Stride Mechanics and Strength Analysis of Lower Limbs in Runners with Medial Tibial Stress Syndrome vs. Asymptomatic Runners
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Data Collection and Evaluation Instruments
2.2.1. Questionnaire
2.2.2. Algometry
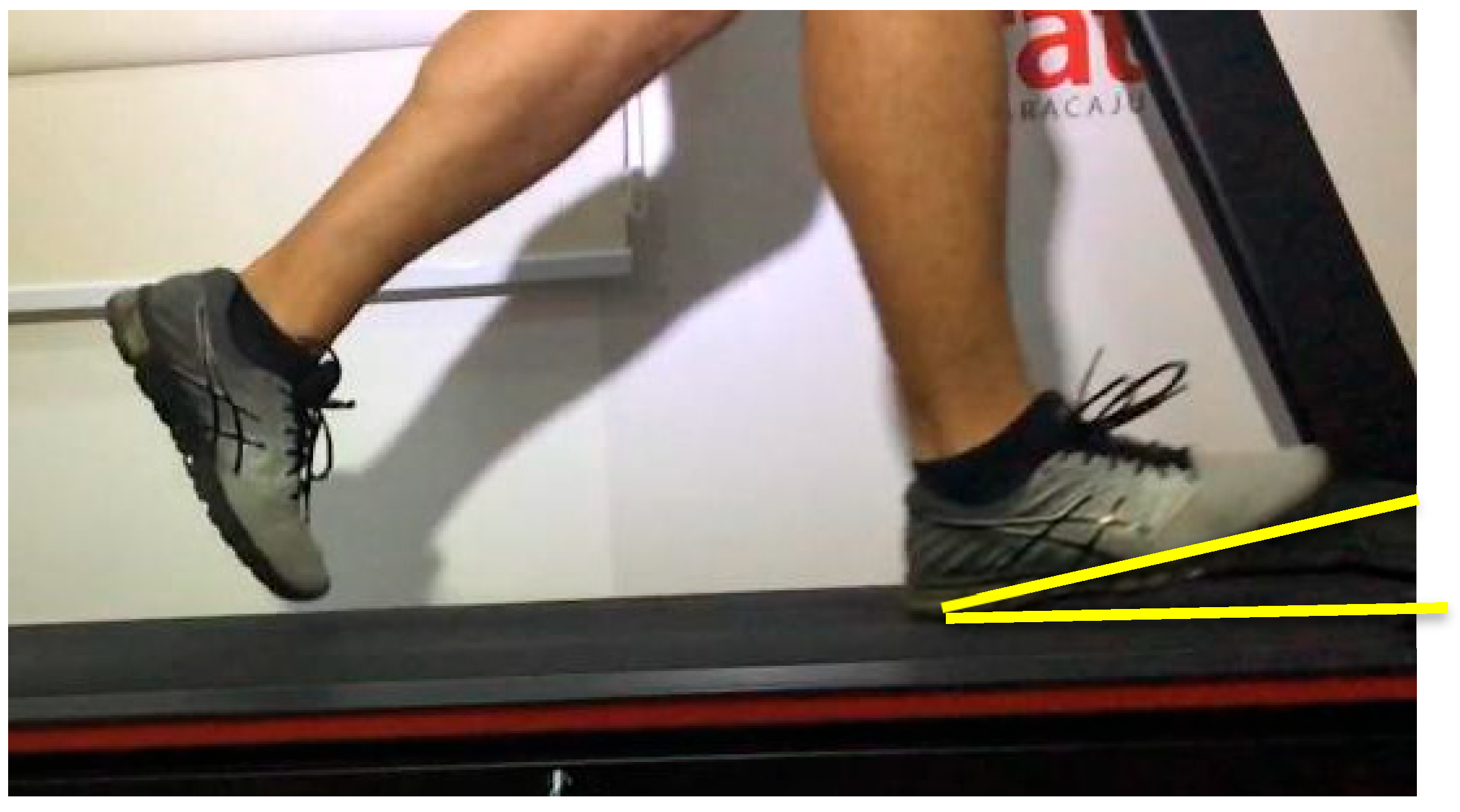
2.2.3. Running Kinematic Analysis
2.2.4. Muscular Strength
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Questionnaires
4.2. Algometry
4.3. Kinematics
4.4. Strength
4.5. Overview Discussion and Synthesis
- increased sensitivity along the posteromedial tibia;
- altered initial-contact mechanics at habitual running speed;
- selective deficits in key lower-limb stabilizing muscles;
- reduced physical activity levels among symptomatic runners.
