The Relationship between Balance Confidence and Center of Pressure in Lower-Limb Prosthesis Users
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedures
2.2. Measures
2.3. Statistical Analysis
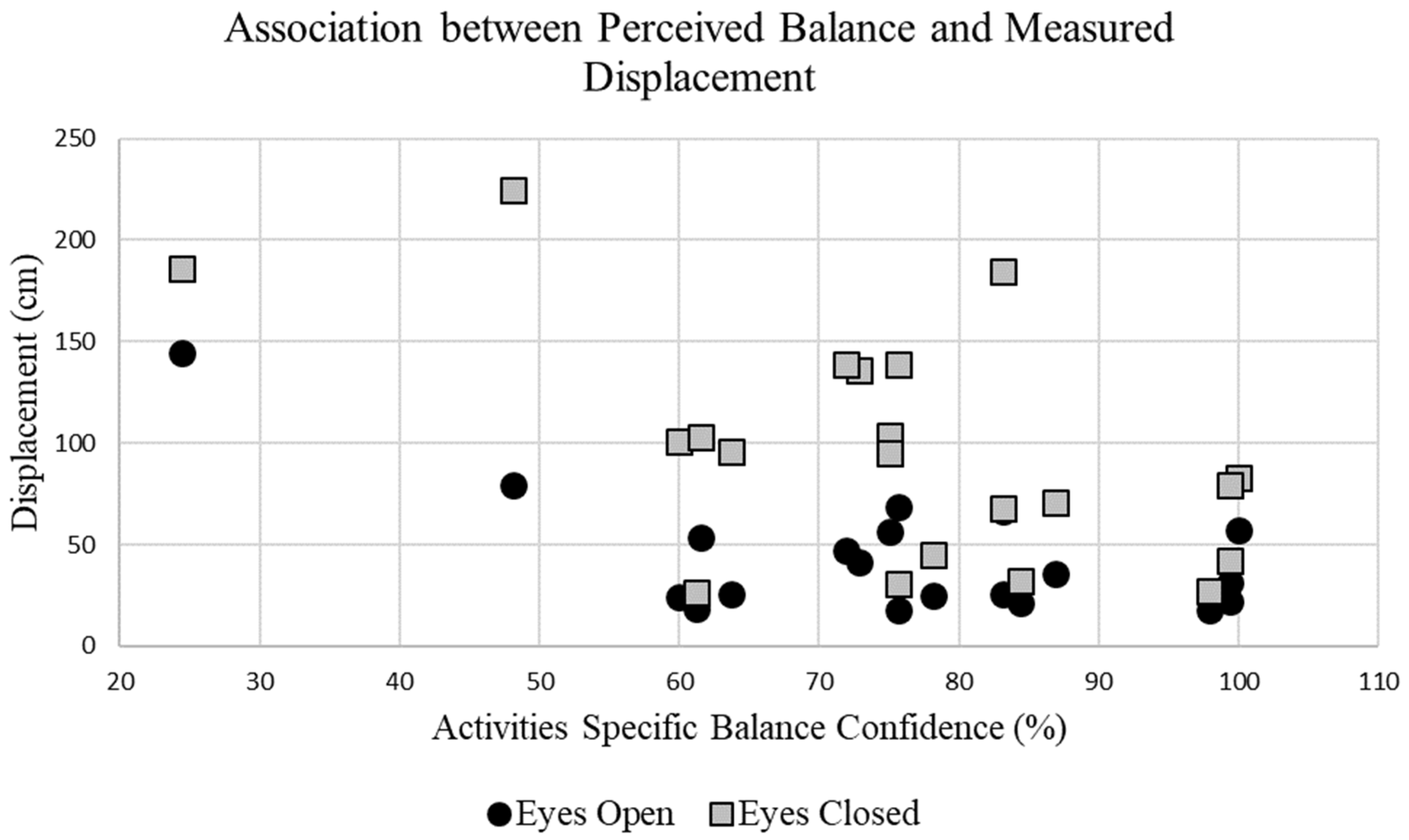
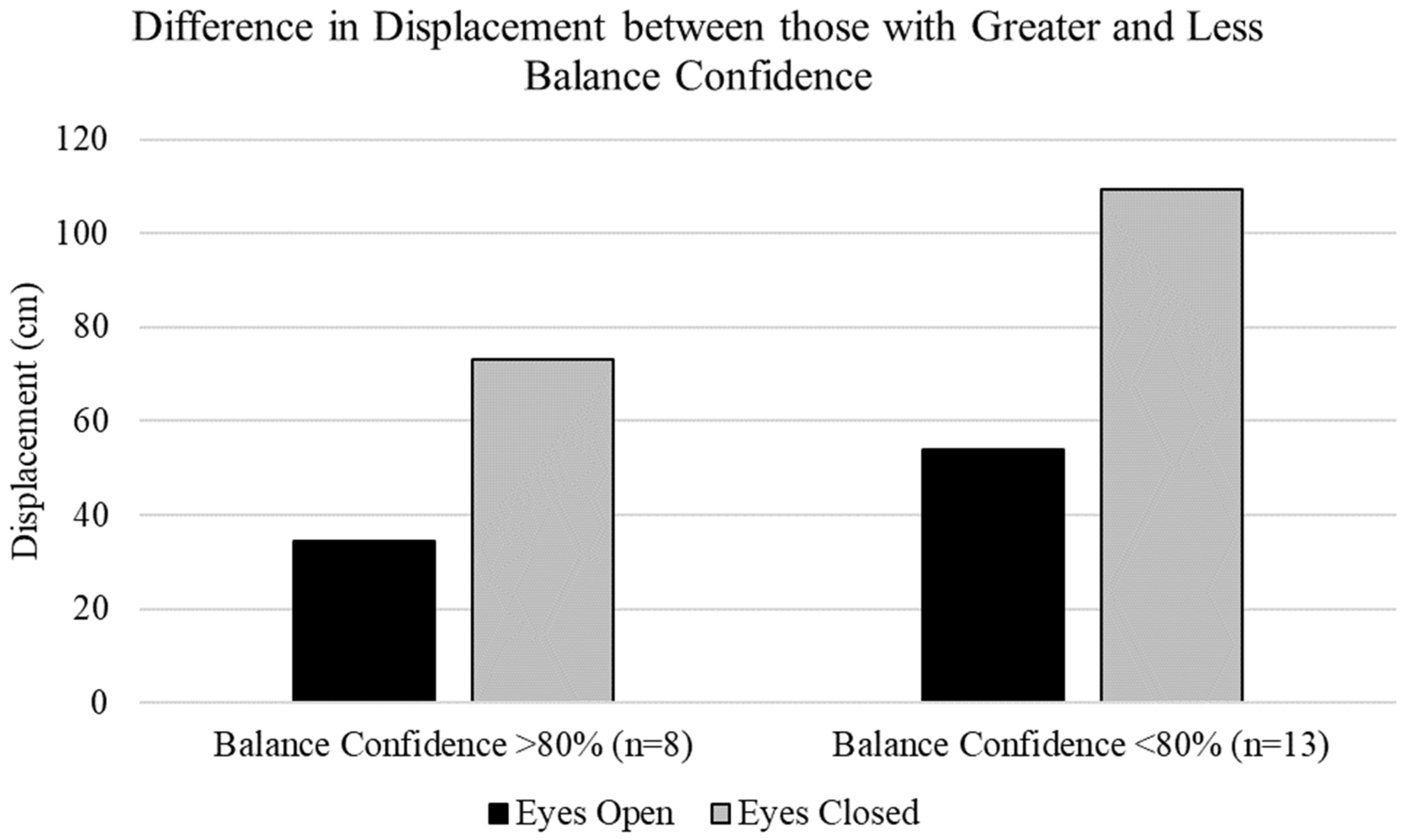
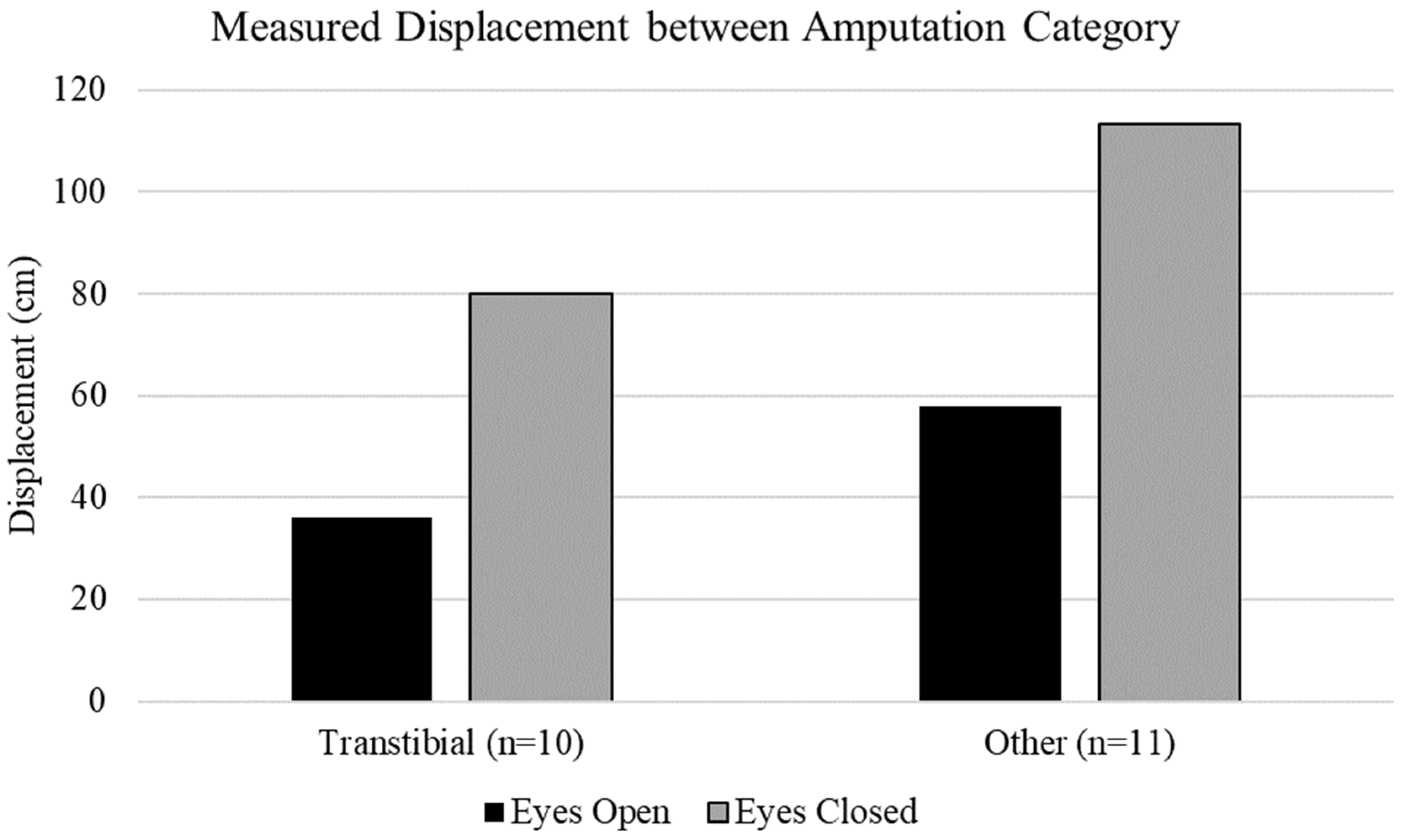
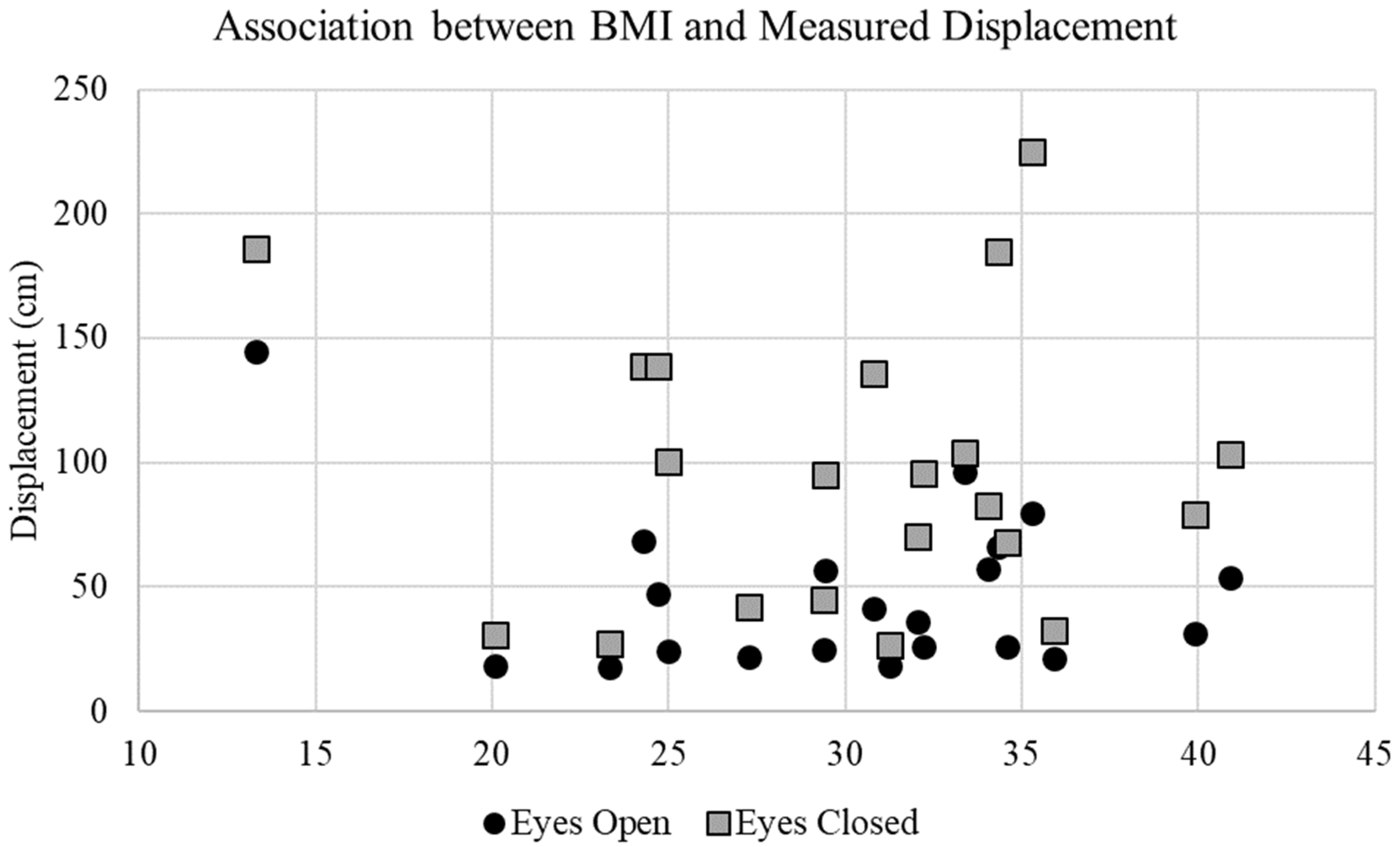
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Amtmann, D.; Morgan, S.J.; Kim, J.; Hafner, B.J. Health-Related Profiles of People with Lower Limb Loss. Arch. Phys. Med. Rehabil. 2015, 96, 1474–1483. [Google Scholar] [CrossRef] [PubMed]
- Finco, M.G.; Kim, S.; Ngo, W.; Menegaz, R.A. A Review of Musculoskeletal Adaptations in Individuals Following Major Lower-Limb Amputation. J. Musculoskelet. Neuronal Interact. 2022, 22, 269–283. [Google Scholar] [PubMed]
- Jiang, G.; Li, C.; Wu, J.; Jiang, T.; Zhang, Y.; Zhao, L.; Evans, A.C.; Li, L.; Ran, S.; Yin, X.; et al. Progressive Thinning of Visual Motion Area in Lower Limb Amputees. Front. Hum. Neurosci. 2016, 10, 79. [Google Scholar] [CrossRef] [PubMed]
- Horak, F.B. Postural Orientation and Equilibrium: What Do We Need to Know about Neural Control of Balance to Prevent Falls? Age Ageing 2006, 35, ii7–ii11. [Google Scholar] [CrossRef] [PubMed]
- Barnett, C.T.; Vanicek, N.; Polman, R.C.J. Temporal Adaptations in Generic and Population-Specific Quality of Life and Falls Efficacy in Men with Recent Lower-Limb Amputations. J. Rehabil. Res. Dev. 2013, 50, 437. [Google Scholar] [CrossRef] [PubMed]
- Geertzen, J.; van der Linde, H.; Rosenbrand, K.; Conradi, M.; Deckers, J.; Koning, J.; Rietman, H.S.; van der Schaaf, D.; van der Ploeg, R.; Schapendonk, J.; et al. Dutch Evidence-Based Guidelines for Amputation and Prosthetics of the Lower Extremity. Prosthet. Orthot. Int. 2015, 39, 361–371. [Google Scholar] [CrossRef] [PubMed]
- Ku, P.X.; Abu Osman, N.A.; Wan Abas, W.A.B. Balance Control in Lower Extremity Amputees during Quiet Standing: A Systematic Review. Gait Posture 2014, 39, 672–682. [Google Scholar] [CrossRef]
