Abstract
Background/Objectives: Surgical guides have been used in a variety of dental procedures, such as implant placement to improve clinical accuracy and reduce post-operative complications. This report presents a novel and versatile workflow for the design and fabrication of a “multi-purpose” fully-guided tooth- and bone-supported one-piece surgical guide. Methods: Briefly, intraoral and perioral anatomical features were captured by an intraoral scan and a cone-beam computed tomography scan. The data were segmented and aligned with analysis software to enable the digital design of surgical guides. The versatility of this method was demonstrated through its application in the two cases presented: the first involved a lateral sinus lift with simultaneous implant placement, and the second involved the removal of a foreign object from the alveolar bone prior to implant placement. Results: Positive clinical outcomes were confirmed at follow-up visits for up to 12 months. Conclusions: This method may be applied to a range of challenging clinical scenarios, such as apicectomy, the extraction of supernumerary or unerupted teeth, corticotomy to facilitate orthodontic movement, the precise reduction of bony spurs or exostoses, and the conservative surgical removal of pathologies.
1. Introduction
Placing dental implants close to critical anatomical structures can be technically challenging, as minor deviations from the target position may damage adjacent anatomic structures or compromise the longevity of the prostheses [1,2]. Thus, surgical guides have been used to improve the functional and aesthetic success of implants [1,2]. Advancements in cone-beam computer tomography (CBCT), intraoral optical scanning, computer-aided design, and three-dimensional (3D) printing have greatly improved their accessibility and versatility [1,3].
A surgical guide is composed of a contact surface, which provides support, and a guiding cylinder, which directs the surgical drill to the exact location and orientation [1,2,4]. Depending on the source of support, surgical guides can be classified into one of three categories: mucosa-supported, bone-supported, and tooth-supported [1,4,5,6]. Both bone- and tooth-supported guides may offer improved stability over the mucosa-supported type due to the compromised firmness and precision of soft tissues [6]. Nonetheless, the bone-supported design may require fixation screws because of its susceptibility to improper positioning [7]. Thus, a combined tooth- and bone-supported design in partially edentulous arches may reduce the complexity of surgical procedures while ensuring sufficient accuracy. Additionally, their design can be either fully or partially guided; the former assists with both osteotomy and implant placement, while the latter supports only osteotomy and requires freehand implant placement [5]. Fully-guided tooth-supported static surgical guides have been demonstrated to result in significantly reduced angular deviation compared to partially guided surgical guides combined with freehand implant surgery [5].
The maxillary lateral sinus lift is a procedure used to achieve sufficient bone height for implants in the posterior maxillary region in cases of alveolar ridge resorption or maxillary sinus pneumatisation [8,9]. Depending on the amount of bone present, maxillary lateral sinus lift and implant placement may be performed together through the one-stage technique or separately through the two-stage technique; the former is usually preferred when possible due to minimised surgical trauma, as well as decreased treatment time and cost [10]. A surgical guide ensures the accuracy of the lateral window extension, improves the speed and comfort of the access, and reduces the uncertainty of the surgery [11,12]. Digital planning combined with 3D printing has been introduced to produce surgical guides for lateral window localisation and simultaneous implant placement [7]. However, these early 3D-printed designs need two separate guides to outline the lateral window and an additional guide for the implant placement [7]. They use bone-supported designs that require fixation screws in the bone for stability, limiting their applicability in cases of a thin sinus bony wall [7]. As a major technical improvement, Goodacre et al. demonstrated a one-piece surgical guide for window access and implant placement, which achieved stability through a tooth-supported design without bone fixation [13].
Aside from implant placement, surgical guides have been adapted for various other purposes in dentistry and oral health, where they effectively improve clinical accuracy and reduce post-operative complications. For example, they are used in the removal of unusual pathologies and foreign objects, especially those at difficult-to-reach sites [14,15]. Further applications for surgical guides other than implant placement include supernumerary tooth extraction, apicectomy, corticotomy, orthognathic surgery, and maxillary sinus lift [7,13,16,17,18,19].
