Abstract
Background/Objectives: This study aimed to assess whether income was associated with dental caries experience and dental care levels among 12-year-old children in two contrasting economic contexts, Sri Lanka (lower-middle-income) and Wales (high-income), regardless of national income status. Methods: An ecological study design was used with published data. For Sri Lanka, the income parameters used included household income, mean per capita income, and the Gini coefficient. For Wales, the Welsh Index of Multiple Deprivation was used. Dental caries was assessed using the DMFT index and its components (DT, MT, FT), while dental care was assessed using the care index, restorative index, and treatment index. Pearson correlations were used to explore associations between income measures and both caries experience and dental care indices across districts in Sri Lanka and unitary authorities in Wales. Results: The mean DMFT for 12-year-old children was 0.6 in both Sri Lanka and Wales, with caries prevalence of 30.4% and 29.6%, respectively. In Sri Lanka, both mean household income and per capita income showed moderate, statistically significant positive correlations with DMFT (r = 0.47, p = 0.01). Income inequality, measured by the Gini coefficient, was positively associated with caries experience (r = 0.42, p = 0.03). In Wales, higher deprivation (lower income) was moderately associated with increased DMFT, in areas within the 20% (r = 0.54, p < 0.01), 30% (r = 0.53, p < 0.01), and 50% (r = 0.61, p < 0.01) deprived quintiles. The dental care indices showed no clear association with income in either of the countries. Conclusions: Income-related disparities in dental caries were evident in both countries. Prevention strategies should focus on higher-income groups in Sri Lanka and on deprived populations in Wales. However, as this was an ecological study, the results are subject to ecological fallacy and should therefore be interpreted with caution.
1. Introduction
Oral disease is an important global public health issue, with dental caries a preventable but most widespread condition [1]. Dental caries, in addition to edentulism (total tooth loss), periodontal disease, and cancers of the lip and oral cavity, is a main contributor to a global burden of chronic disease [2]. Over 2 billion people globally experience untreated caries in permanent teeth, which is the most prevalent condition worldwide [2]. The g average prevalence of caries globally in permanent teeth is around 29%, with relatively minor differences between countries of varying income levels: 29.3% in high-income countries and 30.6% in low-income countries [2]. The largest number of cases are found in low- to middle-income countries (816 million) and upper-middle-income countries (690 million). Over the last 30 years, the total number of caries cases has increased to about 640 million, in spite of a slight decrease in the overall prevalence (−2.6%), which has been driven primarily by population growth in low- and lower-middle-income countries [2]. Caries has widespread impacts, including productivity losses, missed educational opportunities, and poorer academic performance in school [3].
Oral health is essential to general health, and oral diseases share the same health inequalities and risk factors common to other non-communicable diseases. Socio-economic inequalities in health have remained a public health problem worldwide for decades across countries and among sub-populations within countries [4]. Oral health inequalities in the world are not an exception to general health among populations [5]. The underlying causes of oral health inequalities are complex and are related to country-specific historical, economic, cultural, social, or political factors. A systematic review has reported evidence for socio-economic inequalities in dental caries [6]. Schwendicke et al. [6] reported that low socio-economic position measured via education, occupation, and income was associated with a higher risk of experiencing caries lesions. Furthermore, it was suggested that the association between low educational background and having a dental caries experience—a decayed, missing, or filled tooth (DMFT/dmft > 0)—increased in highly developed countries (R2 = 1.32 [0.53–2.13]) [6].
However, there has been inconclusive evidence on whether the national-level income indicators predict population health. There is evidence showing strong positive associations between average income and population health status, which is demonstrated both across countries and within countries [7]. The correlation between average income and health indicators, such as life expectancy and mortality rate, appears to be weak in developed countries [7]. However, this relationship is more pronounced in less developed nations compared to their developed counterparts [7]. Population health parameters, particularly in developed countries, appear to be more strongly tied to income inequality rather than absolute income levels [8]. Studies related to the relationship between aggregate income measures and oral health parameters in the population are scarce. One study by Bernabe et al. [8] reports that the income measures of Gross Domestic Product (GDP) and Gross National Income (GNI) were not related to either dental caries or dental care levels among the 35–44-year-old adults in higher income countries included in their study. However, it was reported that income inequality measures (the Gini coefficient) were inversely and significantly associated with the number of filled teeth, DMFT, the care index, and the restorative index [8].
