Children Suspected for Developmental Coordination Disorder in Hong Kong and Associated Health-Related Functioning: A Survey Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Instruments
2.2.1. DCDQ
2.2.2. PROMIS®
2.2.3. Demographic Information
2.3. Data Processing and Analysis
3. Results
3.1. Suspect for DCD (sDCD) Prevalence
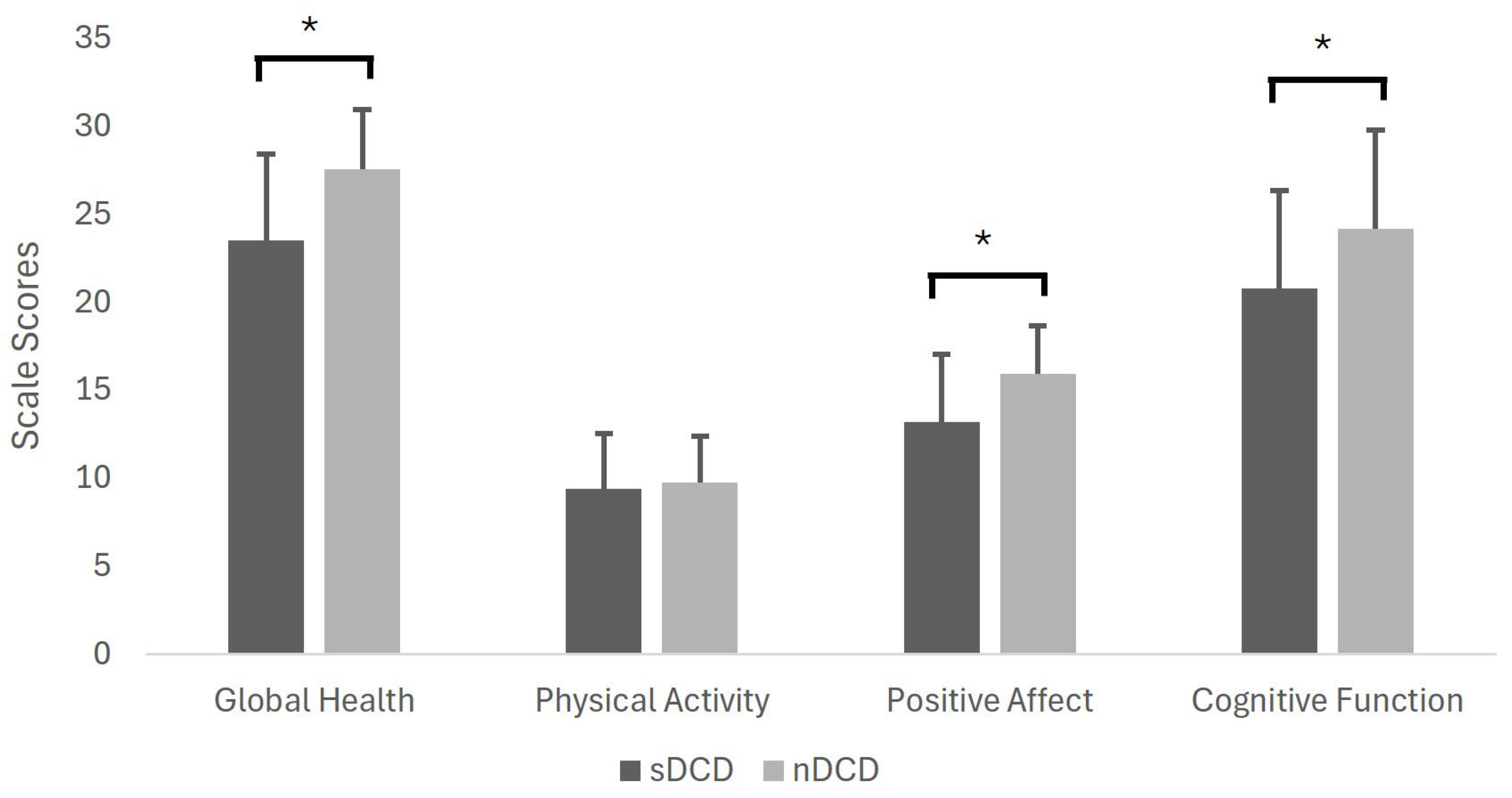
3.2. Motor Difficulties and Associated Health-Related Daily Functioning
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Text Revised ed.; American Psychiatric Association: Washington DC, USA, 2022. [Google Scholar]
- Blank, R.; Barnett, A.L.; Cairney, J.; Green, D.; Kirby, A.; Polatajko, H.; Rosenblum, S.; Smits-Engelsman, B.; Sugden, D.; Wilson, P.; et al. International Clinical Practice Recommendations on the Definition, Diagnosis, Assessment, Intervention, and Psychosocial Aspects of Developmental Coordination Disorder. Dev. Med. Child Neurol. 2019, 61, 242–285. [Google Scholar] [CrossRef] [PubMed]
- Karabak, M.; Akıncı, M.A.; Yıldırım Demirdöğen, E.; Bozkurt, A. Prevalence and Associated Factors of Developmental Coordination Disorder in Primary School Children. Eur. Child Adolesc. Psychiatry 2025, 34, 779–790. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.-C.; Tseng, Y.-T.; Hsu, F.-Y.; Chao, H.-C.; Wu, S.K. Developmental Coordination Disorder and Unhealthy Weight Status in Taiwanese Children: The Roles of Sex and Age. Children 2023, 10, 1171. [Google Scholar] [CrossRef]
- Lee, K.; Jung, T.; Lee, D.K.; Lim, J.-C.; Lee, E.; Jung, Y.; Lee, Y. A Comparison of Using the DSM-5 and MABC-2 for Estimating the Developmental Coordination Disorder Prevalence in Korean Children. Res. Dev. Disabil. 2019, 94, 103459. [Google Scholar] [CrossRef] [PubMed]
- Valentini, N.C.; Coutinho, M.T.C.; Pansera, S.M.; Santos, V.A.P.d.; Vieira, J.L.L.; Ramalho, M.H.; Oliveira, M.A.d. Prevalence of Motor Deficits and Developmental Coordination Disorders in Children from South Brazil. Rev. Paul. Pediatr. 2012, 30, 377–384. [Google Scholar] [CrossRef]
- Klein, E.S.; Licari, M.; Barbic, S.; Zwicker, J.G. Diagnostic Services for Developmental Coordination Disorder: Gaps and Opportunities Identified by Parents. Child Care Health Dev. 2024, 50, e13230. [Google Scholar] [CrossRef]
- Wilson, B.N.; Kaplan, B.J.; Crawford, S.G.; Campbell, A.; Dewey, D. Reliability and Validity of a Parent Questionnaire on Childhood Motor Skills. Am. J. Occup. Ther. 2000, 54, 484–493. [Google Scholar] [CrossRef]
- Wilson, B.N.; Crawford, S.G.; Green, D.; Roberts, G.; Aylott, A.; Kaplan, B.J. Psychometric Properties of the Revised Developmental Coordination Disorder Questionnaire. Phys. Occup. Ther. Pediatr. 2009, 29, 182–202. [Google Scholar] [CrossRef]