This report aims to demonstrate a workflow for designing and producing a “multipurpose” fully-guided tooth- and bone-supported one-piece surgical guide through the combination of CBCT segmentation and intra-oral scanning. Two cases are presented to illustrate the versability of its clinical application: a lateral sinus lift with simultaneous implant placement, and a minimal osteotomy for the removal of gutta percha (GP) material retained in bone prior to implant surgery.
2. Materials and Methods
To design and manufacture a surgical guide supported by both the cortical plate and the dentition, an intraoral scanner (TRIOS 4; 3Shape A/S, Copenhagen, Denmark) and a CBCT scanner (CS 9300, Carestream Health, Rochester, NY, USA) were used to capture the intraoral and perioral anatomical features of a patient. Soft tissue areas irrelevant to the design of the surgical guide were removed from the IOS (Figure 1A). The CBCT data were then imported into the Mimics V.21 analysis program (Materialise NV, Leuven, Belgium) to segment the cortical plate, which was then exported as an STL file (Figure 1B). Segmentation was initially performed using the predefined “cortical bone (adult)” setting, with Hounsfield unit values ranging from 662 to 1988. Necessary manual adjustments were made to ensure the cortical plate was clearly defined. For the segmentation of the tooth structures, predefined Hounsfield units ranging from 750 to 4000 were applied, with visual adjustments made as needed. This segmentation application utilises adjustments to Hounsfield units to define the anatomical structures that need to be segmented. The individual segments were combined using Boolean operation. An STL file containing both the cortical plate and tooth structures was exported.
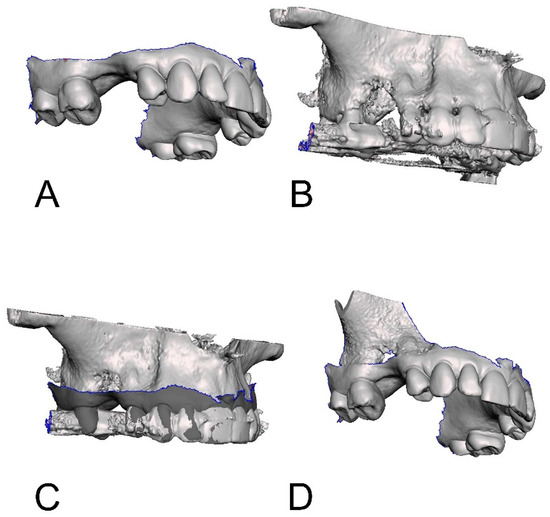
Figure 1.
The digital models for designing the surgical guide: (A) intraoral scan with irrelevant soft tissues removed; (B) segmented maxillary sinus cortical plate; (C) alignment of STL of CBCT and IOS; (D) final model for designing surgical guide.
The two STL files derived from the IOS and CBCT, respectively, were then aligned to create a “watertight” model for the surgical guide design. The separate STLs of the surfaces of the teeth and cortical plates were imported into the open-source 3D editing software, Meshmixer version 3.5.474 (Autodesk, San Francisco, CA, USA). The STL of the cortical plate was then aligned to the teeth using the multi-point inbuilt alignment process (Figure 1C). After the alignment, the overlapped areas of the separate scans were removed by deleting all areas of the CBCT and corresponding areas of the IOS. The separate STL files were then combined to form a single file. In order to make a clear connection between the edges of the tooth section and the cortical plate section, the “bridge” and “fill” functions were used. The “bridge” function joins two edges of an STL file by first highlighting the edges to be joined, while the “fill” function fills a hole in an STL file by defining the borders of the hole. This resulted in a model incorporating the tooth structures and the cortical plate. The solid tooth and bone structure data were then exported as a finalised model for implant planning and surgical guide design (Figure 1D).
The model of tooth and bone structure and the original CBCT data were imported into the commercially available implant planning software, Dental Desktop version 17.1 (3Shape A/S), to design the surgical guide. Implant planning was performed with a Ø 2.2 mm titanium sleeve (steco-system-technik, Hamburg, Germany) defined for a pilot hole corticotomy. For the lateral sinus lift, a surgical guide, after implant planning, was designed by placing a surgical guide outline over the remaining dentition in quadrant 2 with a thickness of 3 mm. An additional outline was placed 5 mm around the plater lateral window site. This was then connected to the main surgical guide outline using bars with a thickness of 4 mm (Figure 2A). Next, windows were longitudinally placed at the ideal outlines (Figure 2A). An STL of the guide was then generated. For the precision corticotomy, a surgical guide was designed using a similar technique, but with a single bar positioned over the expected corticotomy site and a window generated to guide the location of the corticotomy (Figure 2B).
