Survival of Fiber-Reinforced Composite Resin Post-Restored vs. Cast Post-and-Core-Restored Teeth: A Retrospective Clinical Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Treatment Procedures
2.2.1. Cast Post-and-Core
2.2.2. Fiber-Reinforced Composite Resin Post
2.3. Variables, Treatment and Follow-Up Procedures
2.4. Matched Pair Design
2.5. Statistical Analysis and Data Processing
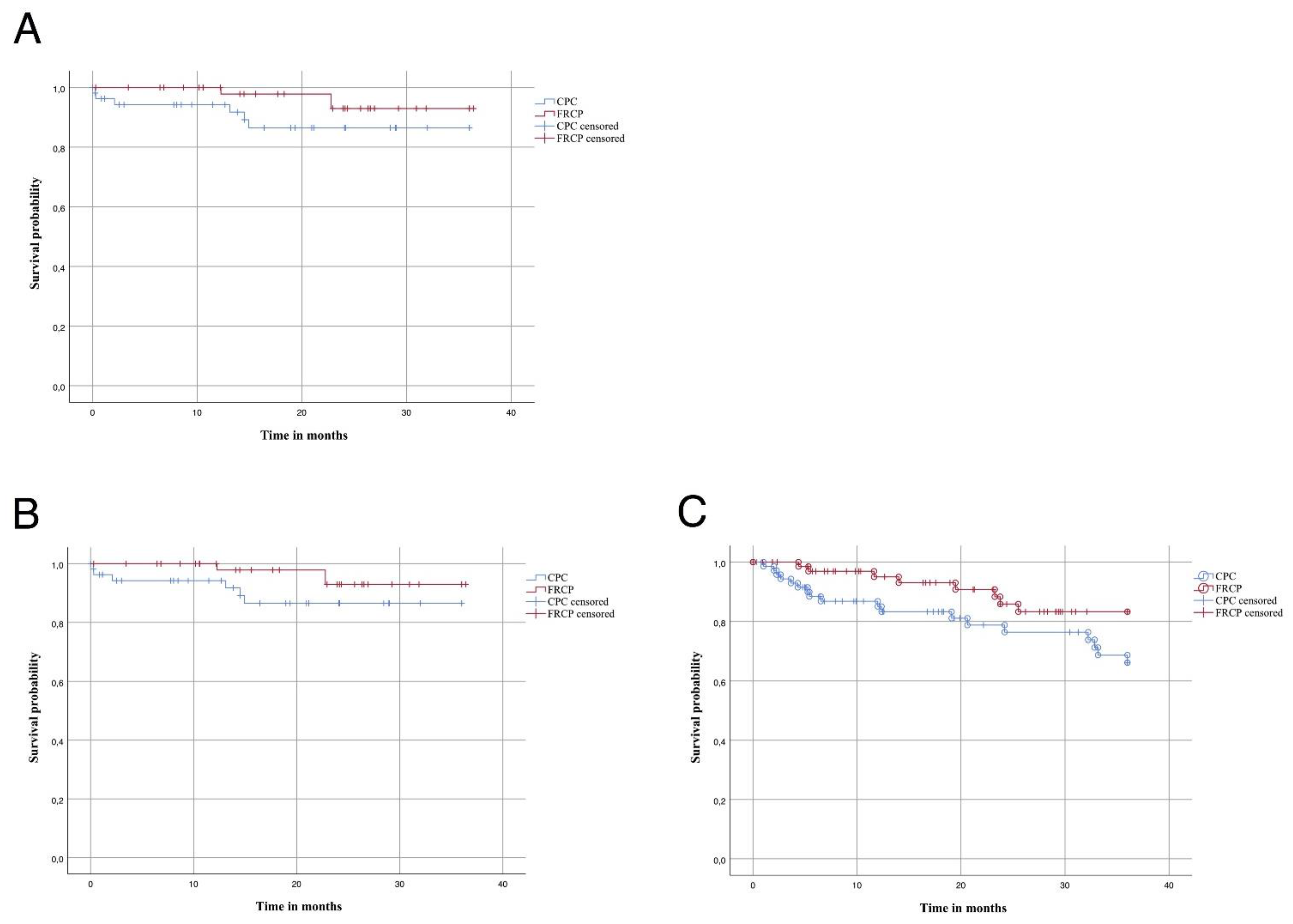
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Juloski, J.; Radovic, I.; Goracci, C.; Vulicevic, Z.R.; Ferrari, M. Ferrule effect: A literature review. J. Endod. 2012, 38, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Theodosopoulou, J.N.; Chochlidakis, K.M. A systematic review of dowel (post) and core materials and systems. J. Prosthodont. 2009, 18, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Naumann, M.; Kiessling, S.; Seemann, R. Treatment concepts for restoration of endodontically treated teeth: A nationwide survey of dentists in Germany. J. Prosthet. Dent. 2006, 96, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Bialy, M.; Targonska, S.; Szust, A.; Wiglusz, R.J.; Dobrzynski, M. In Vitro Fracture Resistance of Endodontically Treated Premolar Teeth Restored with Prefabricated and Custom-Made Fibre-Reinforced Composite Posts. Materials 2021, 14, 6214. [Google Scholar] [CrossRef]
- Tronstad, L.; Asbjornsen, K.; Doving, L.; Pedersen, I.; Eriksen, H.M. Influence of coronal restorations on the periapical health of endodontically treated teeth. Endod. Dent. Traumatol. 2000, 16, 218–221. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.; Gutteridge, D.L. An in vitro study of coronal microleakage in root-canal-treated teeth restored by the post and core technique. Int. Endod. J. 1997, 30, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Peroz, I.; Blankenstein, F.; Lange, K.-P.; Naumann, M. Restoring endodonticall treated teeth with posts and cores—A review. Quintessence Int. 2005, 36, 737–745. [Google Scholar]
- Duret, B.; Reynaud, M.; Duret, F. A new concept of corono-radicular reconstruction, the Composipost (2). Chir. Dent. Fr. 1990, 60, 69–77. [Google Scholar] [PubMed]
