From Denture to the Final Implant-Supported Prosthesis Using a Full-Digital Protocol: A Dental Technique
Abstract
:1. Introduction
2. Materials and Methods
Technique Description
- 1.
- Perform the patient’s documentation including clinical extra- and intraoral photos in occlusion and smiling (Figure 1).
- 2.
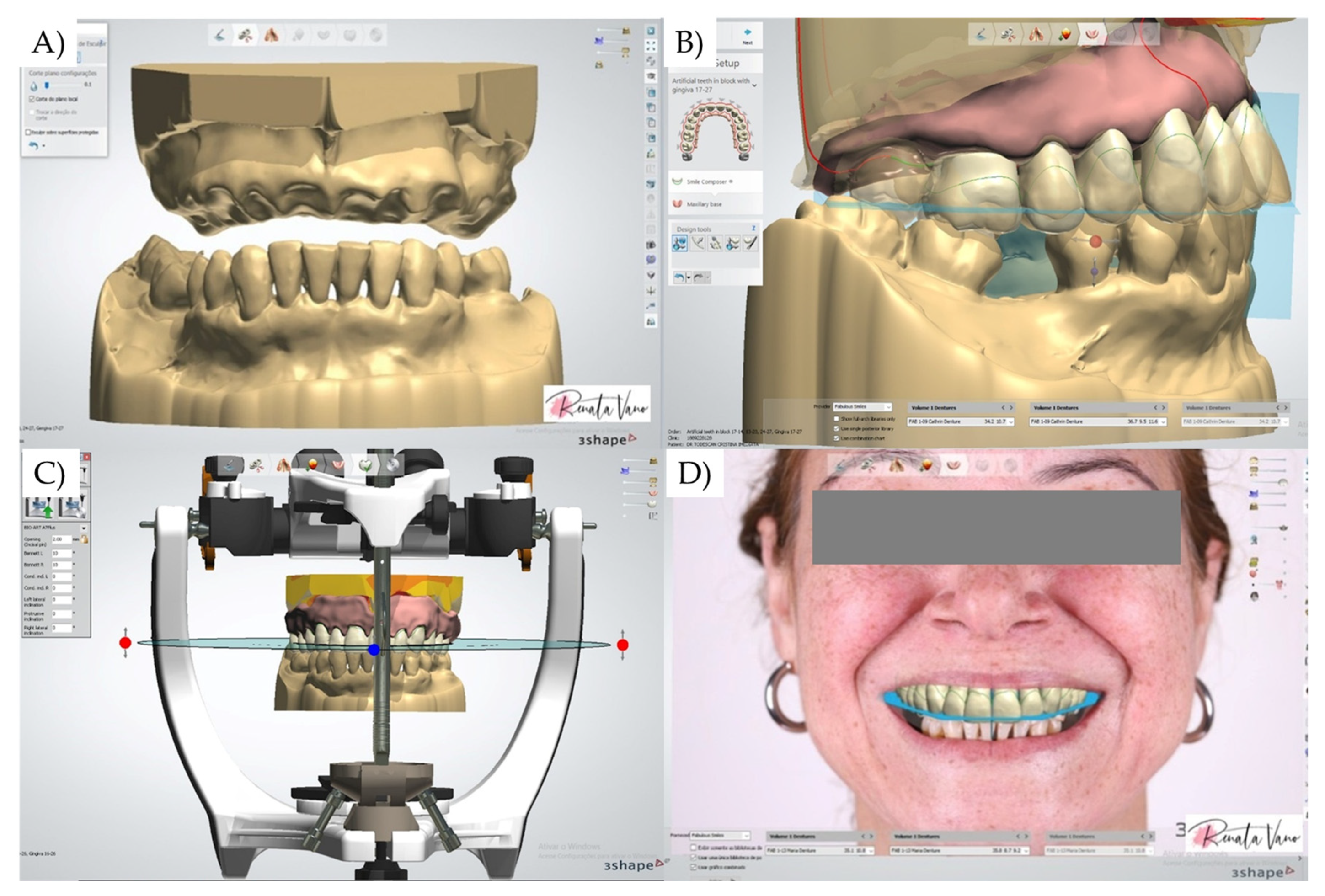
- With the aid of an intraoral scanner device (Medit i500, Medit Corp., Seul, South Korea), perform a digital scan of the dentition (Figure 2). Before scanning, set up the order to export standard tessellation language (STL) files. Import the acquired digital data into CAD software (Dental System 2020; 3Shape Dental System; 3Shape A/S, Copenhagen, Denmark). With the aid of a modeling tool, perform a virtual extraction of the crowns and provide a new complete denture design with corrected esthetics and prosthetic outcomes following the workflow indicated by the software, and generate the new STL files.