- Essien, S.K.; Kopriva, D.; Linassi, A.G.; Zucker-Levin, A. Trends of Limb Amputation Considering Type, Level, Sex and Age in Saskatchewan, Canada 2006–2019: An in-Depth Assessment. Arch. Public Health 2022, 80, 10. [Google Scholar] [CrossRef]
- Rommers, G.M.; Vos, L.D.W.; Groothoff, J.W.; Schuiling, C.H.; Eisma, W.H. Epidemiology of Lower Limb Amputees in the North of the Netherlands. Prosthet. Orthot. Int. 1997, 21, 92–99. [Google Scholar] [CrossRef]
- Ziegler-Graham, K.; MacKenzie, E.J.; Ephraim, P.L.; Travison, T.G.; Brookmeyer, R. Estimating the Prevalence of Limb Loss in the United States: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008, 89, 422–429. [Google Scholar] [CrossRef]
- Krajbich, J.; Pinzur, M.; Potter, B.; Stevens, P. Atlas of Amputations and Limb Deficiencies, 4th ed.; American Academy of Orthopaedic: Rosemont, IL, USA, 2016. [Google Scholar]
- Chen, L.; Feng, Y.; Chen, B.; Wang, Q.; Wei, K. Improving Postural Stability among People with Lower-Limb Amputations by Tactile Sensory Substitution. J. Neuroeng. Rehabil. 2021, 18, 159. [Google Scholar] [CrossRef]
- Gray, V.L.; Ivanova, T.D.; Garland, S.J. Reliability of Center of Pressure Measures within and between Sessions in Individuals Post-Stroke and Healthy Controls. Gait Posture 2014, 40, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Vrieling, A.H.; van Keeken, H.G.; Schoppen, T.; Otten, E.; Hof, A.L.; Halbertsma, J.P.K.; Postema, K. Balance Control on a Moving Platform in Unilateral Lower Limb Amputees. Gait Posture 2008, 28, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Condie, E.; Scott, H.; Treweek, S. Lower Limb Prosthetic Outcome Measures: A Review of the Literature 1995 to 2005. JPO J. Prosthet. Orthot. 2006, 18, P13–P45. [Google Scholar] [CrossRef]
