Spatial Analysis of Different Clinical Forms of Leishmaniasis in Honduras from 2009 to 2016
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area and Data
2.2. Leishmaniasis Morbidity Analysis
2.3. Spatial Analysis
3. Results
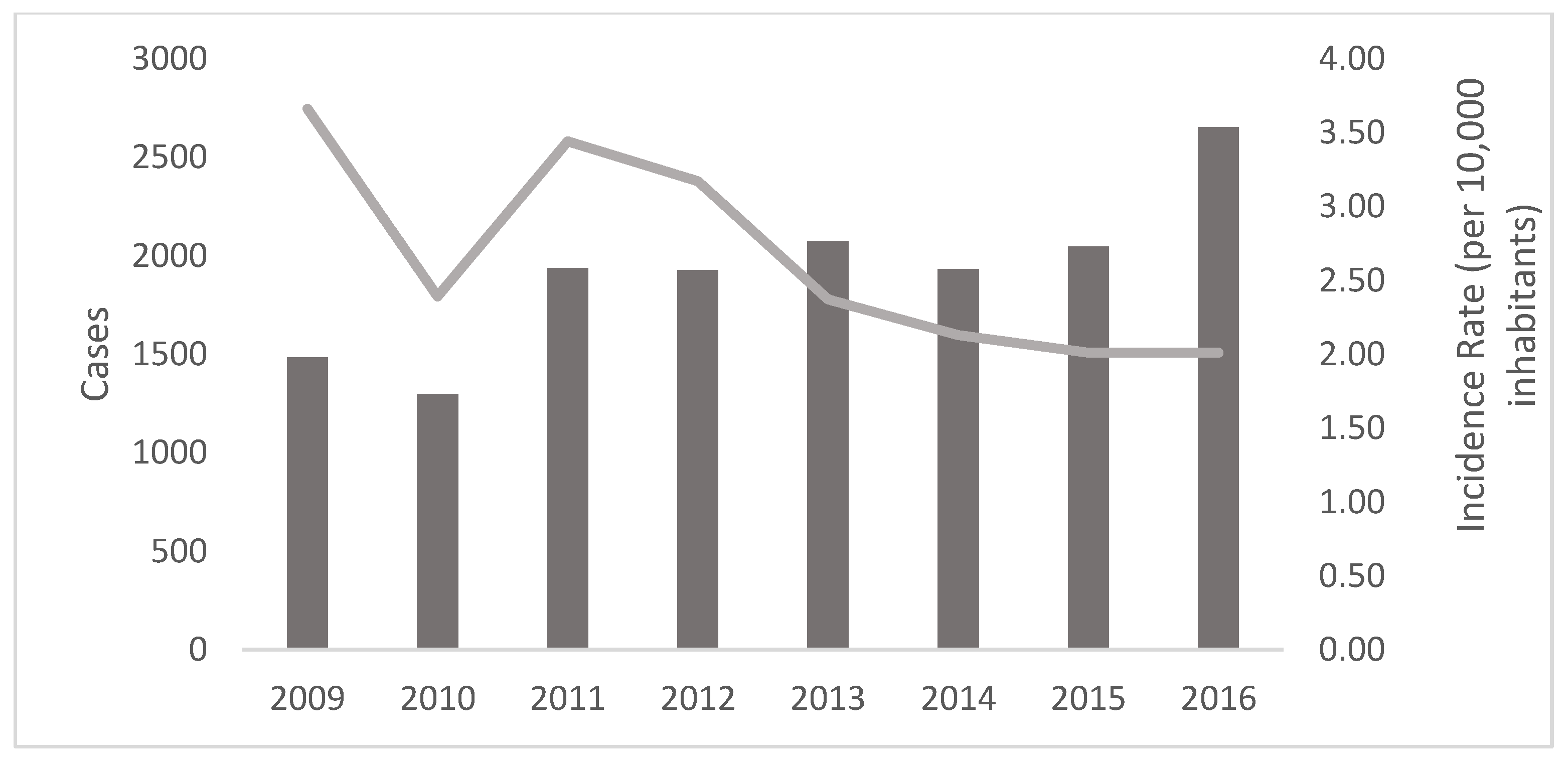
3.1. Distribution of Cases and Incidence
3.2. Age and Gender
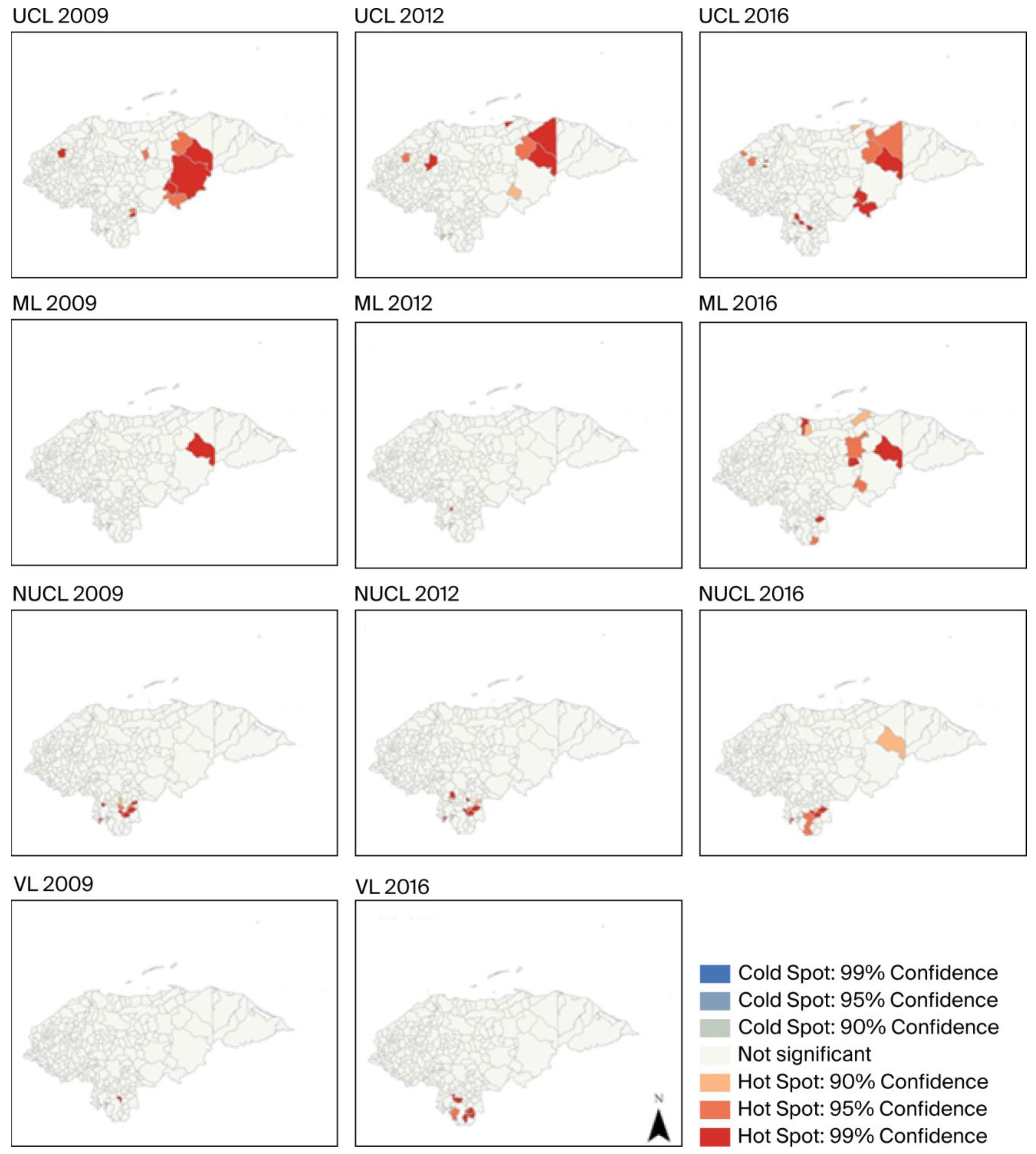
3.3. Hot Spot and Cluster Analysis
3.3.1. Incidence Distribution
3.3.2. Global Spatial Autocorrelation (Global Moran’s I)
3.3.3. Hot Spot Analysis (Getis–Ord Gi*)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| UCL | Ulcerative Cutaneous Leishmaniasis |
| ML | Mucosal Leishmaniasis |
| NUCL | Non-Ulcerated Cutaneous Leishmaniasis |
| VL | Visceral Leishmaniasis |
References
- Jain, S.; Madjou, S.; Junerlyn, F. Global leishmaniasis surveillance updates 2023: 3 years of the NTD road map. Wkly. Epidemiol. Rec. 2024, 45, 653–669. [Google Scholar]
- Alvar, J.; Velez, I.D.; Bern, C.; Herrero, M.; Desjeux, P.; Cano, J.; Jannin, J.; den Boer, M. Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE 2012, 7, e35671. [Google Scholar] [CrossRef]
- Herrera, G.; Teheran, A.; Pradilla, I.; Vera, M.; Ramirez, J.D. Geospatial-temporal distribution of Tegumentary Leishmaniasis in Colombia (2007–2016). PLoS Negl. Trop. Dis. 2018, 12, e0006419. [Google Scholar] [CrossRef]
- Hotez, P.J.; Woc-Colburn, L.; Bottazzi, M.E. Neglected tropical diseases in Central America and Panama: Review of their prevalence, populations at risk and impact on regional development. Int. J. Parasitol. 2014, 44, 597–603. [Google Scholar] [CrossRef]
- Mejia, A.; Matamoros, G.; Fontecha, G.; Sosa-Ochoa, W. Bionomic aspects of Lutzomyia evansi and Lutzomyia longipalpis, proven vectors of Leishmania infantum in an endemic area of non-ulcerative cutaneous leishmaniasis in Honduras. Parasit. Vectors 2018, 11, 15. [Google Scholar] [CrossRef]
- Ponce, C.; Ponce, E.; Morrison, A.; Cruz, A.; Kreutzer, R.; McMahon-Pratt, D.; Neva, F. Leishmania donovani chagasi: New clinical variant of cutaneous leishmaniasis in Honduras. Lancet 1991, 337, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Sosa-Ochoa, W.; Varela Amador, J.; Lozano-Sardaneta, Y.; Rodriguez Segura, G.; Zuniga Valeriano, C.; Araujo, G.V.; Sandoval Pacheco, C.M.; Laurenti, M.D.; Galvis-Ovallos, F. Detection of Leishmania infantum DNA in Pintomyia evansi and Lutzomyia longipalpis in Honduras. Parasit. Vectors 2020, 13, 593. [Google Scholar] [CrossRef] [PubMed]
- Sosa-Ochoa, W.; Zuniga, C.; Chaves, L.F.; Araujo Flores, G.V.; Sandoval Pacheco, C.M.; Ribeiro da Matta, V.L.; Pereira Corbett, C.E.; Tobias Silveira, F.; Dalastra Laurenti, M. Clinical and Immunological Features of Human Leishmania (L.) infantum-Infection, Novel Insights Honduras, Central America. Pathogens 2020, 9, 554. [Google Scholar] [CrossRef] [PubMed]