- 3.
- Process the STL file of the new denture by using a 3D printer (5100 3D Systems; Nextdent) and denture resin (Denture 3D+; Nextdent). Follow the post-processing and finishing technique according to the manufacturer’s instructions (Figure 3).
- 4.
- Follow the surgical plan, perform the necessary tooth extraction and install the printed denture during the healing period.
- 5.
- After healing, perform artificial landmarks using gutta-percha on the external surface of the buccal flange. Make a CBCT scan with and without the denture record in place (Figure 4). For this, the double tomography technique is used: first, the tomography is made with the patient wearing the denture with the gutta-percha marks in a seated position, then a second tomography is performed only for the prosthesis (outside the mouth).
- 6.
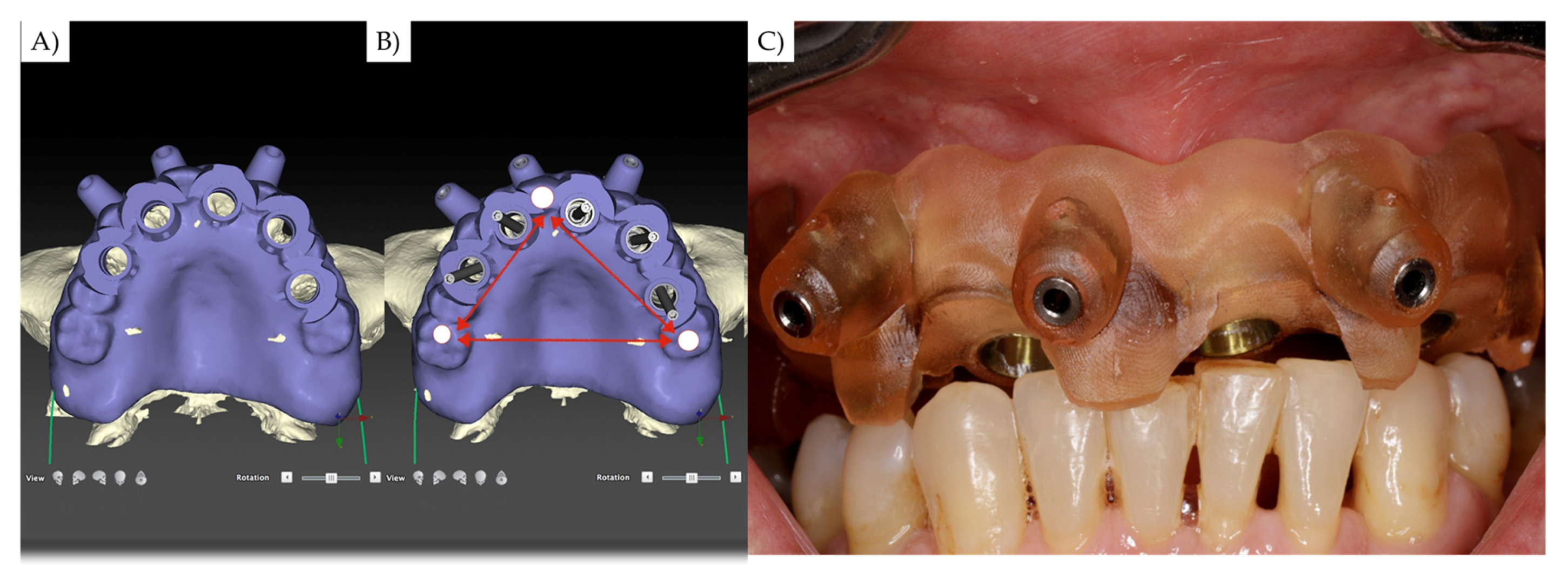
- Identify at least 3 regions with positive and negative features that exhibit adequate contact intraorally. These areas need to be as far apart as possible (Figure 5).