4.6. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Karp, J.R. The effects of strength training on distance running performance and running injury prevention. J. Phys. Educ. Sport 2024, 25, 1352–1367. [Google Scholar] [CrossRef]
- Ruta, D.; Bocianiak, B.; Kajka, A.; Hamerska, J.; Antczak, J.; Hamerska, L.; Fenrych, U.; Wojtczak, K.; Skupińska, O.; Lipska, J. Health Aspects of Amateur Long-Distance Running. Qual. Sport 2024, 20, 53342. [Google Scholar] [CrossRef]
- Lower-Hoppe, L.M.; Aicher, T.J.; Baker, B.J. Intention–behaviour relationship within community running clubs: Examining the moderating influence of leisure constraints and facilitators within the environment. World Leis. J. 2022, 65, 3–27. [Google Scholar] [CrossRef]
- Jiang, X.; Zhang, Q.; Bíró, I. Effects of Long-Distance Running on Lower Limb Joint Kinematics in Recreational Runners. In Proceedings of the 2024 IEEE 18th International Symposium on Applied Computational Intelligence and Informatics (SACI), Timisoara, Romania, 21–25 May 2024; pp. 000095–000098. [Google Scholar] [CrossRef]
- Van Gent, R.N.; Siem, D.; Van Middelkoop, M.; Van Os, A.G.; Bierma-Zeinstra, S.M.; Koes, B.W. Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br. J. Sports Med. 2007, 41, 469–480. [Google Scholar] [CrossRef]
- Fredette, A.; Roy, J.S.; Perreault, K.; Dupuis, F.; Napier, C.; Esculier, J.F. The association between running injuries and training parameters: A systematic review. J. Athl. Train. 2022, 57, 650–671. [Google Scholar] [CrossRef] [PubMed]
- Willwacher, S.; Kurz, M.; Robbin, J.; Thelen, M.; Hamill, J.; Kelly, L.; Mai, P. Running-Related Biomechanical Risk Factors for Overuse Injuries in Distance Runners: A Systematic Review Considering Injury Specificity and the Potentials for Future Research. Sports Med. 2022, 52, 1863–1877. [Google Scholar] [CrossRef] [PubMed]
- Zadpoor, A.A.; Nikooyan, A.A. The relationship between lower-extremity stress fractures and ground reaction forces: A systematic review. Clin. Biomech. 2011, 26, 23–28. [Google Scholar] [CrossRef]
- Milner, C.E.; Hamill, J.; Davis, I.S. Are knee mechanics during early stance related to tibial stress fracture? Clin. Biomech. 2010, 25, 691–695. [Google Scholar] [CrossRef] [PubMed]
- Derrick, T.R.; Hamill, J.; Caldwell, G.E. Energy absorption during running and its relationship to injury risk. Med. Sci. Sports Exerc. 1998, 30, 128–135. [Google Scholar] [CrossRef]
- Frigo, C.A.; Merlo, A.; Brambilla, C.; Mazzoli, D. Balanced Foot Dorsiflexion Requires a Coordinated Activity of the Tibialis Anterior and the Extensor Digitorum Longus: A Musculoskeletal Modelling Study. Appl. Sci. 2023, 13, 7984. [Google Scholar] [CrossRef]
- Alderink, G.J.; Ashby, B.M. Ankle/Foot Complex: Recurrent Stress Fractures. In Clinical Kinesiology and Biomechanics; Springer: Cham, Switzerland, 2023; pp. 329–396. [Google Scholar] [CrossRef]
- Coslick, A.M.; Lestersmith, D.; Chiang, C.C.; Scura, D.; Wilkens, J.H.; Emam, M. Lower Extremity Bone Stress Injuries in Athletes: An Update on Current Guidelines. Curr. Phys. Med. Rehabil. Rep. 2024, 12, 39–49. [Google Scholar] [CrossRef]
- Winters, M.; Bakker, E.W.P.; Moen, M.H.; Barten, C.C.; Teeuwen, R.; Weir, A. Medial tibial stress syndrome can be diagnosed reliably using history and physical examination. Br. J. Sports Med. 2018, 52, 1267–1272. [Google Scholar] [CrossRef]
