Lower-Extremity Kinematics of Soccer Players with Chronic Ankle Instability during Running: A Case-Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instrumentation and Measurement Protocols
2.3. Data Analysis
2.4. Statistical Analysis
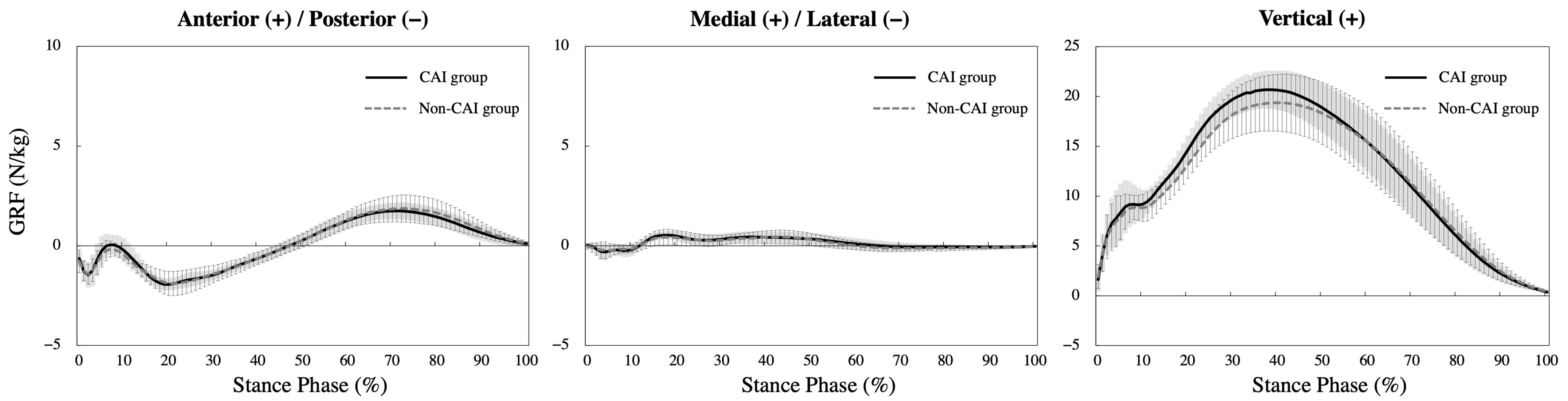
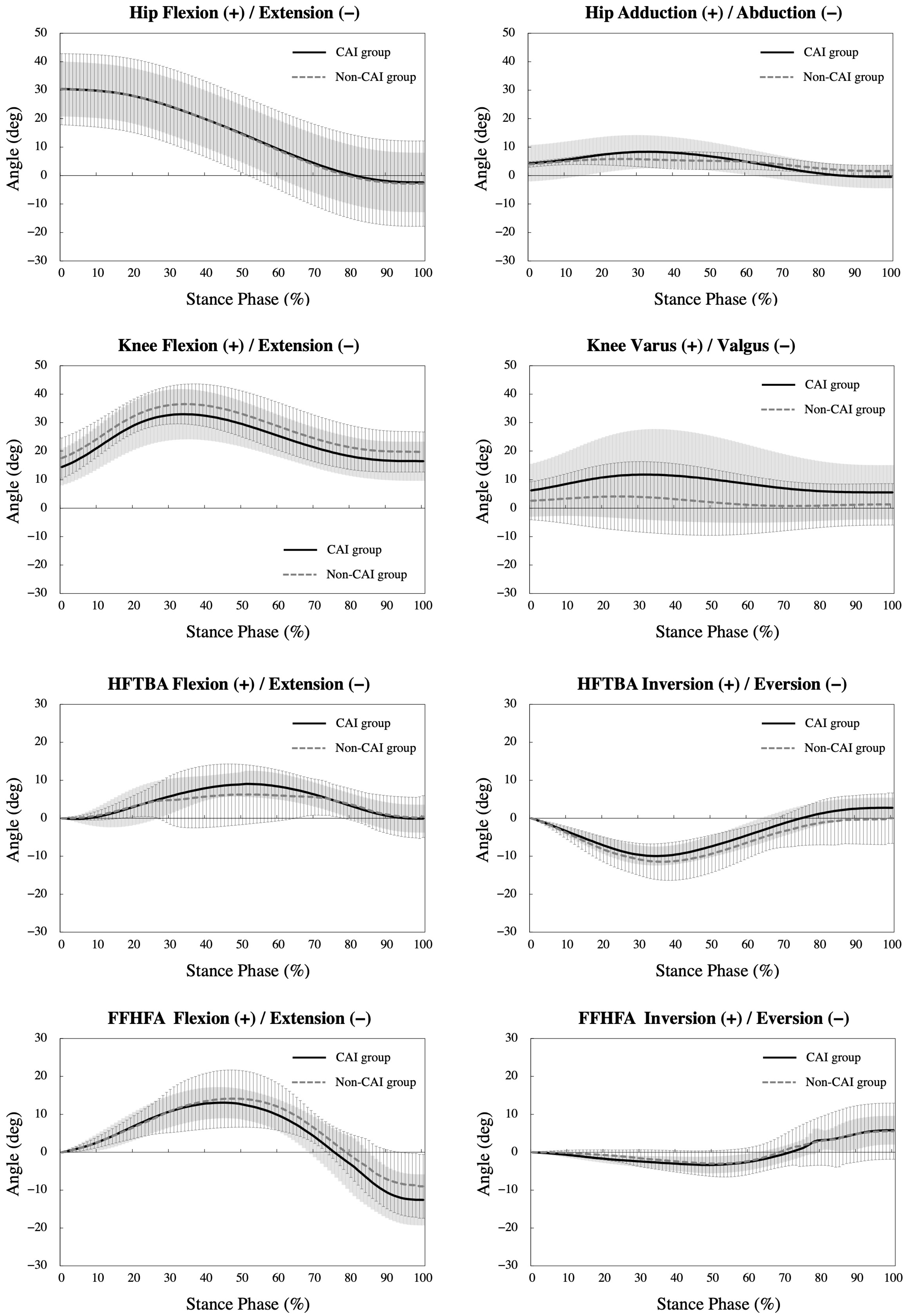
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Woods, C.; Hawkins, R.; Hulse, M. The Football Association Medical Research Programme: An audit of injuries in professional football: An analysis of ankle sprains. Br. J. Sports Med. 2003, 37, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.T.P.; Hong, Y.; Chan, L.K.; Yung, P.S.H.; Chan, K.M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007, 37, 73–94. [Google Scholar] [CrossRef] [PubMed]
- Dvorak, J.; Junge, A.; Derman, W.; Schwellnus, M. Injuries and illnesses of football players during the 2010 FIFA World Cup. Br. J. Sports Med. 2011, 45, 626–630. [Google Scholar] [CrossRef] [PubMed]
- Jain, N.; Murray, D.; Kemp, S.; Calder, J. Frequency and trends in foot and ankle injuries within an English Premier League Football Club using a new impact factor of injury to identify a focus for injury prevention. Foot Ankle Surg. 2014, 20, 237–240. [Google Scholar] [CrossRef]
- Sitler, M.; Ryan, J.; Wheeler, B.; McBride, J.; Arciero, R.; Anderson, J.; Horodyski, M. The efficacy of a semirigid ankle stabilizer to reduce acute ankle injuries in basketball. A randomized clinical study at West Point. Am. J. Sports Med. 1994, 22, 454–461. [Google Scholar] [CrossRef]
- Hertel, J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar]
- Hiller, C.E.; Nightingale, E.J.; Lin, C.W.C.; Coughlan, G.F.; Caulfield, B.; Delahunt, E. Characteristics of people with recurrent ankle sprains: A systematic review with meta-analysis. Br. J. Sports Med. 2011, 45, 660–672. [Google Scholar] [CrossRef]
- Tanen, L.; Docherty, C.L.; Van Der Pol, B.; Simon, J.; Schrader, J. Prevalence of chronic ankle instability in high school and division I athletes. Foot Ankle Spec. 2014, 7, 37–44. [Google Scholar] [CrossRef]
- Hiller, C.E.; Kilbreath, S.L.; Refshauge, K.M. Chronic ankle instability: Evolution of the model. J. Athl. Train. 2011, 46, 133–141. [Google Scholar] [CrossRef]
- Doherty, C.; Bleakley, C.; Hertel, J.; Caulfield, B.; Ryan, J.; Delahunt, E. Recovery From a First-Time Lateral Ankle Sprain and the Predictors of Chronic Ankle Instability: A Prospective Cohort Analysis. Am. J. Sports Med. 2016, 44, 995–1003. [Google Scholar] [CrossRef]
