Abstract
Infertility has a remarkable global impact affecting approximately about 48 million couples worldwide. One of the most contended concerns in reproductive biology is the prospective influence of psychological stress on pregnancy rates. Individuals struggling to conceive face a stupendous amount of emotional turbulence and have a greater risk for psychological vulnerability. Both stress and infertility reinforce the impact of each other; hence, there exists a reciprocal relationship. Stress may be the major contributor to subsequent infertility. Infertility treatments may enhance stress levels as well as reduce treatment outcomes. The biological mechanisms that interlink stress and infertility are the outcome of the hormonal actions at the brain level, where they stimulate or suppress the hypothalamic-pituitary-adrenal axis (HPA) and have a potential influence on the secretion of the respective hormone by the reproductive organs and the pregnancy outcomes. Sex hormones play an essential role in reproductive biology as well as in general physiology where they generate the cycle and provide a potential environment for pregnancy. This article reviews the impact of stress on reproductive rates and the implications of sex hormones on infertility. Additionally, it suggests strategies to overcome the stress conditions and the scenarios that may lead to stress.
1. Introduction
Stress is an inevitable outcome of modern life which is expressed as an uncomfortable condition of mental and physiological arousal that people experience when they perceive a harmful or dangerous situation to their well-being [1]. With continuously changing lifestyles and social systems, the ability to deal with stress and limit its consequences is essential for living a balanced and healthy life [2]. The basis of the complexion, duration, and severity of stress responses can affect homeostasis and have various impacts on the body, including life-threatening effects and even death [3].
Infertility is one of the global health problems and the most distressing condition affecting about 186 million people [4] that may carry significant psychological trauma. Personal stress, pressure from marital relationships, and social networks for married couples’ further family functioning and educational level are negatively correlated with infertility [5]. Although not fatal, it has been described as a serious life-changing problem where one is unable to establish clinical pregnancy [6]. Behind the workup of infertility, traditionally, the female factor is considered the major driving force, and the malefactor is predicted to be 50% of the cause, with a peculiar contribution in 20% of instances [7,8]. In males and females, the influence of mental disorders is often considered the reason for idiopathic (unexplained) infertility including stress, depression, sleep, and eating disorders.
The knowledge of the relationship between stress and infertility is still not broadly accepted. However, it has been reported that stress is a common factor in the development of unexplained reproductive disorders [9]. The major drawback seems to be the hardship in administering the correlation between emotional factors and reproductive outcomes [4]. The inability to reproduce naturally can cause feelings of shame, guilt, and low self-esteem, thus increasing their psychological vulnerability, and these negative feelings may lead to varying degrees of depression, anxiety, distress, and a poor quality of life. This review focuses on elucidating the knowledge of the impact of stress on infertility or reproductive outcomes and the role of hormones in causing stress as well as affecting the fertility rate, which also includes various stress-related ailments that lead to infertility. International databases (PubMed, Scopus, Web of Science) and Google Scholar were searched for articles published from 2000 to February 2023. The search procedure was performed in English using keywords such as “stress”, “depression”, “infertility”, and “reproductive hormones”. The articles were evaluated in terms of their titles, abstracts, and full texts.
2. Possible Mediators of Infertility
Stress is always manifested as a phenomenon that fails to attain the genetic potential and to cope with the environment of any individual [10]. Indelible diagnosis and therapeutic methods may have a pessimistic impact on sexual lives and can also induce stress among infertile couples [4]. Acute stress and chronic stress are two distinct kinds of stress. Acute stress is generally present in times of emergency, such as fighting. The changes that occur in the structure and function of specific chemicals in the brain trigger the emotional cognitive system, leading us to make stress-coping judgments. As a result, acute stress is frequently beneficial to the body, and it also enhances resistance to infection and minimizes the ability of an individual to produce a powerful immunological reflex along with the subsequent rise in ailments [11,12]. However, chronic stress is extensively involved in the pathogenesis of various diseases, and it is now thought to include both professional stress and atypical adversity. It may cause sleeplessness, gastrointestinal issues, anxiety, and depression, as well as an increased risk of complications associated with cardiac, cancer, and mental illness in addition to adversely affecting fertility. It also hampers the process of immune cell migration to the site of inflammation or infection [4,11]. The primary cause of infertility is psychological stress, and it is often preventable. The other mediators reported are metabolic stress and oxidative stress, which are interlinked with psychological stress [13].
2.1. Psychological Stress
Psychological stress is common among infertile women, and it is often manifested as chronic stress. Untreated stress can interfere with the pregnancy success rate or persistence with fertility treatment. The psychological stress that leads to a cytokine storm induces, in turn, oxidative stress which may trigger disruptions in the blood–testis barrier and lead to abnormal semen characteristics [14]. It causes a delay in attempting fertility that has a negative impact on the couple’s fecundity. The disputing psychological stress is reported as the major reason for severe reductions in testicular function leading to infertility [15]. Moreover, psychological stress is shown to be associated with high levels of female infertility that establish greater levels of undesirable pregnancy which includes repeated implantation failure and miscarriage. Psychological distress has a high probability of directly causing endometrial dysfunction by disrupting the secretion and regulation of endometrial hormones [16]. Prolonged psychological distress leads to a higher rate of discontinuous medically assisted reproduction. The vital environmental factor which adversely influences fertility is psychological stress which is associated with multiple health consequences and is considered to be a chronic experience of stress causing infertility [17].
2.2. Emotional Stress
Emotional stress is another major consequence of infertility, and it is broadly accepted [18]. Many men and women experience emotional suffering as a result of failure to conceive. Various reports establish a relationship manifested as a vicious cycle where infertility results in emotional stress, and that can promptly impact fertility by modifying hypothalamic-pituitary pathways, or it may cause tubal spasm dyspareunia, decreased male libido, and frigidity [19,20]. Despite the lack of biological reports regarding the biological relationship between emotional stress and infertility, rigorous care should be taken. Maternal stress is widely blamed for infertility due to miscarriages, late pregnancy problems, and decreased fetal development. Reducing the burden of infertility on women would not only stress the overall stress but also aid in no biologic ways to improving pregnancy chances [18].
2.3. Metabolic Stress
In recent years, the assessment of metabolic risk factors is considered highly essential for understanding reproductive disorders, especially since it may contribute in figuring out the cause behind idiopathic infertility, which might help in enhancing fertility treatment outcomes. Metabolic stress is an underlying cause of various metabolic disorders including obesity, osteoporosis, amenorrhea, or athlete triad (an eating disorder that leads to being underweight) [21]. The imbalance between reproduction and metabolism is mainly due to PCOS which often leads to ovarian dysfunction; further, it causes metabolic syndrome in females. Obesity can contribute to and cause permanent female infertility, and a higher BMI causes a potential reduction in serum adiponectin levels and elevation of insulin, which triggers hyperandrogenemia, inducing the risk of menstrual irregularity, PCOS, acne, and hirsutism. Women with greater BMI exhibit lower fecundity despite many ART treatment cycles [22,23]. The female with athlete triad experiences menstrual dysfunction which is accompanied by the risk of infertility [24].
2.4. Oxidative Stress
An imbalance in Oxidative stress may cause a serious effect on female reproduction and female reproductive ailments such as PCOS, endometriosis, preeclampsia, etc. [25]. The disproportion in equilibrium between reactive oxygen species (ROS) and antioxidant causes peroxidative damage to sperm motility due to scrotal heat, metabolite reflux, and testicular hypoxia. Oxidative stress is also caused by various metals, organic solvents, and ionizing radiation [26]. Oxidative stress can cause or worsen obesity, insulin resistance, vitamin D deficiency, and immune dyscrasia in PCOS physiopathology which is a remarkable risk factor for infertility [27]. Several cellular mechanisms are regulated by oxidative stress. The expression and secretion of sex hormone-binding globulin are inhibited by oxidative stress, by down regulating the HNF-4α in vitro, and this may be an essential factor in promoting hyperandrogenemia in PCOS. Abnormal levels of oxidative stress are found in women with PCOS that are independent of being overweight [28]. The oxidative stress is indicative of the functional efficacy inflammation markers such as resting level of seminal interleukin in men with impaired fertility [29].
2.5. Preconception Stress
Preconception stress is common among both men and women of reproductive age, and it may affect fertility, pregnancy, and neonatal outcomes. Every year, miscarriage pregnancies are accounted for about 23 million globally, resulting in 44 pregnancy losses each minute [30,31]. Preconception stress can be due to marital conflict, difficult bereavement, or any other psychiatric disorders [32]. Routine screening of the paternal parent’s mental health is essential to prevent the impact of the maternal parent’s depression on the child. Stress can disrupt the functions of the HPG axis which results in a reduction in the process of steroidogenesis and spermiogenesis, which may also provoke the chance of infection and inflammation and worsen semen quality [33]. Maternal stress is highly responsible for adverse pregnancy outcomes such as preterm birth, miscarriages, minimum development for gestational age, and low birth weight [34].
3. Reproductive Hormonal Changes during Stress and Infertility Conditions
Hormones administer and coordinate human sexual development, sexuality, reproduction, developmental plasticity, or phenotypic rearrangements that happen perpetually at the entire ontogeny including follicle formation and ovulation which involves hormones such as LH and Follicle-Stimulating Hormone (FSH), as their functions are illustrated in Table 1, together in distinct locations of the body, namely the hypothalamus, pituitary gland, and reproductive organs. An endocrine imbalance accounts for about 10% of the major causes of infertility [35]. During stress, hormone and acoustic tests revealed increased salivary cortisol levels and related alterations in voice pitch, vocal tract resonances (formants), and speech speed. The hormones that are generated in response to stressful conditions aid a depressed body setup that has the potential to cause long-term neuroendocrine changes that impact female fertility [10]. During the normal estrogen cycle, at the follicular phase, the hypothalamus secretes the regular standard outcome of gonadotropin-releasing hormone (GnRH); this results in the pituitary gland’s pulsatile secretion of luteinizing hormone (LH) release, and stress may induce abnormal hormonal production that may mislead the estrogen cycle and end up in failure in conception [36]. Under stress conditions, the serum level of hormones alters to adapt an individual to the persisting circumstances; however, long-term exposure to stress may lead to deleterious endocrine disorders that may have a negative influence upon conception [36].

Table 1.
Reproductive hormones and their generalized functions.
3.1. GnRh
In stressed conditions, the gonadotrophin-secreting hormone, which is the primary driver of reproductive function, is found in a reduced amount [37]. Neurons that are responsible for the synthesis of GnRH have a neural control point for modulating the reproductive function in vertebrates, and those neurons also highly represent the stress responses on reproduction since they are capable of monitoring the physiological status of the body [36]. Stress normally triggers the activation of the hypothalamus-pituitary-adrenal (HPA) axis as well as inhibits the hypothalamus-pituitary-gonadal (HPG) axis which is dealing with the secretion of GnRH. The stress may also interfere at any level of the HPG axis and may influence the reproductive function [38]. Impairment in gonadotropin production and its action results in a spectrum of changes such as relative or absolute LH and FSH deficit, which affects the gametogenesis process and steroid synthesis in gonads, lowering fertility and estradiol levels [37].
3.2. Inhibin
Inhibin is a gonadal hormone that exhibits a negative feedback mechanism on the FSH secretion which was excreted by the gonadotropin cells in the pituitary gland [37]. Following the separation of inhibin from porcine follicular fluid in 1986, activins were recognized as ovarian hormones, which increase pituitary gland FSH secretion. Activin A, in particular, was shown to be the isoform with the greatest physiological value in humans. The present understanding of activin A extends beyond the reproductive system, allowing it to be classified as a hormone, a growth factor, and a cytokine [39]. Various reports suggest that inhibin B is a potential biomarker for determining the oxidative stress in Sertoli cells which are the major production site of inhibin B [40].