- Park, S.-H.; Kim, E.Y. Predictive Validity of the Developmental Coordination Disorder Questionnaire as a Screening Tool to Identify Motor Skill Problems: A Systematic Review and Meta-Analysis. Res. Dev. Disabil. 2024, 150, 104748. [Google Scholar] [CrossRef]
- Delgado-Lobete, L.; Santos-del-Riego, S.; Pértega-Díaz, S.; Montes-Montes, R. Prevalence of Suspected Developmental Coordination Disorder and Associated Factors in Spanish Classrooms. Res. Dev. Disabil. 2019, 86, 31–40. [Google Scholar] [CrossRef]
- Tsang, V.K.L.; Stagnitti, K.; Lo, S.K. Screening Children with Developmental Coordination Disorder: The Development of the Caregiver Assessment of Movement Participation. Child. Health Care 2010, 39, 232–248. [Google Scholar] [CrossRef]
- Sit, C.H.; Yu, J.J.; Wong, S.H.; Capio, C.M.; Masters, R. A School-Based Physical Activity Intervention for Children with Developmental Coordination Disorder: A Randomized Controlled Trial. Res. Dev. Disabil. 2019, 89, 1–9. [Google Scholar] [CrossRef]
- Yu, J.J.; Capio, C.M.; Abernethy, B.; Sit, C.H.P. Moderate-to-Vigorous Physical Activity and Sedentary Behavior in Children with and Without Developmental Coordination Disorder: Associations with Fundamental Movement Skills. Res. Dev. Disabil. 2021, 118, 104070. [Google Scholar] [CrossRef]
- Chung, E.Y. Unveiling Issues Limiting Participation of Children with Developmental Coordination Disorder: From Early Identification to Insights for Intervention. J. Dev. Phys. Disabil. 2018, 30, 373–389. [Google Scholar] [CrossRef]
- Wright, K.E.; Furzer, B.J.; Licari, M.K.; Thornton, A.L.; Dimmock, J.A.; Naylor, L.H.; Reid, S.L.; Kwan, S.R.; Jackson, B. Physiological Characteristics, Self-Perceptions, and Parental Support of Physical Activity in Children with, or at Risk of, Developmental Coordination Disorder. Res. Dev. Disabil. 2019, 84, 66–74. [Google Scholar] [CrossRef]
- Harrowell, I.; Hollén, L.; Lingam, R.; Emond, A. The Impact of Developmental Coordination Disorder on Educational Achievement in Secondary School. Res. Dev. Disabil. 2018, 72, 13–22. [Google Scholar] [CrossRef]
- Omer, S.; Jijon, A.M.; Leonard, H.C. Research Review: Internalising Symptoms in Developmental Coordination Disorder: A Systematic Review and Meta-Analysis. J. Child Psychol. Psychiatry 2019, 60, 606–621. [Google Scholar] [CrossRef]
- O’Dea, Á.; Stanley, M.; Coote, S.; Robinson, K. Children and Young People’s Experiences of Living with Developmental Coordination Disorder/Dyspraxia: A Systematic Review and Meta-Ethnography of Qualitative Research. PLoS ONE 2021, 16, e0245738. [Google Scholar] [CrossRef]
- Zwicker, J.G.; Lee, E.J. Early Intervention for Children with/at Risk of Developmental Coordination Disorder: A Scoping Review. Dev. Med. Child. Neurol. 2021, 63, 659–667. [Google Scholar] [CrossRef]
- Damiano, D.L. Early Identification and Intervention in Developmental Coordination Disorder: Lessons for and from Cerebral Palsy. Dev. Med. Child Neurol. 2021, 63, 630. [Google Scholar] [CrossRef]
