The Toxicological and Pharmacological Evaluation of the Anacyclus pyrethrum Aqueous Extract: Implications for Medicinal and Therapeutic Applications
Abstract
1. Introduction
2. Results
2.1. Acute Toxicity
2.1.1. Lethal Dose 50 Estimation (LD50)
2.1.2. Histopathological Examination
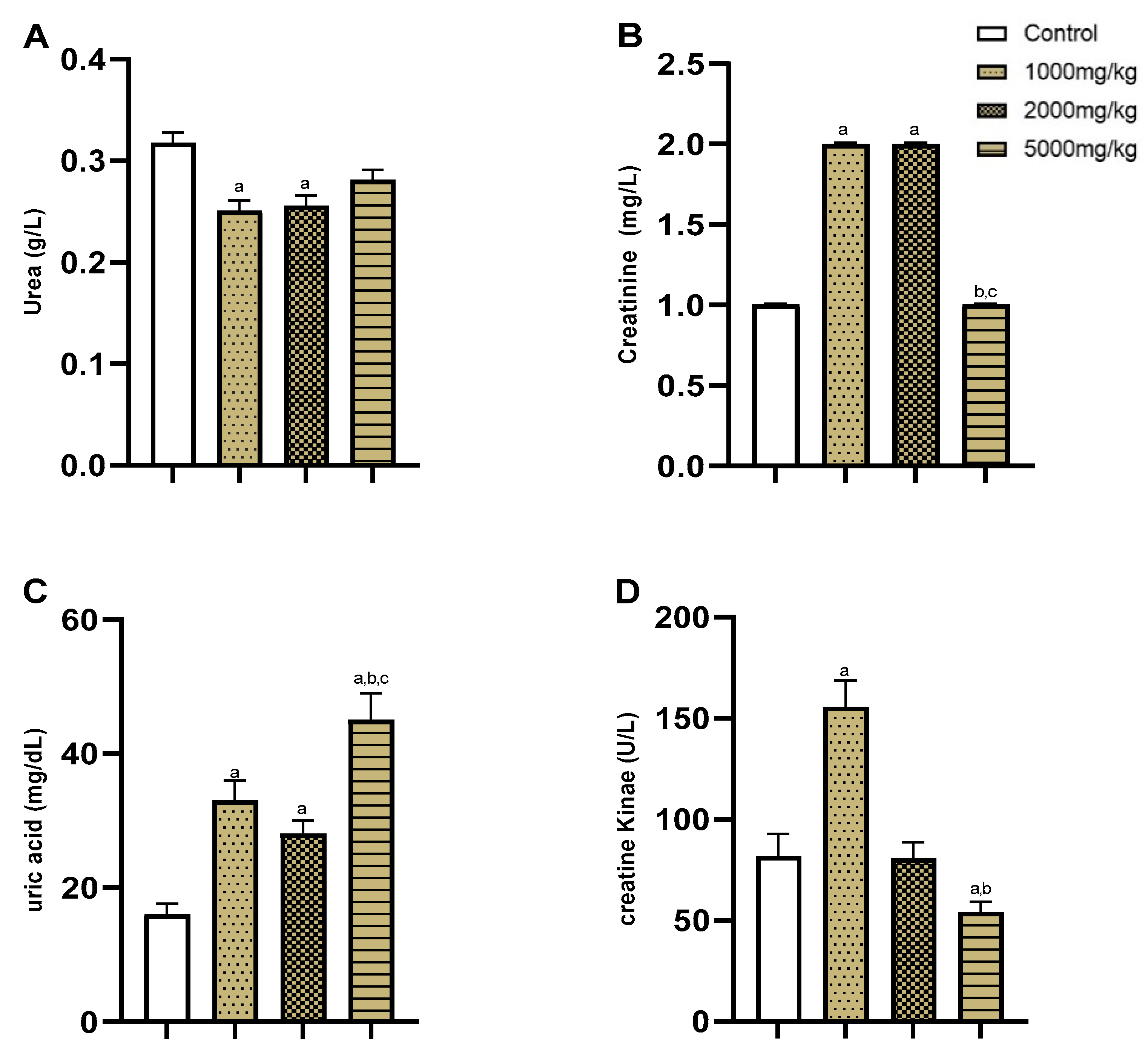
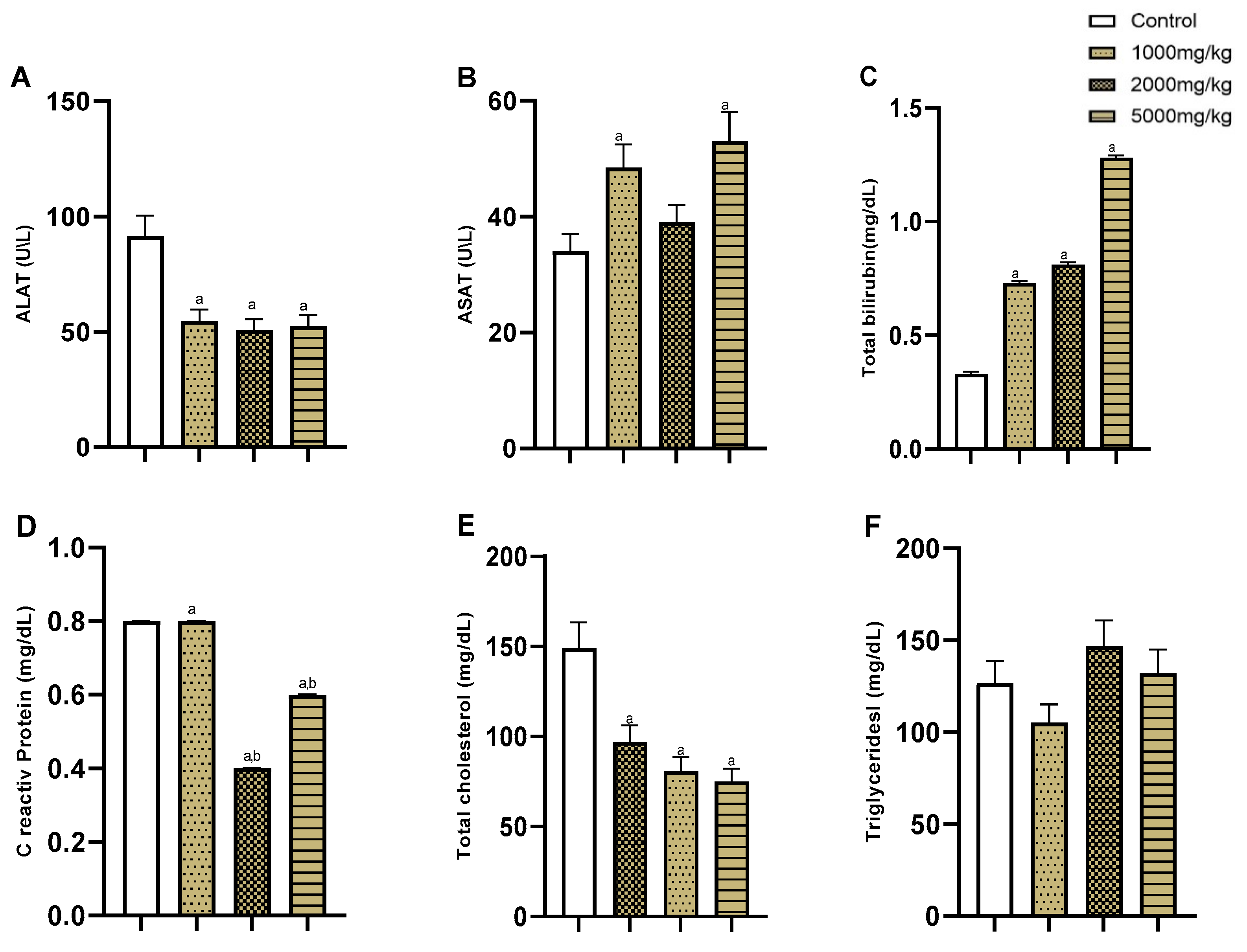
2.1.3. Biochemical Analyses
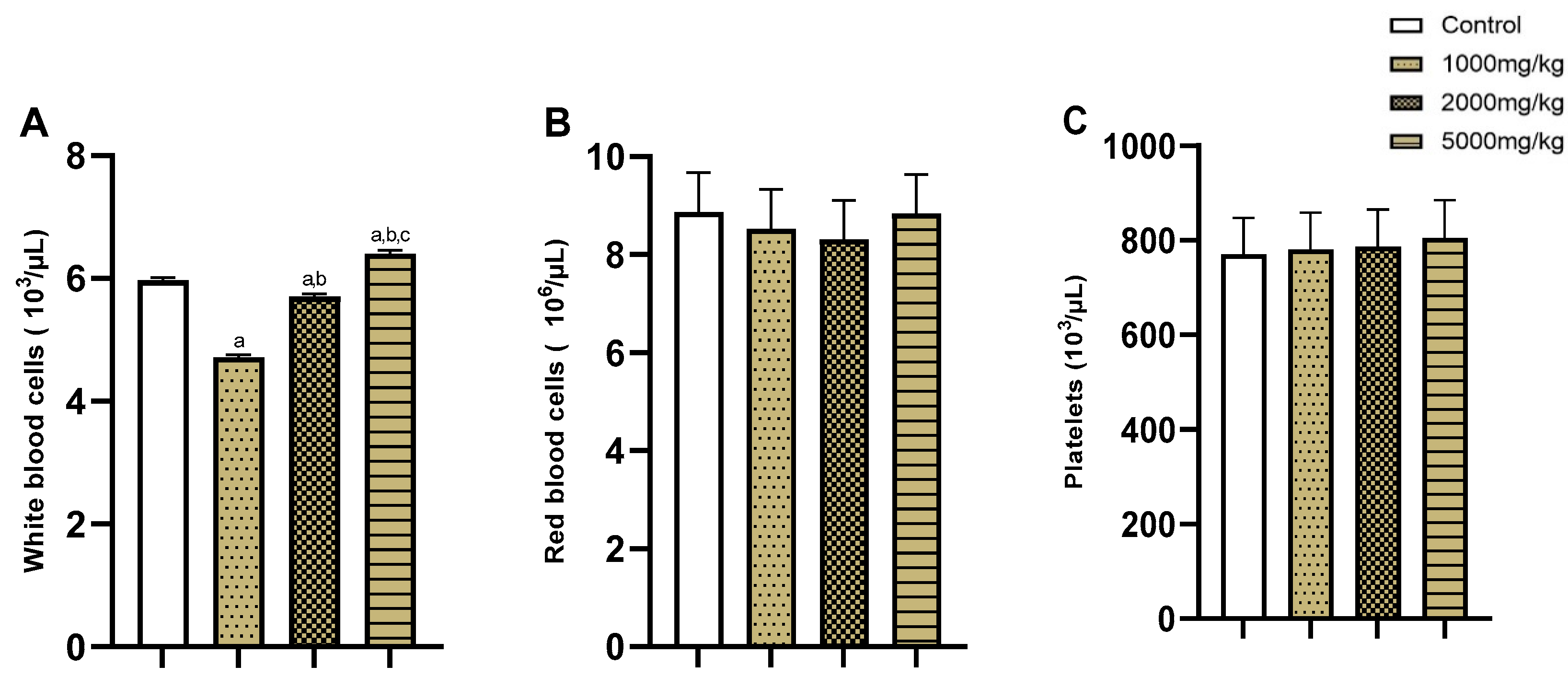
2.1.4. Hematological Analyses
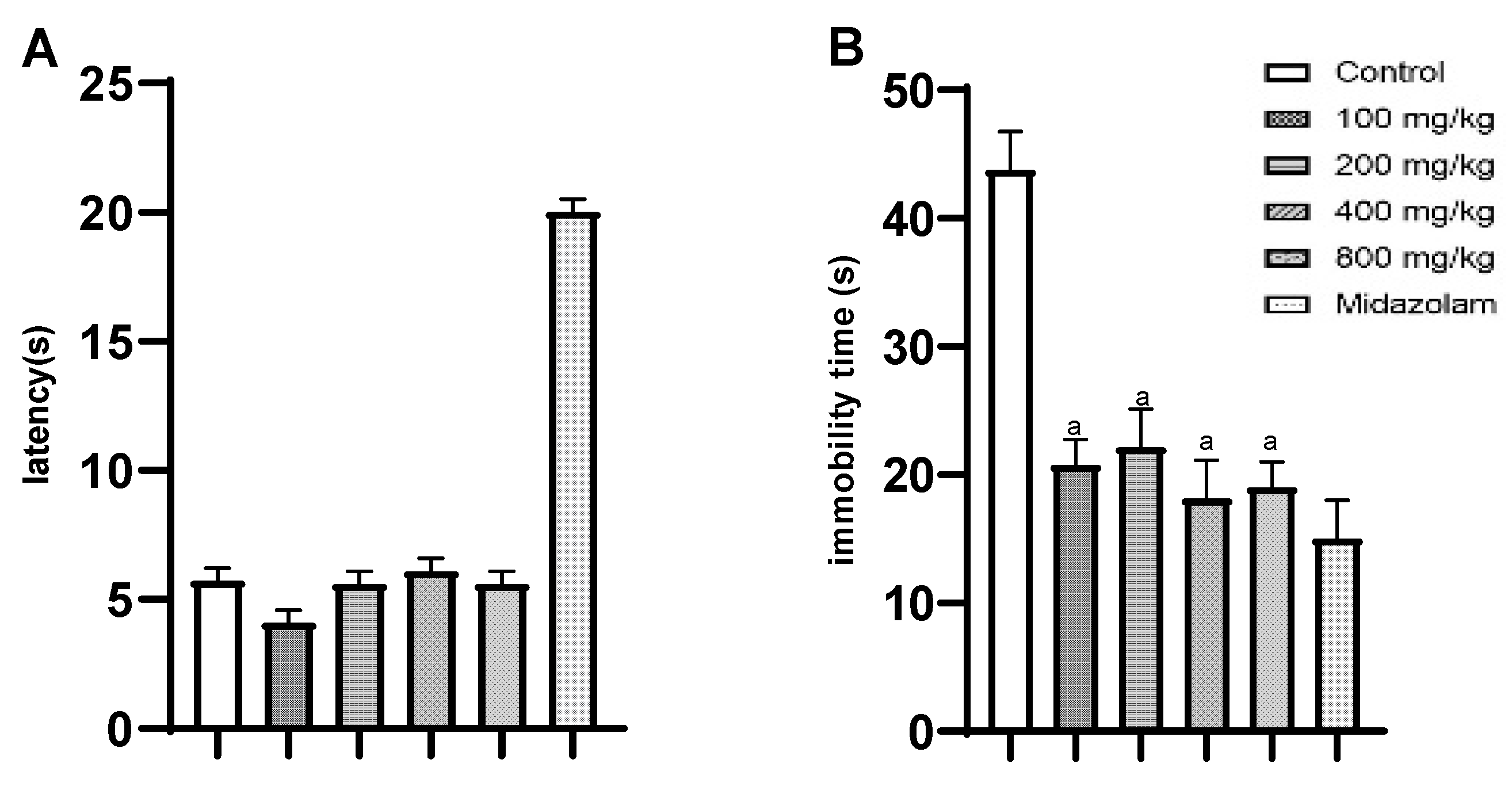
