Abstract
Mandibular condylar fractures can be approached with invasive techniques, such as surgical repositioning and fixation of the fractured condyle, or with conservative techniques using myofunctional appliances. Recent publications recommend non-invasive or conservative approaches when treating mandibular condylar fractures, as they may produce more stable results and fewer consequences. However, to the knowledge of the authors, there is no long-term follow up publications of clinical cases treated with a conservative approach. This report presents a ten-year follow-up of a case report published two years ago by the same authors. In the previous report, the authors showed an eleven year-old girl treated with a myofunctional appliance due to a bilateral mandibular condylar fracture. The treatment produced a stable result over the following ten years with the patient not using any appliance after the myofunctional treatment was completed. The benefits of a conservative treatment, as well as the consequences of mandibular condylar fracture, such as a heart shaped mandibular condyle, are discussed here by the authors.
1. Introduction
The treatment of mandibular condylar fractures is still controversial, with the literature supporting either invasive or non-invasive approaches. A non-invasive approach is highly recommended, as it less traumatic for the patient, remodels the mandibular condyle, and re-establishes mandibular dynamics [1,2]. This was supported by a clinical case reported by these authors, where an 11 year-old female patient, who had a traumatic bilateral mandibular condylar fracture, was treated with a myofunctional conservative approach, which rendered a satisfactory remodeling of the mandibular condyles and the temporomandibular joint (TMJ) on both sides, with a full recovery of the mandibular dynamics, no limitation for mouth opening, and no facial asymmetry [3]. However, long-term follow up reports are not commonly found in the scientific literature. Therefore, the present report aims to present the stability of the results on that clinical case after 10 years of the treatment.
Briefly, the previous report showed the results of a bilateral mandibular condylar fracture in an 11 year-old female girl. The patient was successfully treated with myofunctional appliances in combination with exercises. After an initial treatment with a bionator and, later, with the Indirect Planas’ Tracks appliances. combined with exercises, the treatment leaded to a remodeling of both mandibular condyles and the re-establishment of the oral functions, which resulted in the regaining of a normal mouth opening and closing, which was severely affected by the trauma after one year of treatment. It was also reported that the remodelling of the TMJ structures took about two years when the mandibular condyle was properly sitting in the mandibular fossae. Such a situation was observed in a TMJ tomogram after 28 months of completing the treatment. The only observed consequence after the conservative myofunctional treatment was a mandibular condyle (heart-shaped) on the left side [3].
Bone modelling and remodeling occurs by the interaction of the bone cells, the osteoblasts, the osteoclasts, and the osteocytes. During that remodeling process, the osteoblasts deposit a collagen matrix, which is later mineralized, whereas the osteoclasts remove the bone tissue, which is not viable or biologically stable, and the osteocytes coordinate that response on those other bone cells [4,5,6]. This process is known as intramembranous ossification, which, in the mandibular condyle, occurs together with endochondral ossification and cartilage matrix apposition, which becomes mineralized later, at the postero-superior surface of the mandibular condyle [7,8]. These biological processes are active during all humans’ life span [5,9]. In that context, oral dysfunctions or instability on the TMJs and/or in the dental occlusion may alter the results of the treatment, producing structural or functional changes in the long-term. The authors are presenting, here, the observations after ten years of completing the myofunctional treatment. It is important to notice that the patient did not use any retention appliance during the post-treatment period, up to the preparation of this report.
To determine the stability of a treatment where structural changes are produced in the craniofacial complex, as previously reported in this clinical case, it is necessary to follow up the results for an extended period of time. As was previously reported, a clinical case that was followed-up two years after the end of the treatment may not report degenerative changes, yet, at the mandibular condyles, nor might it report clinical symptoms or mandibular dynamics limitations. [3] In this context, a long-term follow-up report is required to show the stability of the treatment and the functional dynamics of the patient at present.