- Kirby, A.; Sugden, D.; Purcell, C. Diagnosing Developmental Coordination Disorders. Arch. Dis. Child. 2014, 99, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Tseng, M.-H.; Fu, C.-P.; Wilson, B.N.; Hu, F.-C. Psychometric Properties of a Chinese Version of the Developmental Coordination Disorder Questionnaire in Community-Based Children. Res. Dev. Disabil. 2010, 31, 33–45. [Google Scholar] [CrossRef] [PubMed]
- PROMIS Health Organization. PROMIS Instrument Development and Validation Scientific Standards (Version 2.0); PROMIS Health Organization: River Forest, IL, USA, 2013. [Google Scholar]
- Varni, J.W.; Thissen, D.; Stucky, B.D.; Liu, Y.; Gorder, H.; Irwin, D.E.; DeWitt, E.M.; Lai, J.-S.; Amtmann, D.; DeWalt, D.A. PROMIS® Parent Proxy Report Scales: An Item Response Theory Analysis of the Parent Proxy Report Item Banks. Qual. Life Res. 2012, 21, 1223–1240. [Google Scholar] [CrossRef]
- Irwin, D.E.; Gross, H.E.; Stucky, B.D.; Thissen, D.; DeWitt, E.M.; Lai, J.S.; Amtmann, D.; Khastou, L.; Varni, J.W.; DeWalt, D.A. Development of Six PROMIS Pediatrics Proxy-Report Item Banks. Health Qual. Life Outcomes 2012, 10, 22. [Google Scholar] [CrossRef]
- De Walt, D.A.; Gross, H.E.; Gipson, D.S.; Selewski, D.T.; DeWitt, E.M.; Dampier, C.D.; Hinds, P.S.; Huang, I.-C.; Thissen, D.; Varni, J.W. PROMIS® Pediatric Self Report Scales Distinguish Subgroups of Children Within and Across Six Common Pediatric Chronic Health Conditions. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2015, 24, 2195. [Google Scholar] [CrossRef]
- Reeve, B.B.; Hays, R.D.; Bjorner, J.B.; Cook, K.F.; Crane, P.K.; Teresi, J.A.; Thissen, D.; Revicki, D.A.; Weiss, D.J.; Hambleton, R.K.; et al. Psychometric Evaluation and Calibration of Health-Related Quality of Life Item Banks: Plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Med. Care 2007, 45, S22–S31. [Google Scholar] [CrossRef]
- Rothrock, N.E.; Amtmann, D.; Cook, K.F. Development and Validation of an Interpretive Guide for PROMIS Scores. J. Patient-Rep. Outcomes 2020, 4, 16. [Google Scholar] [CrossRef]
- Terwee, C.B. Common Measures or Common Metrics? The Value of IRT-Based Common Metrics. J. Patient-Rep. Outcomes 2023, 7, 117. [Google Scholar] [CrossRef]
- Madley-Dowd, P.; Hughes, R.; Tilling, K.; Heron, J. The Proportion of Missing Data Should Not Be Used to Guide Decisions on Multiple Imputation. J. Clin. Epidemiol. 2019, 110, 63–73. [Google Scholar] [CrossRef]
- Tsang, T.K.; Huang, X.; Fong, M.W.; Wang, C.; Lau, E.H.; Wu, P.; Cowling, B.J. Effects of School-Based Preventive Measures on COVID-19 Incidence, Hong Kong, 2022. Emerg. Infect. Dis. 2023, 29, 1850. [Google Scholar] [CrossRef]