2.2. Pharmacological Effects
3. Discussion
4. Materials and Methods
4.1. Plant Samples and Extraction
4.2. Drugs
4.3. Animals
4.4. Acute Toxicity
4.4.1. Biochemical and Hematological Analyses
4.4.2. Histological Study
4.5. Pharmacological Effects
4.5.1. Forced Swim Test (FST)
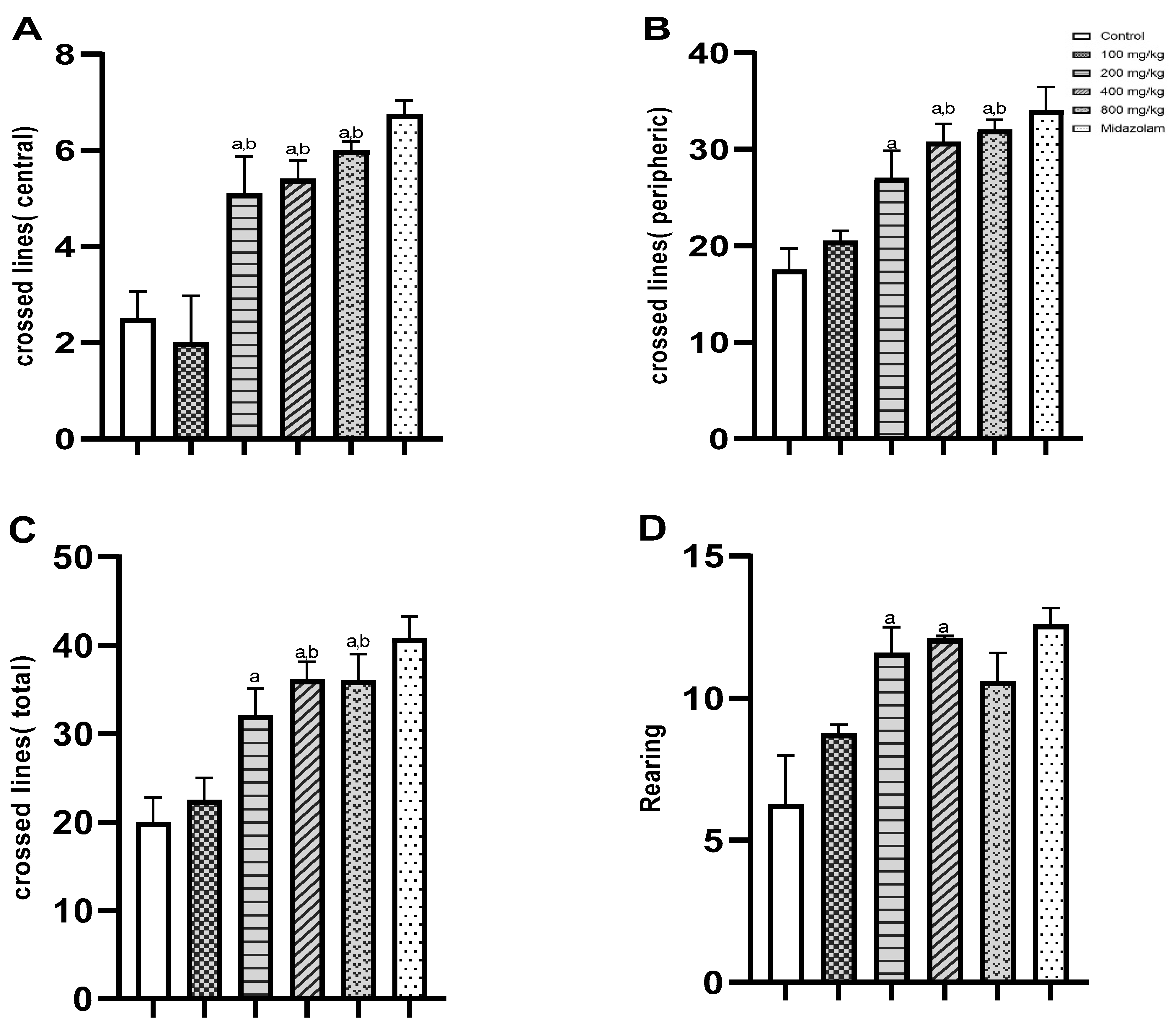
4.5.2. Open Field Test (OFT)
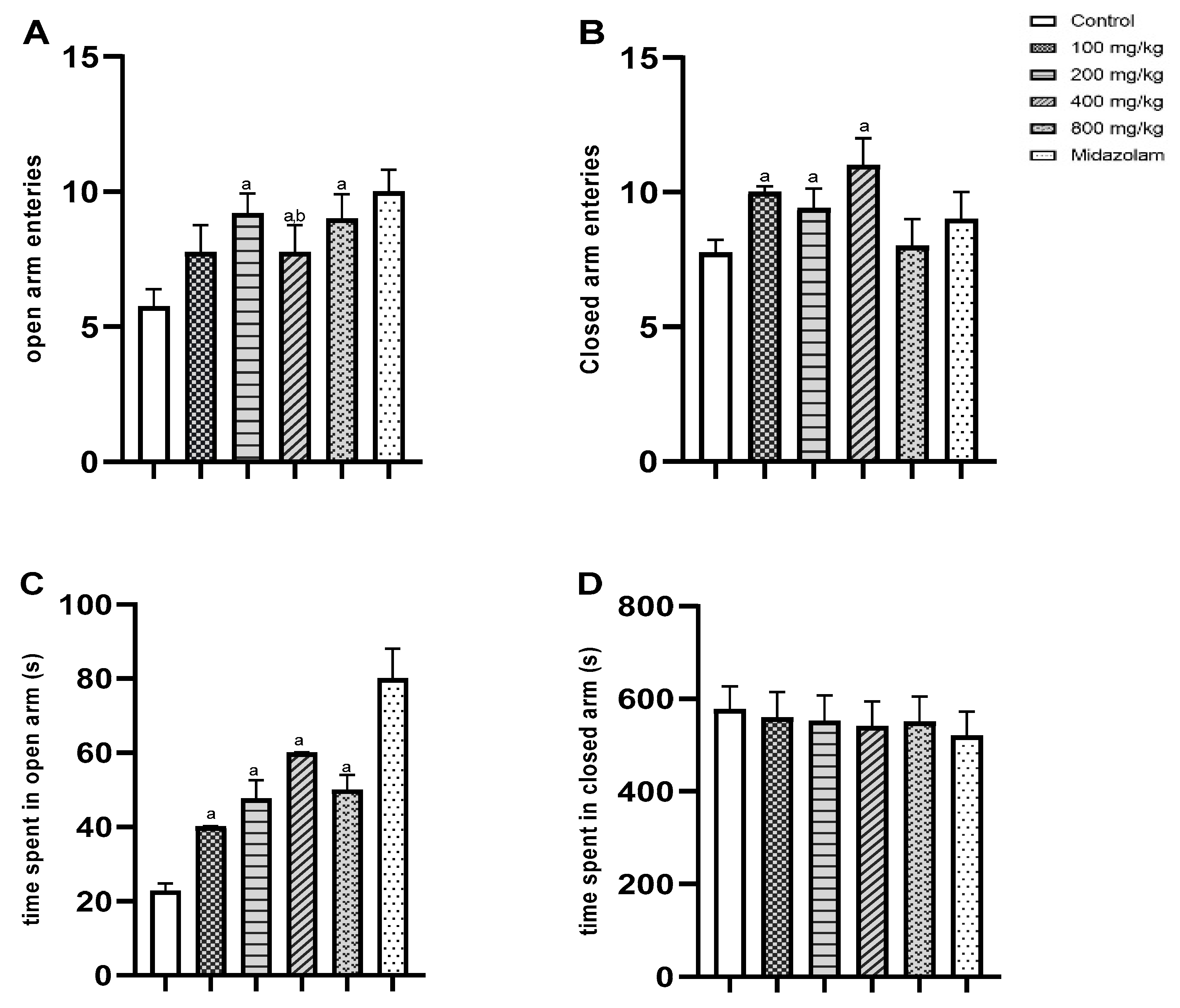
4.5.3. Elevated Plus Maze (EPM)
4.5.4. Hot Plate Test
4.6. Statistical