- Tropp, H. Commentary: Functional Ankle Instability Revisited. J. Athl. Train. 2002, 37, 512. [Google Scholar]
- Tamura, A.; Shimura, K.; Inoue, Y. Hip Flexibility and Dynamic Balance Ability in Soccer Players with Functional Ankle Instability. Trauma Care 2021, 1, 206–214. [Google Scholar] [CrossRef]
- McCann, R.S.; Terada, M.; Kosik, K.B.; Gribble, P.A. Landing Kinematics and Isometric Hip Strength of Individuals With Chronic Ankle Instability. Foot Ankle Int. 2019, 40, 969–977. [Google Scholar] [CrossRef]
- Khalaj, N.; Vicenzino, B.; Smith, M.D. Hip and knee muscle torque and its relationship with dynamic balance in chronic ankle instability, copers and controls. J. Sci. Med. Sport 2021, 24, 647–652. [Google Scholar] [CrossRef]
- Monaghan, K.; Delahunt, E.; Caulfield, B. Ankle function during gait in patients with chronic ankle instability compared to controls. Clin. Biomech. 2006, 21, 168–174. [Google Scholar] [CrossRef]
- Delahunt, E.; Monaghan, K.; Caulfield, B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am. J. Sports Med. 2006, 34, 1970–1976. [Google Scholar] [CrossRef]
- Koldenhoven, R.M.; Hart, J.; Saliba, S.; Abel, M.F.; Hertel, J. Gait kinematics & kinetics at three walking speeds in individuals with chronic ankle instability and ankle sprain copers. Gait Posture 2019, 74, 169–175. [Google Scholar] [CrossRef]
- Lorenzo-Martinez, M.; Kalén, A.; Rey, E.; López-Del Campo, R.; Resta, R.; Lago-Peñas, C. Do elite soccer players cover less distance when their team spent more time in possession of the ball? Sci. Med. Footb. 2020, 5, 310–316. [Google Scholar] [CrossRef]
- Aquino, R.; Gonçalves, L.G.; Galgaro, M.; Santi Maria, T.; Rostaiser, E.; Pastor, A.; Nobari, H.; Rodrigues Garcia, G.; Viana Moraes-Neto, M.; Nakamura, F.Y. Match running performance in Brazilian professional soccer players: Comparisons between successful and unsuccessful teams. BMC Sports Sci. Med. Rehabil. 2021, 13, 93. [Google Scholar] [CrossRef]
- Curtis, R.M.; Huggins, R.A.; Looney, D.P.; West, C.A.; Fortunati, A.; Fontaine, G.J.; Casa, D.J. Match Demands of National Collegiate Athletic Association Division I Men’s Soccer. J. strength Cond. Res. 2018, 32, 2907–2917. [Google Scholar] [CrossRef]
- Koldenhoven, R.M.; Hart, J.; Abel, M.F.; Saliba, S.; Hertel, J. Running gait biomechanics in females with chronic ankle instability and ankle sprain copers. Sport. Biomech. 2021, 21, 447–459. [Google Scholar] [CrossRef] [PubMed]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The Cumberland Ankle Instability Tool: A Report of Validity and Reliability Testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar] [CrossRef]