This study hypothesizes that caries experience and dental care levels are correlated with inequality of income despite the income status of the country. Moreover, it is hypothesized that dental caries experience and dental care levels are correlated with inequality of income in a high-income country, and secondly, that both income and income inequality are linked to caries experience and dental care in a lower-middle-income country. This study focuses on 12-year-old children in Wales (a high-income country) and Sri Lanka (a lower-middle-income country) and uses this age group as a global indicator for international comparisons of oral health, recommended by the World Health Organization [9].
2. Materials and Methods
Ethical clearance for the study was obtained from the Low-Risk Ethics Review Committee of the Faculty of Life Sciences and Education, University of South Wales (230289LR).
This is an ecological study that compares the correlation between income metrics and dental caries experience among 12-year-old children in two countries having different socio-economic backgrounds. The data for this study were extracted from published data related to income and oral health metrics in the two countries. Since the most recent data on dental caries experience and prevalence in Sri Lanka and Wales were from reports for the years 2015/2016 and 2016/2017, respectively, the 2016 income data were used for comparison. For Wales, income-related measures from the Welsh Index of Multiple Deprivation (WIMD) were last reported in 2014, and no updated dataset was available for the same year as the oral health survey. Therefore, the 2014 WIMD data were used as the closest available proxy to align with the 2015/2016 oral health dataset. While the use of data from different years may introduce a minor temporal mismatch, this approach ensured the most up-to-date and comparable data sources were utilized. Oral health-related variables and income-related variables were compared across the 25 districts of Sri Lanka and the 22 unitary authorities of Wales [10].
Exposure variables: The household income and mean per capita household income for each district in Sri Lanka were extracted as a measure of absolute income variables, while the Gini coefficient of per capita income for each district was extracted as a measure of the relative income variable. Both absolute and relative income data for Sri Lanka were obtained from the “Household Income and Expenditure Survey 2016” report, published by the Department of Census and Statistics in Sri Lanka [11].
For Wales, the income data were taken from the “Welsh Index of Multiple Deprivation (WIMD) 2014 revised,” which is a measure of relative income [10]. WIMD, the official measure of relative deprivation for small geographical areas in Wales, identifies areas with the highest deprivation across eight domains: income, housing, community safety, employment, health, access to services, education, and the physical environment. This study does not seek to compare the absolute income data, such as household income or household per capita income, related to Wales.
Outcome variables: National statistics on the level of dental caries for 12-year-old children for Sri Lanka were obtained from the National Oral Health Survey report published in 2015/2016 [12]. The data extracted were prevalence of dental caries and dental caries experience, which were expressed as the population mean for the number of decayed (DT), missing (MT), and filled (FT) teeth, or the DMFT index for each district. Based on the data collected by the DMFT index, three indices of dental care were calculated as an estimate of the proportion of caries that had been treated as well as the type of treatment that was provided. These indices were the care index, which was calculated using the formula 100FT/DMFT%; the restorative index, which was calculated using the formula 100FT/(DT + FT) %; and the treatment index, which was calculated using the formula 100(MT + FT)/DMFT%.
For Wales, the data were extracted from the oral health survey reports published by the Welsh Oral Health Information Unit at Cardiff University [13]. The report contained the data calculated for all dental care indices. The most recent nationally available oral health data for 12-year-olds in Wales were published for 2015/2016.
Data analysis: Pearson correlations were used to provide estimates of the linear association of each income measure with the DMFT index and the components of this index (DT, MT, and FT) as well as with the three dental care indices for each unitary authority in Wales and each district in Sri Lanka. Scatter plots were used to check the form of associations. The strength of the correlations was interpreted according to Cohen’s guidelines, with coefficients classified as mild (r ≈ 0.10), moderate (r ≈ 0.30), and strong (r ≈ 0.50). The data were analyzed using Jamovi (Version 2.7.6).