Analyses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Samtiya, M.; Aluko, R.E.; Dhewa, T.; Moreno-Rojas, J.M. Potential Health Benefits of Plant Food-Derived Bioactive Components: An Overview. Foods 2021, 10, 839. [Google Scholar] [CrossRef]
- Atanasov, A.G.; Zotchev, S.B.; Dirsch, V.M.; Supuran, C.T. Natural products in drug discovery: Advances and opportunities. Nat. Rev. Drug. Discov. 2021, 20, 200–216. [Google Scholar] [CrossRef]
- Lee, E.L.; Barnes, J. Prevalence of Use of Herbal and Traditional Medicines. In Pharmacovigilance for Herbal and Traditional Medicines: Advances, Challenges and International Perspectives; Barnes, J., Ed.; Springer International Publishing: Cham, Switzerland, 2022; pp. 15–25. [Google Scholar] [CrossRef]
- Hamilton, A.C. Medicinal plants, conservation and livelihoods. Biodivers. Conserv. 2004, 13, 1477–1517. [Google Scholar] [CrossRef]
- Newmaster, S.G.; Grguric, M.; Shanmughanandhan, D.; Ramalingam, S.; Ragupathy, S. DNA barcoding detects contamination and substitution in North American herbal products. BMC Med. 2013, 11, 222. [Google Scholar] [CrossRef]
- Van Wyk, B.E. A review of commercially important African medicinal plants. J. Ethnopharmacol. 2015, 176, 118–134. [Google Scholar] [CrossRef]
- Bellakhdar, J. Contribution à l’étude de la Pharmacopée Traditionnelle au Maroc: La Situation Actuelle, les Produits, les Sources du Savoir (Enquête Ethnopharmacologique de Terrain Réalisée de 1969 à 1992); Université Paul Ver-laine: Metz, France, 1997; Available online: https://hal.univ-lorraine.fr/tel-01752084 (accessed on 3 August 2023).