3.3. Testosterone
Testosterone is an androgen that performs an essential function in the growth, reproduction, and maintenance of a healthy body. Sperm formation (spermatogenesis) is regulated by both endocrine and paracrine systems. FSH and LH are both involved in the endocrine stimulation of spermatogenesis and then work through the intermediate testosterone generated by the Leydig cells of the testis [41]. There are only a few reports which insist on the effect of stress on testosterone synthesis and male infertility. Psychological stress primarily reduces the serum testosterone level, followed by the secondary elicit of serum LH and FSH levels, which may have an impact on the semen quality by reducing the rate of motility, count, and normally functioning spermatozoa [42]. In accordance with the guidelines of the Endocrine Society, T replacement therapy is the standard treatment for men who suffer from symptomatic hypogonadism [43]. Intratesticular testosterone is also an important factor for the spermatogenesis process, virility, and male fertility. Testicular biopsy is the only way to measure intratesticular testosterone concentration, which is invasive and can lead to many complications [44]. A transdermal testosterone pretreatment may develop ovarian sensitivity for FSH levels. As well, in low-responder in vitro fertilization (IVF) individuals, gonadotropin therapy had increased follicular response. This perspective leads to higher levels of gonadotropin and increased follicular response compared to the mini-dose GnRH agonist protocol [45]. Few other research studies had reported that after 21 days of unintended chronic stress in adult male rats, reduced body weight, serum testosterone levels, and genital index were observed [37].
3.4. FSH
In both males and females, a dimeric glycoprotein gonadotropin hormone called FSH and its receptor play an essential function in the generation of follicles as well as in regulating the process of steroidogenesis in the ovary and spermatogenesis in the testis. It is generated by the anterior portion of the pituitary gland in various isoforms physiologically and targets the cells of gonads [27,46]. It coordinates its function with LH through G protein-coupled receptors (GPCRs) and alters steroidogenesis and cellular metabolism to regulate reproduction [47]. The interrupted secretion of these hormones by the pituitary glands will lead to infertility and testicular functional disruption. Furthermore, this gonadotropin deficiency stands as the major risk factor accounting for about 0.5% of men’s infertility. FSH interacts with its receptor on the Sertoli cells, triggering those cells in adults to secrete regulatory nutrients that are essential for germ cell maturation [47,48]. Furthermore, the circulating concentration of the germ cells directly depends on the volume of Sertoli cells [49]. It has been extensively employed in assisted reproductive technologies (ART) [50]. This hormone establishes its functionality upon binding to the receptors located in granulosa and Sertoli cells. Any polymorphism in the Follicle Stimulating Hormone Receptor gene figures out infertility in women. It may also lead to ovarian failure and primary or secondary amenorrhea [51]. The level of serum FSH has a significant correlation with stress. During psychologically stressful conditions, serum FSH was observed to lower, which may influence sperm motility and functioning [42].
3.5. LH
The production of LH is the cornerstone of the effective spermatogenesis process, secondary sexual characteristics, functions, and psychoactive and biosynthetic (anabolic) actions. Abnormalities in the function of LH can affect spermatogenesis, leading to infertility [49]. In men, in cases of infertility due to hypogonadotropic hypogonadism, sperm can be restored with HCG or human menopausal gonadotropins (hMG). The higher range of body mass index (BMI) will alter the concentrations of seminal plasma and male reproductive hormones, enhance oxidative stress, and affect sperm quality. These consequences may be linked with male infertility [52]. Longer duration of infertility, women’s age, and weight gain increase stress hormone levels, which exhibit decreased antioxidant activity that may lead to infertility [46]. For the first time, Gamma-aminobutyric acid (GABA) signaling in the MePD suppresses pulsatile LH secretion induced by psychological stress and suggests a functionally important MePD GABAergic projection to the hypothalamic GnRH pulse generator [53]. Chronic stress reduces kisspeptin content in the Anteroventral Periventricular Nucleus fetus and GnRH in the preoptic area in females and disrupts the LH surge, thereby disrupting the estrous cycle and fertility, leading to reduced pregnancy and embryo numbers [54]. p62 deficiency provides a new pathway, the GnRH-p62-OXPHOS (Ndufa2)-Ca2+/ATP-LH pathway, which on a theoretical basis exhibits the abnormal secretion of pituitary LH through OXPHOS signaling of mitochondria that may be a risk pathway for causing infertility in females [55].
3.6. Prolactin
Prolactin is a polypeptide hormone, an essential factor for male reproduction secreted by lactotrophs [56]. Treating prolactin elevation causes an affirmative metabolic effect on the patient, namely controlling glycemic content and other metabolic parameters [57]. Men experiencing long-term psychological stress have greater levels of prolactin which are not noticed in women [58]. Infertile men with oligo- and azoospermia, impaired movement, and hypogonadotropic hypogonadism have an extensively increased volume of serum prolactin levels as well as levels of seminal plasma. High prolactin in serum exhibits a chronic impact on the process of spermatogenesis in infertile men [59].
3.7. Estrogen
It has been debated for a long time that males also have the estrogen hormone. According to early studies, estrogen was harmful to male reproduction since the exogenous treatments led to abnormal developmental outcomes. Estrogen synthesis in the testis and elevated levels of 17-oestradiol in the testis fluid are recommended as an essential factor in healthy male reproduction, but they are still a controversy [60]. Based on the species, the receptors of estrogen such as estrogen receptors (ERs), ESR1 (ER-alpha), and ESR2 (ER-beta) are expressed in certain cells of the testis and also in the epididymal epithelium. Through the enzyme named aromatase, the testis secretes a crucial amount of this hormone [61]. In the human body, biologically active aromatase is expressed by Leydig cells, immature germ cells, and in spermatozoa. Additionally, ESR1 and ESR2 are found in spermatozoa and germ cells, and it is important to note that spermatozoa contain a truncated form of ESR1. These observations unmistakably imply that estrogens are probably involved at various stages of the development of male germ cells [62]. Historically, testosterone and estrogen were thought to be male and female sex hormones, respectively. However, estradiol, the most common type of estrogen, is also important in male sexual function. It is required in males to regulate libido, erectile function, and spermatogenesis [48]. Estrogen is crucial for different physiological functions, including controlling energy metabolism, mineral balance, stress responses, and sexual development [63]. It is a powerful vasodilator that increases blood flow in several organs throughout the body, with reproductive tissues, particularly in the uterus, experiencing the greatest effects [64].
3.8. Progesterone
Progesterone is the steroid hormone that plays a vital role in female reproductive function. It helps the mature ovary to get released into the uterus. During pregnancy, this hormone facilitates implantation and suppresses myometrial contraction to promote uterine growth. Physiological effects of progesterone hormone are particularly arbitrated by an intracellular progesterone receptor (PRs). The PR protein consists of a central globular DNA-binding domain (DBD), a C-terminal ligand-binding domain (LBD), and an amino-terminal domain (NTD) that is largely composed of intrinsically disordered (ID) protein [65]. This PR protein expressed in two isoforms—progesterone receptor-A and progesterone receptor-B—was identified in the 1970s [66]. The AF1 and AF2 are the two functional transcriptional domains located at PR. AF1 is found in NTD, and AF2 is found in LBD [65]. The expression of progesterone receptor-A is essential for the ovulatory function in response to progesterone, and in most cases, progesterone receptor-A inhibits the progesterone receptor-B. The PR-B is a strong co-activator that regulates the target gene response to progesterone [67]. The impaired PR endometrial expression during implantation leads to infertility [68]. The primary hormone during the luteal phase is progesterone. It is essential in both orchestrating the uterus for a prospective gestation and sustaining it. Because there is frequently a luteal phase shortfall in assisted reproduction therapies, it is vital to supplement this key period to get the greatest outcomes, not only for implantation but also for sustaining the pregnancy [69].
3.9. Anti-Mullerian Hormone (AMH)
The Anti-Mullerian hormone (AMH) is made of small developing follicles in the ovary produced by granulose cells [70]. It is a homodimer glycoprotein involved in transforming the growth factor-B (TGFB) super family [71] and is an outcome marker of the ovarian reserve pool belonging to chromosome 19 short arm [72]. It acts as momentum for the quantitative aspect of ovarian reserve constitutes by the quality and quantity of primordial follicles [73]. The primordial follicles undergo atresia by FSH after puberty when the HPG endocrine axis is activated [74]. It produces 140 kDa disulfide-linked homodimer covalently bonded as a monomer of 560 amino acids. AMH exists as an active form of C-terminal about 25 kDa dimer and N-terminal pro region about 110 kDa. It is known for its serum marker assessment of spectrum ovarian reserve and PCOS [75]. AMH provides two distinct receptors, AMHRI and AMHRII, involved in signal transmission relating Suppressor of Mothers Against Decapentaplegic (SMAD) proteins [73]. These receptors transduce intracellular signals effectively through nuclear and physiological binding to AMH, which exhibits an essential function of prenatal gonadal sex differentiation by developing mullerian ducts in males. During embryonic development by the eighth post-conception week, the AMH hormone is produced by immature Sertoli cells in the testes until the age of 2 years post-natal, which declines over pubertal years; then, ultimately, it becomes untraceable in adults due to high concentrations of testosterone. The lower devotion of AMH level in males leads to the growth of the male and female genitalia. In females, analyzing serum AMH levels with autoimmune disease associated with the possibility of infertility [72].
3.10. Prolactin
A polypeptide hormone prolactin is produced by the lactotrophs, a specialized cell of the anterior pituitary gland. Other than lactation during reproduction, it plays an important role in many homeostatic roles [56]. Transmembrane prolactin receptor (PRL-R)is involved in prolactin signaling which is expressed in a wide range of tissues [75]. The hormone prolactin plays an essential function in determining the pathogenesis of schizophrenia and related psychoses [76,77]. Prolactin is concluded as the remarkable marker for diagnosing stress [78]. During hypoglycemia, the prolactin levels are gradually raised, and symptomatic neuroglycopenia is achieved. During the period of pregnancy and lactation, a notable elevation in brain PRL-R expression has been expressed as well as a rise in prolactin gene expression in the hypothalamic region [79]. The adenohypophysis hormone prolactin facilitates adaptive behavior, induces analgesia, and enhances grooming behavior. It plays a protective role against biological modifications induced by stress. There might be a chance of a higher magnitude of increase in prolactin in women than in men, and this is dependent on estradiol levels [79].
3.11. Thyroid Hormones
The frequency of thyroid disease occurrence in females of fertile age has been categorized to be thyroid autoimmunity, hypothyroidism, and hyperthyroidism, wherein infertility is quite common in women with thyroid dysfunction relating to Graves and Hashimoto’s disease [80]. The association of thyroid-stimulating hormone (TSH) elevation and thyroid autoimmunity (TAI) links infertility with a low ovarian reserve pool [81]. The severity of thyroid dysfunction leads to menstrual disorders through the interactions with the hypothalamic-pituitary-ovarian axis by direct and indirect means [82]. The probability for the presence of TAI leads to infertility either by direct or indirect reflections of immune imbalance [83]. A female associated with infertility related to thyroid disorder is then first treated to normalize thyroid dysfunction, and the workout of infertility is resolved by ART treatment [84,85]. Thyroid hormone receptors are directly identified on the testis, located on Sertoli cells in seminiferous tubules [61,86]. Sertoli cells are known to be the first somatic cells in the testes to help in supporting and nurturing spermatogenesis where TR plays a vital role in mediating the thyroid hormone in sperm production [87]. Thyroid dysfunction causes several alterations in semen quality including the volume, density, motility, and morphology of sperm [39]. The elevation of thyroid dysfunction in the condition of hyperthyroidism creates a short period of proliferation in Sertoli cells and leads to a delay in spermatogenesis [88]. Hypothyroidism and hyperthyroidism changes spermatic production and characteristics by creating alterations in thyroid receptors, thus thyroid hormone imbalance may be involved in causative mechanism of male infertility [89]. Thyroid hormones (T3 and T4) are necessary for the healthy state and operation of the female conceptive system because they regulate ovarian, uterine, and placental tissue metabolism and development. As a result, in women as well as in animals, both hypo- and hyperthyroidism can cause sub-fertility or infertility. Menstrual irregularity, anovulation, premature birth, preeclampsia, restriction in the growth of intrauterine, postpartum thyroiditis, and mental impairment in children are all well-documented consequences of maternal thyroid dysfunction [48].