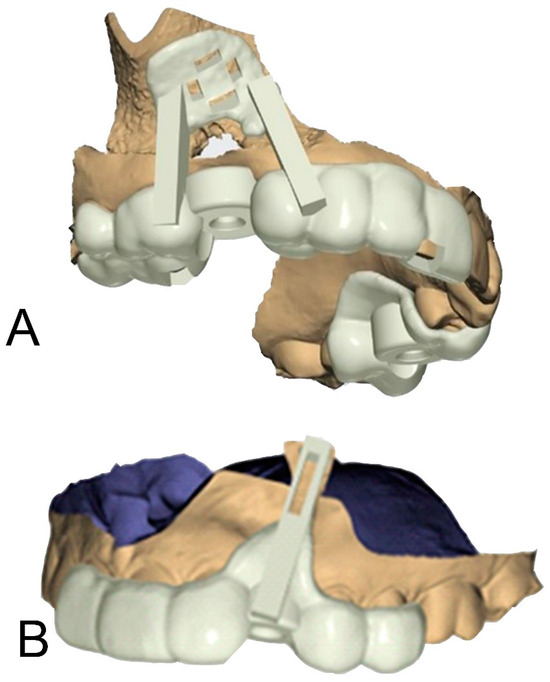
Figure 2.
The digital designs of the surgical guides: (A) for a lateral sinus lift; (B) for a precision osteotomy.
2.1. Case 1: Lateral Sinus Lift
A 64-year-old male patient presented with a complaint of a missing upper right first molar that had been extracted 12 months prior. A CBCT was taken, and restoration with an implant was recommended with lateral sinus augmentation due to the available bone being 3.2 mm in depth (Figure 3A). A surgical treatment plan was formulated, which included a surgical guide to aid in the outline of the bony window and simultaneous implant placement. Consent was obtained from the patient prior to the commencement of the procedure. Local anaesthesia with 4% articaine containing 1:100,000 adrenaline was administered at the buccal and palatal regions of the surgical area. A full thickness flap elevation was performed. The surgical guide was used to direct the lateral window preparation of the sinus wall (Figure 3B,C). The surgical guide sat flush to the cortical plate and dentition. The opening was first outlined and then widened with the piezoelectric diamond burs and round burs from the Lateral Window Bur Kit (Acteon, Lyon, France). Linear osteotomy cuts were performed with rotatory instruments and piezoelectric devices. The resulting window of the sinus wall was reflected superiorly with the mucosa elevated. Simultaneous implant placement and grafting were then performed due to the presence of a satisfactory amount of residual bone. A single Ø 4.1 mm × 10 mm bone level Roxolid SLActive implant (Straumann, Basel, Switzerland) was placed in the preplanned osteotomy site, with Bio-Oss granules and a Bio-Gide membrane (Geislitch, Wolhusen, Switzerland) placed in the sinus cavity (Figure 3D). The full thickness flap was re-approximated with PROLENE suture 5-0 (Ethicon, Raritan, NJ, USA) placed. Typically, three months are required for osseointegration prior to rehabilitation with an implant-supported prothesis, while this may be increased to six months when lateral sinus augmentation is performed at the same appointment. In this case, the surgical site was reviewed six months post-operatively, confirming successful osseointegration and the absence of complications (Figure 4B). The crown was placed at a separate appointment, two months later (Figure 4C).