- Ouarghidi, A.; Martin, G.J.; Powell, B.; Esser, G.; Abbad, A. Botanical identification of medicinal roots collected and traded in Morocco and comparison to the existing literature. J. Ethnobiol. Ethnomedicine 2013, 9, 59. [Google Scholar] [CrossRef]
- Elazzouzi, H.; Fadili, K.; Cherrat, A.; Amalich, S.; Zekri, N.; Zerkani, H.; Tagnaout, I.; Hano, C.; Lorenzo, J.M.; Zair, T. Phytochemistry, Biological and Pharmacological Activities of the Anacyclus pyrethrum (L.) Lag: A Systematic Review. Plants 2022, 11, 2578. [Google Scholar] [CrossRef]
- Anacyclus pyrethrum (L.) Link. Available online: https://www.gbif.org/fr/species/3148578 (accessed on 20 October 2023).
- Kalim, M.D.; Bhattacharyya, D.; Banerjee, A.; Chattopadhyay, S. Oxidative DNA damage preventive activity and antioxidant potential of plants used in Unani system of medicine. BMC Complement. Altern. Med. 2010, 10, 77. [Google Scholar] [CrossRef]
- Manouze, H.; Bouchatta, O.; Bennis, M.; Sokar, Z.; Ba-M’hamed, S. Anticonvulsive and neuroprotective effects of aqueous and methanolic extracts of Anacyclus pyrethrum root in kainic acid-induced-status epilepticus in mice. Epilepsy Res. 2019, 158, 106225. [Google Scholar] [CrossRef]
- Kumar, V.K.; Lalitha, K.G. Pharmacognostical Studies on the Root of Anacyclus pyrethrum DC; NISCAIR-CSIR: Delhi, India, 2012. [Google Scholar]
- Manouze, H.; Bouchatta, O.; Gadhi, A.C.; Bennis, M.; Sokar, Z.; Ba-M’hamed, S. Anti-inflammatory, Antinociceptive, and Antiox-idant Activities of Methanol and Aqueous Extracts of Anacyclus pyrethrum Roots. Front. Pharmacol. 2017, 8, 598. [Google Scholar] [CrossRef]
- Bezza, K.; Gabbas, Z.E.; Laadraoui, J.; Laaradia, M.A.; Oufquir, S.; Chait, A. Ameliorative potential of Anacyclus pyrethrum ex-tract in generalized seizures in rat: Possible cholinergic mediated mechanism. Bangladesh J. Pharmacol. 2019, 14, 188–195. [Google Scholar] [CrossRef]
- Bendjeddou, D.; Lalaoui, K.; Satta, D. Immunostimulating activity of the hot water-soluble polysaccharide extracts of Ana-cyclus pyrethrum, Alpinia galanga and Citrullus colocynthis. J. Ethnopharmacol. 2003, 88, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Kushwaha, M.N.; Jatav, V.S.; Pandey, S. Plant Anacyclus pyrethrum—A review. Res. J. Pharmacogn. Phytochem. 2012, 4, 164–170. [Google Scholar]
- Khare, C.P. Indian Medicinal Plants: An Illustrated Dictionary; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2008. [Google Scholar]
- Boonen, J.; Sharma, V.; Dixit, V.K.; Burvenich, C.; Spiegeleer, B.D. LC-MS N-alkylamide Profiling of an Ethanolic Anacyclus py-rethrum Root Extract. Planta Med. 2012, 80, 1787–1795. [Google Scholar]
- Baslam, A.; Aitbaba, A.; Aboufatima, R.; Agouram, F.; Boussaa, S.; Chait, A.; Baslam, M. Phytochemistry, Antioxidant Potential, and Antibacterial Activities of Anacyclus pyrethrum: Promising Bioactive Compounds. Horticulturae 2023, 9, 1196. [Google Scholar] [CrossRef]
- Usmani, A.; Khushtar, M.; Arif, M.; Siddiqui, M.A.; Sing, S.P.; Mujahid, M. Pharmacognostic and phytopharmacology study of Anacyclus pyrethrum: An insight. J. Appl. Pharm. Sci. 2016, 6, 144–150. [Google Scholar] [CrossRef]
- Ee, G.C.L.; Lim, C.M.; Rahmani, M.; Shaari, K.; Bong, C.F.J. Pellitorine, a Potential Anti-Cancer Lead Compound against HL60 and MCT-7 Cell Lines and Microbial Transformation of Piperine from Piper Nigrum. Molecules 2010, 15, 2398–2404. [Google Scholar] [CrossRef]
- David, D.J.; Gourion, D. Antidepressant and tolerance: Determinants and management of major side effects. L’Encephale 2016, 42, 553–561. [Google Scholar] [CrossRef]
- Slee, A.; Nazareth, I.; Bondaronek, P.; Liu, Y.; Cheng, Z.; Freemantle, N. Pharmacological treatments for generalised anxiety dis-order: A systematic review and network meta-analysis. Lancet 2019, 393, 768–777. [Google Scholar] [CrossRef]
- Fajemiroye, J.O.; da Silva, D.M.; de Oliveira, D.R.; Costa, E.A. Treatment of anxiety and depression: Medicinal plants in retro-spect. Fundam. Clin. Pharmacol. 2016, 30, 198–215. [Google Scholar] [CrossRef]
