The Leisure Time Physical Activity Questionnaire for People with Disabilities: Validity and Reliability
Abstract
1. Introduction
2. Materials and Methods
2.1. Development and Content Validation
2.2. Construct Validation and Reliability
2.3. PA Questionnaire Measures
2.3.1. Leisure Time Physical Activity Questionnaire for People with Disabilities
2.3.2. Physical Activity Scale for Individuals with Physical Disabilities (PASIPD)
2.3.3. International Physical Activity Questionnaire—Short Form (IPAQ-SF)
2.3.4. Physical Activity and Disability Survey
2.3.5. Behavioral Risk Factor Surveillance System Strength Training Questionnaire (BRFSS-SQ)
2.4. Measures of Muscle Strength and Cardiovascular Fitness
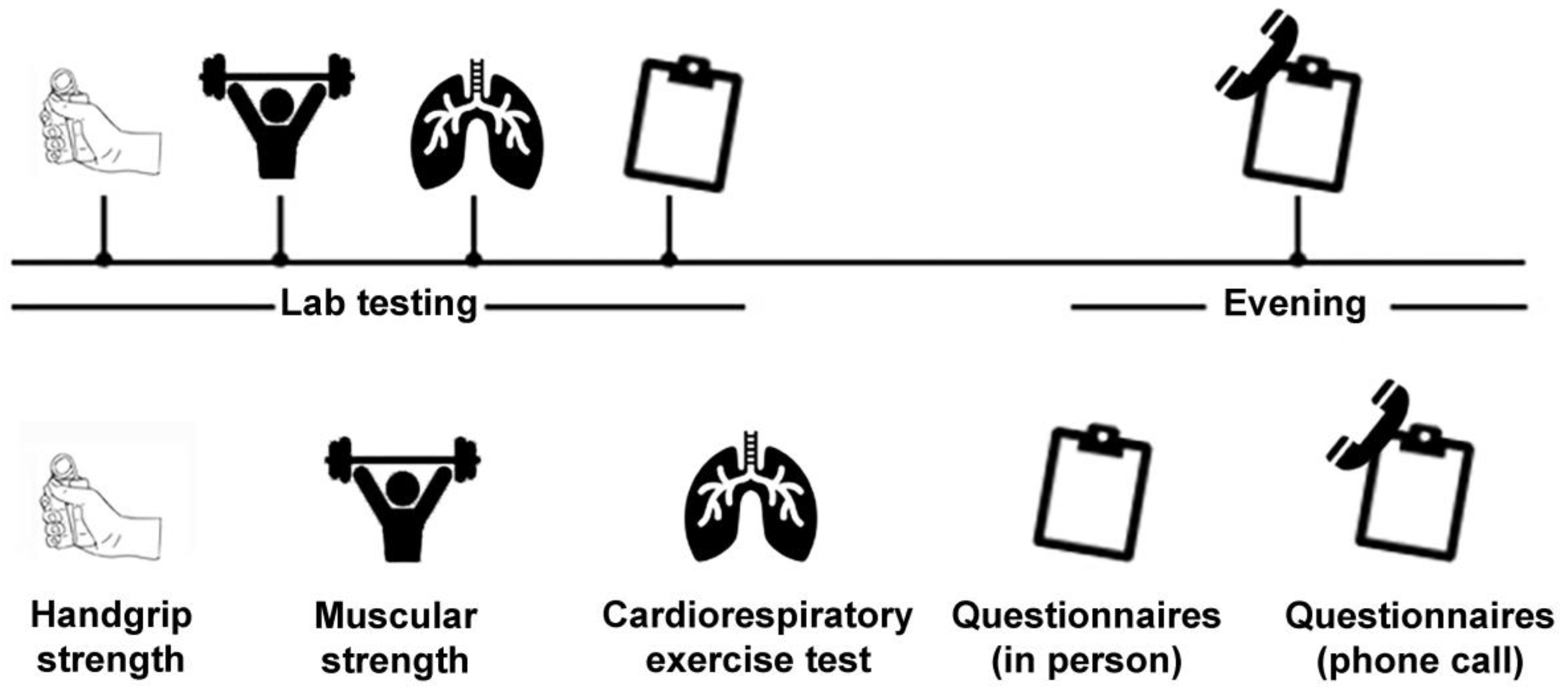
2.5. Procedure
2.6. Sample Size Calculation
2.7. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Construct Validity
3.2.1. Aerobic LTPA
3.2.2. Strength Training LTPA
3.2.3. Combined Aerobic and Strength Training LTPA
3.3. Test–Retest Reliability
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Martin Ginis, K.; van der Ploeg, H.P.; Foster, C.; Lai, B.; McBride, C.B.; Ng, K.; Pratt, M.; Shirazipour, C.H.; Smith, B.; Vasquez, P.M.; et al. Participation of people living with disabilities in physical activity: A global perspective. Lancet 2021, 398, 443–455. [Google Scholar] [CrossRef] [PubMed]
- Martin Ginis, K.A.; Sharma, R.; Brears, S.L. Physical activity and chronic disease prevention: Where is the research on people living with disabilities? CMAJ 2022, 194, E338–E340. [Google Scholar] [CrossRef] [PubMed]