- Kunugi, S.; Masunari, A.; Noh, B.; Mori, T.; Yoshida, N.; Miyakawa, S. Cross-cultural adaptation, reliability, and validity of the Japanese version of the Cumberland ankle instability tool. Disabil. Rehabil. 2017, 39, 50–58. [Google Scholar] [CrossRef]
- De Noronha, M.; Refshauge, K.M.; Crosbie, J.; Kilbreath, S.L. Relationship between functional ankle instability and postural control. J. Orthop. Sports Phys. Ther. 2008, 38, 782–789. [Google Scholar] [CrossRef] [PubMed]
- Tamura, A.; Akasaka, K.; Otsudo, T.; Shiozawa, J.; Toda, Y.; Yamada, K. Dynamic knee valgus alignment influences impact attenuation in the lower extremity during the deceleration phase of a single-leg landing. PLoS ONE 2017, 12, e0179810. [Google Scholar] [CrossRef]
- Carson, M.C.; Harrington, M.E.; Thompson, N.; O’Connor, J.J.; Theologis, T.N. Kinematic analysis of a multi-segment foot model for research and clinical applications: A repeatability analysis. J. Biomech. 2001, 34, 1299–1307. [Google Scholar] [CrossRef]
- Stebbins, J.; Harrington, M.; Thompson, N.; Zavatsky, A.; Theologis, T. Repeatability of a model for measuring multi-segment foot kinematics in children. Gait Posture 2006, 23, 401–410. [Google Scholar] [CrossRef]
- Lobb, N.J.; Fain, A.L.C.; Seymore, K.D.; Brown, T.N. Sex and stride length impact leg stiffness and ground reaction forces when running with body borne load. J. Biomech. 2019, 86, 96–101. [Google Scholar] [CrossRef]
- Moisan, G.; Mainville, C.; Descarreaux, M.; Cantin, V. Lower limb biomechanics in individuals with chronic ankle instability during gait: A case-control study. J. Foot Ankle Res. 2021, 14, 36. [Google Scholar] [CrossRef]
- Hoch, M.C.; McKeon, P.O. Peroneal reaction time after ankle sprain: A systematic review and meta-analysis. Med. Sci. Sports Exerc. 2014, 46, 546–556. [Google Scholar] [CrossRef]
- John, C.T.; Seth, A.; Schwartz, M.H.; Delp, S.L. Contributions of muscles to mediolateral ground reaction force over a range of walking speeds. J. Biomech. 2012, 45, 2438. [Google Scholar] [CrossRef] [PubMed]
- Vaverka, F.; Elfmark, M.; Svoboda, Z.; Janura, M. System of gait analysis based on ground reaction force assessment. Acta Gymnica 2015, 45, 187–193. [Google Scholar] [CrossRef]