- Tweed, J.L.; Avil, S.J.; Campbell, J.A.; Barnes, M.R. Etiologic factors in the development of medial tibial stress syndrome: A review of the literature. J. Am. Podiatr. Med. Assoc. 2008, 98, 107–111. [Google Scholar] [CrossRef]
- Franklyn, M.; Oakes, B. Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World J. Orthop. 2015, 6, 577–589. [Google Scholar] [CrossRef]
- Ohmi, T.; Aizawa, J.; Hirohata, K.; Ohji, S.; Mitomo, S.; Ohara, T.; Yagishita, K. Biomechanical characteristics of the lower extremities during running in male long-distance runners with a history of medial tibial stress syndrome: A case control study. BMC Musculoskelet. Disord. 2023, 24, 103. [Google Scholar] [CrossRef]
- Moreira, P.F.; Veras, P.M.; Oliveira, T.M.; Souza, M.A.; Catharino, L.L.; Borel, W.P.; Barbosa, A.C.; Fonseca, D.S.; Felício, D.C. Incidence and biomechanical risk factors for running-related injuries: A prospective cohort study. J. Clin. Orthop. Trauma 2024, 57, 102562. [Google Scholar] [CrossRef]
- Parry, G.N.; Williams, S.; McKay, C.D.; Johnson, D.J.; Bergeron, M.F.; Cumming, S.P. Associations between growth, maturation and injury in youth athletes engaged in elite pathways: A scoping review. Br. J. Sports Med. 2024, 58, 1001–1010. [Google Scholar] [CrossRef] [PubMed]
- Mousavi, S.H.; Khorramroo, F.; Jafarnezhadgero, A. Gait retraining targeting foot pronation: A systematic review and meta-analysis. PLoS ONE 2024, 19, e0298646. [Google Scholar] [CrossRef] [PubMed]
- Onsen, L.T.; Lima, J.; Hutchinson, M. Chronic Leg Pain in Running Athletes. In Endurance Sports Medicine; Miller, T.L., Ed.; Springer: Cham, Switzerland, 2023; pp. 175–186. [Google Scholar] [CrossRef]
- Menéndez, C.; Batalla, L.; Prieto, A.; Rodríguez, M.Á.; Crespo, I.; Olmedillas, H. Medial Tibial Stress Syndrome in Novice and Recreational Runners: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 7457. [Google Scholar] [CrossRef]
- Napier, C.; Willy, R.W. Biomechanical strategies for injury prevention in distance runners. J. Orthop. Sports Phys. Ther. 2018, 48, 736–742. [Google Scholar]
- Ceyssens, L.; Vanelderen, R.; Barton, C.; Malliaras, P.; Dingenen, B. Biomechanical risk factors associated with running-related injuries: A systematic review. Sports Med. 2019, 49, 1095–1115. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, N.S.; Phansopkar, P. Medial Tibial Stress Syndrome: A Review Article. Cureus 2022, 14, e26641. [Google Scholar] [CrossRef]
- Meardon, S.A.; Hamill, J.; Derrick, T.R. Running injury mechanisms: Biomechanical loading and tissue fatigue. Exerc. Sport Sci. Rev. 2015, 43, 75–81. [Google Scholar]
- Davis, I.S.; Milner, C.E.; Hamill, J. Gait biomechanics and stress fractures in runners. Clin. Sports Med. 2004, 23, 217–231. [Google Scholar]
- BRASIL. Lei nº 14.874, de 28 de maio de 2024. Dispõe Sobre a Pesquisa com Seres Humanos e Institui o Sistema Nacional de Ética em Pesquisa com Seres Humanos. Diário Oficial da União: Seção 1, Brasília, DF, 28 maio 2024. Available online: https://legislacao.presidencia.gov.br/atos/?tipo=LEI&numero=14874&ano=2024&ato=677Izaq1ENZpWT381 (accessed on 15 November 2024).
- World Medical Association (WMA). Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. In Proceedings of the Relatory of 64th WMA General Assembly, Fortaleza, Brazil, 16–19 October 2013; Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 15 November 2024).