- Carty, C.; van der Ploeg, H.P.; Biddle, S.J.; Bull, F.; Willumsen, J.; Lee, L.; Kamenov, K.; Milton, K. The First Global Physical Activity and Sedentary Behavior Guidelines for People Living with Disability. J. Phys. Act. Health 2021, 18, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Nigg, C.R.; Fuchs, R.; Gerber, M.; Jekauc, D.; Koch, T.; Krell-Roesch, J.; Lippke, S.; Mnich, C.; Novak, B.; Ju, Q.; et al. Assessing physical activity through questionnaires—A consensus of best practices and future directions. Psychol. Sport Exerc. 2020, 50, 101715. [Google Scholar] [CrossRef]
- Lavelle, G.; Noorkoiv, M.; Theis, N.; Korff, T.; Kilbride, C.; Baltzopoulos, V.; Shortland, A.; Levin, W.; Ryan, J.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF) as a measure of physical activity (PA) in young people with cerebral palsy: A cross-sectional study. Physiotherapy 2020, 107, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, T.E.; Rouse, P.C.; Thompson, D.; Bilzon, J.L.J. Measurement of Physical Activity and Energy Expenditure in Wheelchair Users: Methods, Considerations and Future Directions. Sports Med. Open 2017, 3, 10. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R.; Schmitz, K.H.; Emplaincourt, P.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S516. [Google Scholar] [CrossRef]
- Martin Ginis, K.A.; Phang, S.H.; Latimer, A.E.; Arbour-Nicitopoulos, K.P. Reliability and Validity Tests of the Leisure Time Physical Activity Questionnaire for People with Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2012, 93, 677–682. [Google Scholar] [CrossRef]
- Terwee, C.B.; Mokkink, L.B.; van Poppel, M.N.; Chinapaw, M.J.; van Mechelen, W.; de Vet, H.C. Qualitative attributes and measurement properties of physical activity questionnaires: A checklist. Sports Med. 2010, 40, 525–537. [Google Scholar] [CrossRef]
- Streiner, D.L.; Norman, G.R.; Cairney, J. Health Measurement Scales: A Practical Guide to Their Development and Use, 5th ed.; Oxford University Press: Oxford, UK, 2014; Available online: https://academic.oup.com/book/24920 (accessed on 7 May 2023).
