L.N. Mental Health of Communities during the COVID-19 Pandemic. Can. J. Psychiatry 2020, 65, 681–687. [Google Scholar] [CrossRef]
- Wang, H.; Xia, Q.; Xiong, Z.; Li, Z.; Xiang, W.; Yuan, Y.; Liu, Y.; Li, Z. The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: A web-based survey. PLoS ONE 2020, 15, e0233410. [Google Scholar] [CrossRef]
- Li, J.; Yang, Z.; Qiu, H.; Wang, Y.; Jian, L.; Ji, J.; Li, K. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry 2020, 19, 249–250. [Google Scholar] [CrossRef]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Lorant, V.; Smith, P.; Broeck, K.V.D.; Nicaise, P. Psychological distress associated with the COVID-19 pandemic and suppression measures during the first wave in Belgium. BMC Psychiatry 2021, 21, 112. [Google Scholar] [CrossRef] [PubMed]
- Quaglieri, A.; Lausi, G.; Fraschetti, A.; Burrai, J.; Barchielli, B.; Pizzo, A.; Cordellieri, P.; De Gennaro, L.; Gorgoni, M.; Ferlazzo, F.; et al. “Stay at Home” in Italy during the COVID-19 Outbreak: A Longitudinal Study on Individual Well-Being among Different Age Groups. Brain Sci. 2021, 11, 993. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Kala, M.P.; Jafar, T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0244630. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef] [Green Version]
- Pilcher, J.J.; Dorsey, L.L.; Galloway, S.M.; Erikson, D.N. Social Isolation and Sleep: Manifestation During COVID-19 Quarantines. Front. Psychol. 2022, 12, 810763. [Google Scholar] [CrossRef]
- Jahrami, H.; Bahammam, A.S.; Bragazzi, N.L.; Saif, Z.; Faris, M.; Vitiello, M.V. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. J. Clin. Sleep Med. 2021, 17, 299–313. [Google Scholar] [CrossRef]
- Alfonsi, V.; Gorgoni, M.; Scarpelli, S.; Zivi, P.; Sdoia, S.; Mari, E.; Fraschetti, A.; Ferlazzo, F.; Giannini, A.M.; De Gennaro, L. COVID-19 lockdown and poor sleep quality: Not the whole story. J. Sleep Res. 2021, 30, e13368. [Google Scholar] [CrossRef]
- Alfonsi, V.; Gorgoni, M.; Scarpelli, S.; Zivi, P.; Sdoia, S.; Mari, E.; Quaglieri, A.; Ferlazzo, F.; Giannini, A.M.; De Gennaro, L. Changes in sleep pattern and dream activity across and after the COVID-19 lockdown in Italy: A longitudinal observational study. J. Sleep Res. 2021, 31, e13500. [Google Scholar] [CrossRef]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, K.C.; Lang, A.J.; Norman, S.B. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depress. Anxiety 2011, 28, 596–606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ainslie, K.E.C.; Walters, C.E.; Fu, H.; Bhatia, S.; Wang, H.; Xi, X.; Baguelin, M.; Bhatt, S.; Boonyasiri, A.; Boyd, O.; et al. Evidence of initial success for China exiting COVID-19 social distancing policy after achieving containment. Wellcome Open Res. 2020, 5, 81. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, H.; Ma, X.; Di, Q. Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int. J. Environ. Res. Public Health 2020, 17, 3722. [Google Scholar] [CrossRef] [PubMed]
- Fernández, R.S.; Crivelli, L.; Guimet, N.M.; Allegri, R.F.; Pedreira, M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. J. Affect. Disord. 2020, 277, 75–84. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Glowacz, F.; Schmits, E. Psychological distress during the COVID-19 lockdown: The young adults most at risk. Psychiatry Res. 2020, 293, 113486. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Oh, S.-T.; Lee, H.; Lee, J.S.; Pak, H.; Choi, W.-J.; Jeon, H.H. Associated risk factors for psychological distress in patients with gastric epithelial neoplasm undergoing endoscopic submucosal dissection. Medicine 2018, 97, e13912. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Pérez, C.; Molina-Montes, E.; Verardo, V.; Artacho, R.; García-Villanova, B.; Guerra-Hernández, E.J.; Ruíz-López, M.D. Changes in Dietary Behaviours during the COVID-19 Outbreak Confinement in the Spanish COVIDiet Study. Nutrients 2020, 12, 1730. [Google Scholar] [CrossRef] [PubMed]
- Scarmozzino, F.; Visioli, F. Covid-19 and the Subsequent Lockdown Modified Dietary Habits of Almost Half the Population in an Italian Sample. Foods 2020, 9, 675. [Google Scholar] [CrossRef] [PubMed]
- Abbas, A.M.; Kamel, M.M. Dietary habits in adults during quarantine in the context of COVID-19 pandemic. Obes. Med. 2020, 19, 100254. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated with Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Liu, N.; Zhang, F.; Wei, C.; Jia, Y.; Shang, Z.; Sun, L.; Wu, L.; Sun, Z.; Zhou, Y.; Wang, Y.; et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020, 287, 112921. [Google Scholar] [CrossRef]
- Tsuboi, S.; Yoshida, H.; Ae, R.; Kojo, T.; Nakamura, Y.; Kitamura, K. Selection Bias of Internet Panel Surveys. Asia Pac. J. Public Health 2015, 27, NP2390–NP2399. [Google Scholar] [CrossRef]
- Stewart, D.E.; Appelbaum, P.S. COVID-19 and psychiatrists’ responsibilities: A WPA position paper. World Psychiatry 2020, 19, 406–407. [Google Scholar] [CrossRef]
- Ghebreyesus, T.A. Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry 2020, 19, 129–130. [Google Scholar] [CrossRef]
- McDaid, D. Viewpoint: Investing in strategies to support mental health recovery from the COVID-19 pandemic. Eur. Psychiatry 2021, 64, e32. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).