- 7.
- Import the DICOM file of the CBCT and the STL file of the digital scan of the dentures into the guided treatment planning software (DTX, KaVo Kerr, Brea, CA, USA) (Figure 6).
- 8.
- Align the STL file with the DICOM file to obtain the relationship between the arches and denture. Then, plan the implants’ 3D position according to your patient, individualizing the surgical guide with buccal screws to stabilize the device during the surgical procedure.
- 9.
- After the implants’ placement, use a scan body in each implant to scan the arches (Medit i500, Medit Corp., Seul, South Korea) and the implants according to the manufacturer’s instructions. Complete the scan and remove unnecessary areas (Figure 6).
- 10.
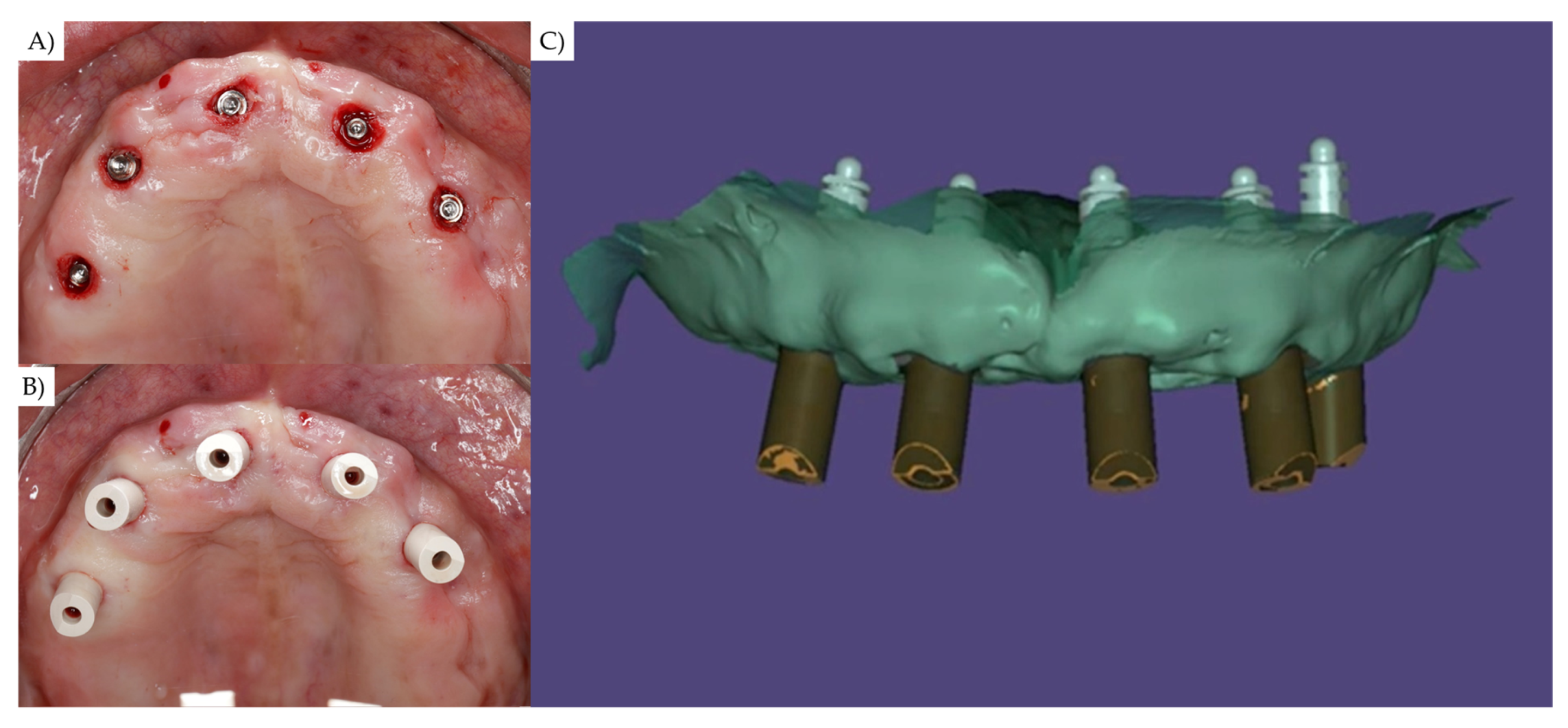
- Perform a second scan with a scan body and surgical guide placed in position. For this step, it is necessary to remove the restrictive metallic cylinders from the surgical guide. The surgical guide must by fixed by endosseuous fixation screws (Figure 7).