4. Various Biological Mechanisms Related to Stress That Leads to Infertility
Stress has a negative impact on reproduction; nevertheless, the mechanism behind this is not well understood. Cadmium build-up to generate free radicals Cd2+ is a complex II non-competitive inhibitor, resulting in semi-ubiquinone reduction which is reactive and unstable, and it may produce necrosis and apoptosis by inducing a long-term production of ROS [90]. This may also result in infertility or poor pregnancy outcomes due to high levels of ROS and poor antioxidants, likely glutathione, that affect the entire life of men and women [10,91]. Through the mechanisms of alpha-amylase activity, using amylase salivary concentrations via the sympathetic-adreno-medullary (SAM) axis reduces fertility by interacting with catecholamine receptors, changing blood flow via the fallopian tubes and gamete transfer [92]. DNA damage caused by oxidative stress is a major cause of sperm dysfunction, leading to congenital malformations and complex neuropsychiatric disorders [93]. Due to low antioxidants, spermatozoa are sensitive to DNA damage. ROS-mediated sperm destruction is key for sperm mobility and the embryo’s paternal genetic contribution, which creates a link between seminal leukocytes and ROS generation. Thus, ROS is inversely connected with sperm DNA integrity. Superoxide dismutase (SOD) is an enzymatic antioxidant, which protects against oxidative stress, a relationship between low seminal catalase activity and male infertility, and the other antioxidant glutathione peroxidase (GPX) with mercapto-succinate causes a significant increase in sperm lipid peroxidation [94]. The inflammatory response deposition under Th1-lymphocyte and M1-macrophage responses regulates cytokines, adipokines, and myokines which are obesity-related inflammatory responses that disrupt the hypothalamic-pituitary-gonadal (HPG) axis preventing the release of hypothalamic GnRH and subsequent release of FSH and LH [95] that might cause intracellular oxidative damage to spermatozoa via increased lipid peroxidation. Thus, the excess formation of ROS affects reproduction [96]. Cortisol, a stress hormone, may inhibit estradiol-17 production in the ovary, resulting in amenorrhea, anovulation, and menstrual abnormalities as a result of stress [97]. Human and animal reproductive activities are primarily governed by the HPG axis as illustrated in Figure 1, and reduced GnRH action in both males and females, resulting in lower gonadotropin levels operating stress-related variables [98]. h various fertility medicines, however, is just Nutritionally induced oxidative stress consists of excessive macronutrient intakes that might cause oxidative stress that may favor inflammation via NF-B-driven cell signaling pathways [99] and make a response to several consequences such as nutritional deficiency, viral infection, and genotoxic stress [100]. The equilibrium shifts towards an excess of ROS, and oxidative stress occurs, which can cause oocyte aging and reduce oocyte number and quality [101]. It can also cause embryo fragmentation and the emergence of a variety of developmental defects and is thought to be one of the major causes of spontaneous and recurrent miscarriage [102]. Reproductive illness due to ROS leads to polycystic ovary syndrome (PCOS), endometriosis, and pre-eclampsia [103]. Pre-eclampsia is linked to fetal morbidity and death, monitored using a valid indicating marker, F2-isoprostanes [104,105]. Endometriosis and pre-eclampsia can impair embryo implantation by stimulating the surge of reactive oxygen and nitrogen species [106]. The microbiota is referred to as a group of microorganisms for the physiological process of the host present in mucosal tissues of the gut, reproductive tract, and skin [107]. The microbiota is very important for sustaining the mucosal barrier structural integrity, pathogen refuge, and immunomodulation [108]. The convulsion in microbiota leads to a decrease in the ratio of pathogenic organisms and a reduction in entire microbial diversity [109]. The gut and intestinal microbiota may affect male and female fertile capability through the impact on inflammatory conditions [110]. Oxidation of glyceraldehyde-3-phosphate dehydrogenase (GAPDH-S) resulting in H2O2 generation has been reported to reduce sperm motility and inhibit GAPDH-S activity [111].
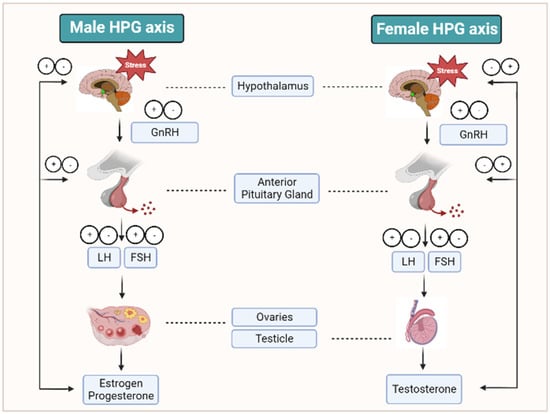
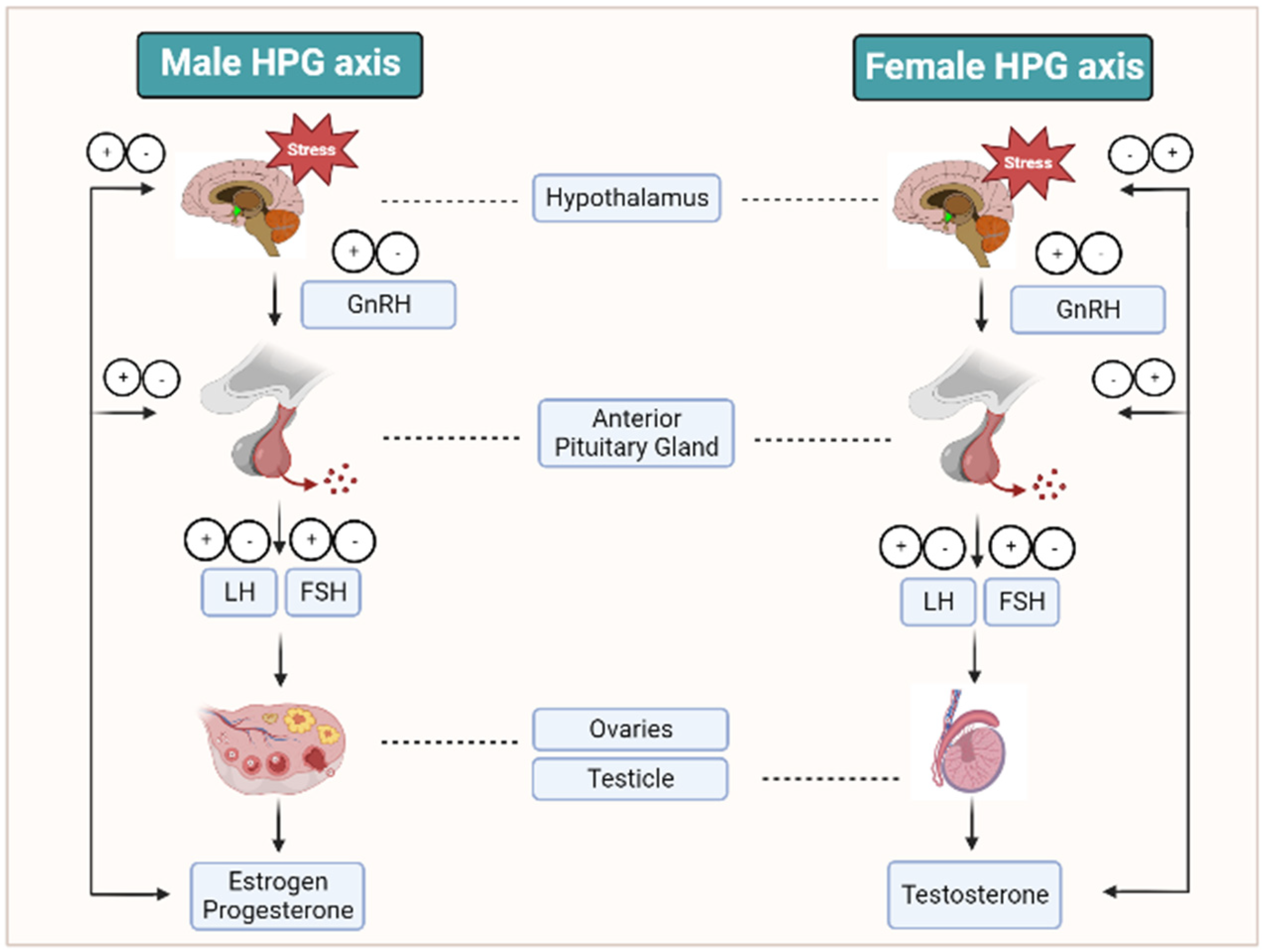
Figure 1.
HPG axis and the reproductive hormones under stress conditions. This figure illustrates that at prolonged stress conditions, the HPG axis produces increased or decreased quantities of hormones that lead to hormonal imbalance, which is associated with the major risk factor PCOS, and this ultimately leads to infertility.
5. Stress and Other Reproductive Ailments
Varicocele, metabolic syndrome, sexually transmitted diseases, tobacco use, alcohol, bacterial prostatitis, microbial infections, mutations, and viral infections are all potential causes of OS and inflammation [112]. Furthermore, increases in sperm quality following varicocelectomy may not always result in spontaneous conception [113]. Stress factors and their relative mechanisms may also cause immune dysregulation in reproductive health [114]. Physical and emotional stress may lead to pubescence, and, at the reproductive stage, they may cause impaired oogenesis and spermatogenesis resulting in transitory sterility in women and permanent infertility in males, respectively. Corticotrophin-releasing hormone (CRH) found in both male and female reproductive systems serve as an autocrine and paracrine modulator that has participated in the regulation of steroidogenesis and the inflammatory processes of the ovary, the endometrium, and placental CRH [115]. Abnormal CRH may cause various conditions including preeclampsia, endometrial growth retardation, abnormal placenta invasion, and preterm delivery [116]. Long-term inhibition of the metabolism by increased activation of glucocorticoid secretion in stress leads to persistent reproductive dysfunction [117]. Melatonin, an important factor of reproduction, attenuates and counteracts oxidative stress. It acts as a scavenger for ROS [118]. During stress, a variety of components of the HPA axis can suppress the activity of the HPG axis at distinct multiple levels. The HPG axis is regulated by a hypothalamic neuropeptide, gonadotropin-inhibitory hormone (GnIH), which is the key negative regulator of reproduction [119].
PCOS—Almost 7 to 15% of women belonging to the reproductive age are diagnosed with a metabolic gyne-endocrine disorder named PCOS [120,121]. It results in clinical hyperandrogenism, biological dysovulation, and infertility [122]. It is also associated with certain pathophysiological symptoms including glucose intolerance, diabetes mellitus, atherogenic dyslipidemia, systemic inflammation, non-alcoholic fatty liver disease, hypertension, coagulation disorders, severe acne, neuroendocrine alterations, hirsutism, insulin resistance, increased androgen, adiponectin levels, adiposity, menstrual irregularities, elevated endocrine, metabolic modifiers, and ovarian abnormalities [123,124]. In the case of PCOS, the OS index is high and is significant even after BMI adjustment. PCOS patients with lower BMI have lower emotional distress than obese patients [125,126]. Women with PCOS have abnormal biomarkers of OS and have lower amounts of antioxidants such as catalase and ferroxidase [127,128]. OS modifications with d-chiro-inositol, an isomer of inositol, vitamin D, and probiotic administration are effective beneficial strategies in reducing oxidative stress in PCOS women [129,130,131]. Depression is the most common effect found in patients with PCOS which has a serious effect on their quality of life [132]. It is three times more common in PCOS women than in non-PCOS women [133,134]. Depression is strongly associated with insulin resistance which serves as a physiological mediator [135]. Electro acupuncture is also a method of treatment provided to PCOS patients. It improves the symptoms of depression and people’s quality of life [136].