3. Results
Wales is situated within the United Kingdom and is considered to be a comparatively small country with an estimated usual resident population of 3,077,200. In 2016 its gross domestic product per capita (GDP) amounted to approximately USD 10,743.9 [14]. The prevalence of dental caries (% D3MFT > 0) among 12-year-old children in Wales in the 2016/2017 academic year was 29.6% and the mean DMFT was 0.6 [13]. By contrast, Sri Lanka, with a population of 2.43 million and a GDP of USD 4,107.83 in 2016 [11], had a prevalence of dental caries (% DMFT > 0) among 12-year-olds of 30.4%, according to the National Oral Health Survey report 2015/2016 [12]. The dental caries experience (DMFT) of 12-year-olds was reported as 0.6 in Sri Lanka [12].
A comparative analysis of the prevalence of dental caries and the severity of dental caries in the two countries and their respective most and least deprived (socio-economic status) unitary authorities/districts is presented in Table 1.

Table 1.
Twelve-year-old children with dental caries experience in Wales and Sri Lanka.
In Sri Lanka, mean DMFT was higher among the 12-year-old children in the districts where mean per capita household income and mean household income was higher. The correlations between mean household income and mean DMFT (r = 0.47, 95% CI: 0.1–0.7, p = 0.01) and between mean per capita household income and mean DMFT (r = 0.47, 95% CI: 0.09–0.7, p = 0.01) were positive moderate correlations and were statistically significant (Table 2 and Figure 1). The higher the mean per capita household income and mean household income, the higher was the mean number of decayed teeth (DT) [r = 0.46, 95% CI: 0.02–0.6, p = 0.04] and mean number of filled teeth (FT) [r = 0.46, 95% CI: 0.07–0.7, p = 0.02] (Table 2 and Figure 1). Mean DMFT was positively correlated with the Gini coefficient of per capita income (r = 0.42, 95% CI: 0.03–0.7, p = 0.03) (Table 2).

Table 2.
Total correlations of measures of income and income inequality with dental caries experience and dental care indices in 12-year-old children in Sri Lanka and Wales.
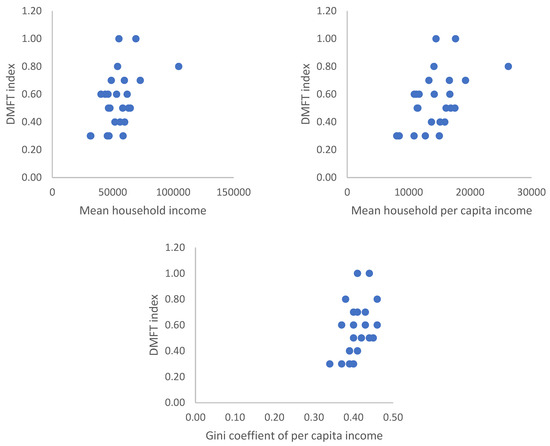
Figure 1.
Relationship between measures of income and income inequality and dental caries experience of 12-year-old children in Sri Lanka. (Mean household income and mean household per capita income are measured in Sri Lankan rupees).
In relation to Wales, the higher the deprivation quintile, the higher was the mean DMFT. However, the correlation was moderate and significant only in the 20%, 30%, and 50% WIMD quintiles (Table 2 and Figure 2). WIMD was significantly correlated with the mean number of decayed teeth (DT) only in its 50% quintile, whereas it was significantly correlated with the mean number of filled teeth (FT) within 30% and 50% of deprivation (Table 2). None of the absolute or relative income measurements were significantly correlated with any of the dental care indices in either country.
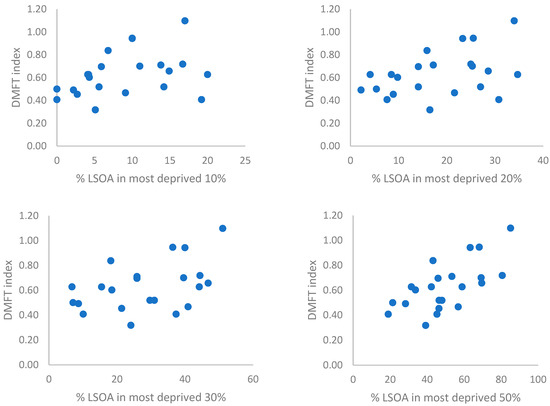
Figure 2.