- Hafner, B.J.; Morgan, S.J.; Askew, R.L.; Salem, R. Psychometric Evaluation of Self-Report Outcome Measures for Prosthetic Applications. J. Rehabil. Res. Dev. 2016, 53, 797–812. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.; Chen, C.C.; Benoy, S.A.; Rahal, R.T.; Blackwell, W.M. Role of Balance Ability and Confidence in Prosthetic Use for Mobility of People with Lower-Limb Loss. J. Rehabil. Res. Dev. 2014, 51, 1353–1364. [Google Scholar] [CrossRef]
- Powell, L.E.; Myers, A.M. The Activities-Specific Balance Confidence (ABC) Scale. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1995, 50, M28–M34. [Google Scholar] [CrossRef] [PubMed]
- Altenburg, B.; Ernst, M.; Maciejasz, P.; Schmalz, T.; Braatz, F.; Gerke, H.; Bellmann, M. Effects of A Prosthetic Foot with Increased Coronal Adaptability on Cross-Slope Walking. Can. Prosthet. Orthot. J. 2021, 4, 35206. [Google Scholar] [CrossRef]
- Miller, W.C.; Deathe, A.B.; Speechley, M.; Koval, J. The Influence of Falling, Fear of Falling, and Balance Confidence on Prosthetic Mobility and Social Activity among Individuals with a Lower Extremity Amputation. Arch. Phys. Med. Rehabil. 2001, 82, 1238–1244. [Google Scholar] [CrossRef]
- Horak, F.B.; Wrisley, D.M.; Frank, J. The Balance Evaluation Systems Test (BESTest) to Differentiate Balance Deficits. Phys. Ther. 2009, 89, 484–498. [Google Scholar] [CrossRef]
- Fuller, K.; Omaña Moreno, H.A.; Frengopoulos, C.; Payne, M.W.; Viana, R.; Hunter, S.W. Reliability, Validity, and Agreement of the Short-Form Activities-Specific Balance Confidence Scale in People with Lower Extremity Amputations. Prosthet. Orthot. Int. 2019, 43, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Frengopoulos, C.; Zia, Z.; Payne, M.; Viana, R.; Hunter, S. Association between Balance Self-Efficacy And Walking Ability in Those With New Lower Limb Amputations. Can. Prosthet. Orthot. J. 2022, 5, 36695. [Google Scholar] [CrossRef] [PubMed]
- Quijoux, F.; Nicolaï, A.; Chairi, I.; Bargiotas, I.; Ricard, D.; Yelnik, A.; Oudre, L.; Bertin-Hugault, F.; Vidal, P.-P.; Vayatis, N.; et al. A Review of Center of Pressure (COP) Variables to Quantify Standing Balance in Elderly People: Algorithms and Open-Access Code. Physiol. Rep. 2021, 9, e15067. [Google Scholar] [CrossRef]