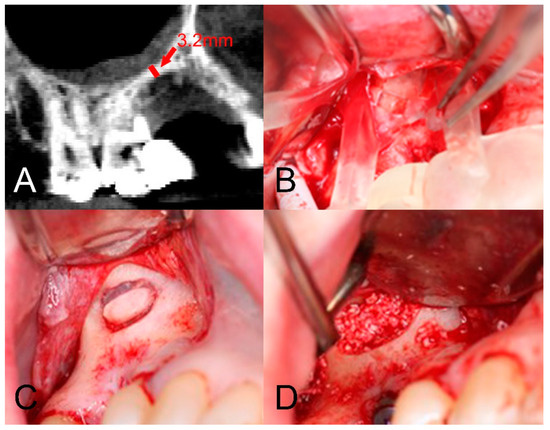
Figure 3.
The use of the surgical guide in a lateral sinus lift: (A) CBCT sagittal cross-section of available bone over crest of ridge; (B) the surgical guide being used to direct the window for the lateral sinus lift; (C) the window for the lateral sinus lift; (D) placement of Bio-Oss granule prior to the membrane placement.
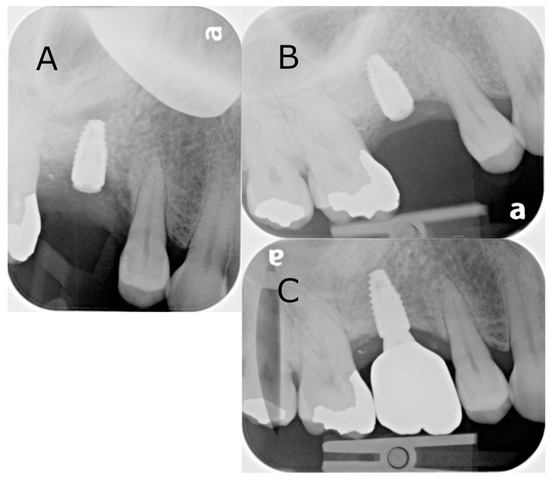
Figure 4.
Intraoral radiographs of the surgical site from the lateral sinus lift with simultaneous implant placement: (A) immediately post-operatively following the implant placement; (B) six-month follow-up; (C) crown placement. Note that the letter “a” is pre-printed on the phosphor storage plate upon acquisition, serving as a reference for orientation.
2.2. Case 2: Precision Osteotomy
A 49-year-old male patient presented requesting restorative options for a missing 23. A dental implant was proposed as a treatment option, and the patient consented to proceed. During screening with OPG and CBCT, a submerged radiopaque GP was observed. The GP intersected the ideal implant position (Figure 5A). It was decided that it would be removed utilising a surgical guide to minimise cortical plate loss for bone preservation prior to implant placement. The treatment plan was discussed with the patient, and informed consent was obtained. Local anaesthesia with 4% articaine containing 1:100,000 adrenaline was administered via buccal, palatal, and mid-crestal infiltrations. A mid-crestal incision and vertical relieving incisions were performed. A full thickness periosteal flap was raised at the left canine region to expose the alveolar ridge. The surgical guide was placed over the exposed ridge to indicate the position of the retained GP and subsequent corticotomy. A Ø 1.4 mm small round bur was then inserted through the surgical guide channel to remove the cortical plate to reveal the GP (Figure 5B). The GP was removed with a small spoon excavator, and a periapical radiograph was taken to ensure the complete removal of restorative debris (Figure 5C). The width of the osteotomy site was 3 mm at the apical end and 2 mm at the coronal end (Figure 5D). The Bio-Gide membrane (Geislitch) was placed over the osteotomy site to prevent soft tissue growth into the defect and enable fibroblast attachment for the formation of new bone tissues and blood vessels in the defect. No bone substitute material was used. The flap was repositioned and secured with six simple interrupted sutures using PROLENE suture 5-0 (Ethicon). The surgical site was reviewed at 6 and 12 months post-operatively, with intraoral radiographs confirming the complete removal of the GP (Figure 6).
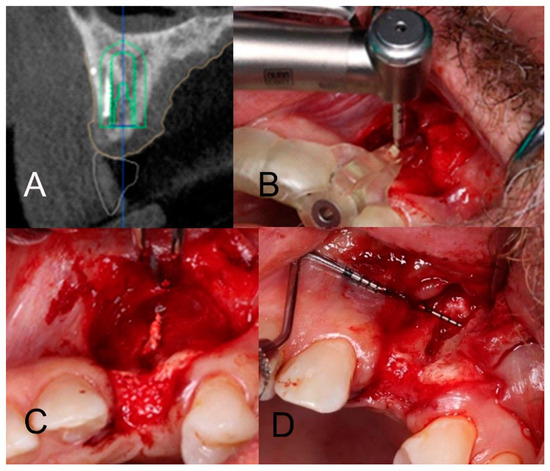
Figure 5.