- Roberts-Lewis, S.F.; White, C.M.; Ashworth, M.; Rose, M.R. The validity of the International Physical Activity Questionnaire (IPAQ) for adults with progressive muscle diseases. Disabil. Rehabil. 2021, 44, 7312–7320. [Google Scholar] [CrossRef]
- Vesal, M.; Roohafza, H.; Feizi, A.; Asgari, K.; Shahoon, H.; Ani, A.; Adibi, P. Pressure algometry in the general adult population: Age and sex differences. Medicine 2024, 103, e39418. [Google Scholar] [CrossRef]
- Oliveira, N.C.D.; Silva, K.R.; Santos, A.C.; Alfieri, F.M. Reproducibility and reliability of pressure algometry: Are digital and analogue devices comparable? BrJP 2024, 7, e20240055. [Google Scholar] [CrossRef]
- Russo, L.; Di Capua, R.; Arnone, B.; Borrelli, M.; Coppola, R.; Esposito, F.; Padulo, J. Shoes and Insoles: The Influence on Motor Tasks Related to Walking Gait Variability and Stability. Int. J. Environ. Res. Public Health 2020, 17, 4569. [Google Scholar] [CrossRef]
- Di Giminiani, R.; Di Lorenzo, D.; La Greca, S.; Russo, L.; Masedu, F.; Totaro, R.; Padua, E. Angle-Angle Diagrams in the Assessment of Locomotion in Persons with Multiple Sclerosis: A Preliminary Study. Appl. Sci. 2022, 12, 7223. [Google Scholar] [CrossRef]
- Russo, L.; Belli, G.; Di Blasio, A.; Lupu, E.; Larion, A.; Fischetti, F.; Montagnani, E.; Di Biase Arrivabene, P.; De Angelis, M. The Impact of Nordic Walking Pole Length on Gait Kinematic Parameters. J. Funct. Morphol. Kinesiol. 2023, 8, 50. [Google Scholar] [CrossRef]
- Ardigò, L.P.; Buglione, A.; Russo, L.; Cular, D.; Esposito, F.; Doria, C.; Padulo, J. Marathon Shoes vs. Track Spikes: A Crossover Pilot Study on Metabolic Demand at Different Speeds in Experienced Runners. Res. Sports Med. 2023, 31, 13–20. [Google Scholar] [CrossRef]
- Bilić, Z.; Sinković, F.; Barbaros, P.; Novak, D.; Zemkova, E. Exercise-Induced Fatigue Impairs Change of Direction Performance and Serve Precision among Young Male Tennis Players. Sports 2023, 11, 111. [Google Scholar] [CrossRef]
- Russo, L.; Montagnani, E.; Buttari, D.; Ardigò, L.P.; Melenco, I.; Larion, A.; Migliaccio, G.M.; Padulo, J. Track Running Shoes: A Case Report of the Transition from Classical Spikes to “Super Spikes” in Track Running. Appl. Sci. 2022, 12, 10195. [Google Scholar] [CrossRef]
- Russo, L.; Micozzi, M.; Racil, G.; Larion, A.; Lupu, E.; Padulo, J.; Migliaccio, G.M. Decoding Motor Skills: Video Analysis Unveils Age-Specific Patterns in Childhood and Adolescent Movement. Children 2024, 11, 1351. [Google Scholar] [CrossRef] [PubMed]
- Kinovea [Computer Software]. 2024. Available online: https://www.kinovea.org (accessed on 1 April 2021).