- Silveira, F.T.; Flores, G.V.A.; Pacheco, C.M.S.; Sosa-Ochoa, W.; Vasconcelos Dos Santos, T.; Sousa, E.C.; Valeriano, C.Z.; da Matta, V.L.; Gomes, C.M.C.; Ramos, P.K.; et al. A comprehensive phenotypic and genotypic taxonomic review of Leishmania (Leishmania) poncei n. sp. (Kinetoplastea: Trypanosomatidae): A novel agent of cutaneous (non-ulcerated) and visceral leishmaniasis in Honduras, Central America. Trop. Dis. Travel. Med. Vaccines 2025, 11, 27. [Google Scholar] [CrossRef] [PubMed]
- Nuernberger, S.; Ramos, C. Leishmaniasis visceral. Informe del primer caso en Honduras. Rev. Médica Hondureña 1974, 42, 234–241. [Google Scholar]
- Risco Oliva, G.E.; Fuentes González, O.; Núñez, F. Leishmaniosis cutánea en la Región Sanitaria No. 3, República de Honduras, enero 1998-Septiembre 2002. Rev. Cuba. Hig. Y Epidemiol. 2009, 47, 27. [Google Scholar]
- Montalvo, A.M.; Fraga, J.; Tirado, D.; Blandon, G.; Alba, A.; Van der Auwera, G.; Velez, I.D.; Muskus, C. Detection and identification of Leishmania spp.: Application of two hsp70-based PCR-RFLP protocols to clinical samples from the New World. Parasitol. Res. 2017, 116, 1843–1848. [Google Scholar] [CrossRef] [PubMed]
- Neva, F.A.; Ponce, C.; Ponce, E.; Kreutzer, R.; Modabber, F.; Olliaro, P. Non-ulcerative cutaneous leishmaniasis in Honduras fails to respond to topical paromomycin. Trans. R. Soc. Trop. Med. Hyg. 1997, 91, 473–475. [Google Scholar] [CrossRef] [PubMed]
- Estadística, I.N.d.; Presidencial, H.S.d.E.e.e.D. XVI Censo de Población y V de Vivienda: Características Económicas de la Población Interrelacionadas; Instituto Nacional de Estadística: Madrid, Spain, 2002; Volume 5. [Google Scholar]
- Secretaria de Salud. Manual Para el Abordaje Integral de Las Leishmaniasis en Honduras, 12016th ed.; Montalvan, W., Medina Ramos, F., Mercedes Tercero, D., Fajardo, G.E., Eds.; Línea Creatica: Tegucigalpa, Honduras, 2016; Volume 89. [Google Scholar]
- ESRI. How Hot Spot Analysis (Getis-Ord Gi*) Works. Available online: https://pro.arcgis.com/en/pro-app/latest/tool-reference/spatial-statistics/h-how-hot-spot-analysis-getis-ord-gi-spatial-stati.htm (accessed on 8 March 2023).
- Hotez, P.J.; Remme, J.H.; Buss, P.; Alleyne, G.; Morel, C.; Breman, J.G. Combating tropical infectious diseases: Report of the Disease Control Priorities in Developing Countries Project. Clin. Infect. Dis. 2004, 38, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Cincura, C.; de Lima, C.M.F.; Machado, P.R.L.; Oliveira-Filho, J.; Glesby, M.J.; Lessa, M.M.; Carvalho, E.M. Mucosal leishmaniasis: A Retrospective Study of 327 Cases from an Endemic Area of Leishmania (Viannia) braziliensis. Am. J. Trop. Med. Hyg. 2017, 97, 761–766. [Google Scholar] [CrossRef]