- 11.
- In the CAD software, align the antagonist arch scan with both STL file of the previous digital scan. This step will allow the recording of planned teeth position, 3D implants’ positioning, and oral tissue characteristics, considering the maxillomandibular relationship and vertical dimension of occlusion (Figure 7).
- 12.
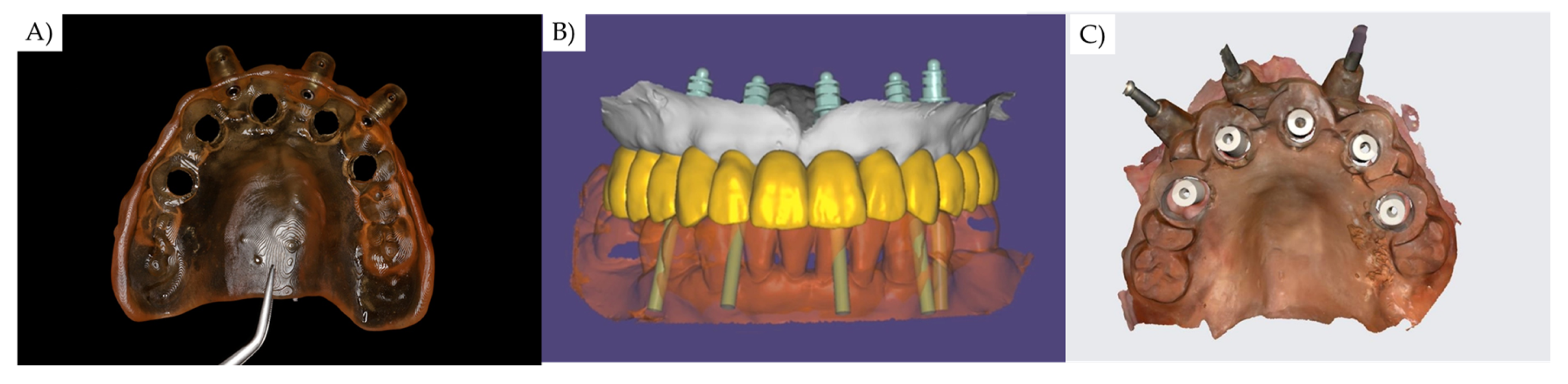
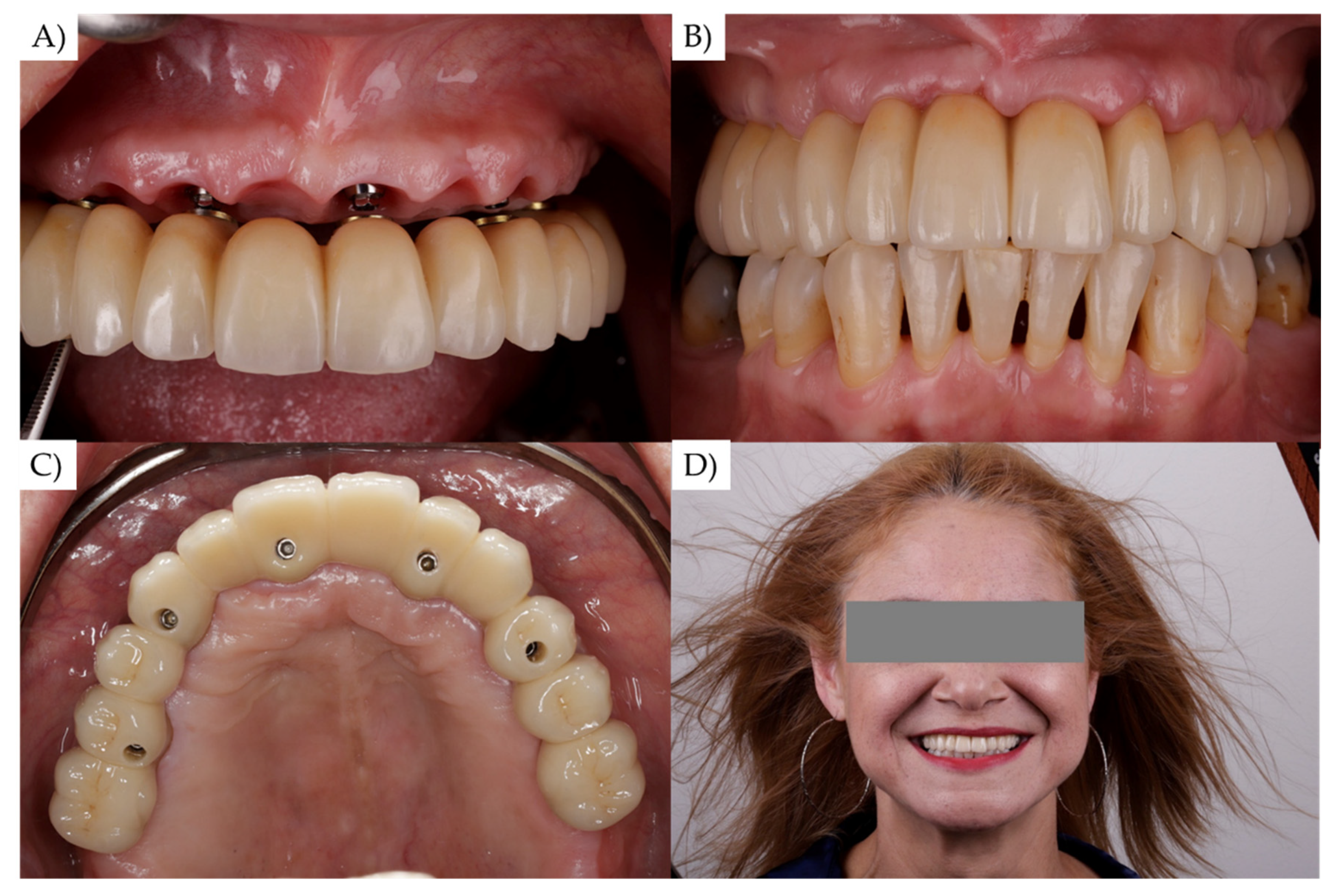
- Proceed with the prosthesis manufacturing based on the acquired information (Figure 8).
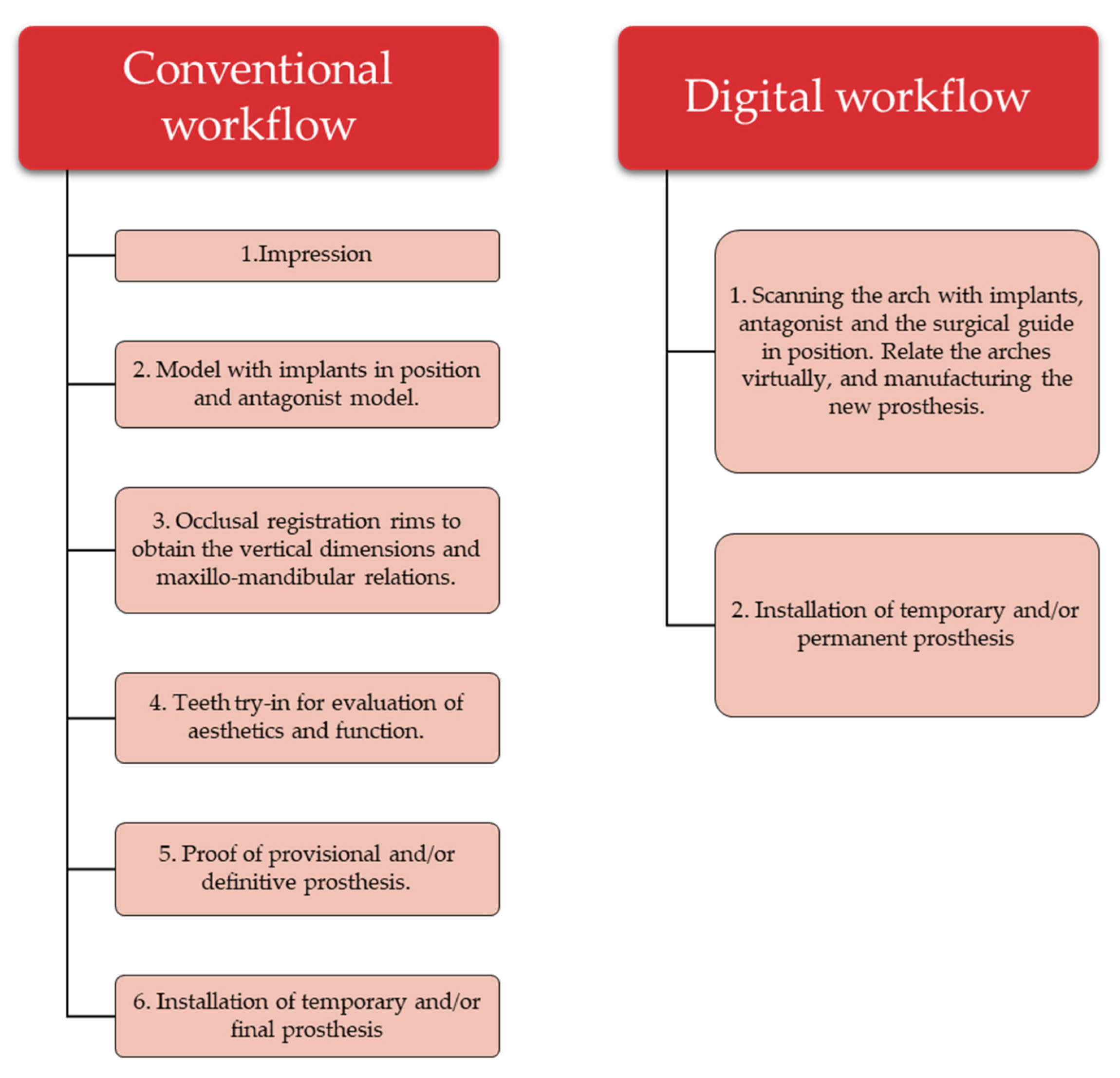
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Michelinakis, G.; Apostolakis, D.; Kamposiora, P.; Papavasiliou, G.; Özcan, M. The direct digital workflow in fixed implant prosthodontics: A narrative review. BMC Oral Health 2021, 21, 37. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Giugovaz, M.G.; Park, S.H.; Revilla-León, M. 3D virtual patient representation for guiding a maxillary overdenture fabrication: A dental technique. J. Prosthodont. 2021, 30, 636–641. [Google Scholar] [CrossRef] [PubMed]
- Arcas, L.P.B.; Tribst, J.P.M.; Baroudi, K.; Amaral, M.; da Silva-Concílio, L.R.; Vitti, R.P. Dimensional accuracy comparison of physical models generated by digital impression/3D-printing or analog impression/plaster methods. Int. J. Odontostomatol. 2021, 15, 562–568. [Google Scholar] [CrossRef]
- Griseto, N.T.; Gallucci, G.O. Digital maxillomandibular relationship registration for an edentulous maxilla: A dental technique. J. Prosthet. Dent. 2021, 125, 858–861. [Google Scholar] [CrossRef] [PubMed]