Endometriosis—A pathological condition that exhibits the presence of endometrial-like tissue around the uterus and triggers chronic inflammatory symptoms; most of the women affected are asymptomatic. About 35–50% of females affected with endometriosis are diagnosed with infertility [137]. OS is highly linked with the prognosis of endometriosis; OS and ROS production is found greater in endometriosis, and it reflects damage and proliferation. It also affects multiple physiological functions such as ovulation, implantation, oocyte maturation, luteolysis, and the maintenance of the luteal phase during pregnancy which partially reflects the infertility status [138]. Infertility caused by endometriosis can be treated by the supplementation of antioxidants such as Vitamin C and E, melatonin, etc. [139]. In endometriosis, individuals correlated with infertility have impaired secretion of gonadotropin hormones, which is proportional to the disease severity [140].
6. Impact of Stress on Infertility Treatment
Fortunately, major advancements in the medical and surgical treatment of infertility have lately been developed. The total increased risk associated with various fertility medicines, however, is just 1–2% [141]. PCOS is the greatest prevalent condition of anovulatory infertility. It is treated with various medications; oral ovulation induction medications are the first-line pharmacological therapy for women with the condition who are unable to conceive. Clomiphene citrate is the most well-established therapy, while aromatase inhibitors have shown promise, although efficacy has yet to be verified in randomized controlled trials [142]. Repeated clomiphene medication may be linked to an increased incidence of hypospadias and neural tube abnormality [143]. Patients with PCOS who were clomiphene-resistant showed lower antioxidant levels than the people who were clomiphene sensitive but did not have PCOS. Myeloperoxidase levels followed the same pattern, which might be explained by a compensatory mechanism [127]. Females with PCOS have increased levels of inflammatory markers as well as lower levels of antioxidants. N-acetylcysteine appears to be effective in restoring oxidative equilibrium and fostering high-quality oocytes with optimal follicular size. It also boosts ovulation and conception rates while having fewer negative effects including ovarian hyperstimulation syndrome, which is frequent with other drugs [144]. Premature ovarian insufficiency (POI) affects at least 1% of all women and creates long-term health issues as well as psychological stress. POI-induced infertility was once thought to be absolute, with infertility therapy having little or no efficacy. In general, it has been assumed that medicine can only give little assistance to these individuals [141].
7. Factors That Cause Decreased Infertility Rate
In these modern days, infertility has become the most prevalent health issue, and it has been impacted by various risk elements including lifestyle habits, diet, environment, stress, and endocrine disruptors. The great attention to quality-of-life choices such as food habits, stress, drinking, smoking, and obesity affects the physiology of an individual and exerts long-term effects [145]. Healthy lifestyle behaviors from preconception through postpartum are regarded as an important precaution for attaining healthy pregnancies and avoiding gestational disorders. Healthy diet control, BMI control, physical exercise, and physical, mental, and emotional health are among the World Health Organization’s (WHO) preconception priorities [146].
7.1. Nutrition
A healthy diet is opulent in carbs, fiber, fruits, and vegetables, and folate is linked to enhanced sperm quality [147]. Another possible benefit might be antioxidants, which are majorly essential for sperm capacitation and perform a crucial in ROS scavenging activity, where ROS overloading might cause sperm malfunction and affect its motility, damage DNA, and lower its membrane integrity. The antioxidants aid in the removal of excess ROS or convert ROS into molecules that are less harmful to cells. It is recommended to have a diet rich in antioxidants [148].
7.2. Smoking
Usage of tobacco causes exposure to about 4700 mutagenic substances such as hazardous chemicals and polycyclic aromatic hydrocarbons which lead to oxidative stress in the testes that affects spermatogenesis and steroidogenesis and results in poor chromatin condensation, DNA integrity, oocyte binding, and epigenetic alterations [149].
7.3. Caffeine Consumption
Caffeine usage is associated with elevated levels of testosterone as well as the sex hormone binding globulin (SHBG). It alters the crucial properties of Sertoli cells which include the glycolytic and oxidative properties that may impair reproductive ability in men. In embryos as well as in adults, caffeine can modify the hormonal system and has a modifying influence on the germinative epithelium [150].
7.4. Gadgets
The increased use of mobile phones, as well as the storing of phones in trouser pockets, has been identified as a source of harmful radiation to the male reproductive system. A recent study found that DNA fragmentation was the only variable that changed among mobile phone users with high usage (>4 h daily) who kept their phone in their trouser pocket [151]. The growing usage of hands-free kits with belt-holstered phones, in particular, has generated concerns about the possibility of radiofrequency-electromagnetic radiation (RF-EMR) exposure to the gonads [152].
7.5. Age
Age has a high impact on human reproduction. It also affects the HPG axis function, resulting in alterations in other reproductive hormones. This is because males go through a lot of physiological changes. As early as age 35, sperm parameters begin to drop steadily. The volume and motility of the sperm decline, and the morphology may become progressively aberrant [153].
7.6. Marijuana
Given the deleterious effects of marijuana on male reproductive physiology, marijuana includes the cannabinoid delta-9-tetrahydrocannabinol (THC), which inhibits the secretion of hypothalamic luteinizing hormone-releasing hormone (LHRH)and adenohypophysis LH. Furthermore, 1 THC’s central blockage of the HPG axis in males causes a dose-dependent decrease in plasma T levels, which may take up to 3 months to normalize following discontinuation. Chronic usage can cause gynecomastia, decreased libido, erectile dysfunction (ED), and ejaculatory dysfunction [152].
7.7. Obesity
Obesity was related to the risk for erectile dysfunction (ED). Being overweight or obesity is observed in 79% of males reporting ED symptoms. In very obese males, BMI was related to higher avoidance of sexual contact and increased difficulty with sexual performance, resulting in decreased satisfaction with sexual life [154]. This leading risk factor influences the metabolic processes; namely hypercaloric diet alters the low energy state which targets the HPG axis, thus creating a negative impact on female fecundity [155].
7.8. Stress
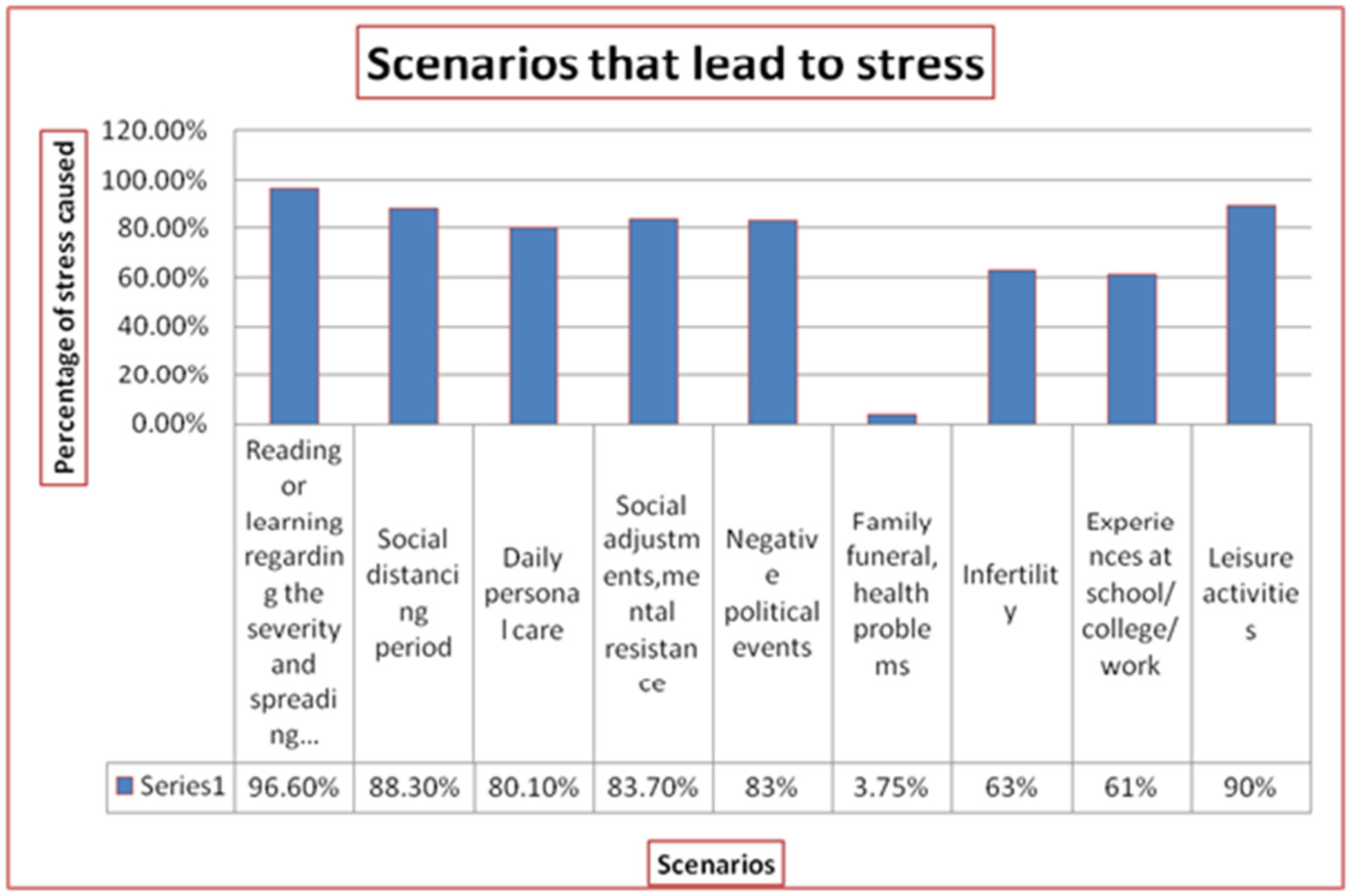
Stress is referred to as the non-peculiar response of the body to danger or unexpected events as well as the ability to trigger various stimuli [156]. Stress may be due to sexual attitude, marital life, quality of life, work life, motherhood, social tension, etc. Any of these may have a detrimental influence on sperm quality. The recent scenarios that may lead to stress are illustrated in Figure 2 [157]. Stress may not have a great impact on sperm morphology, but it has a 39% reduction in sperm quantity and a 48% reduction in motility. Thus it is indicated that stress is negatively associated with semen quality [150,152].
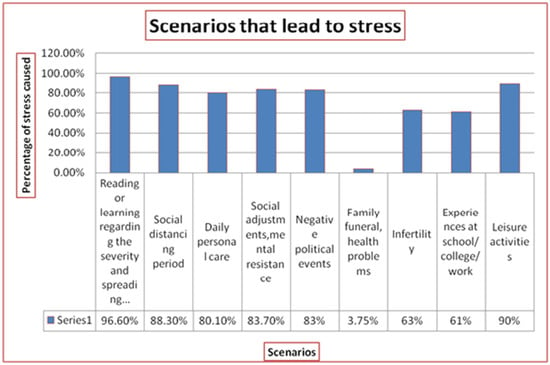
Figure 2.
Scenarios that lead to stress. This figure illustrates certain scenarios in human life that may lead to acute or chronic stress conditions and depicts them as a graphical representation of the percentage of stress they induce.
7.9. Anxiety
As an outcome of infertility treatment, the individuals affected by infertility have reported sexual distress, anxiety, frustration, emotional distress, marital problems, and loss of self-esteem [158]. The anxiety level is high in infertile men and women compared to a normal fertile control group that has been recently founded in research. Most of the psychological consequences show that women with infertility have a stringent experience of anxiety, and the women undergoing infertility treatment have to deal with two different types of stressors: the loss of parenthood hopes and the threat of certain infertility lead to a chronic stressor, and the fertility treatment itself leads to an acute stressor [159,160]. The cost of infertility treatment causes financial pressure, and the unpredictability of this treatment influences the sexual relationship [161].
7.10. Depression
In the case of women, culture, clinic visits, and sexual and social concerns were the elements associated with the symptoms of depression, whereas in men, financial status and social pressure were linked with depression symptoms [158]. Almost 30% of the population is suffering from clinical depression which causes lower libido, loss of interest, lower live births, etc. Thus, it stands as the major factor influencing the success rate of pregnancy, and its treatment deserves particular attention [159].