- Augusto de Oliveira Guerra, J.; Vale Barbosa Guerra, M.D.G.; Vasconcelos, Z.S.; da Silva Freitas, N.; Rodrigues Fonseca, F.; Celso Andrade da Silva Júnior, R.; Soares da Silva, A.; Sampaio, V.; Gonçalves Maciel, M.; de Sousa Melo Cavalcante, M.; et al. Socioenvironmental aspects of the Purus Region—Brazilian Amazon: Why relate them to the occurrence of American Tegumentary Leishmaniasis? PLoS ONE 2019, 14, e0211785. [Google Scholar] [CrossRef] [PubMed]
- Medina-Morales, D.A.; Machado-Duque, M.E.; Machado-Alba, J.E. Epidemiology of Cutaneous Leishmaniasis in a Colombian Municipality. Am. J. Trop. Med. Hyg. 2017, 97, 1503–1507. [Google Scholar] [CrossRef]
- Maia-Elkhoury, A.N.S.; EYadón, Z.; Idali Saboyá Díaz, M.; de Fátima de Araújo Lucena, F.; Gerardo Castellanos, L.; JSanchez-Vazquez, M. Exploring Spatial and Temporal Distribution of Cutaneous Leishmaniasis in the Americas, 2001–2011. PLoS Negl. Trop. Dis. 2016, 10, e0005086. [Google Scholar] [CrossRef]
- Noyes, H.; Chance, M.; Ponce, C.; Ponce, E.; Maingon, R. Leishmania chagasi: Genotypically similar parasites from Honduras cause both visceral and cutaneous leishmaniasis in humans. Exp. Parasitol. 1997, 85, 264–273. [Google Scholar] [CrossRef]
- Belli, A.; Garcia, D.; Palacios, X.; Rodriguez, B.; Valle, S.; Videa, E.; Tinoco, E.; Marin, F.; Harris, E. Widespread atypical cutaneous Leishmaniasis caused by Leishmania (L.) chagasi in Nicaragua. Am. J. Trop. Med. Hyg. 1999, 61, 380–385. [Google Scholar] [CrossRef]
- Convit, J.; Ulrich, M.; Pérez, M.; Hung, J.; Castillo, J.; Rojas, H.; Viquez, A.; Araya, L.N.; Lima, H.D. Atypical cutaneous leishmaniasis in Central America: Possible interaction between infectious and environmental elements. Trans. R. Soc. Trop. Med. Hyg. 2005, 99, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Zeledon, R.; Hidalgo, H.; Viquez, A.; Urbina, A. Atypical cutaneous leishmaniasis in a semiarid region of north-west Costa Rica. Trans. R. Soc. Trop. Med. Hyg. 1989, 83, 786. [Google Scholar] [CrossRef] [PubMed]
- Salvioni, O.D.; Pereira, J.; Sander, M.; Gómez, C. Molecular detection of Leishmania infantum in atypical cutaneous lesions from Paraguayan patients. J. Dermatol. Clin. Res. 2017, 3, 1104. [Google Scholar]
- Sandoval Pacheco, C.M.; Araujo Flores, G.V.; Favero Ferreira, A.; Sosa Ochoa, W.; Ribeiro da Matta, V.L.; Zuniga Valeriano, C.; Pereira Corbett, C.E.; Dalastra Laurenti, M. Histopathological features of skin lesions in patients affected by non-ulcerated or atypical cutaneous leishmaniasis in Honduras, Central America. Int. J. Exp. Pathol. 2018, 99, 249–257. [Google Scholar] [CrossRef]
- Sosa-Ochoa, W.; Zuniga, C.; Flores, G.V.A.; Pacheco, C.M.S.; Corbett, C.E.P.; Silveira, F.T.; Laurenti, M.D. Cohort study of human infection by Leishmania (L.) infantum chagasi in southern Honduras, Central America. Trans. R. Soc. Trop. Med. Hyg. 2025. [Google Scholar] [CrossRef]