- Moura, G.F.; Siqueira, R.; Meirelles, L.; Maska, B.; Wang, H.-L.; Mendonça, G. Denture scanning technique for computer-guided implant-supported restoration treatment of edentulous patients. J. Prosthet. Dent. 2021, 125, 726–731. [Google Scholar] [CrossRef] [PubMed]
- Mai, H.-N.; Lee, D.-H. A digital technique to replicate edentulous arches with functional borders and accurate maxillomandibular relationship for digital complete denture. J. Prosthodont. 2020, 29, 356–359. [Google Scholar] [CrossRef] [PubMed]
- Flügge, T.; van der Meer, W.J.; Gonzalez, B.G.; Vach, K.; Wismeijer, D.; Wang, P. The accuracy of different dental impression techniques for implant-supported dental prostheses: A systematic review and meta-analysis. Clin. Oral Implants Res. 2018, 29 (Suppl. 16), 374–392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Figueras-Alvarez, O.; Cantó-Navés, O.; Real-Voltas, F.; Roig, M. Protocol for the clinical assessment of passive fit for multiple implant-supported prostheses: A dental technique. J. Prosthet. Dent. 2020. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, R.A.C.; Cabral, B.L.; Siqueira, G.R.; Mendonça, G.; Wang, H.L. Using digital technique to obtain the ideal soft tissue contour in immediate implants with provisionalization. Implant Dent. 2019, 28, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Bover-Ramos, F.; Viña-Almunia, J.; Cervera-Ballester, J.; Peñarrocha-Diago, M.; García-Mira, B. Accuracy of implant placement with computer-guided surgery: A systematic review and meta-analysis comparing cadaver, clinical, and in vitro studies. Int. J. Oral Maxillofac. Implant 2018, 33, 101–115. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Galli, M.; Chen, Z.; Venezia, P.; Mangano, F.; Lepidi, L. A novel digital technique for maintaining maxillomandibular relations in fixed prosthetic rehabilitations. J. Dent. 2021, 114, 103798. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; de Oliveira Dal Piva, A.M.; da Silva-Concílio, L.R.; Ausiello, P.; Kalman, L. Influence of implant-abutment contact surfaces and prosthetic screw tightening on the stress concentration, fatigue life and microgap formation: A finite element analysis. Oral 2021, 1, 88–101. [Google Scholar] [CrossRef]
- Michelinakis, G.; Nikolidakis, D. Using the surgical guide for impression-free digital bite registration in the edentulous maxilla-a technical note. Int. J. Implant Dent. 2019, 5, 19. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.-W.; Liu, Q.; Yue, Z.-G.; Hou, J.-X.; Afrashtehfar, K.I. Digital workflow for full-arch immediate implant placement using a stackable surgical guide fabricated using SLM technology. J. Prosthodont. 2021, 30, 645–650. [Google Scholar] [CrossRef] [PubMed]
- Dahiya, A.; Garbacea, A.; Kattadiyil, M.T.; AlHelal, A. Digital technology for performing a nasopalatine and greater palatine nerve block with a modified implant surgical guide: A technique article. J. Prosthet. Dent. 2018, 120, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Turkyilmaz, I. Keys to achieving successful restoratively driven implant placement with CAD/CAM surgical guide: A technical note. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 462–466. [Google Scholar] [CrossRef] [PubMed]