- Padulo, J.; Trajković, N.; Cular, D.; Grgantov, Z.; Madić, D.M.; Di Vico, R.; Traficante, A.; Alin, L.; Ardigò, L.P.; Russo, L. Validity and Reliability of Isometric-Bench for Knee Isometric Assessment. Int. J. Environ. Res. Public Health 2020, 17, 4326. [Google Scholar] [CrossRef]
- Sørensen, L.; Oestergaard, L.G.; Van Tulder, M.; Petersen, A.K. Measurement Properties of Isokinetic Dynamometry for Assessment of Shoulder Muscle Strength: A Systematic Review. Arch. Phys. Med. Rehabil. 2021, 102, 510–520. [Google Scholar] [CrossRef] [PubMed]
- Staggs, V.S.; Feldman, K. Use of between-within degrees of freedom as an alternative to the Kenward–Roger method for small-sample inference in generalized linear mixed modeling of clustered count data. Commun. Stat. Simul. Comput. 2021, 52, 5099–5109. [Google Scholar] [CrossRef]
- Joachim, M.R.; Kuik, M.L.; Krabak, B.J.; Kraus, E.M.; Rauh, M.J.; Heiderscheit, B.C. Risk Factors for Running-Related Injury in High School and Collegiate Cross-country Runners: A Systematic Review. J. Orthop. Sports Phys. Ther. 2024, 54, 120–132. [Google Scholar] [CrossRef]
- Castillo-Domínguez, A.; García-Romero, J.C.; Alvero-Cruz, J.R.; Ponce-García, T.; Benítez-Porres, J.; Páez-Moguer, J. Systematic Review of Patient-Reported Outcome Measures for Patients with Exercise-Induced Leg Pain. Medicina 2022, 58, 841. [Google Scholar] [CrossRef]
- Saad, M.A.; Jamal, J.M.; Aldhafiri, A.T.; Alkandari, S.A. Medial Tibial Stress Syndrome: A Scoping Review of Epidemiology, Biomechanics, and Risk Factors. Cureus 2025, 17, e81463. [Google Scholar] [CrossRef]
- Galbraith, R.M.; Lavallee, M.E. Medial tibial stress syndrome: Conservative treatment options. Curr. Rev. Musculoskelet. Med. 2009, 2, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Naderi, A.; Fallah Mohammadi, M.; Heidaralizadeh, A.; Moen, M.H. Effects of Integrating Lower-Leg Exercises Into a Multimodal Therapeutic Approach on Medial Tibial Stress Syndrome Management Among Recreational Runners: A Randomized Controlled Study. Orthop. J. Sports Med. 2025, 13, 23259671241311849. [Google Scholar] [CrossRef] [PubMed]
- Leporace, G.; Guadagnin, E.C.; Carpes, F.P.; Gustafson, J.; Gonzalez, F.F.; Chahla, J.; Metsavaht, L. The Search for the Holy Grail in Running Biomechanics: Is There an Ideal Movement Profile for Minimizing Mechanical Overload? Sports Health A Multidiscip. Approach 2025. [Google Scholar] [CrossRef]
- Van Oeveren, B.T.; De Ruiter, C.J.; Beek, P.J.; Van Dieën, J.H. The Biomechanics of Running and Running Styles: A Synthesis. Sports Biomech. 2024, 23, 516–554. [Google Scholar] [CrossRef] [PubMed]

| Group | Age (Years) | Weight (kg) | Height (cm) |
|---|---|---|---|
| MTSS | 32.7 ± 8.1 | 66.4 ± 13.9 | 164.9 ± 10.9 |
| Control | 36.4 ± 10.4 | 71.9 ± 14.6 | 169.3 ± 7.2 |
| Control (n = 29) | MTSS (n = 27) | p-Value | Effect Size (95% CI) | |
|---|---|---|---|---|
| Before run | ||||
| Left leg (kgf ± SD) | 9.0 ± 2.0 | 5.7 ± 1.4 | <0.001 | 1.90 (1.26–2.53) |
| Right leg (kgf ± SD) | 8.9 ± 2.3 | 5.6 ± 1.8 | <0.001 | 1.59 (0.99–2.19) |
| After run | ||||
| Left leg (kgf ± SD) | 8.8 ± 2.1 | 4.4 ± 1.5 | <0.001 | 2.40 (1.70–3.09) |
| Right leg (kgf ± SD) | 8.8 ± 2.4 | 4.4 ± 1.6 | <0.001 | 2.14 (1.48–2.80) |
| Variable |
Control (n = 29) | MTSS (n = 27) | p-Value | Effect Size (95% CI) |
