“Someone Like Anyone Else”: A Qualitative Exploration of New Zealand Health Professional Students’ Understanding of Disability
Abstract
:1. Introduction
2. Materials and Methods
2.1. Recruitment
2.2. Data Collection
2.3. Methodological Approach: Thematic Analysis
2.3.1. Reflexivity
2.3.2. Familiarization of Data and Coding (Phase 1 and 2)
2.3.3. Generating Initial Themes, Reviewing, Refining, and Defining Themes (Phase 3, 4 and 5)
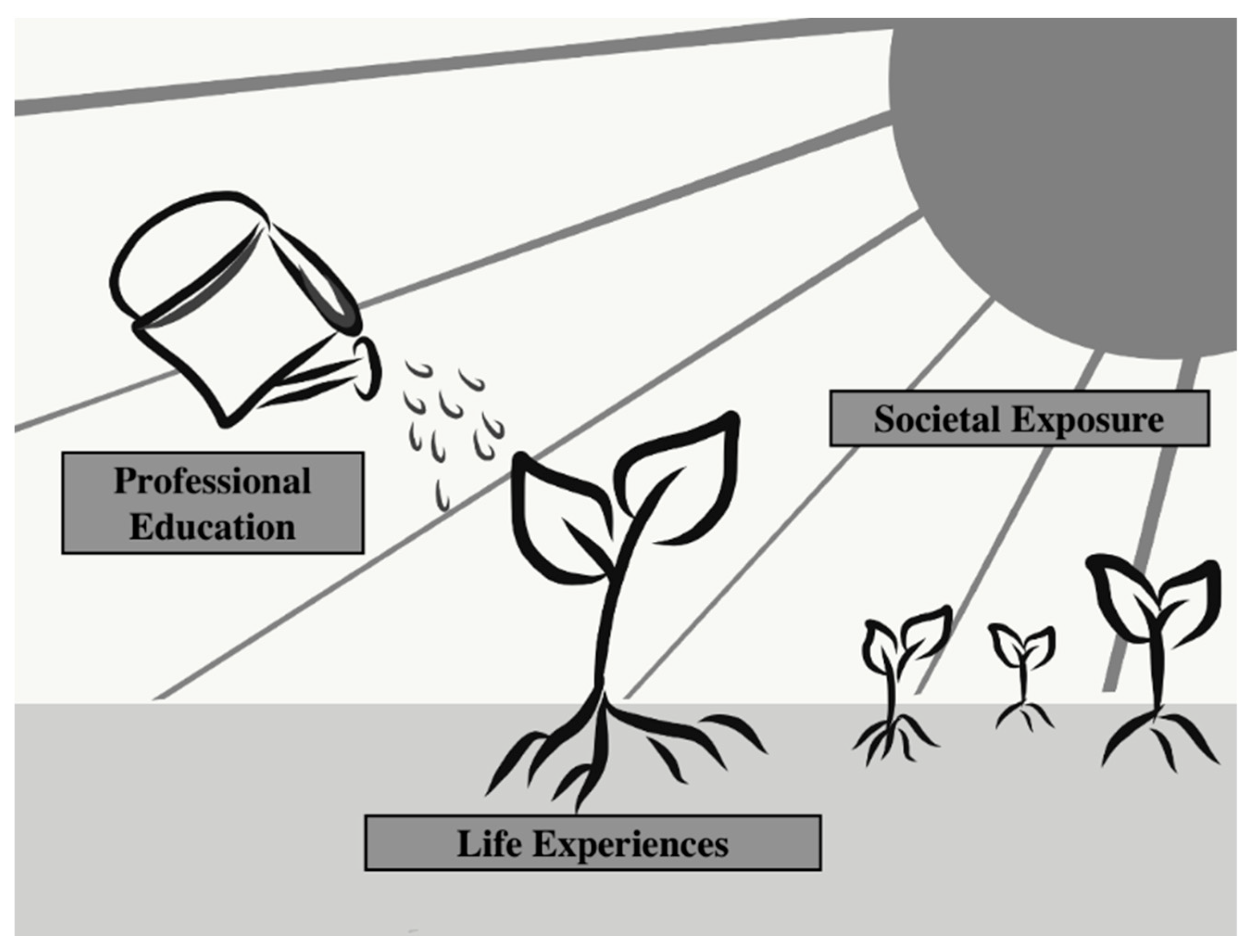
3. Results
3.1. Demographics
3.2. Life Experiences
3.2.1. Culturally Diverse Upbringing
3.2.2. Experiences with Disabled People Enabled a More Nuanced Understanding of Disability
3.3. Professional Education
3.3.1. Professional Education Awakened Students to Disability
3.3.2. Theoretical Knowledge Provided a Foundational Understanding of Disability Concepts
3.3.3. Experiential Learning Deepened Their Understanding
3.4. Societal Exposure: Being Part of an Inclusive Society
4. Discussion
4.1. Introduction
4.2. Previous Experience
4.3. Ethnoculture
4.4. Experiential Learning Opportunities for Student HPs
4.5. Education Bias
4.6. Strengths
4.7. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Global Disability Action Plan 2014–2021: Better Health for All People with Disability; World Health Organization: Geneva, Switzerland, 2015; Available online: https://apps.who.int/iris/handle/10665/199544 (accessed on 14 August 2018).