- Araujo Flores, G.V.; Sandoval Pacheco, C.M.; Tomokane, T.Y.; Sosa Ochoa, W.; Zuniga Valeriano, C.; Castro Gomes, C.M.; Corbett, C.E.P.; Laurenti, M.D. Evaluation of Regulatory Immune Response in Skin Lesions of Patients Affected by Nonulcerated or Atypical Cutaneous Leishmaniasis in Honduras, Central America. Mediat. Inflamm. 2018, 2018, 3487591. [Google Scholar] [CrossRef]
- Cardoso, C.A.; Araujo, G.V.; Sandoval, C.M.; Nogueira, P.M.; Zuniga, C.; Sosa-Ochoa, W.H.; Laurenti, M.D.; Soares, R.P. Lipophosphoglycans from dermotropic Leishmania infantum are more pro-inflammatory than those from viscerotropic strains. Mem. Inst. Oswaldo Cruz. 2020, 115, e200140. [Google Scholar] [CrossRef]
- Carrasco, J.; Morrison, A.; Ponce, C. Behaviour of Lutzomyia longipalpis in an area of southern Honduras endemic for visceral/atypical cutaneous leishmaniasis. Ann. Trop. Med. Parasitol. 1998, 92, 869–876. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, J.G.; Ward, R.D.; Dougherty, M.J.; Maignon, R.; Ponce, C.; Ponce, E.; Noyes, H.; Zeledon, R. Comparison of the sex-pheromone components of Lutzomyia longipalpis (Diptera: Psychodidae) from areas of visceral and atypical cutaneous leishmaniasis in Honduras and Cost Rica. Ann. Trop. Med. Parasitol. 1996, 90, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Chaves, L.F.; Pascual, M. Climate cycles and forecasts of cutaneous leishmaniasis, a nonstationary vector-borne disease. PLoS Med. 2006, 3, e295. [Google Scholar] [CrossRef] [PubMed]
- González, K.; Calzada, J.E.; Saldaña, A.; Rigg, C.A.; Alvarado, G.; Rodríguez-Herrera, B.; Kitron, U.D.; Adler, G.H.; Gottdenker, N.L.; Chaves, L.F.; et al. Survey of wild mammal hosts of cutaneous leishmaniasis parasites in panamá and costa rica. Trop. Med. Health 2015, 43, 75–78. [Google Scholar] [CrossRef]
- Yamada, K.; Valderrama, A.; Gottdenker, N.; Cerezo, L.; Minakawa, N.; Saldaña, A.; Calzada, J.E.; Chaves, L.F. Macroecological patterns of American Cutaneous Leishmaniasis transmission across the health areas of Panamá (1980–2012). Parasite Epidemiol. Control 2016, 1, 42–55. [Google Scholar] [CrossRef]
- Marchi, M.N.A.; Caldart, E.T.; Martins, F.D.C.; Freire, R.L. Spatial analysis of leishmaniasis in Brazil: A systematized review. Rev. Inst. Med. Trop. 2019, 61, e68. [Google Scholar] [CrossRef]
- de Araujo, V.E.; Pinheiro, L.C.; Almeida, M.C.; de Menezes, F.C.; Morais, M.H.; Reis, I.A.; Assuncao, R.M.; Carneiro, M. Relative risk of visceral leishmaniasis in Brazil: A spatial analysis in urban area. PLoS Negl. Trop. Dis. 2013, 7, e2540. [Google Scholar] [CrossRef]
- Santos, M.F.d.; Lorenz, C.; Chiaravalotti-Neto, F.; Lima-Camara, T.N. Spatial analysis of American cutaneous leishmaniasis in the state of Amazonas. Rev. Saúde Pública 2024, 58, 11. [Google Scholar] [CrossRef]