Relationship between measures of deprivation (income inequality) and dental caries experience of 12-year-old children in Wales. (% LSOA typically refers to the proportion of Lower-layer Super Output Areas (LSOAs) within a local authority that fall within a specific deprivation band, such as 10%, 20%, 30%, and 50%).
4. Discussion
Relative income correlated with higher experience of dental caries in the respective administrative units in both countries. However, in Sri Lanka, districts where absolute income and household income levels were higher were associated with a greater experience of dental caries among 12-year-old children.
A systematic review assessing socio-economic contributors to dental caries among children in low- and lower-middle-income countries (LMICs) found that both low and high socio-economic status (SES) increased the risk of dental caries [15]. Children from low-SES backgrounds had the highest increased risk (approximately 54%, p < 0.001), followed by those from high-SES backgrounds (~3% increased risk, p = 0.81). In contrast, children from middle-SES backgrounds had a 20% reduced risk (p = 0.17) [15]. In these studies, SES was measured using household income, which may explain the findings of the current study. The systematic review attributed the higher dental caries experience among higher-SES groups in LMICs to multiple risk factors, notably the increased consumption of sugar-sweetened beverages and sugary foods. This increase is linked to higher affordability over the past two decades due to rapid income growth rather than a decline in the real price of sugar-sweetened beverages [16]. This affordability trend has been more pronounced in low- and middle-income countries than in high-income countries, according to the authors [16]. The positive correlation between household income status and the mean number of filled teeth suggests better access to dental services for reactive care. Sri Lanka, which is working toward universal health coverage, provides free dental care services through its primary, secondary, and tertiary healthcare institutions. By the academic year 2015–2016, 67% of 12-year-old children had access to a dental clinic within 5 kilometers of their homes, offering free dental care at the point of delivery [13]. Despite this high level of geographical and financial access to dental care in Sri Lanka, higher dental caries experience was observed in the districts where income inequality was higher (high Gini coefficient) emphasizing the importance of focusing on other socio-economic constraints in policy decisions.
Our findings support our hypothesis related to the correlation between income inequality and dental caries experience among 12-year-old children in a high-income country. Although there was a positive correlation between income inequality as measured by WIMD and dental caries experience, this correlation was significant only in the 20%, 30%, and 50% WIMD quintiles. Our findings are similar to another ecological study in which correlation was assessed between income inequality by Gini coefficient and dental caries experience in children aged 5 to 6 years, which showed a strong correlation [17]. Another ecological study, undertaken to compare the relationship between income inequality and dental caries experience in adults aged 35–44 years, showed an inverse relationship between income inequality and DMFT score [8]. The authors explain that DMFT was higher in equally rich countries, and this was mainly owing to the number of filled teeth, which reflects aspects related to restorative treatment. Moreover, they emphasize that this inverse relationship was observed due to the reduced number of filled teeth in countries having a larger gap between the richest and the poorest (i.e., higher income inequality), which have reduced opportunities to access care [8]. However, according to our findings related to Wales, both mean DT and mean FT scores were equally correlated with higher quintiles within 30% and 50% WIMD. This was also evident in the descriptive statistics related to the most deprived and least deprived unitary authorities of Wales, which show that both mean DT and mean FT of both unitary authorities were at similar levels. Therefore, according to the findings of this study, income inequality was positively correlated to dental caries experience, mean number of dental caries, and mean number of filled teeth due to caries in Wales.
In Wales 65% of 0–17-year-old children accessed general dental practices in 2014, 2015, and 2016 [18]. It seems that access is problematic for the most deprived 20% of the population, who have the greatest opportunity to benefit from prevention at the primary, secondary, and tertiary levels. There are no significant associations regarding DT and FT for these social sub-groups. This could be interpreted as showing that the lack of active restorative care has not influenced the need in the most deprived sub-group. In the least deprived local authority (Vale of Glamorgan), the DT for those where DT > 0 was 2.06, compared to the figure for the most deprived authority (Blaenau Gwent) of 1.86 [13]. Richards et al. [19] concluded that increasing the dental workforce alone cannot improve oral health in a diverse population like Wales. Levels of deprivation need to be considered. In Wales, access to dental services is difficult for people living in lower socio-economic status areas, as well as being due to dental contract reform for general dental practitioners, which is an ongoing issue in Wales and the UK.