2. Case Follow-Up Report and Results
After ten years of completing the myofunctional treatment, new records, including photographs, as well as a TMJ tomogram, were taken. The clinical exam revealed the patient’s facial appearance, and craniofacial growth and development has continued within normal limits, maintaining a symmetric growth at the craniofacial complex (Figure 1). The dental occlusion stays symmetrical on both sides, with a normal vertical dimension, as it was at the end of the treatment ten years before (Figure 2A). The opening of the mouth (Figure 2B), as well as the mandibular lateral excursions, are currently under normal limits, demonstrating that the mandibular dynamics are within a normal range of motion (Figure 2C,D). The most recent tomogram revealed that the mandibular condyles are sitting in the mandibular fossae (Figure 3—upper), the right mandibular condyle has a normal shape, and the left mandibular condyle has a heart-shaped morphology, as was observed at the end of the myofunctional treatment and previously reported (Figure 3 middle and bottom). Besides that, the patient has not felt any symptoms, nor does the patient present any signs of temporomandibular dysfunction or craniofacial pain.

Figure 1.
(A) Frontal (B) and profile photos of the face of the reported patient ten years after the myofunctional treatment of the bilateral mandibular fracture.

Figure 2.
Intraoral photos of the (A) dental occlusion; (B) maximum opening; and (C,D) mandibular lateral excursions, showing the stability of the mandibular dynamics ten years after the myofunctional treatment of the mandibular condylar fracture.
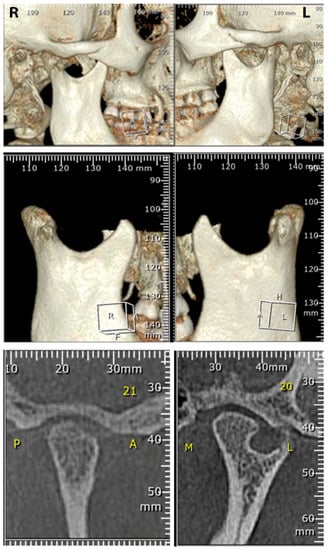
Figure 3.
Images showing the tomographic view of the condyles sitting on the mandibular fossae, as well as the heart-shaped mandibular condyle on the left TMJ (bottom), which is a consequence of the condylar fracture. R: Right; L: Left; P: Posterior; A: Anterior: M: Medial; L: Lateral.
By presenting these clinical and radiographic findings after ten years of completing the myofunctional treatment with the patient, who did not use any appliance in her mouth, confirms that the results reported previously continue to be stable, and no alteration in the structures, nor in the oral functions, have occurred in the long-term. The reasoning for not needing a retention appliance after a myofunctional approach for the treatment of condylar mandibular fractures, as well as the potential biological process occurring to maintain the features of the TMJs after the myofunctional treatment, as well as why a heart shaped mandibular condyle may appear after a mandibular condylar fracture, are discussed below.
3. Discussion
The mandibular condyle is covered by a secondary cartilage, which has been reported to be present and patent until late in life [9]. That secondary cartilage is formed by a layer of fibrous cartilage on the outer surface and a layer of hyaline cartilage at the inner surface. The role of the fibrous cartilage is to permit a smooth displacement of the mandibular condyle against the disc in the mandibular fossae at the TMJ, [10], thereby producing the mandibular excursions guided by the masticatory muscles. On the other hand, the inner layer, the hyaline cartilage, maintains the production of a cartilage matrix, which later becomes mineralized to apposition bone tissue in the mandibular condyle. That process is known as endochondral ossification [8,11].
The myofunctional treatment delivered to the patient presented here permitted us to remodel the mandibular condyle, inferring that that endochondral ossification was activated by a treatment that permitted the patient to heal the fractured mandibular condyles. It also re-established a correct position of the mandibular condyle in the fossae, as was shown on the initial report and confirmed with a follow-up tomogram ten years later. Furthermore, the mandibular dynamics, as well as the lateral excursions, were re-established and maintained over the last ten years, suggesting the features of the mandibular condyle are there with a fibrous cartilage at the outer surface. In that way, a smooth displacement of the mandibular condyle with the disc occurs in the mandibular fossae, producing no deviations during the opening and closing of the mouth, as well as proper lateral mandibular excursions, as shown in this report.