- Lewnard, J.A.; Jirmanus, L.; Junior, N.N.; Machado, P.R.; Glesby, M.J.; Ko, A.I.; Carvalho, E.M.; Schriefer, A.; Weinberger, D.M. Forecasting temporal dynamics of cutaneous leishmaniasis in Northeast Brazil. PLoS Negl. Trop. Dis. 2014, 8, e3283. [Google Scholar] [CrossRef]
- Franke, C.R.; Staubach, C.; Ziller, M.; Schluter, H. Trends in the temporal and spatial distribution of visceral and cutaneous leishmaniasis in the state of Bahia, Brazil, from 1985 to 1999. Trans. R. Soc. Trop. Med. Hyg. 2002, 96, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Munoz Morales, D.; Suarez Daza, F.; Franco Betancur, O.; Martinez Guevara, D.; Liscano, Y. The Impact of Climatological Factors on the Incidence of Cutaneous Leishmaniasis (CL) in Colombian Municipalities from 2017 to 2019. Pathogens 2024, 13, 462. [Google Scholar] [CrossRef] [PubMed]
- Tarnas, M.C.; Abbara, A.; Desai, A.N.; Parker, D.M. Ecological study measuring the association between conflict, environmental factors, and annual global cutaneous and mucocutaneous leishmaniasis incidence (2005–2022). PLoS Negl. Trop. Dis. 2024, 18, e0012549. [Google Scholar] [CrossRef] [PubMed]
- Carrasco López, B.E. Diversidad de especies Lutzomyia spp. como potenciales vectores de leishmanniasis en las comunidades de San José de la montaña y Nueva Esperanza del municipio de Dulce Nombre de Culmi. Bachelor’s Thesis, Universidad Nacional de Agricultura de Honduras, Catacamas, Honduras, 2011. [Google Scholar]
- Lawyer, P.; Killick-Kendrick, M.; Rowland, T.; Rowton, E.; Volf, P. Laboratory colonization and mass rearing of phlebotomine sand flies (Diptera, Psychodidae). Parasite 2017, 24, 42. [Google Scholar] [CrossRef]
- Castillo-Castaneda, A.; Herrera, G.; Ayala, M.S.; Fuya, P.; Ramirez, J.D. Spatial and Temporal Variability of Visceral Leishmaniasis in Colombia, 2007 to 2018. Am. J. Trop. Med. Hyg. 2021, 105, 144–155. [Google Scholar] [CrossRef] [PubMed]

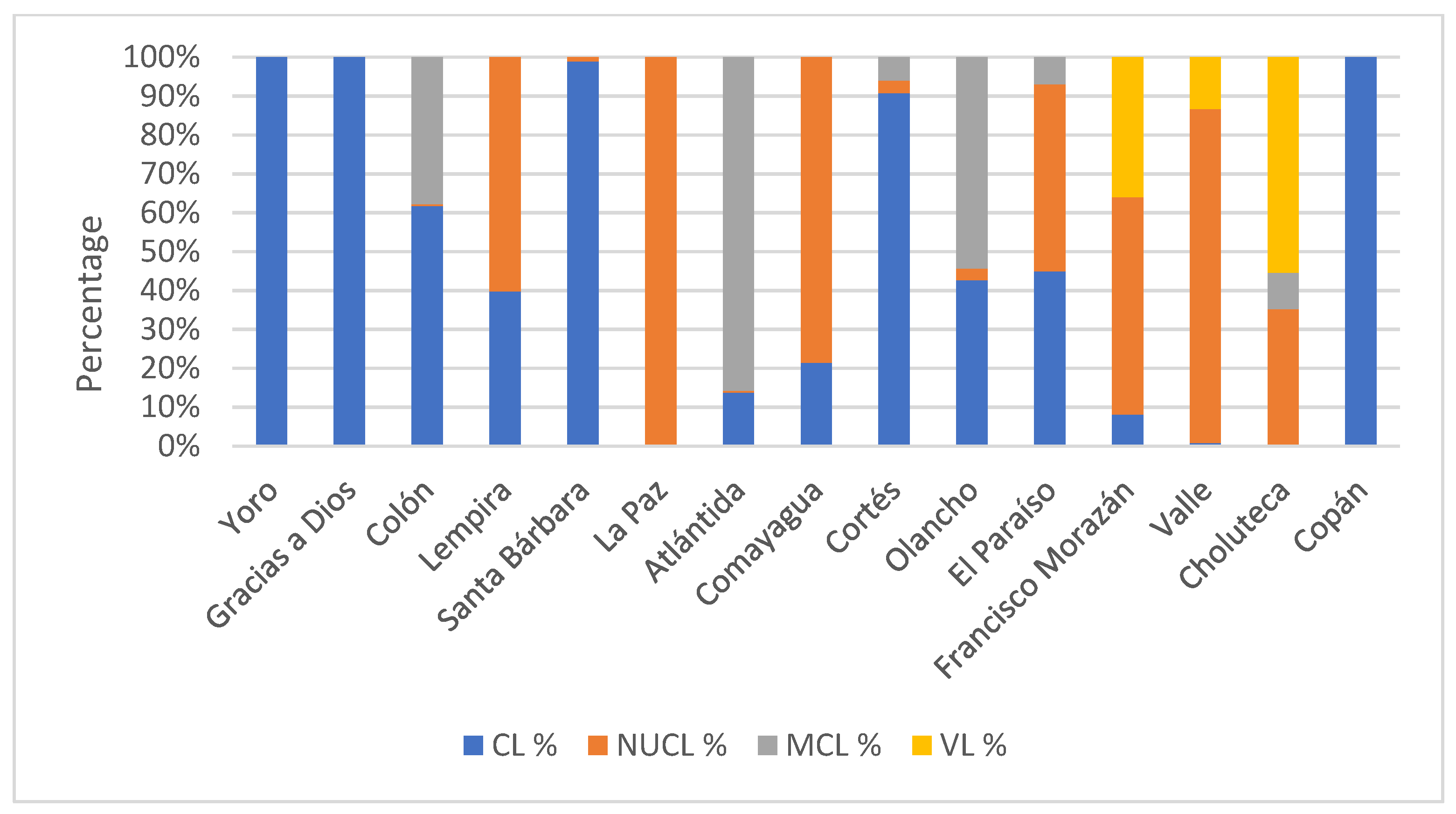

| Department | Total Cases | Incidence Rate | UCL Cases | Incidence Rate | CL % | NUCL Cases | Incidence Rate * | NUCL % | ML Cases | Incidence Rate * | ML % | VL Cases | Incidence Rate * | VL % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yoro | 291 | 5.4 | 291 | 5.4 | 3.2 | 0 | 0.0 | 0.0 | 0 | 0.0 | 0.0 | 0 | 0.0 | 0.0 |
| Gracias a Dios | 18 | 2.3 | 18 | 2.3 | 0.2 | 0 | 0.0 | 0.0 | 0 | 0.0 | 0.0 | 0 | 0.0 | 0.0 |
| Colón | 1315 | 40.1 | 1300 | 39.7 | 14.2 | 7 | 0.2 | 0.1 | 8 | 0.2 | 8.7 | 0 | 0.0 | 0.0 |
| Lempira | 10 | 0.7 | 5 | 0.4 | 0.1 | 5 | 0.4 | 0.1 | 0 | 0.0 | 0.0 | 0 | 0.0 | 0.0 |
| Santa Bárbara | 1074 | 26.2 | 1066 | 26.0 | 11.6 | 8 | 0.2 | 0.1 | 0 | 0.0 | 0.0 | 0 | 0.0 | 0.0 |
| La Paz | 9 | 16.0 | 0 | 0.0 | 0.0 | 9 | 16.0 | 0.1 | 0 | 0.0 | 0.0 | 0 | 0.0 | 0.0 |
| Atlántida | 329 | 7.3 | 302 | 6.7 | 3.3 | 8 | 0.2 | 0.1 | 19 | 0.4 | 20.7 | 0 | 0.0 | 0.0 |