8. Infertility Management
8.1. Supplementations
Various formulations and uses of oral antioxidants that are readily available in the market were expected to treat infertile men and also increase the pregnancy outcomes in women with multiple miscarriages, but in certain case reports, it has been registered that over-usage of antioxidants will have an impact on sperm cells [162,163]. Another systematic review identified antioxidant vitamin E, vitamin C, N-acetylcysteine, selenium, and zinc as significantly beneficial for treating men with OS-related infertility [164].
8.2. Health Management
Exposure to harmful toxins or chemicals, pollution, and heavy metals; often taking hot baths; prolonged sitting or driving; and a workplace without great ventilation may induce OS. Hence, carrying out healthy habitual activities such as wearing personnel protective equipment, respiratory protection, eye protection, and hazard banding; following yoga and meditation; regular exercise; adequate sleep; and balanced nutrition are recommended [9,33,94,164]. Anxiety, depression, and fertility-related quality of life illustrate an improvement with participation in a yoga program [165]. Management of mental health during the pregnancy period and postpartum has to involve the obstetrician, pediatrician, and concerned members of the family [166]. Regular exercise leads to improved sperm and semen quality in lifestyle-induced infertility by increasing testicular antioxidant defenses, reducing levels of pro-inflammatory cytokines, and enhancing the steroidogenesis process [167].
8.3. Therapeutics
On understanding, the etiopathology mechanisms facilitate clinicians to undergo optimal treatment to overcome infertility. For most cases of infertility, targeted therapy that is a contributory cause of infertility is well known. Forthis, either hormonal or non-hormonal assistance is followed. Whereas idiopathic infertility is treated with empirical non-hormonal therapeutic assistance [168,169], the purpose of hormone therapy is well-defined in men with pin-down abnormalities which include hypogonadism [15]. A combined treatment of surgical approaches and hormonal therapy or customized therapeutic strategies have reported convincing results in recent years [168]. The therapeutic elements may include antioxidants, antibiotics, anti-inflammatory drugs, micronutrients, and non-hormonal compounds [169].
8.4. Psychological Support
The psychological status of infertility patients should be assessed ideally by a mental health professional with the framework of a questionnaire. This may hopefully increase the pregnancy outcomes. The support may be extended by providing the individuals with information on self-care skills and relaxation techniques to resolve anxiety or any distress conditions [33,169].
9. Conclusions
The couple facing infertility will be going through a stressful and depressing period of life. Silent struggle with infertility is prevailingly common among today’s individuals. The diagnosis and treatment are a tremendous burden. The impact of stress on infertility is still a controversial concept, However, stress, anxiety, and depression are found to have interventions in the reproductive rate. This review emphasizes that stress can be a major contributor to infertility, and it may also affect the treatment success rates, concerns about fertility, and the role of hormones in fertility outcomes. Finally, stress may be one of the reasons for infertility in this modern era. Furthermore, the documentation on the hormonal pathways that correlate the stress and infertility should be emphasized, which could enhance our view on the association between the common symptoms, stress, and infertility.
Author Contributions
Conceptualization, Methodology, Validation, and Draft preparation, S.R., M.D., P.P. (Prasad Poornima), S.E., S.S. and A.V.A.; Reviewing and editing, S.R. and A.V.A.; Formal analysis, A.J., I.P.G., V.B., P.P. (Palanisamy Priyanga) and J.V.; Language correction, S.R., B.B. and A.V.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The authors confirm that the data supporting the review are available upon reasonable request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Aldhuwayhi, S.; Shaikh, S.A.; Mallineni, S.K.; Kumari, V.V.; Thakare, A.A.; Ahmed Khan, A.R.; Mustafa, M.Z.; Manva, M.Z. Occupational Stress and Stress Busters Used Among Saudi Dental Practitioners During the COVID-19 Pandemic Outbreak. Disaster Med. Public Health Prep. 2022, 16, 1975–1981. [Google Scholar] [CrossRef] [PubMed]
- Arora, M.; Singh, A.; Singh, A.K.; Sharma, V.; Kotwal, A. Coping Strategies and Perception toward Drugs, Electronic Gadgets, and Media in Relation to Stress: A Cross-sectional Study among Residents of a Suburban Area. Indian J. Community Med. 2021, 46, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Yaribeygi, H.; Panahi, Y.; Sahraei, H.; Johnston, T.P.; Sahebkar, A. The impact of stress on body function: A review. EXCLI J. 2017, 16, 1057–1072. [Google Scholar] [CrossRef]
- Inhorn, M.C.; Patrizio, P. Infertility around the globe: New thinking on gender, reproductive technologies and global movements in the 21st century. Hum. Reprod. Update 2015, 21, 411–426. [Google Scholar] [CrossRef]
- Gnoth, C.; Godehardt, E.; Frank-Herrmann, P.; Friol, K.; Tigges, J.; Freundl, G. Definition and prevalence of subfertility and infertility. Hum. Reprod. 2005, 20, 1144–1147. [Google Scholar] [CrossRef] [PubMed]
- Adeoye, O.; Olawumi, J.; Opeyemi, A.; Christiania, O. Review on the role of glutathione on oxidative stress and infertility. JBRA Assist. Reprod. 2018, 22, 61–66. [Google Scholar] [CrossRef]
- Chu, K.Y.; Patel, P.; Ramasamy, R. Consideration of gender differences in infertility evaluation. Curr. Opin. Urol. 2019, 29, 267–271. [Google Scholar] [CrossRef]
- Makker, K.; Agarwal, A.; Sharma, R. Oxidative stress & male infertility. Indian J. Med. Res. 2009, 129, 357–367. [Google Scholar]
- Wu, J.X.; Lin, S.; Kong, S.B. Psychological Stress and Functional Endometrial Disorders: Update of Mechanism Insights. Front. Endocrinol. 2021, 3, 12–690255. [Google Scholar] [CrossRef]
- Lei, A.; You, H.; Luo, B.; Ren, J. The associations between infertility-related stress, family adaptability, and family cohesion in infertile couples. Sci. Rep. 2021, 11, 24220. [Google Scholar] [CrossRef]
- Dobson, H.; Smith, R.F. What is stress, and how does it affect reproduction? Anim. Reprod. Sci. 2000, 60–61, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Dai, S.; Mo, Y.; Wang, Y.; Xiang, B.; Liao, Q.; Zhou, M.; Li, X.; Li, Y.; Xiong, W.; Li, G.; et al. Chronic Stress Promotes Cancer Development. Front. Oncol. 2020, 10, 1492. [Google Scholar] [CrossRef]
- Dragoş, D.; Tănăsescu, M.D. The effect of stress on the defense systems. J. Med. Life 2010, 3, 10–18. [Google Scholar]
- Mintziori, G.; Duntas, L.H.; Veneti, S.; Goulis, D.G. Metabolic, oxidative and psychological stress as mediators of the effect of COVID-19 on male infertility: A literature review. Int. J. Environ. Res. Public Health 2022, 19, 5277. [Google Scholar] [CrossRef]
- Brauner, E.V.; Nordkap, L.; Priskorn, L.; Hansen, A.M.; Bang, A.K.; Holmboe, S.A.; Schmidt, L.; Jensen, T.K.; Jorgensen, N. Psychological stress, stressful life events, male factor infertility, and testicular function: A cross-sectional study. Fertil. Steril. 2020, 113, 865–875. [Google Scholar] [CrossRef]
- Vitale, S.G.; La Rosa, V.L.; Rapisarda, A.M.; Laganà, A.S. Psychology of infertility and assisted reproductive treatment: The Italian situation. J. Psychosom. Obstet. Gynaecol. 2017, 38, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Negris, O.; Lawson, A.; Brown, D.; Warren, C.; Galic, I.; Bozen, A.; Swanson, A.; Jain, T. Emotional stress and reproduction: What do fertility patients believe? J. Assist. Reprod. Genet. 2021, 38, 877–887. [Google Scholar] [CrossRef]
- Teklemicheal, A.G.; Kassa, E.M.; Weldetensaye, E.K. Prevalence and correlates of infertility related psychological stress in women with infertility: A cross-sectional hospital-based survey. BMC Psychol. 2022, 10, 91. [Google Scholar] [CrossRef]
- Zegers-Hochschild, F.; Adamson, G.D.; Dyer, S.; Racowsky, C.; de Mouzon, J.; Sokol, R. The international glossary on Infertility and fertility care. Fertil. Steril. 2017, 108, 393–406. [Google Scholar] [CrossRef]
- Westerman, R.; Kuhnt, A.K. Metabolic risk factors and fertility disorders: A narrative review of the female perspective. Reprod. Biomed. Online 2022, 14, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Lin, H.; Pan, P.; Yang, D.; Zhang, Q. Impact of central obesity on women with polycystic ovary syndrome undergoing in vitro fertilization. Biores. Open Access 2018, 7, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Khairy, M.; Rajkhowa, M. Effect of obesity on assisted reproductive treatment outcomes and its management: A literature review. Obstet. Gynecol. 2017, 19, 47–54. [Google Scholar] [CrossRef]
- Boutari, C.; Pappas, P.D.; Mintziori, G.; Nigdelis, M.P.; Athanasiadis, L.; Goulis, D.G.; Mantzoros, C.S. The effect of underweight on female and male reproduction. Metabolism 2020, 107, 154229. [Google Scholar] [CrossRef]
- Lu, J.; Wang, Z.; Cao, J.; Chen, Y.; Dong, Y. A novel and compact review on the role of oxidative stress in female reproduction. Reprod. Biol. Endocrinol. 2018, 16, 80. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Sharma, A.; Kshetrimayum, C. Environmental & occupational exposure & female reproductive dysfunction. Indian J. Med. Res. 2019, 150, 532–545. [Google Scholar] [CrossRef] [PubMed]
- Mancini, A.; Bruno, C.; Vergani, E.; d’Abate, C.; Giacchi, E.; Silvestrini, A. Oxidative Stress and Low-Grade Inflammation in Polycystic Ovary Syndrome: Controversies and New Insights. Int. J. Mol. Sci. 2021, 22, 1667. [Google Scholar] [CrossRef]
- Sun, Y.; Li, S.; Liu, H.; Bai, H.; Hu, K.; Zhang, R.; Liu, Q.; Fan, P. Oxidative stress promotes hyperandrogenism by reducing sex hormone-binding globulin in polycystic ovary syndrome. Fertil. Steril. 2021, 116, 1641–1650. [Google Scholar] [CrossRef]