- Johansson, J.; Jarocka, E.; Westling, G.; Nordström, A.; Nordström, P. Predicting Incident Falls: Relationship between Postural Sway and Limits of Stability in Older Adults. Hum. Mov. Sci. 2019, 66, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Koltermann, J.; Gerber, M.; Beck, H.; Beck, M. Validation of the HUMAC Balance System in Comparison with Conventional Force Plates. Technologies 2017, 5, 44. [Google Scholar] [CrossRef]
- Sahoo, P.K.; Sahu, M.M. Quantitative Assessment of Postural Balance in Patients with Chronic Anterior Cruciate Ligament Injury—A Controlled Study. J. Clin. Orthop. Trauma 2021, 23, 101645. [Google Scholar] [CrossRef] [PubMed]
- Guerra, G.; Smith, J.D. Correlates of Balance and Aerobic Indices in Lower-Limb Prostheses Users on Arm Crank Exercise. Sensors 2021, 21, 6917. [Google Scholar] [CrossRef]
- Stone, A.A.; Shiffman, S. Capturing Momentary, Self-Report Data: A Proposal for Reporting Guidelines. Ann. Behav. Med. 2002, 24, 236–243. [Google Scholar] [CrossRef]
- Krumpal, I. Determinants of Social Desirability Bias in Sensitive Surveys: A Literature Review. Qual. Quant. 2013, 47, 2025–2047. [Google Scholar] [CrossRef]
- Cameron, M.H.; Huisinga, J. Objective and Subjective Measures Reflect Different Aspects of Balance in Multiple Sclerosis. J. Rehabil. Res. Dev. 2013, 50, 1401–1410. [Google Scholar] [CrossRef]
- Lee, H.K.; Altmann, L.J.P.; McFarland, N.; Hass, C.J. The Relationship between Balance Confidence and Control in Individuals with Parkinson’s Disease. Park. Relat. Disord. 2016, 26, 24–28. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Miller, W.C.; Deathe, A.B.; Speechley, M. Psychometric Properties of the Activities-Specific Balance Confidence Scale among Individuals with a Lower-Limb Amputation. Arch. Phys. Med. Rehabil. 