- So, H.-K.; Chua, G.T.; Yip, K.-M.; Tung, K.T.S.; Wong, R.S.; Louie, L.H.T.; Tso, W.W.Y.; Wong, I.C.K.; Yam, J.C.; Kwan, M.Y.W.; et al. Impact of COVID-19 Pandemic on School-Aged Children’s Physical Activity, Screen Time, and Sleep in Hong Kong: A Cross-Sectional Repeated Measures Study. Int. J. Environ. Res. Public Health 2022, 19, 10539. [Google Scholar] [CrossRef] [PubMed]
- Barba, P.C.d.S.D.; Luiz, E.M.; Pinheiro, R.C.; Lourenço, G.F. Prevalence of Developmental Coordination Disorder Signs in Children 5 to 14 Years in São Carlos. Motricidade 2017, 13, 22–30. [Google Scholar] [CrossRef]
- Ganapathy Sankar, U.; Monisha, R. The Prevalence of Developmental Co-Ordination Disorder among Primary School. Int. J. Res. Pharm. Sci. 2020, 11, 6543–6547. [Google Scholar] [CrossRef]
- Komal, K.B.; Sanjay, P. Indication or Suspect of Developmental Coordination Disorder in 5–15 Years of School Going Children in India (Dharwad, Karnataka). Int. J. Health Sci. Res. 2014, 4, 117–122. [Google Scholar]
- Koning, M.; de Jong, A.; de Jong, E.; Visscher, T.L.S.; Seidell, J.C.; Renders, C.M. Agreement Between Parent and Child Report of Physical Activity, Sedentary and Dietary Behaviours in 9–12-Year-Old Children and Associations with Children’s Weight Status. BMC Psychol. 2018, 6, 14. [Google Scholar] [CrossRef]
- Humble, A.; Yu, M.-L.; Brown, T. Association between Parent-Proxy-Reported and Child-Self-Reported Perceptions of Children’s Motor Competence and Children’s Performance-Based Motor Skill Abilities. Scand. J. Occup. Ther. 2024, 31, 2274883. [Google Scholar] [CrossRef]
- Ke, L.; Su, X.; Yang, S.; Du, Z.; Huang, S.; Wang, Y. New Trends in Developmental Coordination Disorder: Multivariate, Multidimensional and Multimodal. Front. Psychiatry 2023, 14, 1116369. [Google Scholar] [CrossRef]
- Sugden, D.A.; Chambers, M.E. Stability and Change in Children with Developmental Coordination Disorder. Child Care Health Dev. 2007, 33, 520–528. [Google Scholar] [CrossRef]
- Green, D.; Lingam, R.; Mattocks, C.; Riddoch, C.; Ness, A.; Emond, A. The Risk of Reduced Physical Activity in Children with Probable Developmental Coordination Disorder: A Prospective Longitudinal Study. Res. Dev. Disabil. 2011, 32, 1332–1342. [Google Scholar] [CrossRef]
- Tran, H.-T.; Ho, W.-C.; Chou, L.-W.; Li, Y.-C. Objectively Measured Physical Activity in Children with Developmental Coordination Disorder: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2024, 106, 269–279. [Google Scholar] [CrossRef]
- Tapia-Serrano, M.A.; Sevil-Serrano, J.; Sánchez-Miguel, P.A.; López-Gil, J.F.; Tremblay, M.S.; García-Hermoso, A. Prevalence of Meeting 24-Hour Movement Guidelines from Pre-School to Adolescence: A Systematic Review and Meta-Analysis Including 387,437 Participants and 23 Countries. J. Sport Health Sci. 2022, 11, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Zwicker, J.G.; Harris, S.R.; Klassen, A.F. Quality of Life Domains Affected in Children with Developmental Coordination Disorder: A Systematic Review. Child Care Health Dev. 2013, 39, 562–580. [Google Scholar] [CrossRef] [PubMed]