- Ministry of Health. 2013 New Zealand Disability Survey; Ministry of Health, Ed.; Ministry of Health: Wellington, New Zealand, 2014. Available online: http://archive.stats.govt.nz/browse_for_stats/health/disabilities/other-versions-disability-survey-2013.aspx#gsc.tab=0 (accessed on 22 May 2015).
- Jones, R.; Crowshoe, L.; Reid, P.; Calam, B.; Curtis, E.; Green, M.; Huria, T.; Jacklin, K.; Kamaka, M.; Lacey, C.; et al. Educating for indigenous health equity: An international consensus statement. Acad. Med. J. Assoc. Am. Med. Coll. 2019, 94, 512–519. [Google Scholar] [CrossRef]
- Jones, B.; King, P.T.; Baker, G.; Ingham, T. COVID-19, intersectionality, and health equity for indigenous peoples with lived experience of disability. Am. Indian Cult. Res. J. 2020, 44, 71–88. [Google Scholar] [CrossRef]
- Dirth, T.P.; Branscombe, N.R. Disability models affect disability policy support through awareness of structural discrimination. J. Soc. Issues 2017, 73, 413–442. [Google Scholar] [CrossRef]
- Frier, A.; Barnett, F.; Devine, S.; Barker, R. Understanding disability and the ‘social determinants of health’: How does disability affect peoples’ social determinants of health? Disabil. Rehabil. 2018, 40, 538–547. [Google Scholar] [CrossRef]
- Statistics New Zealand. Measuring Inequality for Disabled New Zealanders: 2018. 2020. Available online: https://www.stats.govt.nz/reports/measuring-inequality-for-disabled-new-zealanders-2018 (accessed on 18 December 2021).
- Mathias, K.; Pant, H.; Marella, M.; Singh, L.; Murthy, G.V.S.; Grills, N. Multiple barriers to participation for people with psychosocial disability in dehradun district, north India: A cross-sectional study. BMJ Open 2018, 8, e019443. [Google Scholar] [CrossRef] [Green Version]
- Pelleboer-Gunnink, H.; Van Oorsouw, W.; Van Weeghel, J.; Embregts, P. Mainstream health professionals’ stigmatising attitudes towards people with intellectual disabilities: A systematic review. J. Intellect. Disabil. Res. 2017, 61, 411–434. [Google Scholar] [CrossRef] [PubMed]
- Sahin, H.; Akyol, A.D. Evaluation of nursing and medical students’ attitudes towards people with disabilities. J. Clin. Nurs. 2010, 19, 2271–2279. [Google Scholar] [CrossRef]
- Ali, A.; Scior, K.; Ratti, V.; Strydom, A.; King, M.; Hassiotis, A. Discrimination and other barriers to accessing health care: Perspectives of patients with mild and moderate intellectual disability and their carers. PLoS ONE 2013, 8, e70855. [Google Scholar] [CrossRef]
- Hogan, A.; Jain, N.R.; Peiris-John, R.; Ameratunga, S. Disabled people say ‘nothing about us without us’. Clin. Teach. 2020, 17, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Kocman, A.; Fischer, L.; Weber, G. The employers’ perspective on barriers and facilitators to employment of people with intellectual disability: A differential mixed-method approach. J. Appl. Res. Intellect. Disabil. 2018, 31, 120–131. [Google Scholar] [CrossRef]
- Marshall, J.; Doone, E.; Price, M. Cultural models of child disability: Perspectives of parents in Malaysia. Disabil. Rehabil. 2019, 41, 2653–2662. [Google Scholar] [CrossRef] [PubMed]
- Ryan, T.A.; Scior, K. Medical students’ attitudes towards people with intellectual disabilities: A literature review. Res. Dev. Disabil. 2014, 35, 2316–2328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shakespeare, T.; Kleine, I. Educating health professionals about disability: A review of interventions. Health Soc. Care Educ. 2013, 2, 20–37. [Google Scholar] [CrossRef] [Green Version]
- Tervo, R.C.; Azuma, S.; Palmer, G.; Redinius, P. Medical students’ attitudes toward persons with disability: A comparative study. Arch. Phys. Med. Rehabil. 2002, 83, 1537–1542. [Google Scholar] [CrossRef]