- Wannop, J.W.; Worobets, J.T.; Stefanyshyn, D.J. Normalization of ground reaction forces, joint moments, and free moments in human locomotion. J. Appl. Biomech. 2012, 28, 665–676. [Google Scholar] [CrossRef] [PubMed]
- Orendurff, M.S.; Segal, A.D.; Klute, G.K.; Berge, J.S.; Rohr, E.S.; Kadel, N.J. The effect of walking speed on center of mass displacement. J. Rehabil. Res. Dev. 2004, 41, 829–834. [Google Scholar] [CrossRef]
- Caderby, T.; Yiou, E.; Peyrot, N.; Begon, M.; Dalleau, G. Influence of gait speed on the control of mediolateral dynamic stability during gait initiation. Influence of gait speed on the control of mediolateral dynamic stability during gait initiation. J. Biomech. 2014, 47, 417–423. [Google Scholar] [CrossRef]
- Wilson, E.L.; Madigan, M.L. Effects of fatigue and gender on peroneal reflexes elicited by sudden ankle inversion. J. Electromyogr. Kinesiol. 2007, 17, 160–166. [Google Scholar] [CrossRef]
- Sinclair, J.; Greenhalgh, A.; Edmundson, C.J.; Brooks, D.; Hobbs, S.J. Gender Differences in the Kinetics and Kinematics of Distance Running: Implications for Footwear Design. Int. J. Sports Sci. Eng. 2012, 6, 118–128. [Google Scholar]
- Sakaguchi, M.; Ogawa, H.; Shimizu, N.; Kanehisa, H.; Yanai, T.; Kawakami, Y. Gender differences in hip and ankle joint kinematics on knee abduction during running. Eur. J. Sport Sci. 2014, 14 (Suppl. 1), S302–S309. [Google Scholar] [CrossRef]
- Taylor, J.B.; Wright, A.A.; Dischiavi, S.L.; Townsend, M.A.; Marmon, A.R. Activity Demands During Multi-Directional Team Sports: A Systematic Review. Sports Med. 2017, 47, 2533–2551. [Google Scholar] [CrossRef]
- Baker, R.; Robb, J. Foot models for clinical gait analysis. Gait Posture 2006, 23, 399–400. [Google Scholar] [CrossRef]
- Bruening, D.A.; Cooney, K.M.; Buczek, F.L. Analysis of a kinetic multi-segment foot model part II: Kinetics and clinical implications. Gait Posture 2012, 35, 535–540. [Google Scholar] [CrossRef]
| CAI Group | Non-CAI Group | p Value | |
|---|---|---|---|
| Mean ± SD a | Mean ± SD a | ||
| Number | 12 | 10 | - |
| CAIT score | 23.6 ± 4.3 | 29.6 ± 0.8 | - |
| Age (years) | 20.6 ± 0.9 | 20.8 ± 0.9 | 0.54 |
| Height (cm) | 173.7 ± 5.3 | 172.1 ± 5.5 | 0.46 |
| Weight (kg) | 66.5 ± 4.9 | 64.5 ± 6.5 | 0.12 |
| Playing experience (years) | 9.8 ± 2.4 | 10.7 ± 2.7 | 0.36 |
| CAI | Non-CAI | Mean Difference (95% CI b) | t Value | p Value | Effect Size Cohen’s d | ||
|---|---|---|---|---|---|---|---|
| Mean ± SD a | Mean ± SD a | ||||||
| GRF c, N/kg | |||||||