| V1 (km/h ± SD) | 8.5 ± 1.0 | 7.6 ± 1.0 | 0.002 | 0.90 (0.36–1.42) |
| V2 (km/h ± SD) | 11.5 ± 1.6 | 10.5 ± 1.6 | 0.026 | 0.62 (0.10–1.14) |
| V3 (km/h ± SD) | 14.5 ± 2.3 | 13.5 ± 2.3 | 0.097 | 0.43 (–0.08–0.93) |
| V1 | V2 | V3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | MTSS | p | d (95% CI) | Control | MTSS | p | d (95% CI) | Control | MTSS | p | d (95% CI) | |
| Left foot-strike angle (°) | −14.4 ± 9.2 | −19.0 ± 6.7 | 0.04 | 0.57 (0.03–1.10) | −14.1 ± 9.6 | −17.4 ± 6.2 | 0.13 | 0.39 (−0.16–0.93) | −15.3 ± 9.3 | −17.5 ± 6.3 | 0.33 | 0.37 (−0.19–0.92) |
| Right foot-strike angle (°) | −17.0 ± 9.5 | −21.4 ± 5.8 | 0.04 | 0.55 (0.02–1.09) | −18.1 ± 9.0 | −20.3 ± 7.8 | 0.36 | 0.25 (−0.28–0.79) | −18.0 ± 7.3 | −20.4 ± 9.6 | 0.25 | 0.28 (−0.24–0.81) |
| Left push-off angle (°) | 38.3 ± 5.0 | 36.1 ± 6.1 | 0.14 | 0.40 (−0.13–0.93) | 37.2 ± 5.2 | 35.8 ± 6.1 | 0.38 | 0.25 (−0.28–0.79) | 39.0 ± 5.2 | 37.2 ± 5.7 | 0.54 | 0.33 (−0.20–0.86) |
| Right push-off angle (°) | 36.4 ± 9.6 | 34.8 ± 4.6 | 0.40 | 0.18 (−0.33–0.70) | 35.2 ± 5.4 | 35.7 ± 6.7 | 0.77 | 0.08 (−0.44–0.60) | 38.0 ± 6.6 | 36.4 ± 4.8 | 0.58 | 0.28 (−0.25–0.80) |
| Muscle Group | Control (n = 29) | MTSS (n = 27) | p-Value | Effect Size d (95% CI) |
|---|---|---|---|---|
| Left Quadriceps femoris (N ± SD) | 212.4 ± 73.1 | 151.9 ± 78.3 | 0.00 | 0.80 (0.25–1.35) |
| Right Quadriceps femoris (N ± SD) | 222.8 ± 72.8 | 159.9 ± 73.1 | 0.00 | 0.86 (0.31–1.41) |
| Left abductors (N ± SD) | 180.4 ± 56.9 | 165.1 ± 71.4 | 0.39 | 0.24 (−0.29–0.76) |
| Right abductors (N ± SD) | 186.7 ± 68.4 | 158.6 ± 62.2 | 0.12 | 0.43 (−0.10–0.96) |
| Left external rotators (N ± SD) | 211.5 ± 95.1 | 149.7 ± 95.9 | 0.02 | 0.65 (0.11–1.19) |
| Right external rotators (N ± SD) | 217.9 ± 102.0 | 156.6 ± 92.3 | 0.02 | 0.63 (0.09–1.17) |
| Left Gluteus maximus (N ± SD) | 171.7 ± 74.8 | 157.8 ± 80.4 | 0.51 | 0.18 (−0.35–0.70) |
| Right Gluteus maximus (N ± SD) | 176.5 ± 76.7 | 145.7 ± 67.7 | 0.13 | 0.42 (−0.11–0.96) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dantas, E.H.M.; Barreto, R.B.; Narvaez Silva, M.A.; Almeida-Santos, M.A.; Belli, G.; Russo, L. Stride Mechanics and Strength Analysis of Lower Limbs in Runners with Medial Tibial Stress Syndrome vs. Asymptomatic Runners. Biomechanics 2025, 5, 106. https://doi.org/10.3390/biomechanics5040106
Dantas EHM, Barreto RB, Narvaez Silva MA, Almeida-Santos MA, Belli G, Russo L. Stride Mechanics and Strength Analysis of Lower Limbs in Runners with Medial Tibial Stress Syndrome vs. Asymptomatic Runners. Biomechanics. 2025; 5(4):106. https://doi.org/10.3390/biomechanics5040106
Chicago/Turabian StyleDantas, Estélio Henrique Martin, Ronald Bispo Barreto, Miguel Angel Narvaez Silva, Marcos Antonio Almeida-Santos, Guido Belli, and Luca Russo. 2025. "Stride Mechanics and Strength Analysis of Lower Limbs in Runners with Medial Tibial Stress Syndrome vs. Asymptomatic Runners" Biomechanics 5, no. 4: 106. https://doi.org/10.3390/biomechanics5040106
APA StyleDantas, E. H. M., Barreto, R. B., Narvaez Silva, M. A., Almeida-Santos, M. A., Belli, G., & Russo, L. (2025). Stride Mechanics and Strength Analysis of Lower Limbs in Runners with Medial Tibial Stress Syndrome vs. Asymptomatic Runners. Biomechanics, 5(4), 106. https://doi.org/10.3390/biomechanics5040106