The use of the surgical guide in a precision osteotomy: (A) implant planning showing a foreign body intersecting the proposed implant site; (B) surgical guide in situ being used to guide the corticotomy; (C) removal of the foreign body; (D) osteotomy site with a periodontal probe indicating the dimensions of the bone removed.
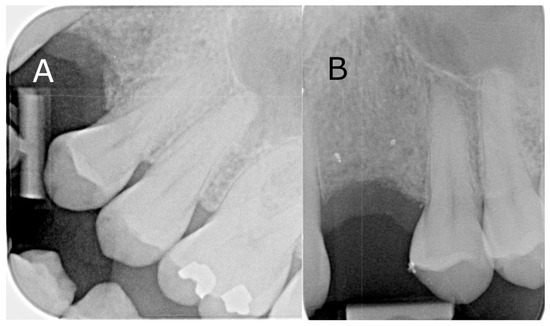
Figure 6.
Intraoral radiographs of the surgical site from the precision osteotomy: (A) 6-month follow-up; (B) 12-month follow-up.
3. Discussion
Currently, surgical guides find diverse applications across various procedures in dentistry and oral surgery, allowing for precise planning and execution and achieving improved safety and efficiency. In lateral sinus lift procedures, surgical guides effectively aid in ensuring the precise size and positioning of the lateral window, thus decreasing the risk of sinus membrane perforations and avoiding adjacent anatomical structures, such as sinus septa and arterial branches [12,20,21,22]. This report presents a novel alternative method to design and fabricate combined tooth- and bone-supported one-piece surgical guides suitable for diverse clinical situations. As shown in the first case, it was successfully used in lateral sinus lift with simultaneous implant placement. The versatility of this method in other procedures was then also demonstrated in the second case of an osteotomy for the removal of a GP retained in trabecular bone prior to implant placement. This technique can be used for a variety of procedures requiring precision removal of bone in the maxillofacial region.
Surgical guides for lateral sinus lift are not a new concept. Their first application was introduced by Mandelaris and Rosenfeld in 2009. They utilised one cutting guide for the superior boundary and a second cutting guide for the anterior, inferior, and posterior boundaries, with a third separate guide needed for implant placement [7]. A major improvement was then accomplished in 2018 by Goodacre et al., who presented a 3D-printed one-piece surgical guide that both indicated all boundaries of the lateral window and directed simultaneous implant placement [13]. The alternative method for fabricating one-piece surgical guides in this report not only achieved performance in lateral sinus lift at least equivalent to that of Goodacre et al., but also allowed successful application in the removal of GP retained in bone. Compared to previous studies, this report presents a novel and versatile workflow that enables the design and fabrication of surgical guides for multiple purposes.
The early iterations of surgical guides for lateral sinus lift were bone-supported, which were often prone to improper positioning and compromised accuracy [7,16]. This lack of sufficient stability required fixation screws to be placed in the bone [7]. This complicated the procedure and was not applicable in cases of a thin sinus bony wall. They also tended to be bulky, hindering clear visualisation of the field and compromising proper positioning [1,7,9]. The method provided in this report uses a tooth- and bone-supported design similar to that of Goodacre et al., with further improvement by utilising the dentition as the positioning reference. This was verified with the addition of windows in the occlusal surface [13]. Stable support was achieved with coverage of the contact surface from the tooth cusps to the buccal vestibule.