2003, 84, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, H.L.; Ting, L.H.; Bingham, J.T. Accuracy of Force and Center of Pressure Measures of the Wii Balance Board. Gait Posture 2014, 39, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, B.; Pothier, D.; Hughes, C.; Rutka, J. A Portable, Low-Cost System for Posturography: A Platform for Longitudinal Balance Telemetry. J. Otolaryngol. Head Neck Surg. 2012, 41 (Suppl. 1), S31–S35. [Google Scholar]
- Miller, W.C.; Speechley, M.; Deathe, A.B. Balance Confidence among People with Lower-Limb Amputations. Phys. Ther. 2002, 82, 856–865. [Google Scholar] [CrossRef]
- Miller, W.; Deathe, A. A Prospective Study Examining Balance Confidence among Individuals with Lower Limb Amputation. Disabil. Rehabil. 2004, 26, 875–881. [Google Scholar] [CrossRef]
- Myers, A.M.; Fletcher, P.C.; Myers, A.H.; Sherk, W. Discriminative and Evaluative Properties of the Activities-Specific Balance Confidence (ABC) Scale. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1998, 53, M287–M294. [Google Scholar] [CrossRef]
- Wong, C.K.; Young, R.S.; Ow-Wing, C.; Karimi, P. Determining 1-Yr Prosthetic Use for Mobility Prognoses for Community-Dwelling Adults with Lower-Limb Amputation. Am. J. Phys. Med. Rehabil. 2016, 95, 339–347. [Google Scholar] [CrossRef]
- Abasıyanık, Z.; Özdoğar, A.T.; Sağıcı, Ö.; Kahraman, T.; Baba, C.; Ertekin, Ö.; Özakbaş, S. Explanatory Factors of Balance Confidence in Persons with Multiple Sclerosis: Beyond the Physical Functions. Mult. Scler. Relat. Disord. 2020, 43, 102239. [Google Scholar] [CrossRef]
- Huang, T.-T.; Wang, W.-S. Comparison of Three Established Measures of Fear of Falling in Community-Dwelling Older Adults: Psychometric Testing. Int. J. Nurs. Stud. 2009, 46, 1313–1319. [Google Scholar] [CrossRef]
- Pavlou, M.; Costafreda, S.G.; Galsworthy, W.; Korres, G.; Bamiou, D.-E. The Interplay between Cognition, Functional and Dual-Task Gait in Persons with a Vestibular Disorder versus Healthy Controls. Sci. Rep. 2023, 13, 10130. [Google Scholar] [CrossRef] [PubMed]