| Comayagua | 24 | 1.0 | 7 | 0.3 | 0.1 | 17 | 0.7 | 0.3 | 0 | 0.0 | 0.0 | 0 | 0.0 | 0.0 |
| Cortés | 1545 | 10.1 | 1508 | 9.9 | 16.5 | 36 | 0.2 | 0.6 | 1 | 0.0 | 1.1 | 0 | 0.0 | 0.0 |
| Olancho | 4064 | 75.2 | 3831 | 70.9 | 41.8 | 184 | 3.4 | 3.0 | 49 | 0.9 | 53.3 | 0 | 0.0 | 0.0 |
| El Paraíso | 1106 | 23.6 | 647 | 13.8 | 7.1 | 458 | 9.8 | 7.6 | 1 | 0.0 | 1.1 | 0 | 0.0 | 0.0 |
| Francisco Morazán | 742 | 5.3 | 133 | 0.9 | 1.5 | 607 | 4.3 | 10.0 | 0 | 0.0 | 0.0 | 2 | 0.0 | 6.5 |
| Valle | 1283 | 71.4 | 16 | 0.9 | 0.2 | 1266 | 70.4 | 20.9 | 0 | 0.0 | 0.0 | 1 | 0.1 | 3.2 |
| Choluteca | 3528 | 79.8 | 36 | 0.8 | 0.4 | 3450 | 78.0 | 57.0 | 14 | 0.3 | 15.2 | 28 | 0.6 | 90.3 |
| Copán | 7 | 0.7 | 7 | 0.7 | 0.1 | 0 | 0.0 | 0.0 | 0 | 0.0 | 0.0 | 0 | 0.0 | 0.0 |
| 15345 | 9167 | 6055 | 92 | 31 |
| General | Females | Males | ||||||
|---|---|---|---|---|---|---|---|---|
| Year | Cases | % | Cases | % | Incidence Rate * | Cases | % | Incidence Rate * |
| 2013 | 2075 | 23.8 | 697 | 21.19 | 1.16 | 1316 | 24.3 | 2.19 |
| 2014 | 1931 | 22.2 | 771 | 23.34 | 1.24 | 1175 | 21.7 | 1.89 |
| 2015 | 2045 | 23.5 | 881 | 26.80 | 1.29 | 1197 | 22.1 | 1.76 |
| 2016 | 2652 | 30.5 | 943 | 28.67 | 1.37 | 1727 | 31.9 | 2.52 |
| Total | 8703 | 100.0 | 3288 | 100 | 5415 | 100 | ||
| Year | <5 Years | 5–9 Years | 10–19 Years | 20–49 Years | >50 Years | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Incidence Rate * | Cases | Incidence Rate * | Cases | Incidence Rate * | Cases | Incidence Rate * | Cases | Incidence Rate * | |
| 2013 | 152 | 1.78 | 252 | 2.95 | 727 | 8.50 | 756 | 8.84 | 202 | 2.36 |
| 2014 | 129 | 1.53 | 190 | 2.25 | 650 | 7.71 | 733 | 8.69 | 199 | 2.36 |
| 2015 | 182 | 2.12 | 165 | 1.92 | 668 | 7.79 | 820 | 9.56 | 225 | 2.62 |
| 2016 | 261 | 2.99 | 282 | 3.23 | 839 | 9.62 | 1027 | 11.78 | 244 | 2.80 |
| Total | 724 | 889 | 2884 | 3336 | 870 | |||||
| Year | UCL | ML | NUCL | VL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moran’s I | z-Score | p-Value | Moran’s I | z-Score | p-Value | Moran’s I | z-Score | p-Value | Moran’s I | z-Score | p-Value | |
| 2009 | 0.039573 | 3.907069 | 0.000093 | 0.010298 | 2.492981 | 0.012668 | 0.146927 | 13.480736 | 0.000000 | −0.003354 | 0.004182 | 0.996663 |
| 2010 | 0.063343 | 6.475721 | 0.000000 | 0.002619 | 1.883818 | 0.059590 | 0.097058 | 9.975942 | 0.000000 | 0.049209 | 5.04188 | 0.000000 |
| 2011 | 0.031314 | 3.869622 | 0.000109 | 0.019649 | 2.671906 | 0.007542 | 0.113616 | 11.585693 | 0.000000 | 0.012615 | 1.895551 | 0.058019 |
| 2012 | 0.044129 | 5.395738 | 0.000000 | −0.005884 | −0.790557 | 0.429203 | 0.146254 | 13.397129 | 0.000000 | ** | ** | ** |
| 2013 | 0.047576 | 4.885245 | 0.000001 | 0.005041 | 0.977825 | 0.328161 | 0.144689 | 14.469943 | 0.000000 | 0.057306 | 6.799102 | 0.000000 |