- Missiuna, C.; Campbell, W.N. Psychological Aspects of Developmental Coordination Disorder: Can We Establish Causality? Curr. Dev. Disord. Rep. 2014, 1, 125–131. [Google Scholar] [CrossRef]
- Caçola, P. Physical and Mental Health of Children with Developmental Coordination Disorder. Front. Public Health 2016, 4, 224. [Google Scholar] [CrossRef]
- Leonard, H.C. The Impact of Poor Motor Skills on Perceptual, Social and Cognitive Development: The Case of Developmental Coordination Disorder. Front. Psychol. 2016, 7, 311. [Google Scholar] [CrossRef]
- Roebers, C.M.; Röthlisberger, M.; Neuenschwander, R.; Cimeli, P.; Michel, E.; Jäger, K. The Relation between Cognitive and Motor Performance and Their Relevance for Children’s Transition to School: A Latent Variable Approach. Hum. Mov. Sci. 2014, 33, 284–297. [Google Scholar] [CrossRef]
- Wulf, G.; Lewthwaite, R. Optimizing Performance through Intrinsic Motivation and Attention for Learning: The OPTIMAL Theory of Motor Learning. Psychon. Bull. Rev. 2016, 23, 1382–1414. [Google Scholar] [CrossRef]
- Capio, C.M.; Poolton, J.M.; Sit, C.H.P.; Holmstrom, M.; Masters, R.S.W. Reducing Errors Benefits the Field-Based Learning of a Fundamental Movement Skill in Children. Scand. J. Med. Sci. Sports 2013, 23, 181–188. [Google Scholar] [CrossRef]
- Tran, H.-T.; Tseng, Y.-T.; Chen, S.; Wu, S.K.; Li, Y.-C. Moderation of Parental Socioeconomic Status on the Relationship between Birth Health and Developmental Coordination Disorder at Early Years. Front. Pediatr. 2023, 11, 1020428. [Google Scholar] [CrossRef]
- Brooks-Gunn, J.; Duncan, G.J. The Effects of Poverty on Children. Future Child. 1997, 7, 55–71. [Google Scholar] [CrossRef]
- Piketty, T.; Yang, L. Income and Wealth Inequality in Hong Kong, 1981–2020: The Rise of Pluto-Communism? World Bank Econ. Rev. 2022, 36, 803–834. [Google Scholar] [CrossRef]
- Oxfam Hong Kong. Hong Kong Poverty Report 2024: Pathways out of Adversity—Embracing Change Through Transformation; Oxfam Hong Kong: Hong Kong SAR, China, 2024. [Google Scholar]
| n | Percentage | |
|---|---|---|
| Age group of child | ||
| 5 years–7 years, 11 months | 293 | 44.67% |
| 8 years–9 years, 11 months | 156 | 23.78% |
| 10 years–12 years | 206 | 31.40% |
| Missing | 1 | 0.15% |
| Sex of child | ||
| Male | 340 | 51.83% |
| Female | 316 | 48.17% |
| Missing | 0 | 0 |
| Age group of parent | ||
| 18–24 years | 10 | 1.52% |
| 25–34 years | 130 | 19.82% |
| 35–44 years | 370 | 56.40% |
| 45–54 years | 130 | 19.82% |
| 55–60 years | 8 | 1.22% |
| >60 years | 6 | 0.92% |
| Missing | 2 | 0.31% |
| Education attainment of parent | ||
| Primary education or below | 2 | 0.31% |
| Secondary education | 141 | 21.49% |