Interestingly, there were no significant correlations between the dental care indices and income parameters in both countries, using either of the income parameters. This lack of correlation may reflect the mitigating effect of Sri Lanka’s free oral healthcare services, which could reduce disparities in access to treatment. However, this begs the question as to the effectiveness of the reactive approach to dental caries management. While the DMFT is a measure of current status, a caries-free mouth can change from disease inactive to disease active or vice versa depending on compliance with preventive behaviors [20,21]. These include adequate plaque control, diet control, and fluoride usage [20,21]. Clearly, 70.4% and 69.6% of Welsh and Sri Lankan 12-year-olds, respectively, are controlling behaviors towards disease inactivity [12]. Primary prevention will have been successful in this cohort of the population, possibly because of a common risk approach. Monitoring of ongoing behaviors will be needed to establish whether individuals are continuing to maintain disease-inactive mouths. Thus, there is a need for monitoring on a risk basis as described in the NICE guidelines [22]. The one-third of the population having disease-active mouths will need secondary and tertiary care provided by dental professionals, and this applies particularly to the children with >2 DMFT in Wales and >2.7 DMFT in Sri Lanka.
Although several studies have explored inequalities in dental caries, they have primarily focused on national samples within a single country or on cross-country comparisons involving nations with similar geographic or socio-economic contexts [8,15,23]. In contrast, the present study offers epidemiological evidence for the association between income inequality and dental caries experience using data from two countries with differing economic statuses. This study has highlighted the importance of disease management at the population level and the value placed on preventive care. In Sri Lanka, targeting secondary and tertiary prevention among more affluent 12-year-olds could be beneficial as they transition into adulthood. In Wales, a similar emphasis on secondary and tertiary prevention is warranted, particularly for children within the most deprived 50% of the population. To achieve this, equitable access to services and comprehensive population coverage are essential. A general dental service contract that prioritizes prevention would be a key step toward this goal. In the UK, Milsom et al. [24] identified an opportunity to convert irregular dental attenders into regular users through a revised dental contract for general dental practitioners. Richards et al. [19] have also emphasized the potential for reform to improve population-level access. Similarly, the Alliance for a Cavity-Free Future (ACFF) recognizes universal population coverage as a core objective [25].
While the analysis examined associations between income and dental caries within each country, a direct comparison between the two nations is not feasible due to differences in the measurement tools used for both income and oral health outcomes. For instance, dental caries in Sri Lanka was assessed using the DMFT index based on the World Health Organization’s Basic Oral Health Survey guidelines [9], which may include cavitated enamel lesions. In Wales, however, the assessment followed the criteria set by the British Association for the Study of Community Dentistry (BASCD), which uses the D3MFT index, recording decay only at the dentinal level [13]. Furthermore, the income-related indicators used in the two countries differ in scope and scale. The Gini index, used in Sri Lanka, reflects income inequality at a national or regional level [12]. In contrast, the Welsh Index of Multiple Deprivation (WIMD) captures a broader concept of deprivation, incorporating not only income-related measures but also domains such as education, employment, housing, health, and access to services [13].
Another limitation of this study is the reliance on different sources of aggregated data for the selected variables. For instance, the data on dental caries were obtained from national survey reports in both countries, while the income-related measurements were drawn from a separate source of national data collected from a different population sample from the respective countries. Further, this study has limitations that are common to ecological study designs. Ecological studies typically investigate the association between outcome measures using correlation analysis. A significant correlation does not mean that a cause-and-effect association can be implied [26]. The correlation between income, income inequality, and dental caries experience among 12-year-children observes an association and not necessarily a causal relationship. Therefore, the authors cannot draw a conclusion about a causal relationship between these children’s dental caries experiences and the income status of their families. This ecological study assesses and compares the correlation between income status and dental caries experience at the population level rather than the individual level. At the same time, conclusions are drawn for individual-level associations, which is a common bias named the ecological fallacy [26]. However, these types of ecological studies will allow the generation of hypotheses for further research on the risk factors and outcomes of diseases [26]. Moreover, these types of ecological studies will allow the generation of hypotheses for further research on the risk factors and outcomes of diseases [26]. Area-based measures have been promoted by Locker (1993) for research to identify where deprived groups with relatively poor health live [27].