- Datte, C.E.; Datte, F.B.; Borges, A.L.; Campos, J.F.; Lopes, G.D.; Tribst, J.P.; Nishioka, R.S. The influence of restorative material, bone height and implant system on the stress distribution of implant-supported posterior crowns. Int. J. Dev. Res. 2021, 11, 1–7. [Google Scholar]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Todescan, F.F.; Hayashi, M.M.; Giugni, L.R.; Bottino, M.A.; Tribst, J.P.M. From Denture to the Final Implant-Supported Prosthesis Using a Full-Digital Protocol: A Dental Technique. Oral 2021, 1, 332-339. https://doi.org/10.3390/oral1040033
Todescan FF, Hayashi MM, Giugni LR, Bottino MA, Tribst JPM. From Denture to the Final Implant-Supported Prosthesis Using a Full-Digital Protocol: A Dental Technique. Oral. 2021; 1(4):332-339. https://doi.org/10.3390/oral1040033
Chicago/Turabian StyleTodescan, Francisco Fernando, Marcos Masayuki Hayashi, Luiz Roberto Giugni, Marco Antonio Bottino, and João Paulo Mendes Tribst. 2021. "From Denture to the Final Implant-Supported Prosthesis Using a Full-Digital Protocol: A Dental Technique" Oral 1, no. 4: 332-339. https://doi.org/10.3390/oral1040033
APA StyleTodescan, F. F., Hayashi, M. M., Giugni, L. R., Bottino, M. A., & Tribst, J. P. M. (2021). From Denture to the Final Implant-Supported Prosthesis Using a Full-Digital Protocol: A Dental Technique. Oral, 1(4), 332-339. https://doi.org/10.3390/oral1040033