| Nondegree postsecondary | 111 | 16.92% |
| Undergraduate degree | 298 | 45.43% |
| Postgraduate degree | 102 | 15.55% |
| Missing | 2 | 0.31% |
| Household monthly income (HK$) | ||
| <200,000 | 44 | 6.71% |
| 20,001–40,000 | 142 | 21.65% |
| 40,001–60,000 | 189 | 28.81% |
| 60,001–80,000 | 125 | 19.06% |
| 80,001–100,000 | 60 | 9.15% |
| >100,000 | 94 | 14.33% |
| Missing | 2 | 0.31% |
| Variable | B | SE (B) | Wald X2 | p | OR | 95% CI |
|---|---|---|---|---|---|---|
| Household income | −0.253 | 0.075 | 11.454 | <0.001 | 0.776 | 0.671 to 0.899 |
| Child’s age (months) | 0.012 | 0.004 | 8.513 | 0.004 | 1.012 | 1.004 to 1.020 |
| Child’s sex (male) | −1.221 | 0.649 | 3.543 | 0.060 | 0.295 | 0.083 to 1.052 |
| Parent’s education | −0.057 | 0.064 | 0.776 | 0.378 | 0.945 | 0.833 to 1.072 |
| Parent’s age (years) | −0.026 | 0.140 | 0.036 | 0.850 | 0.974 | 0.741 to 1.280 |
| Mean (SD) | Correlation Coefficient (r) Significance (p) | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| 1. DCDQ total | 61.58 (12.89) | - | ||||||
| 2. DCDQ-CM | 24.32 (5.37) | 0.93 * <0.001 | - | |||||
| 3. DCDQ-FM | 16.93 (3.79) | 0.91 * <0.001 | 0.78 * <0.001 | - | ||||
| 4. DCDQ-GC | 20.325 (4.61) | 0.94 * <0.001 | 0.79 * <0.001 | 0.82 * <0.001 | - | |||
| 5. GH | 26.74 (4.07) | 0.52 * <0.001 | 0.45 * <0.001 | 0.46 * <0.001 | 0.53 * <0.001 | - | ||
| 6. Pact | 9.67 (2.72) | 0.06 0.15 | 0.05 0.17 | 0.01 0.75 | 0.08 * 0.04 | 0.04 0.36 | - | |
| 7. Paff | 15.36 (3.19) | 0.38 * <0.001 | 0.35 * <0.001 | 0.32 * <0.001 | 0.38 * <0.001 | 0.56 * <0.001 | 0.15 * <0.001 | - |
| 8. CF | 23.00 (5.78) | 0.34 * <0.001 | 0.27 * <0.001 | 0.36 * <0.001 | 0.34 * <0.001 | 0.41 * <0.001 | −0.06 0.13 | 0.22 * <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eguia, K.F.; Cheung, S.K.; Chung, K.K.H.; Capio, C.M. Children Suspected for Developmental Coordination Disorder in Hong Kong and Associated Health-Related Functioning: A Survey Study. Disabilities 2025, 5, 32. https://doi.org/10.3390/disabilities5010032
Eguia KF, Cheung SK, Chung KKH, Capio CM. Children Suspected for Developmental Coordination Disorder in Hong Kong and Associated Health-Related Functioning: A Survey Study. Disabilities. 2025; 5(1):32. https://doi.org/10.3390/disabilities5010032
Chicago/Turabian StyleEguia, Kathlynne F., Sum Kwing Cheung, Kevin K. H. Chung, and Catherine M. Capio. 2025. "Children Suspected for Developmental Coordination Disorder in Hong Kong and Associated Health-Related Functioning: A Survey Study" Disabilities 5, no. 1: 32. https://doi.org/10.3390/disabilities5010032
APA StyleEguia, K. F., Cheung, S. K., Chung, K. K. H., & Capio, C. M. (2025). Children Suspected for Developmental Coordination Disorder in Hong Kong and Associated Health-Related Functioning: A Survey Study. Disabilities, 5(1), 32. https://doi.org/10.3390/disabilities5010032