- Doudach, L.; Meddah, B.; Alnamer, R.; Chibani, F.; Cherrah, Y. In vitro antibacterial activity of the methanolic and aqueous ex-tracts of Anacyclus pyrethrum used in Moroccan traditional medicine. Int. J. Pharm. Pharm. Sci. 2012, 4, 4. [Google Scholar]
- Jawhari, F.Z.; El Moussaoui, A.; Imtara, H.; Mechchate, H.; Es-Safi, I.; Bouhrim, M.; Kharchoufa, L.; Miry, A.; Bousta, D.; Bari, A. Evaluation of the acute toxicity of the extracts of Anacyclus pyrethrum var. pyrethrum (L.) and Anacyclus pyrethrum var. depressus Maire in Swiss mice. Veter-World 2021, 14, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Thakur, M.; Chauhan, N.S.; Dixit, V.K. Immunomodulatory activity of petroleum ether extract of Anacyclus pyrethrum. Pharm. Biol. 2010, 48, 1247–1254. [Google Scholar] [CrossRef]
- Oanh, N.C.; Lam, T.Q.; Tien, N.D.; Hornick, J.L.; Ton, V.D. Effects of medicinal plants mixture on growth performance, nutrient digestibility, blood profiles, and fecal microbiota in growing pigs. Veter-World 2021, 14, 1894–1900. [Google Scholar] [CrossRef]
- Richelson, E. Pharmacology of antidepressants. Mayo Clin. Proc. 2001, 76, 511–527. [Google Scholar] [CrossRef] [PubMed]
- Badhe, S.R.; Badhe, R.V.; Ghaisas, M.M.; Chopade, V.V.; Deshpande, A.D. Evaluations of antidepressant activity of Anacyclus pyrethrum root extract. IJGP 2010, 4. Available online: https://www.greenpharmacy.info/index.php/ijgp/article/view/124 (accessed on 25 August 2023). [CrossRef]
- Millan, M.J.; Hjorth, S.; Samanin, R.; Schreiber, R.; Jaffard, R.; De Ladonchamps, B.; Veiga, S.; Goument, B.; Peglion, J.L.; Spedding, M.; et al. S 15535, a novel benzodioxopiperazine ligand of serotonin (5-HT)1A receptors: II. Modulation of hippocampal serotonin release in relation to potential anxiolytic properties. J. Pharmacol. Exp. Ther. 1997, 282, 148–161. [Google Scholar]
- Nishikawa, H.; Hata, T.; Itoh, E.; Funakami, Y. A role for corticotropin-releasing factor in repeated cold stress-induced anxiety-like behavior during forced swimming and elevated plus-maze tests in mice. Biol. Pharm. Bull. 2004, 27, 352–356. [Google Scholar] [CrossRef]
- Baslam, A.; Aitbaba, A.; Lamrani Hanchi, A.; Tazart, Z.; Aboufatima, R.; Soraa, N.; Ait-El-Mokhtar, M.; Boussaa, S.; Baslam, M.; Chait, A. Modulation of Gut Microbiome in Ecstasy/MDMA-Induced Behavioral and Biochemical Impairment in Rats and Potential of Post-Treatment with Anacyclus pyrethrum L. Aqueous Extract to Mitigate Adverse Effects. Int. J. Mol. Sci. 2023, 24, 9086. [Google Scholar] [CrossRef]
- Farhoosh, R.; Johnny, S.; Asnaashari, M.; Molaahmadibahraseman, N.; Sharif, A. Structure–antioxidant activity relationships of o-hydroxyl, o-methoxy, and alkyl ester derivatives of p-hydroxybenzoic acid. Food Chem. 2016, 194, 128–134. [Google Scholar] [CrossRef]
- Na Yin, Z.; Wu, W.J.; Sun, C.Z.; Liu, H.F.; Chen, W.B.; Zhan, Q.P.; Lei, Z.G.; Xin, X.; Ma, J.J.; Yao, K.; et al. Antioxidant and Anti-inflammatory Capacity of Ferulic Acid Released from Wheat Bran by Solid-state Fermentation of Aspergillus niger. Biomed. Environ. Sci. 2019, 32, 11–21. [Google Scholar]
- Sarı, A.; Şahin, H.; Özsoy, N.; Özbek Çelik, B. Phenolic compounds and in vitro antioxidant, anti-inflammatory, antimicrobial activities of Scorzonera hieraciifolia Hayek roots. S. Afr. J. Bot. 2019, 125, 116–119. [Google Scholar] [CrossRef]
- Kilani-Jaziri, S.; Mokdad-Bzeouich, I.; Krifa, M.; Nasr, N.; Ghedira, K.; Chekir-Ghedira, L. Immunomodulatory and cellular anti-oxidant activities of caffeic, ferulic, and p-coumaric phenolic acids: A structure–activity relationship study. Drug. Chem. Toxicol. 2017, 40, 416–424. [Google Scholar] [CrossRef] [PubMed]
- Elufioye, T.O.; Habtemariam, S.; Adejare, A. Chemistry and Pharmacology of Alkylamides from Natural Origin. Rev. Bras. Farmacogn. Orgao. Soc. Bras. Farmacogn. 2020, 30, 622–640. [Google Scholar] [CrossRef] [PubMed]