- Wunder, D.; Kretschmer, R.; Bersinger, N.A. Concentrations of leptin and C-reactive protein in serum and follicular fluid during assisted reproductive cycles. Hum. Reprod. 2005, 20, 1266–1271. [Google Scholar] [CrossRef]
- Quenby, S.; Gallos, I.D.; Dhillon-Smith, R.K.; Podesek, M.; Stephenson, M.D.; Fisher, J.; Brosens, J.J.; Brewin, J.; Ramhorst, R.; Lucas, E.S.; et al. Miscarriage matters: The epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet 2021, 397, 1658–1667. [Google Scholar] [CrossRef]
- Din, H.N.; Strong, D.; Singh-Carlson, S.; Corliss, H.L.; Hartman, S.J.; Madanat, H.; Su, H.I. Association between pregnancy intention and preconception health behaviors. Cancer 2022, 128, 615–623. [Google Scholar] [CrossRef]
- Bhat, A.; Byatt, N. Infertility and Perinatal Loss: When the Bough Breaks. Curr. Psychiatry Rep. 2016, 18, 31. [Google Scholar] [CrossRef] [PubMed]
- Frey, K.A.; Navarro, S.M.; Kotelchuck, M.; Lu, M.C. The clinical content of preconception care: Preconception care for men. Am. J. Obstet. Gynecol. 2008, 199, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.; Lynch, C.D.; Kim, S.; Sundaram, R.; Sapra, K.J.; Buck Louis, G.M. Preconception stress and the secondary sex ratio in a population-based preconception cohort. Fertil. Steril. 2017, 107, 714–722. [Google Scholar] [CrossRef]
- Jungwirth, A.; Diemer, T.; Kopa, Z.; Krausz, C.; Minhas, S.; Tournaye, H. EAU guidelines on male infertility. Eur. Urol. 2018, 62, 324–332. [Google Scholar] [CrossRef] [PubMed]
- Palomba, S.; Daolio, J.; Romeo, S.; Battaglia, F.A.; Marci, R.; La Sala, G.B. Lifestyle and fertility: The influence of stress and quality of life on female fertility. Reprod. Biol. Endocrinol. 2018, 16, 113. [Google Scholar] [CrossRef]
- Rehman, R.; Amjad, S.; Tariq, H.; Zahid, N.; Akhter, M.; Ashraf, M. Oxidative stress and male infertility: A cross-sectional study. J. Pak. Med. Assoc. 2020, 70, 461–466. [Google Scholar] [CrossRef]
- Clarke, I.J.; Arbabi, L. New concepts of the central control of reproduction, integrating the influence of stress, metabolic state, and season. Domest. Anim. Endocrinol. 2016, 56, 165–179. [Google Scholar] [CrossRef]
- Ohlander, S.J.; Lindgren, M.C.; Lipshultz, L.I. Testosterone and Male Infertility. Urol. Clin. N. Am. 2016, 43, 195–202. [Google Scholar] [CrossRef]
- Semercioz, A.; Baltaci, A.K.; Mogulkoc, R.; Avunduk, M.C. Effect of Zinc and Melatonin on Oxidative Stress and Serum Inhibin-B Levels in a Rat Testicular Torsion-Detorsion Model. Biochem. Genet. 2017, 55, 395–409. [Google Scholar] [CrossRef]
- de Kretser, D.M.; Loveland, K.L.; Meinhardt, A.; Simorangkir, D.; Wreford, N. Spermatogenesis. Hum. Reprod. 1998, 13, 1–8. [Google Scholar] [CrossRef]
- Bhongade, M.B.; Prasad, S.; Jiloha, R.C.; Ray, P.C.; Mohapatra, S.; Koner, B.C. Effect of psychological stress on fertility hormones and seminal quality in male partners of infertile couples. Andrologia 2015, 47, 336–342. [Google Scholar] [CrossRef]
- Samplaski, M.K.; Loai, Y.; Wong, K.; Lo, K.C.; Grober, E.D.; Jarvi, K.A. Testosterone use in the male infertility population: Prescribing patterns and effects on semen and hormonal parameters. Fertil. Steril. 2014, 101, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Sidhom, K.; Panchendrabose, K.; Mann, U.; Patel, P. An update on male infertility and intratesticular testosterone-insight into novel serum biomarkers. Int. J. Impot. Res. 2022, 34, 673–678. [Google Scholar] [CrossRef] [PubMed]
- Fábregues, F.; Peñarrubia, J.; Creus, M.; Manau, D.; Casals, G.; Carmona, F.; Balasch, J. Transdermal testosterone may improve ovarian response to gonadotrophins in low-responder IVF patients: A randomized, clinical trial. Hum. Reprod. 2009, 24, 349–359. [Google Scholar] [CrossRef]
- Bakun, O.V.; Yurkiv, O.I.; Slobodian, K.V.; Kolesnik, O.V.; Maruschak, A.V. The level of some hormones in the blood women with endometriosis which associated with infertility. Wiadomości Lek. 2019, 72, 654–656. [Google Scholar] [CrossRef] [PubMed]
- Retana-Márquez, S.; Juárez-Rojas, L.; Ávila-Quintero, A.; Rojas-Maya, S.; Perera, G.; Casillas, F.; Betancourt, M.; Gómez-Quiroz, L. Neuroendocrine disruption is associated to infertility in chronically stressed female rats. Reprod. Biol 2020, 20, 474–483. [Google Scholar] [CrossRef]
- Cheng, C.Y.; Mruk, D.D. Cell junction dynamics in the testis: Sertoli-germ cell interactions and male contraceptive development. Physiol. Rev. 2002, 82, 825–874. [Google Scholar] [CrossRef]
- Goto, T.; Hirabayashi, M.; Watanabe, Y.; Sanbo, M.; Tomita, K.; Inoue, N.; Tsukamura, H.; Uenoyama, Y. Testosterone Supplementation Rescues Spermatogenesis and In Vitro Fertilizing Ability of Sperm in Kiss1 Knockout Mice. Endocrinology 2020, 161, bqaa092. [Google Scholar] [CrossRef]
- Allan, C.M.; Garcia, A.; Spaliviero, J. Complete Sertoli cell proliferation induced by follicle-stimulating hormone (FSH) independently of luteinizing hormone activity: Evidence from genetic models of isolated FSH action. Endocrinology 2004, 145, 1587–1593. [Google Scholar] [CrossRef]
- Conneely, O.M.; Mulac-Jericevic, B.; DeMayo, F.; Lydon, J.P.; O’Malley, B.W. Reproductive functions of progesterone receptors. Recent Prog. Horm. Res. 2002, 57, 339–355. [Google Scholar] [CrossRef]
- Bolyakov, A.; Paduch, D.A. Prolactin in men’s health and disease. Curr. Opin. Urol. 2011, 21, 527–534. [Google Scholar] [CrossRef]
- McIntyre, C.; Li, X.F.; de Burgh, R.; Ivanova, D.; Lass, G.; O’Byrne, K.T. GABA Signaling in the Posterodorsal Medial Amygdala Mediates Stress-induced Suppression of LH Pulsatility in Female Mice. Endocrinology 2022, 164, 197. [Google Scholar] [CrossRef]
- Li, X.; Zhou, L.; Peng, G.; Liao, M.; Zhang, L.; Hu, H.; Long, L.; Tang, X.; Qu, H.; Shao, J.; et al. Pituitary P62 deficiency leads to female infertility by impairing luteinizing hormone production. Exp. Mol. Med. 2021, 53, 1238–1249. [Google Scholar] [CrossRef]
- Freeman, M.E.; Kanyicska, B.; Lerant, A.; Nagy, G. Prolactin: Structure, function, and regulation of secretion. Physiol. Rev. 2000, 80, 1523–1631. [Google Scholar] [CrossRef]
- Lennartsson, A.K.; Billig, H.; Jonsdottir, I.H. Burnout is associated with elevated prolactin levels in men but not in women. J. Psychosom. Res. 2014, 76, 380–383. [Google Scholar] [CrossRef]
- Arowojolu, A.O.; Akinloye, O.; Shittu, O.B. Serum and seminal plasma prolactin levels in male attenders of an infertility clinic in Ibadan. J. Obstet. Gynaecol. 2004, 24, 306–309. [Google Scholar] [CrossRef]
- Hess, R.A.; Cooke, P.S. Estrogen in the male: A historical perspective. Biol. Reprod. 2018, 99, 27–44. [Google Scholar] [CrossRef]
- Carreau, S.; Hess, R.A. Oestrogens and spermatogenesis. Philos. Trans. R Soc. Lond. B Biol. Sci. 2010, 365, 1517–1535. [Google Scholar] [CrossRef]
- Lambard, S.; Carreau, S. Aromatase and oestrogens in human male germ cells. Int. J. Androl. 2005, 28, 254–259. [Google Scholar] [CrossRef]
- Bhardwaj, P.; Au, C.C.; Benito-Martin, A. Estrogens and breast cancer: Mechanisms involved in obesity-related development, growth and progression. J. Steroid. Biochem. Mol. Biol. 2019, 189, 161–170. [Google Scholar] [CrossRef]
- Bai, J.; Qi, Q.R.; Li, Y. Estrogen Receptors and Estrogen-Induced Uterine Vasodilation in Pregnancy. Int. J. Mol. Sci. 2020, 21, 4349. [Google Scholar] [CrossRef]
- Grimm, S.L.; Hartig, S.M.; Edwards, D.P. Progesterone receptor signaling mechanisms. J. Mol. Biol. 2016, 428, 3831–3849. [Google Scholar] [CrossRef]
- Petousis, S.; Prapas, Y.; Margioula-Siarkou, C. Unexplained infertility patients present the mostly impaired levels of progesterone receptors: Prospective observational study. Am. J. Reprod. Immunol. 2018, 79, 12828. [Google Scholar] [CrossRef]
- Poorasamy, J.; Sengupta, J.; Patil, A.; Ghosh, D. Progesterone resistance in endometriosis. Eur. Med. J. 2022, 8, 51–63. [Google Scholar] [CrossRef]
- Kim, H.H.; Schlegel, P.N. Endocrine manipulation in male infertility. Urol. Clin. N. Am. 2008, 35, 303–318. [Google Scholar] [CrossRef]
- Jeppesen, J.V.; Anderson, R.A.; Kelsey, T.W.; Christiansen, S.L.; Kristensen, S.G.; Jayaprakasan, K.; Raine-Fenning, N.; Campbell, B.K.; Yding Andersen, C. Which follicles make the most anti-Mullerian hormone in humans? Evidence for an abrupt decline in AMH production at the time of follicle selection. Mol. Hum. Reprod. 2013, 19, 519–527. [Google Scholar] [CrossRef]
- Silva, M.S.B.; Giacobini, P. New insights into anti-Müllerian hormone role in the hypothalamic-pituitary-gonadal axis and neuroendocrine development. Cell. Mol. Life Sci. 2021, 78, 1–16. [Google Scholar] [CrossRef]
- Luo, W.; Mao, P.; Zhang, L.; Chen, X.; Yang, Z. Assessment of ovarian reserve by serum antiMullerian hormone in patients with systemic lupus erythematosus: A meta-analysis. Ann. Palliat. Med. 2020, 9, 207–215. [Google Scholar] [CrossRef]
- Gleicher, N.; Weghofer, A.; Barad, D.H. Defining ovarian reserve to better understand ovarian aging. Reprod. Biol. Endocrinol. 2011, 9, 23. [Google Scholar] [CrossRef]
- McGee, E.A.; Hsueh, A.J. Initial and cyclic recruitment ofovarian follicles. Endocr. Rev. 2000, 21, 200–214. [Google Scholar] [CrossRef]
- Bernard, V.; Young, J.; Binart, N. Prolactin—A pleiotropic factor in health and disease. Nat. Rev. Endocrinol. 2019, 15, 356–365. [Google Scholar] [CrossRef]
- Studerus, E.; Ittig, S.; Beck, K.; Del Cacho, N.; Vila-Badia, R.; Butjosa, A.; Usall, J.; Riecher-Rössler, A. Relation between self-perceived stress, psychopathological symptoms and the stress hormone prolactin in emerging psychosis. J. Psychiatr. Res. 2021, 136, 428–434. [Google Scholar] [CrossRef]
- Sobrinho, L.G. Prolactin, psychological stress and environment in humans: Adaptation and maladaptation. Pituitary 2003, 6, 35–39. [Google Scholar] [CrossRef]
- Chu, Y.L.; Xu, Y.R.; Yang, W.X.; Sun, Y. The role of FSH and TGF-β superfamily in follicle atresia. Aging 2018, 10, 305–321. [Google Scholar] [CrossRef]