There is no general consensus on what the best approach for the treatment of fractures at the mandibular condyle could be. However, the literature supports that any approach intending to treat a mandibular condylar fracture must lead to a normal growth of the mandible in the future without potential long-term consequences, such as growth disturbances, facial asymmetry, and/or limited mouth opening [12]. Previous publications by one of the authors have shown that a conservative approach with myofunctional techniques rendered a remodeling of the mandibular condyle after a fracture without long-term consequences and a re-establishment of the madibular dynamics without limitations [13,14]. The results of the case presented here showed that the treatment produced satisfactory results in recovering the manibular dynamics with a normal oral function, which was stable in the long-term. In this way, the previous clinical case report describing the myofunctional treatment, [3] as well as this report presenting a ten-year follow up of the same clinical case, support the idea that a conservative approach to treat mandibular condylar fractures is a good alternative to treat mandibular condylar fractures, which leads to a full recovery of the condylar morphology, as well as a re-establishment of the oral functions [1]. Furthermore, functional exercises at an early stage of the treatment may help to recover the mandibular dynamics and oral functions [2].
The only consequence from the fracture, but not from the treatment, was a heart shaped mandibular condyle, which did not produce any limitation in mouth opening, facial asymmetry, or TMJ dysfunction. Why a mandibular condylar fracture may result in a heart-shaped mandibular condyle after a conservative myofunctional approach is not well understood yet. However, it has been previously reported in the literature as a consequence of a mandibular condylar fracture [10]. It occurred, in this case, on the left TMJ. That is a rare condition, also known as bifid mandibular condyle, which presents two heads. Such a condition may have a congenital or traumatic etiology [15]. In the case presented here, the appearance of the heart-shaped mandibular condyle is associated with a traumatic event, as has been reported by other authors [16]. Even though the knowledge of the authors leads to the idea that there are not studies focusing on this matter, a heart-shaped or bifid mandibular condyle has been proposed to appear due to an obstruction of the blood supply, which may cause the formation of a septum in the condyle area early during the development of the mandibular condyle or later during the remodeling process after a traumatic event involving a mandibular condylar fracture [17,18]. However, the biological process leading to the formation of a double head in the mandibular condyle after a traumatic event remains unknown.
Another long-term consequence reported with the presence of a heart shaped or bifid mandibular condyle is that patients may develop TMJ dysfunctions and craniofacial pain later in life [19]. In the case presented here, after ten years of the myofunctional treatment, the patient reported that she had no signs or symptoms of TMJ dysfunction, nor craniofacial pain. The later condition will continue being monitored in the future.
This report permits to confirm that a myofunctional approach produces stable results in the long-term. It has been reported in the literature that a correction of the oral dysfunctions with myofunctional exercises, concurrently with oral appliances, produces more stable results in the long-term [20]. This may be due to the fact that a myofunctional approach permits one to correct oral dysfunctions, which may be present in the system, and it maintains a proper intermaxillary relationship with the masticatory muscles, guiding the mandibular dynamics in a proper manner. Such a situation leads to a physiological loading of the bone tissue, maintaining a balance in the continuous remodeling of the bone tissue in the mandible and particularly in the mandibular condyle [5]. In that way, the re-establishment of a proper relationship of the mandibular condyle in the mandibular fossae has been maintained without altering the structural changes produced by the treatment on those sites. Such a biologically ideal homeostasis, produced by the myofunctional treatment, explains how the structural and functional results obtained with the treatment can be maintained in the long-term without any retentive appliance in the mouth.
4. Conclusions
The current report confirms that the myofunctional treatment, a conservative approach, delivered to this patient after a bilateral mandibular condylar fracture, has produced a stable long-term remodeling of the mandibular condyle. The treatment also re-established all the mandibular dynamics and lateral excursions within normal limits. All those results have been maintained over the last ten years, with no need of using retentive appliances, and the patient reported no signs or symptoms of TMJ dysfunction or craniofacial pain.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors state they do not have any conflict of interest for the publication of this article. They also declare that both authors contributed in the treatment provided to the patient and the preparation of this manuscript.