- Washburn, R.A.; Zhu, W.; McAuley, E.; Frogley, M.; Figoni, S.F. The physical activity scale for individuals with physical disabilities: Development and evaluation. Arch. Phys. Med. Rehabil. 2002, 83, 193–200. [Google Scholar] [CrossRef]
- van der Ploeg, H.P.; Streppel, K.R.; van der Beek, A.J.; van der Woude, L.H.; Vollenbroek-Hutten, M.; van Mechelen, W. The Physical Activity Scale for Individuals with Physical Disabilities: Test-retest reliability and comparison with an accelerometer. J. Phys. Act. Health 2007, 4, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Menezes, D.; Laranjo, L.; Marmeleira, J. Criterion-related validity of the short form of the international physical activity questionnaire in adults who are Deaf. Disabil. Health J. 2017, 10, 33–38. [Google Scholar] [CrossRef]
- Roberts-Lewis, S.F.; White, C.M.; Ashworth, M.; Rose, M.R. The validity of the International Physical Activity Questionnaire (IPAQ) for adults with progressive muscle diseases. Disabil. Rehabil. 2022, 44, 7312–7320. [Google Scholar] [CrossRef] [PubMed]
- Rimmer, J.H.; Riley, B.B.; Rubin, S.S. A New Measure for Assessing the Physical Activity Behaviors of Persons with Disabilities and Chronic Health Conditions: The Physical Activity and Disability Survey. Am. J. Health Promot. 2001, 16, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Kayes, N.M.; McPherson, K.M.; Taylor, D.; Schluter, P.J.; Wilson, B.-J.K.; Kolt, G.S. The Physical Activity and Disability Survey (PADS): Reliability, validity and acceptability in people with multiple sclerosis. Clin. Rehabil. 2007, 21, 628–639. [Google Scholar] [CrossRef]
- Ciccolo, J.T.; Gabriel, K.K.P.; Macera, C.; Ainsworth, B.E. Association Between Self-Reported Resistance Training and Self-Rated Health in a National Sample of U.S. Men and Women. J. Phys. Act. Health 2010, 7, 289–298. [Google Scholar] [CrossRef]
- Ribeiro Neto, F.; Guanais, P.; Dornelas, E.; Coutinho, A.C.B.; Costa, R.R.G. Validity of one-repetition maximum predictive equations in men with spinal cord injury. Spinal Cord 2017, 55, 950–956. [Google Scholar] [CrossRef]
- Shoepe, T.C.; LaBrie, J.W.; Mello, G.T.; Leggett, A.G.; Almstedt, H.C. Intensity of resistance training via self-reported history is critical in properly characterizing musculoskeletal health. BMC Musculoskelet. Disord. 2020, 21, 729. [Google Scholar] [CrossRef]
- American Thoracic Society. ATS/ACCP Statement on Cardiopulmonary Exercise Testing. Am. J. Respir. Crit. Care Med. 2003, 167, 211–277. [Google Scholar] [CrossRef] [PubMed]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 6th ed.; Allyn & Bacon: Boston, MA, USA, 2012. [Google Scholar]
- Talbot, L.A.; Metter, E.J.; Fleg, J.L. Leisure-time physical activities and their relationship to cardiorespiratory fitness in healthy men and women 18–95 years old. Med. Sci. Sports Exerc. 2000, 32, 417. [Google Scholar] [CrossRef] [PubMed]
- Francis, P.; Lyons, M.; Piasecki, M.; Mc Phee, J.; Hind, K.; Jakeman, P. Measurement of muscle health in aging. Biogerontology 2017, 18, 901–911. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Martin Ginis, K.A.; Latimer-Cheung, A.E.; West, C.R. Commentary on “the first global physical activity and sedentary behavior guidelines for people living with disability”. J. Phys. Act. Health 2021, 18, 348–349. [Google Scholar] [CrossRef]
- Gee, C.M.; Lacroix, M.A.; Stellingwerff, T.; Gavel, E.H.; Logan-Sprenger, H.M.; West, C.R. Physiological Considerations to Support Podium Performance in Para-Athletes. Front. Rehabil. Sci. 2021, 2, 84. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, L.D.; Leech, N.L. Understanding correlation: Factors that affect the size of r. J. Exp. Educ. 2006, 74, 249–266. [Google Scholar] [CrossRef]
- Sallis, J.F.; Saelens, B.E. Assessment of physical activity by self-report: Status, limitations, and future directions. Res. Q. Exerc. Sport 2000, 71, S1–S14. [Google Scholar] [CrossRef]