- Torner, L.; Neumann, I.D. The brain prolactin system: Involvement in stress response adaptations in lactation. Stress 2002, 5, 249–257. [Google Scholar] [CrossRef]
- Lennartsson, A.K.; Jonsdottir, I.H. Prolactin in response to acute psychosocial stress in healthy men and women. Psychoneuroendocrinology 2011, 36, 1530–1539. [Google Scholar] [CrossRef]
- Quintino-Moro, A.; Zantut-Wittmann, D.E.; Tambascia, M.; Machado, H.C.; Fernandes, A. High Prevalence of Infertility among Women with Graves’ Disease and Hashimoto’s Thyroiditis. Int. J. Endocrinol. 2014, 2014, 982705. [Google Scholar] [CrossRef]
- Maraka, S.; Ospina, N.M.; O’Keeffe, D.T.; Espinosa De Ycaza, A.E.; Gionfriddo, M.R.; Erwin, P.J.; Coddington, C.C.; Stan, M.N.; Murad, M.H.; Montori, V.M. Subclinical Hypothyroidism in Pregnancy: A Systematic Review and Meta-Analysis. Thyroid 2016, 26, 580–590. [Google Scholar] [CrossRef]
- Krassas, G.E.; Poppe, K.; Glinoer, D. Thyroid function and human reproductive health. Endocr. Rev. 2010, 31, 702–755. [Google Scholar] [CrossRef]
- Prummel, M.F.; Wiersinga, W.M. Thyroid autoimmunity and miscarriage. Eur. J. Endocrinol. 2004, 150, 751–755. [Google Scholar] [CrossRef]
- Vander Borght, M.; Wyns, C. Fertility and infertility: Definition and epidemiology. Clin. Biochem. 2018, 62, 2–10. [Google Scholar] [CrossRef]
- Poppe, K.; Glinoer, D.; Tournaye, H.; Devroey, P.; Velkeniers, B. Impact of the ovarian hyperstimulation syndrome on thyroid function. Thyroid 2008, 18, 801–802. [Google Scholar] [CrossRef]
- Wagner, M.S.; Wajner, S.M.; Maia, A.L. The role of thyroid hormone in testicular development and function. J. Endocrinol. 2008, 199, 351–365. [Google Scholar] [CrossRef]
- Capel, B. The battle of the sexes. Mech. Dev. 2000, 92, 89–103. [Google Scholar] [CrossRef]
- La Vignera, S.; Vita, R.; Condorelli, R.A. Impact of thyroid disease on testicular function. Endocrine 2017, 58, 397–407. [Google Scholar] [CrossRef]
- Rijntjes, E.; Gomes, M.L.M.; Zupanic, N. Transient hypothyroidism: Dual effect on adult-type Leydig cell and Sertoli cell development. Front. Physiol. 2017, 8, 323. [Google Scholar] [CrossRef]
- Bhardwaj, J.K.; Paliwal, A.; Saraf, P. Effects of heavy metals on reproduction owing to infertility. J. Biochem. Mol. Toxicol. 2021, 35, 22823. [Google Scholar] [CrossRef]
- Alahmar, A.; Dutta, S.; Sengupta, P. Thyroid hormones in male reproduction and infertility. Asian Pac. J. Reprod. 2019, 8, 203. [Google Scholar] [CrossRef]
- Romano, R.M.; Gomes, S.N.; Cardoso, N.C.S.; Schiessl, L.; Romano, M.A.; Oliveira, C.A. New insights for male infertility revealed by alterations in spermatic function and differential testicular expression of thyroid-related genes. Endocrine 2017, 55, 607–617. [Google Scholar] [CrossRef]
- Louis, G.M.; Lum, K.J.; Sundaram, R.; Chen, Z.; Kim, S.; Lynch, C.D.; Schisterman, E.F.; Pyper, C. Stress reduces conception probabilities across the fertile window: Evidence in support of relaxation. Fertil. Steril. 2011, 95, 2184–2189. [Google Scholar] [CrossRef]
- Bisht, S.; Faiq, M.; Tolahunase, M.; Dada, R. Oxidative stress and male infertility. Nat. Rev. Urol. 2017, 14, 470–485. [Google Scholar] [CrossRef] [PubMed]
- Tremellen, K. Oxidative stress and male infertility—A clinical perspective. Hum. Reprod. Update 2008, 14, 243–258. [Google Scholar] [CrossRef]
- Leisegang, K.; Dutta, S. Do lifestyle practices impede male fertility? Andrologia 2021, 53, 13595. [Google Scholar] [CrossRef]
- Dutta, S.; Sengupta, P. SARS-CoV-2 and Male Infertility: Possible Multifaceted Pathology. Reprod. Sci. 2021, 28, 23–26. [Google Scholar] [CrossRef]
- Pandey, A.K.; Gupta, A.; Tiwari, M.; Prasad, S.; Pandey, A.N.; Yadav, P.K.; Sharma, A.; Sahu, K.; Asrafuzzaman, S.; Vengayil, D.T.; et al. Impact of stress on female reproductive health disorders: Possible beneficial effects of shatavari (Asparagus racemosus). Biomed. Pharmacother. 2018, 103, 46–49. [Google Scholar] [CrossRef]
- Iwasa, T.; Matsuzaki, T.; Yano, K.; Mayila, Y.; Irahara, M. The roles of kisspeptin and gonadotropin inhibitory hormone in stress-induced reproductive disorders. Endocr. J. 2018, 65, 133–140. [Google Scholar] [CrossRef]
- Tan, B.L.; Norhaizan, M.E.; Liew, W.P. Nutrients and Oxidative Stress: Friend or Foe? Oxid. Med. Cell. Longev. 2018, 2018, 9719584. [Google Scholar] [CrossRef]
- Filomeni, G.; De Zio, D.; Cecconi, F. Oxidative stress and autophagy: The clash between damage and metabolic needs. Cell Death Differ. 2015, 22, 377–388. [Google Scholar] [CrossRef]
- Wang, L.; Tang, J.; Wang, L.; Tan, F.; Song, H.; Zhou, J.; Li, F. Oxidative stress in oocyte aging and female reproduction. J. Cell. Physiol. 2021, 236, 7966–7983. [Google Scholar] [CrossRef]
- Wojsiat, J.; Korczyński, J.; Borowiecka, M.; Żbikowska, H.M. The role of oxidative stress in female infertility and in vitro fertilization. Postep. Hig. Med. Dosw. 2017, 71, 359–366. [Google Scholar] [CrossRef]
- Alkadi, H. A review on free radicals and antioxidants. Infect. Disord. Drug Targets 2020, 20, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Gupta, S.; Sharma, R.K. Role of oxidative stress in female reproduction. Reprod. Biol. Endocrinol. 2005, 3, 28. [Google Scholar] [CrossRef] [PubMed]
- Scutiero, G.; Iannone, P.; Bernardi, G.; Bonaccorsi, G.; Spadaro, S.; Volta, C.A.; Greco, P.; Nappi, L. Oxidative Stress and Endometriosis: A Systematic Review of the Literature. Oxid. Med. Cell Longev. 2017, 2017, 7265238. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Aponte-Mellado, A.; Premkumar, B.J.; Shaman, A.; Gupta, S. The effects of oxidative stress on female reproduction: A review. Reprod. Biol. Endocrinol. 2012, 10, 49. [Google Scholar] [CrossRef] [PubMed]
- Dinan, T.G.; Cryan, J.F. The microbiome-gut-brain axis in health and disease. Gastroenterol. Clin. N. Am. 2017, 46, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Lynch, S.V.; Pedersen, O. The human intestinal microbiome in health and disease. N. Engl. J. Med. 2016, 375, 2369–2379. [Google Scholar] [CrossRef]
- Boers, S.A.; Jansen, R.; Hays, J.P. Understanding and overcoming the pitfalls and biases of next-generation sequencing (NGS) methods for use in the routine clinical microbiological diagnostic laboratory. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 1059–1070. [Google Scholar] [CrossRef]
- Lundy, S.D.; Sangwan, N.; Parekh, N.V. Functional and taxonomic dysbiosis of the gut, urine, and semen microbiomes in male infertility. Eur. Urol. 2021, 79, 826–836. [Google Scholar] [CrossRef]
- Agarwal, A.; Rana, M.; Qiu, E.; AlBunni, H.; Bui, A.D.; Henkel, R. Role of oxidative stress, infection and inflammation in male infertility. Andrologia 2018, 50, 13126. [Google Scholar] [CrossRef]
- Jensen, C.F.S.; Østergren, P.; Dupree, J.M.; Ohl, D.A.; Sønksen, J.; Fode, M. Varicocele and male infertility. Nat. Rev. Urol. 2017, 14, 523–533. [Google Scholar] [CrossRef]
- Ma, F.; Feng, Y.; Zhang, Y.; Wang, R.H.; Su, D. The Roles of Stress-Induced Immune Response in Female Reproduction. Adv. Exp. Med. Biol. 2021, 1300, 161–179. [Google Scholar] [CrossRef] [PubMed]
- Kalantaridou, S.N.; Zoumakis, E.; Makrigiannakis, A.; Lavasidis, L.G.; Vrekoussis, T.; Chrousos, G.P. Corticotropin-releasing hormone, stress and human reproduction: An update. J. Reprod. Immunol. 2010, 85, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Makrigiannakis, A.; Vrekoussis, T.; Zoumakis, E.; Navrozoglou, I.; Kalantaridou, S.N. CRH Receptors in Human Reproduction. Curr. Mol. Pharmacol. 2018, 11, 81–87. [Google Scholar] [CrossRef]
- Geraghty, A.C.; Kaufer, D. Glucocorticoid Regulation of Reproduction. Adv. Exp. Med. Biol. 2015, 872, 253–278. [Google Scholar] [CrossRef] [PubMed]
- Tamura, H.; Takasaki, A.; Taketani, T.; Tanabe, M.; Lee, L.; Tamura, I.; Maekawa, R.; Aasada, H.; Yamagata, Y.; Sugino, N. Melatonin and female reproduction. J. Obstet. Gynaecol. Res. 2014, 40, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Son, Y.L.; Ubuka, T.; Tsutsui, K. Regulation of stress response on the hypothalamic-pituitary-gonadal axis via gonadotropin-inhibitory hormone. Front. Neuroendocrinol. 2022, 64, 100953. [Google Scholar] [CrossRef]
- El Hayek, S.; Bitar, L.; Hamdar, L.H.; Mirza, F.G.; Daoud, G. Poly Cystic Ovarian Syndrome: An Updated Overview. Front. Physiol. 2016, 7, 124. [Google Scholar] [CrossRef]
- Collée, J.; Mawet, M.; Tebache, L.; Nisolle, M.; Brichant, G. Polycystic ovarian syndrome and infertility: Overview and insights of the putative treatments. Gynecol. Endocrinol. 2021, 37, 869–874. [Google Scholar] [CrossRef]
- Bachelot, A. Polycystic ovarian syndrome: Clinical and biological diagnosis. Ann. Biol. Clin. 2016, 74, 661–667. [Google Scholar] [CrossRef]
- Anagnostis, P.; Tarlatzis, B.C.; Kauffman, R.P. Polycystic ovarian syndrome (PCOS): Long-term metabolic consequences. Metabolism 2018, 86, 33–43. [Google Scholar] [CrossRef]
- Ibáñez, L.; Oberfield, S.E.; Witchel, S.; Auchus, R.J.; Chang, R.J.; Codner, E.; Dabadghao, P.; Darendeliler, F.; Elbarbary, N.S.; Gambineri, A.; et al. An International Consortium Update: Pathophysiology, Diagnosis, and Treatment of Polycystic Ovarian Syndrome in Adolescence. Horm. Res. Paediatr. 2017, 88, 371–395. [Google Scholar] [CrossRef] [PubMed]
- Barry, J.A.; Kuczmierczyk, A.R.; Hardiman, P.J. Anxiety and depression in polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. 2011, 26, 2442–2451. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yu, Z.; Zhao, S.; Cheng, L.; Man, Y.; Gao, X.; Zhao, H. Oxidative stress markers in the follicular fluid of patients with polycystic ovary syndrome correlate with a decrease in embryo quality. J. Assist. Reprod. Genet. 2021, 38, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Peker, N.; Turan, G.; Ege, S.; Bademkıran, M.H.; Karaçor, T.; Erel, Ö. The effect of clomiphene citrate on oxidative stress parameters in polycystic ovarian syndrome. J. Obstet. Gynaecol. 2021, 41, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Murri, M.; Luque-Ramírez, M.; Insenser, M.; Ojeda-Ojeda, M.; Escobar-Morreale, H.F. Circulating markers of oxidative stress and polycystic ovary syndrome (PCOS): A systematic review and meta-analysis. Hum. Reprod. Update 2013, 19, 268–288. [Google Scholar] [CrossRef]