The two cases included indicate that the digitally planned and 3D-printed one-piece surgical guides produced by the presented method achieved sufficient stability and sound clinical outcome. The lateral sinus lift with simultaneous implant placement in the first case was completed without any significant post-operative complication or healing issue. The Bio-Oss bone graft material used in this clinical case, combined with barrier membranes, has previously been shown to significantly improve the treatment of periodontal intrabony defects [23]. In the second case, the surgical stent was well seated over the exposed ridge and accurately indicated the position of the retained object; the spot removal of foreign material was important to minimize bone loss. The surgical guides made through this method may also be used in other challenging cases or procedures, such as apicectomy, the extraction of supernumerary or unerupted teeth, corticotomy to aid in orthodontic movement, the precise reduction of bony spurs or exostoses, and the removal of pathologies that require conservative and precise surgical interventions.
It should be noted that this report includes only two clinical cases without long-term follow-up. The limitations of this method include the requirement of access to multiple software packages and a 3D printer. It may also be technically demanding and time consuming for novices. The alignment of the IOS and CBCT needs to be precise to generate a surgical guide with the correct fit. With recent advancements and increased user-friendliness in software for the segmentation of anatomical structures and the alignment of multiple scans, these techniques are expected to become commonplace in oral surgical procedures.
4. Conclusions
This report presents a novel workflow for designing and fabricating a “multi-purpose” fully-guided tooth- and bone-supported one-piece surgical guide. Positive clinical outcomes have been demonstrated through their use in two clinical cases: a lateral sinus lift with simultaneous implant placement, and a minimal osteotomy for the removal of GP retained in bone. Compared to previous studies, the major improvement of this method lies in its versatility, which may allow for its application in a range of clinical situations.
Author Contributions
Conceptualisation and methodology, A.B.C. and A.S.; data curation, R.A. and T.-T.L.; original draft preparation, L.A.S., P.S. and A.B.C.; review and editing, L.A.S., P.S. and A.B.C.; supervision, A.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The case report merely documents the use of these established techniques in a real-world setting and does not introduce any new treatments, protocols, or interventions, it was not considered necessary to seek ethical approval, as it does not meet the criteria for research involving human subjects as per the university guidelines.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent was obtained from the patients to publish this paper.
Data Availability Statement
The data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ramasamy, M.; Raja, R.; Narendrakumar, R. Implant surgical guides: From the past to the present. J. Pharm. Bioallied Sci. 2013, 5 (Suppl. S1), S91–S94. [Google Scholar] [CrossRef]
- Widmann, G.; Bale, R.J. Accuracy in computer-aided implant surgery—A review. Int. J. Oral Maxillofac. Implants 2006, 21, 305–313. [Google Scholar] [PubMed]
- Arfai, N.K.; Kiat-Amnuay, S. Radiographic and surgical guide for placement of multiple implants. J. Prosthet. Dent. 2007, 97, 310–312. [Google Scholar] [CrossRef]
- Raico Gallardo, Y.N.; da Silva-Olivio, I.R.T.; Mukai, E.; Morimoto, S.; Sesma, N.; Cordaro, L. Accuracy comparison of guided surgery for dental implants according to the tissue of support: A systematic review and meta-analysis. Clin. Oral Implants Res. 2017, 28, 602–612. [Google Scholar] [CrossRef] [PubMed]