- Tao, G.; Miller, W.C.; Eng, J.J.; Esfandiari, E.; Imam, B.; Lindstrom, H.; Payne, M.W. Group-Based Telerehabilitation Intervention Using Wii Fit to Improve Walking in Older Adults with Lower Limb Amputation (WiiNWalk): A Randomized Control Trial. Clin. Rehabil. 2022, 36, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.; Gibbs, W.B. Factors Associated with Committed Participation in a Wellness-Walking Program for People with Lower Limb Loss. Prosthet. Orthot. Int. 2019, 43, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Rosenblatt, N.J.; Stachowiak, A.; Reddin, C. Prosthetic Disuse Leads to Lower Balance Confidence in a Long-Term User of a Transtibial Prosthesis. Adv. Wound Care 2021, 10, 529–533. [Google Scholar] [CrossRef] [PubMed]
- Jayaraman, C.; Mummidisetty, C.K.; Albert, M.V.; Lipschutz, R.; Hoppe-Ludwig, S.; Mathur, G.; Jayaraman, A. Using a Microprocessor Knee (C-Leg) with Appropriate Foot Transitioned Individuals with Dysvascular Transfemoral Amputations to Higher Performance Levels: A Longitudinal Randomized Clinical Trial. J. Neuroeng. Rehabil. 2021, 18, 88. [Google Scholar] [CrossRef] [PubMed]
- Deathe, A.B.; Miller, W.C. The L Test of Functional Mobility: Measurement Properties of a Modified Version of the Timed “Up & Go” Test Designed for People with Lower-Limb Amputations. Phys. Ther. 2005, 85, 626–635. [Google Scholar] [CrossRef]
- Elboim-Gabyzon, M.; Agmon, M.; Azaiza, F. Psychometric Properties of the Arabic Version of the Activities-Specific Balance Confidence (ABC) Scale in Ambulatory, Community-Dwelling, Elderly People. Clin. Interv. Aging 2019, 14, 1075–1084. [Google Scholar] [CrossRef]
- Major, M.J.; Fatone, S.; Roth, E.J. Validity and Reliability of the Berg Balance Scale for Community-Dwelling Persons With Lower-Limb Amputation. Arch. Phys. Med. Rehabil. 2013, 94, 2194–2202. [Google Scholar] [CrossRef]
- Lohnes, C.A.; Earhart, G.M. External Validation of Abbreviated Versions of the Activities-Specific Balance Confidence Scale in Parkinson’s Disease. Mov. Disord. 2010, 25, 485–489. [Google Scholar] [CrossRef]