- Wu, X.; Wu, H.; Sun, W.; Wang, C. Improvement of anti-Müllerian hormone and oxidative stress through regular exercise in Chinese women with polycystic ovary syndrome. Hormones 2021, 20, 339–345. [Google Scholar] [CrossRef]
- Simic, D.; Nikolic Turnic, T.; Dimitrijevic, A.; Zivadinovic, A.; Milosevic-Stevanovic, J.; Djuric, D.; Zivkovic, V.; Jakovljevic, V. Potential role of d-chiro-inositol in reducing oxidative stress in the blood of nonobese women with polycystic ovary syndrome. Can. J. Physiol. Pharmacol. 2022, 100, 629–636. [Google Scholar] [CrossRef]
- Ostadmohammadi, V.; Jamilian, M.; Bahmani, F.; Asemi, Z. Vitamin D and probiotic co-supplementation affects mental health, hormonal, inflammatory and oxidative stress parameters in women with polycystic ovary syndrome. J. Ovarian Res. 2019, 12, 5. [Google Scholar] [CrossRef]
- Xing, L.; Xu, J.; Wei, Y.; Chen, Y.; Zhuang, H.; Tang, W.; Yu, S.; Zhang, J.; Yin, G.; Wang, R.; et al. Depression in polycystic ovary syndrome: Focusing on pathogenesis and treatment. Front. Psychiatry 2022, 13, 1001484. [Google Scholar] [CrossRef]
- Zehravi, M.; Maqbool, M.; Ara, I. Depression and anxiety in women with polycystic ovarian syndrome: A literature survey. Int. J. Adolesc. Med. Health 2021, 33, 367–373. [Google Scholar] [CrossRef]
- Damone, A.L.; Joham, A.E.; Loxton, D.; Earnest, A.; Teede, H.J.; Moran, L.J. Depression, anxiety and perceived stress in women with and without PCOS: A community-based study. Psychol. Med. 2019, 49, 1510–1520. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, E.A.; Pasch, L.A.; Cedars, M.I.; Legro, R.S.; Eisenberg, E.; Huddleston, H.G. Eunice Kennedy Shriver National Institute of Child Health and Human Development Reproductive Medicine Network. Insulin resistance is associated with depression risk in polycystic ovary syndrome. Fertil. Steril. 2018, 110, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Dai, Y.; Tong, X.; Xu, W.; Huang, Q.; Jin, X.; Li, C.; Zhou, F.; Zhou, H.; Lin, X.; et al. Excessive oxidative stress in cumulus granulosa cells induced cell senescence contributes to endometriosis-associated infertility. Redox. Biol. 2020, 30, 101431. [Google Scholar] [CrossRef] [PubMed]
- Quigley, M.M. Drugs in the treatment of female infertility. Recent advances. Drugs 1986, 32, 169–177. [Google Scholar] [CrossRef]
- Al-Inany, H.; Johnson, N. Drugs for anovulatory infertility in polycystic ovary syndrome. BMJ 2006, 332, 1461–1462. [Google Scholar] [CrossRef]
- Elizur, S.E.; Tulandi, T. Drugs in infertility and fetal safety. Fertil. Steril. 2008, 89, 1595–1602. [Google Scholar] [CrossRef]
- Bulletti, C.; Coccia, M.E.; Battistoni, S.; Borini, A. Endometriosis and infertility. J. Assist. Reprod. Genet. 2010, 27, 441–447. [Google Scholar] [CrossRef]
- Augoulea, A.; Mastorakos, G.; Lambrinoudaki, I.; Christodoulakos, G.; Creatsas, G. The role of the oxidative-stress in the endometriosis-related infertility. Gynecol. Endocrinol. 2009, 25, 75–81. [Google Scholar] [CrossRef]
- Harley, A.; Gupta, S.; Agarwal, A. Targeting oxidative stress to treat endometriosis. Expert Opin. Ther. Targets 2015, 19, 1447–1464. [Google Scholar] [CrossRef]
- Sandhu, J.K.; Waqar, A.; Jain, A.; Joseph, C.; Srivastava, K.; Ochuba, O.; Alkayyali, T.; Ruo, S.W.; Poudel, S. Oxidative Stress in Polycystic Ovarian Syndrome and the Effect of Antioxidant N-Acetylcysteine on Ovulation and Pregnancy Rate. Cureus 2021, 13, 17887. [Google Scholar] [CrossRef]
- Painter, R.C.; Roseboom, T.J.; de Rooij, S.R. Long-term effects of prenatal stress and glucocorticoid exposure. Birth Defects Res. Part C Embryo Today Rev. 2012, 96, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Mate, A.; Reyes-Goya, C.; Santana-Garrido, Á.; Vázquez, C.M. Lifestyle, Maternal Nutrition and Healthy Pregnancy. Curr. Vasc. Pharmacol. 2021, 19, 132–140. [Google Scholar] [CrossRef]
- Bisconti, M.; Simon, J.F.; Grassi, S.; Leroy, B.; Martinet, B.; Arcolia, V.; Isachenko, V.; Hennebert, E. Influence of Risk Factors for Male Infertility on Sperm Protein Composition. Int. J. Mol. Sci. 2021, 22, 13164. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Biedenharn, K.R.; Fedor, J.M.; Agarwal, A. Lifestyle factors and reproductive health: Taking control of your fertility. Reprod. Biol. Endocrinol. 2013, 11, 66. [Google Scholar] [CrossRef] [PubMed]
- Osadchuk, L.V.; Osadchuk, A.V. Individual Lifestyle, and Male Fertility. Hum Physiol. 2023, 49, 196–207. [Google Scholar] [CrossRef]
- Kumar, M.; Zilate, S.; Gupta, C. Effect of Stress and Caffeine on Male Infertility. Cureus 2022, 14, 28487. [Google Scholar] [CrossRef]
- Wright, C.; Milne, S.; Leeson, H. Sperm DNA damage caused by oxidative stress: Modifiable clinical, lifestyle and nutritional factors in male infertility. Reprod. Biomed. Online 2014, 28, 684–703. [Google Scholar] [CrossRef]
- Barazani, Y.; Katz, B.F.; Nagler, H.M.; Stember, D.S. Lifestyle, environment, and male reproductive health. Urol. Clin. N. Am. 2014, 41, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Emokpae, M.A.; Brown, S.I. Effects of lifestyle factors on fertility: Practical recommendations for modification. Reprod. Fertil. 2021, 2, R13–R26. [Google Scholar] [CrossRef]
- Hammoud, A.O.; Meikle, A.W.; Reis, L.O.; Gibson, M.; Peterson, C.M.; Carrell, D.T. Obesity and male infertility: A practical approach. Semin. Reprod. Med. 2012, 30, 486–495. [Google Scholar] [CrossRef]
- Sutton-McDowall, M.L.; Gilchrist, R.B.; Thompson, J.G. The pivotal role of glucose metabolism in determining oocyte developmental competence. Reproduction 2010, 139, 685–695. [Google Scholar] [CrossRef] [PubMed]
- Koolhaas, J.M.; Bartolomucci, A.; Buwalda, B.; de Boer, S.F.; Flügge, G.; Korte, S.M.; Meerlo, P.; Murison, R.; Olivier, B.; Palanza, P.; et al. Stress revisited: A critical evaluationof the stress concept. Neurosci. Biobehav. Rev. 2011, 35, 1291–1301. [Google Scholar] [CrossRef] [PubMed]
- Klemetti, R.; Raitanen, J.; Sihvo, S.; Saarni, S.; Koponen, P. Infertility, mental disorders and well-being—A nationwide survey. Acta Obstet. Gynecol. Scand. 2010, 89, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Maroufizadeh, S.; Karimi, E.; Vesali, S.; Samani, R.O. Anxiety and depression after failure of assisted reproductive treatment among patients experiencing infertility. Int. J. Gynecol. Obstet. 2015, 130, 253–256. [Google Scholar] [CrossRef]
- Donarelli, Z.; Lo Coco, G.; Gullo, S.; Marino, A.; Volpes, A.; Allegra, A. Are attachment dimensions associated with infertility-related stress in couples undergoing their first IVF treatment? A study on the individual and cross-partner effect. Hum. Reprod. 2012, 27, 3215–3225. [Google Scholar] [CrossRef] [PubMed]
- Bakhtiari, A.; Basirat, Z.; Nasiri-Amiri, F. Sexual dysfunction in women undergoing fertility treatment in Iran: Prevalence and associated risk factors. J. Reprod. Infertil. 2016, 17, 26–33. [Google Scholar]
- Henkel, R.; Sandhu, I.S.; Agarwal, A. The excessive use of antioxidant therapy: A possible cause of male infertility? Andrologia 2019, 51, 13162. [Google Scholar] [CrossRef]
- Bai, C.F.; Sun, J.W.; Li, J.; Jing, W.H.; Zhang, X.K.; Zhang, X.; Ma, L.L.; Yue, R.; Cao, F.L. Gender differences in factors associated with depression in infertility patients. J. Adv. Nurs. 2019, 75, 3515–3524. [Google Scholar] [CrossRef]
- Gdańska, P.; Drozdowicz-Jastrzębska, E.; Grzechocińska, B.; Radziwon-Zaleska, M.; Węgrzyn, P.; Wielgoś, M. Anxiety and depression in women undergoing infertility treatment. Ginekol. Pol. 2017, 88, 109–112. [Google Scholar] [CrossRef]
- Gil-Villa, A.M.; Cardona-Maya, W.; Agarwal, A.; Sharma, R.; Cadavid, A. Role of male factor in early recurrent embryo loss: Do antioxidants have any effect? Fertil. Steril. 2009, 92, 565–571. [Google Scholar] [CrossRef]
- Sengupta, P.; Dutta, S.; Metals, I.; Skinner, M.K. Reference module in biomedical sciences: Encyclopedia. Asian Pac. J. Reprod. 2018, 99, 579–587. [Google Scholar] [CrossRef]
- Oron, G.; Allnutt, E.; Lackman, T.; Sokal-Arnon, T.; Holzer, H.; Takefman, J. A prospective study using Hatha Yoga for stress reduction among women waiting for IVF treatment. Reprod. Biomed. Online 2015, 30, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Majzoub, A.; Agarwal, A. Systematic review of antioxidant types and doses in male infertility: Benefits on semen parameters, advanced sperm function, assisted reproduction and live-birth rate. Arab. J. Urol. 2018, 16, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Mason, S.A.; Trewin, A.J.; Parker, L.; Wadley, G.D. Antioxidant supplements and endurance exercise: Current evidence and mechanistic insights. Redox Biol. 2020, 35, 101471. [Google Scholar] [CrossRef] [PubMed]
- Lolak, S.; Rashid, N.; Wise, T.N. Interface of Women’s Mental and Reproductive Health. Curr. Psychiatry Rep. 2005, 7, 220–227. [Google Scholar] [CrossRef]
- Schmidt, L. Infertility and assisted reproduction in Denmark. Epidemiology and psychosocial consequences. Dan Med. Bull 2006, 53, 390–417. [Google Scholar]
- Elkina, Y.L.; Atroshchenko, M.M.; Bragina, E.E.; Muronetz, V.I.; Schmalhausen, E.V. Oxidation of glyceraldehyde-3-phosphate dehydrogenase decreases sperm motility. Biochemistry 2011, 76, 268–272. [Google Scholar] [CrossRef]
- Alkatout, I.; Mettler, L.; Beteta, C.; Hedderich, J.; Jonat, W.; Schollmeyer, T.; Salmassi, A. Combined surgical and hormone therapy for endometriosis is the most effective treatment: Prospective, randomized, controlled trial. J. Minim. Invasive Gynecol. 2013, 20, 473–481. [Google Scholar] [CrossRef]
- Calogero, A.E.; Condorelli, R.A.; Russo, G.I.; La Vignera, S. Conservative Nonhormonal Options for the Treatment of Male Infertility: Antibiotics, Anti-Inflammatory Drugs, and Antioxidants. Biomed. Res. Int. 2017, 2017, 4650182. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).