References
- Staderini, E.; Patini, R.; Tepedino, M.; Gasparini, G.; Zimbalatti, M.A.; Marradi, F.; Gallenzi, P. Radiographic assessment of pediatric condylar fractures after conservative treatment with functional appliances—A systematic review. Int. J. Environ. Res. Public. Health 2020, 17, 9204. [Google Scholar] [CrossRef] [PubMed]
- Zachariades, N.; Mezitis, M.; Mourouzis, C.; Spanou, A. Fractures of the mandibular condyle: A review of 466 cases. Literature review, reflections on treatment and proposals. J. Cranio-Maxillofac. Surg. 2006, 34, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Bedoya-Rodriguez, A.; Ramirez-Yanez, G. Bilateral condylar fracture: A case treated with a conservative myofunctional approach. J. Clin. Pediatr. Dent. 2020, 44, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Clarke, B. Normal bone anatomy and physiology. Clin. J. Am. Soc. Nephrol. 2008, 3, S131–S139. [Google Scholar] [CrossRef] [PubMed]
- Frost, H. A 2003 update of bone physiology and Wolff’s law for clinicians. Angle. Orthod. 2004, 74, 3–15. [Google Scholar] [PubMed]
- Hazelwood, S.J.; Martin, R.B.; Rashid, M.M.; Rodrigo, J.J. A mechanistic model for internal bone remodeling exhibits different dynamic responses in disuse and overload. J. Biomech. 2001, 34, 299–308. [Google Scholar] [CrossRef] [PubMed]
- Luder, H.U. Frequency and distribution of articular tissue features in adult human mandibular condyles: A semiquantitative light microscopic study. Anat. Rec. 1997, 248, 18–28. [Google Scholar] [CrossRef]
- Stutzmann, J.; Petrovic, A. Intrinsic regulation of the condylar cartilage growth rate. Eur. J. Orthod. 1979, 1, 41–54. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Yanez, G.; Scott, J. Architecture of the Mandibular Condylar Cartilage of Elderly Individuals: A Semiquantitative Light Microscopic Histological Study. J. Contemp. Dent. Pract. 2019, 20, 768–772. [Google Scholar] [CrossRef] [PubMed]
- Thilander, B.; Carlsson, G.; Ingervall, B. Postnatal development of the human temporomandibular joint. I. A histological study. Acta. Odontol. Scand. 1976, 34, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Luder, H.; Schroeder, H. Light and electron microscopic morphology of the temporomandibular joint in growing and mature crab-eating monkeys (Macaca fascicularis): The condylar articular layer. Anat. Embryol. 1990, 181, 499–511. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, J.; Phillips, J. Pediatric Facial Fractures and Potential Long-Term Growth Disturbances. Craniomaxillofac. Trauma Reconstr. 2011, 4, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Mejia-Gomez, C.; Ramirez-Yanez, G. Mandibular condylar aplasia treated with a functional approach. J. Clin. Pediatr. Dent. 2013, 38, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Yañez, G.; Saxby, P.; Young, W. Condylar fracture: Nontretament case followed over 23 years. World J. Orthod. 2002, 3, 349–352. [Google Scholar]
- Borrás-Ferreres, J.; Sánchez-Torres, A.; Gay-Escoda, C. Bifid mandibular condyles: A systematic review. Med. Oral. Patol. Oral. Cir. Bucal. 2018, 23, e672–e680. [Google Scholar] [CrossRef] [PubMed]
- Antoniades, K.; Karakasis, D.; Elephtheriades, J. Bifid mandibular condyle resulting from a sagittal fracture of the condylar head. British. J. Oral. Maxillofac. Surg. 1993, 31, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Blackwood, H.J.J. The double-headed mandibular condyle. Am. J. Phys. Anthropol. 1957, 15, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hrdlička, A. Lower jaw: Double condyles. Am. J. Phys. Anthropol. 1941, 28, 75–89. [Google Scholar] [CrossRef]
- Coclici, A.; Raluca, A.; Roman, R.A.; Crasnean, E.; Faur, C.; Bran, S.; Baciut, M.; Dinu, C.; Hedesiu, M. An overview of the post-traumatic mandibular bifid condyle. Maedica 2020, 15, 258–265. [Google Scholar] [PubMed]
- Smithpeter, J.; Covell, D.J. Relapse of anterior open bites treated with orthodontic appliances with and without orofacial myofunctional therapy. Am. J. Orthod. Dentofacial. Orthop. 2010, 137, 605–614. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).