5. Conclusions
This ecological study found that both absolute and relative income measures were associated with dental caries and its components in Sri Lanka, whereas in Wales, income inequality showed a positive association with caries experience. No associations were observed between income indicators and reactive dental care in either setting. Given the ecological design and temporal differences in the data sources, these findings should be interpreted with caution. Future research using individual-level data is needed to better understand the social determinants of oral health in children. From a public health perspective, preventive efforts may warrant attention to more affluent subgroups in Sri Lanka and to deprived populations in Wales.
Author Contributions
Conceptualization, D.L.R. and W.R.; formal analysis, D.L.R. and J.A.; methodology, D.L.R. and W.R.; writing—original draft, D.L.R., W.R. and J.A.; writing—review and editing, A.-M.C. and T.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and ethical clearance for the study was obtained from the Low-Risk Ethics Review Committee of the Faculty of Life Sciences and Education, University of South Wales (230289LR) on 26 July 2024.
Informed Consent Statement
This study is based on anonymized secondary data obtained from previously published sources. As no identifiable individual data were collected, separate informed consent was not required.
Data Availability Statement
The datasets analyzed during the current study are available in the following published reports related to Sri Lanka (Department of Census and Statistics. Household Income and Expenditure Survey 2016; Ministry of Healthcare and Nutrition. National Oral Health Survey Sri Lanka 2015–2016. 2018) and webpages of Wales (Welsh Government. Welsh Index of Multiple Deprivation (WIMD) 2014: Revised. Cardiff, Wales: Welsh Government; 2015. Available from https://www.gov.wales/sites/default/files/statistics-and-research/2019-04/welsh-index-of-multiple-deprivation-2014-revised.pdf; Welsh Oral Health Information Unit. Data Report: School Year 7, 2016/2017. Cardiff: Cardiff University; 2017. Accessed 12 August 2024. https://www.cardiff.ac.uk/research/explore/research-units/welsh-oral-health-information-unit).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Peres, M.A.; Macpherson, L.M.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Ruff, R.R.; Senthi, S.; Susser, S.R.; Tsutsui, A. Oral health, academic performance, and school absenteeism in children and adolescents: A systematic review and meta-analysis. J. Am. Dent. Assoc. 2019, 150, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Barreto, M.L. Health inequalities: A global perspective. Desigualdades em Saúde: Uma perspectiva global. Cien. Saude Colet. 2017, 22, 2097–2108. [Google Scholar] [CrossRef] [PubMed]
- Watt, R.G. Oral health inequalities-Developments in research, policy and practice over the last 50 years. Community Dent. Oral. Epidemiol. 2023, 51, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Dörfer, C.E.; Schlattmann, P.; Foster Page, L.; Thomson, W.M.; Paris, S. Socioeconomic inequality and caries: A systematic review and meta-analysis. J. Dent. Res. 2015, 94, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Lange, S.; Vollmer, S. The effect of economic development on population health: A review of the empirical evidence. British Medical. Bulletin. 2017, 121, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Bernabé, E.; Sheiham, A.; Sabbah, W. Income, income inequality, dental caries and dental care levels: An ecological study in rich countries. Caries Res. 2009, 43, 294–301. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Oral Health Surveys: Basic Methods, 5th ed; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Welsh Government. Welsh Index of Multiple Deprivation (WIMD) 2014: Revised; Welsh Government: Cardiff, UK, 2015. Available online: https://www.gov.wales/sites/default/files/statistics-and-research/2019-04/welsh-index-of-multiple-deprivation-2014-revised.pdf (accessed on 12 March 2025).