- Bateni, H. Postural Sway in Lower Extremity Amputees and Older Adults May Suggest Increased Fall Risk in Amputees. Can. Prosthet. Orthot. J. 2020, 3, 33804. [Google Scholar] [CrossRef]
- Li, Z.; Liang, Y.-Y.; Wang, L.; Sheng, J.; Ma, S.-J. Reliability and Validity of Center of Pressure Measures for Balance Assessment in Older Adults. J. Phys. Ther. Sci. 2016, 28, 1364–1367. [Google Scholar] [CrossRef] [PubMed]
- Sawacha, Z.; Carraro, E.; Contessa, P.; Guiotto, A.; Masiero, S.; Cobelli, C. Relationship between Clinical and Instrumental Balance Assessments in Chronic Post-Stroke Hemiparesis Subjects. J. Neuroeng. Rehabil. 2013, 10, 95. [Google Scholar] [CrossRef] [PubMed]
- Jayakaran, P.; Johnson, G.M.; Sullivan, S.J. Concurrent Validity of the Sensory Organization Test Measures in Unilateral Transtibial Amputees. Prosthet. Orthot. Int. 2012, 37, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Hermodsson, Y.; Ekdahl, C.; Persson, B.M.; Roxendal, G. Standing Balance in Trans-Tibial Amputees Following Vascular Disease or Trauma. Prosthet. Orthot. Int. 1994, 18, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Nadollek, H.; Brauer, S.; Isles, R. Outcomes after Trans-Tibial Amputation: The Relationship between Quiet Stance Ability, Strength of Hip Abductor Muscles and Gait. Physiother. Res. Int. 2002, 7, 203–214. [Google Scholar] [CrossRef] [PubMed]
- Wurdeman, S.R.; Stevens, P.M.; Campbell, J.H. Mobility Analysis of AmpuTees (MAAT 6): Mobility, Satisfaction, and Quality of Life among Long-Term Dysvascular/Diabetic Prosthesis Users-Results of a Cross-Sectional Analysis. J. Prosthet. Orthot. 2021, 33, 161–167. [Google Scholar] [CrossRef]
- Hafner, B.J.; Amtmann, D.; Morgan, S.J.; Abrahamson, D.C.; Askew, R.L.; Bamer, A.M.; Salem, R.; Gaunaurd, I.A.; Gailey, R.S.; Czerniecki, J.M.; et al. Development of an Item Bank for Measuring Prosthetic Mobility in People with Lower Limb Amputation: The Prosthetic Limb Users Survey of Mobility (PLUS-M). PM&R 2023, 15, 456–473. [Google Scholar] [CrossRef]