- Wilkinson, J.; Dreyfus, D.; Bowen, D.; Bokhour, B. Patient and provider views on the use of medical services by women with intellectual disabilities. J. Intellect. Disabil. Res. 2013, 57, 1058–1067. [Google Scholar] [CrossRef]
- Adler, P.; Cregg, M.; Duignan, A.; Ilett, G.; Margaret Woodhouse, J. Effect of training on attitudes and expertise of optometrists towards people with intellectual disabilities. Ophthalmic Physiol. Opt. 2005. [Google Scholar] [CrossRef]
- Coyle, C.; Saunderson, W.; Freeman, R. Dental students, social policy students and learning disability: Do differing attitudes exist? Eur. J. Dent. Educ. 2004, 8, 133–139. [Google Scholar] [CrossRef]
- Crotty, M.; Finucane, P.; Ahern, M. Teaching medical students about disability and rehabilitation: Methods and student feedback. Med. Educ. 2000, 34, 659–664. [Google Scholar] [CrossRef]
- Desroches, M.L.; Howie, V.A.; Wilson, N.J.; Lewis, P. Nurses’ attitudes and emotions toward caring for adults with intellectual disability: An international replication study. J. Nurs. Scholarsh. 2022, 54, 117–124. [Google Scholar] [CrossRef]
- Desroches, M.L.; Sethares, K.A.; Curtin, C.; Chung, J. Nurses’ attitudes and emotions toward caring for adults with intellectual disabilities: Results of a cross-sectional, correlational-predictive research study. J. Appl. Res. Intellect. Disabil. 2019, 32, 1501–1513. [Google Scholar] [CrossRef] [PubMed]
- DeLucia, L.M.; Davis, E.L. Dental students’ attitudes toward the care of individuals with intellectual disabilities: Relationship between instruction and experience. J. Dent. Educ. 2009, 73, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Satchidanand, N.; Gunukula, S.K.; Lam, W.Y.; McGuigan, D.; New, I.; Symons, A.B.; Withiam-Leitch, M.; Akl, E.A. Attitudes of healthcare students and professionals toward patients with physical disability: A systematic review. Am. J. Phys. Med. Rehabil. 2012, 91, 533–545. [Google Scholar] [CrossRef] [PubMed]
- Shakespeare, T.; Iezzoni, L.I.; Grace, N.E. Disability and the training of health professionals. Lancet 2009, 374, 1815–1816. [Google Scholar] [CrossRef]
- Cashin, A.; Pracilio, A.; Buckley, T.; Kersten, M.; Trollor, J.; Morphet, J.; Howie, V.A.; Griffin, K.; Wilson, N.J. A survey of registered nurses’ educational experiences and self-perceived capability to care for people with intellectual disability and/or autism spectrum disorder. J. Intellect. Dev. Disabil. 2021, 1–13. [Google Scholar] [CrossRef]
- Cashin, A.; Pracilio, A.; Buckley, T.; Morphet, J.; Kersten, M.; Trollor, J.N.; Griffin, K.; Bryce, J.; Wilson, N.J. A cross-practice context exploration of nursing preparedness and comfort to care for people with intellectual disability and autism. J. Clin. Nurs. 2021. [Google Scholar] [CrossRef] [PubMed]
- Ankam, N.S.; Bosques, G.; Sauter, C.; Stiens, S.; Therattil, M.; Williams, F.H.; Atkins, C.C.; Mayer, R.S. Competency-based curriculum development to meet the needs of people with disabilities: A call to action. Acad. Med. 2019, 94, 781–788. [Google Scholar] [CrossRef] [Green Version]
- Gitlow, L.; Flecky, K. Integrating disability studies concepts into occupational therapy education using service learning. Am. J. Occup. Ther. 2005, 59, 546–553. [Google Scholar] [CrossRef] [Green Version]
- Peiris-John, R.; Jain, N.R.; Hogan, A.; Ameratunga, S. Educating health science students about disability: Teachers’ perspectives on curricular gaps. Disabil. Health J. 2021, 14, 100985. [Google Scholar] [CrossRef] [PubMed]