- Department of Census and Statistics. Household Income and Expenditure Survey 2016; Department of Census and Statistics in Sri Lanka: Battaramulla, Sri Lanka, 2018. [Google Scholar]
- Ministry of Healthcare and Nutrition. National Oral Health Survey Sri Lanka 2015–2016; Ministry of Healthcare and Nutrition: Colombo, Sri Lanka, 2018. [Google Scholar]
- Welsh Oral Health Information Unit. Data Report: School Year 7, 2016/2017; Cardiff University: Cardiff, UK, 2017; Available online: https://www.cardiff.ac.uk/research/explore/research-units/welsh-oral-health-information-unit (accessed on 21 March 2025).
- Office for National Statistics. Population Estimates for the UK, England and Wales, Scotland and Northern Ireland: Mid-2016. Office for National Statistics: Newport, UK, 2017. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/mid2016 (accessed on 21 November 2024).
- Yousaf, M.; Aslam, T.; Saeed, S.; Sarfraz, A.; Sarfraz, Z.; Cherrez-Ojeda, I. Individual, Family, and Socioeconomic Contributors to Dental Caries in Children from Low- and Middle-Income Countries. Int. J. Environ. Res. Public Health 2022, 19, 7114. [Google Scholar] [CrossRef] [PubMed]
- Blecher, E.; Liber, A.C.; Drope, J.M.; Nguyen, B.; Stoklosa, M. Global trends in the affordability of sugar-sweetened beverages, 1990–2016. Prev. Chronic Dis. 2017, 14, E37. [Google Scholar] [CrossRef] [PubMed]
- Bernabé, E.; Hobdell, M.H. Is income inequality related to childhood dental caries in rich countries? J. Am. Dent. Assoc. 2010, 141, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Welsh Government. NHS Dental Services: April 2021 to March 2022; Welsh Government: Cardiff, UK, 2022. Available online: https://www.gov.wales/nhs-dental-services-april-2021-march-2022 (accessed on 30 March 2025).
- Richards, W.; Ameen, J.; Coll, A.M.; Filipponi, T. Building back better. BDJ Pract. 2021, 34, 20–22. [Google Scholar] [CrossRef]
- Nassar, Y.; Brizuela, M. The Role of Fluoride on Caries Prevention; [Updated 19 March 2023]; Stat Pearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK587342/?utm_source=chatgpt.com (accessed on 19 May 2025).
- Tungare, S.; Paranjpe, A.G. Diet and Nutrition to Prevent Dental Problems; [Updated 10 July 2023]; Stat Pearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK534248/?utm_source=chatgpt.com (accessed on 28 May 2025).
- National Institute for Health and Care Excellence (NICE). Dental Checks: Intervals Between Oral Health Reviews—Clinical Guidance; National Institute for Health and Care Excellence (NICE): London, UK, 2004; Available online: https://www.nice.org.uk/guidance/cg19 (accessed on 28 May 2025).
- Medina-Solís, C.E.; Ávila-Burgos, L.; Borges-Yañez, S.A.; Irigoyen-Camacho, M.E.; Sánchez-Pérez, L.; Zepeda-Zepeda, M.A.; Lucas-Rincón, S.E.; Medina-Solís, J.J.; Márquez-Corona, M.D.L.; Islas-Granillo, H.; et al. Ecological study on needs and cost of treatment for dental caries in schoolchildren aged 6, 12, and 15 years: Data from a national survey in Mexico. Medicine 2020, 99, e19092. [Google Scholar] [CrossRef] [PubMed]
- Milsom, K.M.; Blinkhorn, A.S.; Tickle, M. The incidence of dental caries in the primary molar teeth of young children receiving regular dental care. Br. Dent. J. 2008, 206, E9. [Google Scholar] [CrossRef]
- Pitts, N.B.; Mayne, C. Making cavities history: A global policy consensus for achieving a dental cavity–free future. JDR Clin. Transl. Res. 2021, 6, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Sedgwick, P. Ecological studies: Advantages and disadvantages. BMJ 2014, 348, g2979. [Google Scholar] [CrossRef] [PubMed]
- Locker, D. Measuring social inequality in dental health services research: Individual, household and area-based measures. Community Dent. Health 1993, 10, 139–150. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).