| 2014 | 0.074792 | 6.841419 | 0.000000 | 0.034964 | 3.805863 | 0.000141 | 0.084995 | 8.677335 | 0.000000 | −0.000563 | 0.882399 | 0.377561 |
| 2015 | 0.070127 | 6.379846 | 0.000000 | 0.015346 | 2.201847 | 0.027676 | 0.144997 | 13.876317 | 0.000000 | 0.003423 | 0.68698 | 0.492096 |
| 2016 | 0.072236 | 6.315367 | 0.000000 | 0.014101 | 1.624236 | 0.104325 | 0.078689 | 8.549363 | 0.000000 | 0.118458 | 11.910415 | 0.000000 |
| Clinical Form Code | Observed General G | Expected General G | Z-Score | p-Value | Statistical Significance | Spatial Pattern Interpretation |
|---|---|---|---|---|---|---|
| NUCL_09 | 0.00003 | 0.000005 | 10.64 | 0 | p < 0.01 | High spatial clustering of elevated values (significant hot spots) |
| NUCL_10 | 0.000029 | 0.000005 | 8.068 | 0 | p < 0.01 | High spatial clustering of elevated values (significant hot spots) |
| NUCL_11 | 0.000034 | 0.000005 | 10.141 | 0 | p < 0.01 | High spatial clustering of elevated values (significant hot spots) |
| NUCL_12 | 0.000029 | 0.000005 | 10.524 | 0 | p < 0.01 | High spatial clustering of elevated values (significant hot spots) |
| NUCL_13 | 0.000032 | 0.000005 | 11.933 | 0 | p < 0.01 | High spatial clustering of elevated values (significant hot spots) |
| NUCL_14 | 0.000024 | 0.000005 | 6.757 | 0 | p < 0.01 | High spatial clustering of elevated values (significant hot spots) |
| NUCL_15 | 0.000032 | 0.000005 | 11.023 | 0 | p < 0.01 | High spatial clustering of elevated values (significant hot spots) |
| NUCL_16 | 0.00002 | 0.000005 | 5.866 | 0 | p < 0.01 | High spatial clustering of elevated values (significant hot spots) |
| UCL_09 | 0.000005 | 0.000005 | −0.376 | 0.70684 | Not significant | Random spatial distribution, no evidence of clustering |
| UCL_10 | 0.00001 | 0.000005 | 2.269 | 0.0233 | p < 0.05 | Moderate clustering of elevated values (weak hot spots) |
| UCL_11 | 0.000005 | 0.000005 | 0.008 | 0.99325 | Not significant | Random spatial distribution |
| UCL_12 | 0.000004 | 0.000005 | −0.777 | 0.4369 | Not significant | Random spatial distribution |
| UCL_13 | 0.000005 | 0.000005 | −0.084 | 0.93281 | Not significant | Random spatial distribution |
| UCL_14 | 0.000007 | 0.000005 | 0.989 | 0.32225 | Not significant | Random spatial distribution |
| UCL_15 | 0.000005 | 0.000005 | 0.172 | 0.86308 | Not significant | Random spatial distribution |
| UCL_16 | 0.000006 | 0.000005 | 0.812 | 0.41657 | Not significant | Random spatial distribution |
| ML_09 | — | — | — | — | Error 000906 | Analysis failed (identical values, zero variance) |
| ML_10 | — | — | — | — | Error 000906 | Analysis failed (identical values, zero variance) |
| ML_11 | 0.000011 | 0.000005 | 0.717 | 0.4736 | Not significant | Random spatial distribution |
| ML_12 | — | — | — | — | Error 000906 | Analysis failed (identical values, zero variance) |