- Shields, N.; Taylor, N.F. Physiotherapy students’ self-reported assessment of professional behaviours and skills while working with young people with disability. Disabil. Rehabil. 2014, 36, 1834–1839. [Google Scholar] [CrossRef]
- Shields, N.; Taylor, N.F. Contact with young adults with disability led to a positive change in attitudes toward disability among physiotherapy students. Physiother. Can. 2014, 66, 298–305. [Google Scholar] [CrossRef] [Green Version]
- Teal, C.R.; Gill, A.C.; Green, A.R.; Crandall, S. Helping medical learners recognise and manage unconscious bias toward certain patient groups. Med. Educ. 2012, 46, 1365–2923. [Google Scholar] [CrossRef]
- Thompson, T.; Lamont-Robinson, C.; Williams, V. At sea with disability! Transformative learning in medical undergraduates voyaging with disabled sailors. Med. Educ. 2016, 50, 866–879. [Google Scholar] [CrossRef]
- Braun, A.T.; Clarke, V. Thematic Analysis: A Practical Guide, 1st ed.; Sage: Thousand Oaks, CA, USA, 2021. [Google Scholar]
- Braun, V.; Clarke, V. Reflecting on reflexive thematic analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Andrews, E.E. Disability models. In Practical Psychology in Medical Rehabilitation; Budd, M.A., Hough, S., Wegener, S.T., Stiers, W., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 77–83. [Google Scholar]
- Bronfenbrenner, U. Ecology of the family as a context for human development: Research perspectives. Dev. Psychol. 1986, 22, 723–742. [Google Scholar] [CrossRef]
- Tracy, S.J. Qualitative quality: Eight “big-tent” criteria for excellent qualitative research. Qual. Inq. 2010, 16, 837–851. [Google Scholar] [CrossRef] [Green Version]
- Yardley, L. Dilemmas in qualitative health research. Psychol. Health 2000, 15, 215–228. [Google Scholar] [CrossRef]
- Shafaroodi, N.; Kamali, M.; Parvizy, S.; Mehraban, A.H.; O’Toole, G. Factors affecting clinical reasoning of occupational therapists: A qualitative study. Med. J. Islam. Repub. Iran 2014, 28, 8. [Google Scholar] [PubMed]
- Stineman, M.G.; Rist, P.M.; Burke, J.P. Through the clinician’s lens: Objective and subjective views of disability. Qual. Health Res. 2009, 19, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Rochford, T. Whare tapa whā: A mäori model of a unified theory of health. J. Prim. Prev. 2004, 25, 41–57. [Google Scholar] [CrossRef]
- Hickey, H.; Wilson, D. Whānau hauā: Reframing disability from an indigenous perspective. Mai J. 2017, 6, 82–94. [Google Scholar] [CrossRef] [Green Version]
- Akobirshoev, I.; Mitra, M.; Li, F.; Dembo, R.; Dooley, D.; Mehta, A.; Batra, N. The compounding effect of race/ethnicity and disability status on children’s health and health care by geography in the united states. Med. Care 2020, 58, 1059–1068. [Google Scholar] [CrossRef] [PubMed]
- Sue, S. Cultural competency: From philosophy to research and practice. J. Community Psychol. 2006, 34, 237–245. [Google Scholar] [CrossRef]
- Eddey, G.E.; Robey, K.L. Considering the culture of disability in cultural competence education. Acad. Med. 2005, 80, 706–712. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.T.; Roth, J.J.; Okoro, O.; Kimberlin, C.; Odedina, F.T. Disability in cultural competency pharmacy education. Am. J. Pharm. Educ. 2011, 75, 26. [Google Scholar] [CrossRef] [Green Version]
- Hoang, L.; LaHousse, S.F.; Nakaji, M.C.; Sadler, G.R. Assessing deaf cultural competency of physicians and medical students. J. Cancer Educ. 2011, 26, 175–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrison, T.C.; Kahn, D.L. Disability rites: The cultural shift following impairment. Fam. Community Health 2004, 27, 86–93. [Google Scholar] [CrossRef]