- Mijangos-Ramos, I.F.; Zapata-Estrella, H.E.; Ruiz-Vargas, J.A.; Escalante-Erosa, F.; Gómez-Ojeda, N.; García-Sosa, K.; Cechinel-Filho, V.; Meira-Quintão, N.L.; Peña-Rodríguez, L.M. Bioactive dicaffeoylquinic acid derivatives from the root extract of Calea urticifolia. Rev. Bras. Farmacogn. 2018, 28, 339–343. [Google Scholar] [CrossRef]
- Miao, Y.L.; Guo, W.Z.; Shi, W.Z.; Fang, W.W.; Liu, Y.; Liu, J.; Li, B.W.; Wu, W.; Li, Y.F. Midazolam Ameliorates the Behavior Deficits of a Rat Posttraumatic Stress Disorder Model through Dual 18 kDa Translocator Protein and Central Benzodiazepine Receptor and Neuroster-oidogenesis. PLoS ONE 2014, 9, e101450. [Google Scholar] [CrossRef] [PubMed]
- Laboureyras, E.; Boujema, M.B.; Mauborgne, A.; Simmers, J.; Pohl, M.; Simonnet, G. Fentanyl-induced hyperalgesia and analgesic tolerance in male rats: Common underlying mechanisms and prevention by a polyamine deficient diet. Neuropsychopharmacology 2022, 47, 599–608. [Google Scholar] [CrossRef] [PubMed]
- OECD. Guidelines for the Testing of Chemicals. Acute Oral Toxicity—Acute Toxic Cl Method Test No-423; Organisation for Economic Co-Operation and Development (OECD): Paris, France, 2001. [Google Scholar]
- Malatesta, M. Histological and Histochemical Methods—Theory and Practice. Eur. J. Histochem. 2016, 60, 2639. [Google Scholar] [CrossRef]
- Porsolt, R.D.; Anton, G.; Blavet, N.; Jalfre, M. Behavioural despair in rats: A new model sensitive to antidepressant treatments. Eur. J. Pharmacol. 1978, 47, 379–391. [Google Scholar] [CrossRef]
- Gould, T.D.; Dao, D.T.; Kovacsics, C.E. The Open Field Test. In Mood and Anxiety Related Phenotypes in Mice: Characterization Using Behavioral Tests; Gould, T.D., Ed.; Humana Press: Totowa, NJ, USA, 2009; pp. 1–20. [Google Scholar]
- Rodgers, R.J.; Dalvi, A. Anxiety, defence and the elevated plus-maze. Neurosci. Biobehav. Rev. 1997, 21, 801–810. [Google Scholar] [CrossRef]
- Okolo, C.O.; Johnson, P.B.; Abdurahman, E.M.; Abdu-Aguye, I.; Hussaini, I.M. Analgesic effect of Irvingia gabonensis stem bark extract. J. Ethnopharmacol. 1995, 45, 125–129. [Google Scholar] [CrossRef] [PubMed]

| Control | 1000 mg/kg | 2000 mg/kg | 5000 mg/kg | |
|---|---|---|---|---|
| Body weight (g) | 30.4 ± 0.8 | 30.8 ± 1.3 | 28.9 ± 1.0 | 31.5 ± 1.2 |
| Relative organ weights (g/100 b.wt) | ||||
| Liver | 8.07 ± 0.5 | 7.00 ± 0.8 | 9.10 ± 0.6 | 7.46 ± 0.7 |
| Kidney | 0.58 ± 0.1 | 0.52 ± 0.2 | 0.48 ± 0.0 | 0.63 ± 0.2 |
| Brain | 1.30 ± 0.1 | 1.43 ± 0.1 | 1.50 ± 0.2 | 1.40 ± 0.1 |
| Spleen | 0.33 ± 0.02 | 0.33 ± 0.0 | 0.34 ± 0.0 | 0.35 ± 0.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baslam, A.; Aboufatima, R.; Kabdy, H.; Boussaa, S.; Chait, A.; Baslam, M. The Toxicological and Pharmacological Evaluation of the Anacyclus pyrethrum Aqueous Extract: Implications for Medicinal and Therapeutic Applications. Stresses 2024, 4, 79-93. https://doi.org/10.3390/stresses4010005
Baslam A, Aboufatima R, Kabdy H, Boussaa S, Chait A, Baslam M. The Toxicological and Pharmacological Evaluation of the Anacyclus pyrethrum Aqueous Extract: Implications for Medicinal and Therapeutic Applications. Stresses. 2024; 4(1):79-93. https://doi.org/10.3390/stresses4010005
Chicago/Turabian StyleBaslam, Abdelmounaim, Rachida Aboufatima, Hamid Kabdy, Samia Boussaa, Abderrahman Chait, and Marouane Baslam. 2024. "The Toxicological and Pharmacological Evaluation of the Anacyclus pyrethrum Aqueous Extract: Implications for Medicinal and Therapeutic Applications" Stresses 4, no. 1: 79-93. https://doi.org/10.3390/stresses4010005
APA StyleBaslam, A., Aboufatima, R., Kabdy, H., Boussaa, S., Chait, A., & Baslam, M. (2024). The Toxicological and Pharmacological Evaluation of the Anacyclus pyrethrum Aqueous Extract: Implications for Medicinal and Therapeutic Applications. Stresses, 4(1), 79-93. https://doi.org/10.3390/stresses4010005