| ML_13 | — | — | — | — | Error 000906 | Analysis failed (identical values, zero variance) |
| ML_14 | 0.000012 | 0.000005 | 1.415 | 0.15694 | Not significant | Random spatial distribution |
| ML_15 | 0.000003 | 0.000005 | −0.491 | 0.62374 | Not significant | Random spatial distribution |
| ML_16 | 0.000009 | 0.000005 | −0.666 | 0.50528 | Not significant | Random spatial distribution |
| LV_09 | — | — | — | — | Error 000906 | Analysis failed (identical values, zero variance) |
| LV_10 | 0.000039 | 0.000005 | 4.038 | 5.4 × 10−5 | p < 0.01 | Significant clustering of elevated values (hot spots) |
| LV_11 | 0.000023 | 0.000005 | 1.984 | 0.04723 | p < 0.05 | Moderate clustering of elevated values (weak hot spots) |
| LV_12 | — | — | — | — | Error 000906 | Analysis failed (identical values, zero variance) |
| LV_13 | 0.000065 | 0.000005 | 5.804 | 0 | p < 0.01 | High spatial clustering of elevated values (significant hot spots) |
| LV_14 | — | — | — | — | Error 000906 | Analysis failed (identical values, zero variance) |
| LV_15 | — | — | — | — | Error 000906 | Analysis failed (identical values, zero variance) |
| LV_16 | 0.00005 | 0.000005 | 9.853 | 0 | p < 0.01 | High spatial clustering of elevated values (significant hot spots) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sosa-Ochoa, W.; Argüello-Vargas, S.; Moraga-López, G.; Ríos-Muñoz, C.A.; Zúñiga, C.; Zambrano, O.N.; Alcántara Henrriquez, E.; Sandoval-Pacheco, C.M.; Araujo-Flores, G.V.; Laurenti, M.D. Spatial Analysis of Different Clinical Forms of Leishmaniasis in Honduras from 2009 to 2016. Parasitologia 2025, 5, 63. https://doi.org/10.3390/parasitologia5040063
Sosa-Ochoa W, Argüello-Vargas S, Moraga-López G, Ríos-Muñoz CA, Zúñiga C, Zambrano ON, Alcántara Henrriquez E, Sandoval-Pacheco CM, Araujo-Flores GV, Laurenti MD. Spatial Analysis of Different Clinical Forms of Leishmaniasis in Honduras from 2009 to 2016. Parasitologia. 2025; 5(4):63. https://doi.org/10.3390/parasitologia5040063
Chicago/Turabian StyleSosa-Ochoa, Wilfredo, Silvia Argüello-Vargas, Geannina Moraga-López, César A. Ríos-Muñoz, Concepción Zúñiga, Orlinder Nicolas Zambrano, Elisa Alcántara Henrriquez, Carmen Maria Sandoval-Pacheco, Gabriela Venicia Araujo-Flores, and Marcia Dalastra Laurenti. 2025. "Spatial Analysis of Different Clinical Forms of Leishmaniasis in Honduras from 2009 to 2016" Parasitologia 5, no. 4: 63. https://doi.org/10.3390/parasitologia5040063
APA StyleSosa-Ochoa, W., Argüello-Vargas, S., Moraga-López, G., Ríos-Muñoz, C. A., Zúñiga, C., Zambrano, O. N., Alcántara Henrriquez, E., Sandoval-Pacheco, C. M., Araujo-Flores, G. V., & Laurenti, M. D. (2025). Spatial Analysis of Different Clinical Forms of Leishmaniasis in Honduras from 2009 to 2016. Parasitologia, 5(4), 63. https://doi.org/10.3390/parasitologia5040063