- Ratna Bajracharya, A.; Seng-iad, S.; Sasaki, K.; Guerra, G. Cross-Cultural Adaptation and Validation of the Nepali Version of the Prosthetic Limb Users Survey of Mobility Short-Form (PLUS-Mtm/Nepali-12sf) In Lower Limb Prosthesis Users. Can. Prosthet. Orthot. J. 2023, 6, 1. [Google Scholar] [CrossRef]

| Characteristics | Total (N = 21) | Male (n = 14) | Female (n = 7) |
|---|---|---|---|
| Age (y) | 53.5 ± 12.8 | 51.7 ± 11.8 | 57.3 ± 14.8 |
| Height (cm) | 171.9 ± 9.2 | 176.6 ± 5.9 | 162.6 ± 7.4 |
| Mass (kg) | 89.7 ± 22.4 | 97.3 ± 16.1 | 74.3 ± 26.5 |
| Amputation Duration (years) | 15.7 ± 17.0 | 17.8 ± 17.5 | 11.7 ± 16.6 |
| Classification | |||
| Right Transtibial | 4 | 3 | 1 |
| Left Transtibial | 8 | 5 | 3 |
| Right Transfemoral | 1 | 1 | |
| Left Transfemoral | 1 | 1 | |
| Bilateral Transtibial | 3 | 1 | 2 |
| Bilateral Transfemoral | 1 | 1 | |
| Bilateral Knee Disarticulation | 1 | 1 | |
| Other | 2 | 1 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guerra, G.; Smith, J.D.; Yoon, E.-J. The Relationship between Balance Confidence and Center of Pressure in Lower-Limb Prosthesis Users. Biomechanics 2023, 3, 561-570. https://doi.org/10.3390/biomechanics3040045
Guerra G, Smith JD, Yoon E-J. The Relationship between Balance Confidence and Center of Pressure in Lower-Limb Prosthesis Users. Biomechanics. 2023; 3(4):561-570. https://doi.org/10.3390/biomechanics3040045
Chicago/Turabian StyleGuerra, Gary, John D. Smith, and Eun-Jung Yoon. 2023. "The Relationship between Balance Confidence and Center of Pressure in Lower-Limb Prosthesis Users" Biomechanics 3, no. 4: 561-570. https://doi.org/10.3390/biomechanics3040045
APA StyleGuerra, G., Smith, J. D., & Yoon, E.-J. (2023). The Relationship between Balance Confidence and Center of Pressure in Lower-Limb Prosthesis Users. Biomechanics, 3(4), 561-570. https://doi.org/10.3390/biomechanics3040045