| Anterior (−)/Posterior (+) | 2.11 ± 0.37 | 1.94 ± 2.73 | 1.8 (−3.0–6.6) | 0.78 | 0.45 | 0.35 | |
| Medial (−)/Lateral (+) | 0.55 ± 0.24 | 0.46 ± 0.22 | 0.9 (−1.2–2.9) | 0.89 | 0.38 | 0.41 | |
| Vertical | 20.85 ± 1.70 | 19.54 ± 2.74 | 13.1 (−6.8–33.0) | 1.37 | 0.19 | 0.59 | |
| CAI | Non-CAI | Mean Difference (95% CI b) | t Value | p Value | Effect Size Cohen’s d | |||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD a | Mean ± SD a | |||||||
| Hip, deg | ||||||||
| Flexion | 30.5 ± 9.6 | 30.3 ± 12.5 | 0.2 (−9.6–10.0) | 0.04 | 0.97 | 0.17 | ||
| Adduction | 8.5 ± 5.7 | 10.3 ± 2.6 | −1.8 (−5.7–2.2) | −0.96 | 0.35 | −0.38 | ||
| Internal Rotation | 18.4 ± 24.0 | 7.4 ± 21.8 | 11.0 (−9.5–31.6) | 1.12 | 0.28 | 0.48 | ||
| Knee, deg | ||||||||
| Flexion | 33.2 ± 8.6 | 36.7 ± 6.9 | −3.5 (−10.6–3.5) | −1.05 | 0.31 | −0.45 | ||
| Varus | 13.2 ± 14.6 | 6.2 ± 10.5 | 7.0 (−4.5–18.5) | 1.27 | 0.22 | 0.54 | ||
| Internal Rotation | 2.9 ± 12.0 | 0.6 ± 16.7 | 2.2 (−10.6–15.0) | 0.36 | 0.72 | 0.16 | ||
| Ankle and Foot, deg | ||||||||
| Ankle Dorsi Flexion | 24.4 ± 9.1 | 24.5 ± 5.5 | −0.2 (−7.0–6.7) | −0.05 | 0.96 | −0.02 | ||
| HFTBA c Dorsi Flexion | 9.4 ± 3.2 | 8.4 ± 5.2 | 1.0 (−2.8–4.8) | 0.57 | 0.58 | 0.24 | ||
| HFTBA c Inversion | −10.3 ± 2.6 | −12.7 ± 4.9 | 2.4 (−1.5–3.2) | 1.47 | 0.16 | 0.63 | ||
| FFHFA d Dorsi Flexion | 13.5 ± 4.2 | 14.6 ± 7.2 | −1.1 (−6.2–4.0) | −0.44 | 0.66 | −0.19 | ||
| FFHFA d Inversion | −4.0 ± 1.8 | −4.5 ± 3.5 | 0.5 (−3.9–4.7) | 0.47 | 0.65 | 0.20 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tamura, A.; Shimura, K.; Inoue, Y. Lower-Extremity Kinematics of Soccer Players with Chronic Ankle Instability during Running: A Case-Control Study. Biomechanics 2023, 3, 93-102. https://doi.org/10.3390/biomechanics3010009
Tamura A, Shimura K, Inoue Y. Lower-Extremity Kinematics of Soccer Players with Chronic Ankle Instability during Running: A Case-Control Study. Biomechanics. 2023; 3(1):93-102. https://doi.org/10.3390/biomechanics3010009
Chicago/Turabian StyleTamura, Akihiro, Keita Shimura, and Yuri Inoue. 2023. "Lower-Extremity Kinematics of Soccer Players with Chronic Ankle Instability during Running: A Case-Control Study" Biomechanics 3, no. 1: 93-102. https://doi.org/10.3390/biomechanics3010009
APA StyleTamura, A., Shimura, K., & Inoue, Y. (2023). Lower-Extremity Kinematics of Soccer Players with Chronic Ankle Instability during Running: A Case-Control Study. Biomechanics, 3(1), 93-102. https://doi.org/10.3390/biomechanics3010009