- Floriani, F.; Jurado, C.A.; Cabrera, A.J.; Duarte, W.; Porto, T.S.; Afrashtehfar, K.I. Depth distortion and angular deviation of a fully guided tooth-supported static surgical guide in a partially edentulous patient: A systematic review and meta-analysis. J. Prosthodont. 2024, 33 (Suppl. S1), 10–24. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Wang, J.; Ma, C.; Shen, J.; Dong, X.; Lin, D. A systematic review of the accuracy of digital surgical guides for dental implantation. Int. J. Implant Dent. 2023, 9, 38. [Google Scholar] [CrossRef]
- Mandelaris, G.A.; Rosenfeld, A.L. Alternative applications of guided surgery: Precise outlining of the lateral window in antral sinus bone grafting. J. Oral Maxillofac. Surg. 2009, 67, 23–30. [Google Scholar] [CrossRef]
- Raghoebar, G.M.; Onclin, P.; Boven, G.C.; Vissink, A.; Meijer, H.J. Long-term effectiveness of maxillary sinus floor augmentation: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46, 307–318. [Google Scholar] [CrossRef]
- Wallace, S.S.; Tarnow, D.P.; Froum, S.J.; Cho, S.-C.; Zadeh, H.H.; Stoupel, J.; Del Fabbro, M.; Testori, T. Maxillary sinus elevation by lateral window approach: Evolution of technology and technique. J. Evid. Based Dent. Pract. 2012, 12, 161–171. [Google Scholar] [CrossRef]
- Khatiblou, F.A. Sinus floor augmentation and simultaneous implant placement, part I: The 1-stage approach. J. Oral Implantol. 2005, 31, 205–208. [Google Scholar] [CrossRef]
- Pardal-Peláez, B.; Córdoba-Llorente, J.R.; Belarra-Arenas, C. Sinus lift through the use of a surgical guide: A case report. Int. J. Comput. Dent. 2020, 23, 493–497. [Google Scholar]
- Elian, N.; Wallace, S.; Cho, S.-C.; Jalbout, Z.N.; Froum, S. Distribution of the maxillary artery as it relates to sinus floor augmentation. Int. J. Oral Maxillofac. Implants 2005, 20, 699–704. [Google Scholar]
- Goodacre, B.J.; Swamidass, R.S.; Lozada, J.; Al-Ardah, A.; Sahl, E. A 3D-printed guide for lateral approach sinus grafting: A dental technique. J. Prosthet. Dent. 2018, 119, 897–901. [Google Scholar] [CrossRef]
- Jeong, M.; Kwon, D.H.; Lee, S.J. Computer guided root tip extraction and implant placement: A clinical report. J. Prosthet. Dent. 2024; in press. [Google Scholar]
- Mao, M.Y.; Wang, C.Z.; Zhu, H.H.; Fan, M.X.; Wu, X.F.; Zhu, F.D. Design and validation of a surgical guide for the retrieval of foreign body instruments in jaw. Acta Anat. Sin. 2023, 54, 244. [Google Scholar]
- Brunso, J.; Franco, M.; Constantinescu, T.; Barbier, L.; Santamaría, J.A.; Alvarez, J. Custom-machined miniplates and bone-supported guides for orthognathic surgery: A new surgical procedure. J. Oral Maxillofac. Surg. 2016, 74, 1061.e1–1061.e12. [Google Scholar] [CrossRef]
- Cassetta, M.; Giansanti, M.; Di Mambro, A.; Calasso, S.; Barbato, E. Minimally invasive corticotomy in orthodontics using a three-dimensional printed CAD/CAM surgical guide. Int. J. Oral Maxillofac. Surg. 2016, 45, 1059–1064. [Google Scholar] [CrossRef]
- Lee, H.; Chae, Y.K.; Choi, S.; Jih, M.K.; Lee, J.-W.; Choi, S.C.; Nam, O.H. Feasibility of a 3D surgical guide technique for impacted supernumerary tooth extraction: A pilot study with 3D printed simulation models. Appl. Sci. 2019, 9, 3905. [Google Scholar] [CrossRef]
- Peng, L.; Wang, Z.H.; Sun, Y.C.; Qu, W.; Han, Y.; Liang, Y.H. Computer aided design and three-dimensional printing for apicoectomy guide template. J. Peking Univ. Health Sci. 2018, 50, 905–910. [Google Scholar]
- Katranji, A.; Fotek, P.; Wang, H.L. Sinus augmentation complications: Etiology and treatment. Implant Dent. 2008, 17, 339–349. [Google Scholar] [CrossRef]
- Kim, M.J.; Jung, U.W.; Kim, C.S.; Kim, K.D.; Choi, S.H.; Kim, C.K.; Cho, K.S. Maxillary sinus septa: Prevalence, height, location, and morphology. A reformatted computed tomography scan analysis. J. Periodontol. 2006, 77, 903–908. [Google Scholar] [CrossRef]
- Wallace, S.S.; Froum, S.J. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol. 2003, 8, 328–343. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Cui, W.; Zhao, Y.; Lei, L.; Li, H. Clinical and radiographic evaluation of Bio-Oss granules and Bio-Oss Collagen in the treatment of periodontal intrabony defects: A retrospective cohort study. J. Appl. Oral Sci. 2024, 32, e20230268. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).