- Symons, A.B.; McGuigan, D.; Akl, E.A. A curriculum to teach medical students to care for people with disabilities: Development and initial implementation. BMC Med. Educ. 2009, 9, 78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amosun, S.L.; Volmink, L.; Rosin, R. Perceived images of disability: The reflections of two undergraduate medical students in a university in south africa on life in a wheelchair. Disabil. Rehabil. 2005, 27, 961–966. [Google Scholar] [CrossRef] [PubMed]
- Wozencroft, A.J.; Pate, J.R.; Griffiths, H.K. Experiential learning and its impact on students’ attitudes toward youth with disabilities. J. Exp. Educ. 2014, 38, 129–143. [Google Scholar] [CrossRef]
- Anderson, E.S.; Smith, R.; Thorpe, L.N. Learning from lives together: Medical and social work students’ experiences of learning from people with disabilities in the community. Health Soc. Care Community 2010, 18, 229–240. [Google Scholar] [CrossRef]
- Jones, J.; McQueen, M.; Lowe, S.; Minnes, P.; Rischke, A. Interprofessional education in Canada: Addressing knowledge, skills, and attitudes concerning intellectual disability for future healthcare professionals. J. Policy Pract. Intellect. Disabil. 2015, 12, 172–180. [Google Scholar] [CrossRef]
- Szumski, G.; Smogorzewska, J.; Grygiel, P. Attitudes of students toward people with disabilities, moral identity and inclusive education—A two-level analysis. Res. Dev. Disabil. 2020, 102, 103685. [Google Scholar] [CrossRef]
- Martins, H.M.; Borges, M.L.; Gonçalves, T. Attitudes towards inclusion in higher education in a portuguese university. Int. J. Incl. Educ. 2018, 22, 527–542. [Google Scholar] [CrossRef]
- Moriña, A.; Sandoval, M.; Carnerero, F. Higher education inclusivity: When the disability enriches the university. High. Educ. Res. Dev. 2020, 39, 1202–1216. [Google Scholar] [CrossRef]
- Frank, H.; McLinden, M.; Douglas, G. Investigating the learning experiences of student physiotherapists with visual impairments: An exploratory study. Br. J. Vis. Impair. 2014, 32, 223–235. [Google Scholar] [CrossRef]
| Demographic Variable | Demographics | Number of Participants |
|---|---|---|
| Gender | Female | 8 |
| Male | 1 | |
| Year | 2nd | 1 |
| 4th | 8 | |
| Degree | MB ChB | 3 |
| BPhty | 3 | |
| BDS | 2 | |
| BPharm | 1 | |
| Previous higher education degree | Yes | 3 |
| No | 6 | |
| Previous life experiences with disabled people | Yes | 6 |
| No | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ravichandran, S.; Calder, A.; Ingham, T.; Jones, B.; Perry, M. “Someone Like Anyone Else”: A Qualitative Exploration of New Zealand Health Professional Students’ Understanding of Disability. Disabilities 2022, 2, 131-144. https://doi.org/10.3390/disabilities2010011
Ravichandran S, Calder A, Ingham T, Jones B, Perry M. “Someone Like Anyone Else”: A Qualitative Exploration of New Zealand Health Professional Students’ Understanding of Disability. Disabilities. 2022; 2(1):131-144. https://doi.org/10.3390/disabilities2010011
Chicago/Turabian StyleRavichandran, Sadhana, Allyson Calder, Tristram Ingham, Bernadette Jones, and Meredith Perry. 2022. "“Someone Like Anyone Else”: A Qualitative Exploration of New Zealand Health Professional Students’ Understanding of Disability" Disabilities 2, no. 1: 131-144. https://doi.org/10.3390/disabilities2010011
APA StyleRavichandran, S., Calder, A., Ingham, T., Jones, B., & Perry, M. (2022). “Someone Like Anyone Else”: A Qualitative Exploration of New Zealand Health Professional Students’ Understanding of Disability. Disabilities, 2(1), 131-144. https://doi.org/10.3390/disabilities2010011