- Ma, J.K.; McCracken, L.A.; Voss, C.; Chan, F.H.; West, C.R.; Martin Ginis, K.A. Physical activity measurement in people with spinal cord injury: Comparison of accelerometry and self-report (the Physical Activity Recall Assessment for People with Spinal Cord Injury). Disabil. Rehabil. 2020, 42, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Martin Ginis, K.A.; Úbeda-Colomer, J.; Alrashidi, A.A.; Nightingale, T.E.; Au, J.S.; Currie, K.D.; Hubli, M.; Krassioukov, A. Construct validation of the leisure time physical activity questionnaire for people with SCI (LTPAQ-SCI). Spinal Cord 2021, 59, 311–318. [Google Scholar] [CrossRef] [PubMed]
| Demographic Variables | n (% Total); Mean ± SD |
|---|---|
| Sex | |
| Male | 14 (52%) |
| Female | 13 (48%) |
| Age (years (range)) | 45 ± 21 (18–78) |
| Height (m) | 1.74 ± 0.11 |
| Male | 1.78 ± 0.09 |
| Female | 1.69 ± 0.11 |
| Body mass (kg) | 82 ± 24 |
| Male | 84 ± 18 |
| Female | 79 ± 29 |
| Years living with disability | 14 ± 8 |
| LTPAQ-D measures | |
| Mild-intensity aerobic (min/week) | 236 ± 202 |
| Moderate-intensity aerobic (min/week) | 104 ± 114 |
| Vigorous-intensity aerobic (min/week) | 50 ± 94 |
| Aerobic LTPA (min/week) | 391 ± 300 |
| Aerobic MVPA (min/week) | 154 ± 157 |
| Strength training (day/week) | 2 ± 2 |
| Strength training (min/week) | 92 ± 169 |
| All LTPA (min/week) | 483 ± 398 |
| Measure | LTPAQ-D Aerobic LTPA (min/week) | LTPAQ-D Aerobic MVPA (min/week) | LTPAQ-D All LTPA (min/week) |
|---|---|---|---|
| PASIPD (MET h/day) | 0.662 † | 0.577 * | 0.613 † |
| IPAQ-SF LTPA (min/week) | 0.635 † | 0.458 * | 0.657 † |
| IPAQ-SF MVPA (min/week) | 0.651 † | 0.649 † | 0.656 † |
| PADS Exercise + LTPA (min/week) | 0.744 † | 0.536 * | 0.718 † |
| O2peak (mL/kg/min) | 0.341 | 0.356 | 0.387 |
| Measure | LTPAQ-D Strength Training (day/week) | LTPAQ-D Strength Training (min/week) |
|---|---|---|
| BRFSS-SQ (day/week) | 0.942 † | 0.861 † |
| POpeak (Watts) | 0.182 | 0.201 |
| Seated Row Predicted 1RM (kg) | 0.254 | 0.429 |
| Chest Press Predicted 1RM (kg) | 0.514 * | 0.621 * |
| Grip Strength Dominant (kg) | 0.351 | 0.390 |
| Grip Strength Non-Dominant (kg) | 0.065 | 0.240 |
| Measure | Intraclass Correlation (95% CI) | p-Value |
|---|---|---|
| Measures of aerobic LTPA | ||
| Mild-intensity aerobic (min/week) | 0.709 (0.454–0.857) | <0.001 |
| Moderate-intensity aerobic (min/week) | 0.885 (0.764–0.946) | <0.001 |
| Vigorous-intensity aerobic (min/week) | 0.814 (0.681–0.924) | <0.001 |
| Aerobic LTPA (min/week) | 0.792 (0.592–0.899) | <0.001 |
| Aerobic MVPA (min/week) | 0.923 (0.838–0.964) | <0.001 |
| Strength training LTPA | ||
| Strength training (day/week) | 0.908 (0.808–0.957) | <0.001 |
| a Strength training (min/week) | 0.836 (0.675–0.921) | <0.001 |
| b Strength training total time (min/week) | 0.948 (0.890–0.976) | <0.001 |
| c Strength training resting time (min/week) | 0.775 (0.568–0.891) | <0.001 |
| Combined aerobic + strength training LTPA | ||
| All LTPA (min/week) | 0.751 (0.522–0.878) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gee, C.M.; Neely, A.; Jevdjevic, A.; Olsen, K.; Martin Ginis, K.A. The Leisure Time Physical Activity Questionnaire for People with Disabilities: Validity and Reliability. Disabilities 2024, 4, 321-331. https://doi.org/10.3390/disabilities4020021
Gee CM, Neely A, Jevdjevic A, Olsen K, Martin Ginis KA. The Leisure Time Physical Activity Questionnaire for People with Disabilities: Validity and Reliability. Disabilities. 2024; 4(2):321-331. https://doi.org/10.3390/disabilities4020021
Chicago/Turabian StyleGee, Cameron M., Ava Neely, Aleksandra Jevdjevic, Kenedy Olsen, and Kathleen A. Martin Ginis. 2024. "The Leisure Time Physical Activity Questionnaire for People with Disabilities: Validity and Reliability" Disabilities 4, no. 2: 321-331. https://doi.org/10.3390/disabilities4020021
APA StyleGee, C. M., Neely, A., Jevdjevic, A., Olsen, K., & Martin Ginis, K. A. (2024). The Leisure Time Physical Activity Questionnaire for People with Disabilities: Validity and Reliability. Disabilities, 4(2), 321-331. https://doi.org/10.3390/disabilities4020021