- Bateman, G.; Ricketts, D.N.; Saunders, W.P. Fibre-based post systems: A review. Br. Dent. J. 2003, 195, 43–48; discussion 37. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, R.S.; Robbins, J.W. Post placement and restoration of endodontically treated teeth: A literature review. J. Endod. 2004, 30, 289–301. [Google Scholar] [CrossRef]
- Marchionatti, A.M.E.; Wandscher, V.F.; Rippe, M.P.; Kaizer, O.B.; Valandro, L.F. Clinical performance and failure modes of pulpless teeth restored with posts: A systematic review. Braz. Oral Res. 2017, 31, e64. [Google Scholar] [CrossRef] [Green Version]
- Morgano, S.M.; Brackett, S.E. Foundation restorations in fixed prosthodontics: Current knowledge and future needs. J. Prosthet. Dent. 1999, 82, 643–657. [Google Scholar] [CrossRef]
- Zhou, L.; Wang, Q. Comparison of fracture resistance between cast posts and fiber posts: A meta-analysis of literature. J. Endod. 2013, 39, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Heydecke, G.; Peters, M.C. The restoration of endodontically treated, single-rooted teeth with cast or direct posts and cores: A systematic review. J. Prosthet. Dent. 2002, 87, 380–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naumann, M.; Schmitter, M.; Frankenberger, R.; Krastl, G. “Ferrule Comes First. Post Is Second!” Fake News and Alternative Facts? A Systematic Review. J. Endod. 2018, 44, 212–219. [Google Scholar] [CrossRef]
- Sorensen, J.A.; Engelman, M.J. Ferrule design and fracture resistance of endodontically treated teeth. J. Prosthet. Dent. 1990, 63, 529–536. [Google Scholar] [CrossRef]
- Stankiewicz, N.R.; Wilson, P.R. The ferrule effect: A literature review. Int. Endod. J. 2002, 35, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Bergman, B.; Lundquist, P.; Sjogren, U.; Sundquist, G. Restorative and endodontic results after treatment with cast posts and cores. J. Prosthet. Dent. 1989, 61, 10–15. [Google Scholar] [CrossRef]
- Eckerbom, M.; Magnusson, T.; Martinsson, T. Prevalence of apical periodontitis, crowned teeth and teeth with posts in a Swedish population. Endod. Dent. Traumatol. 1991, 7, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Eckerbom, M.; Magnusson, T.; Martinsson, T. Reasons for and incidence of tooth mortality in a Swedish population. Endod. Dent. Traumatol. 1992, 8, 230–234. [Google Scholar] [CrossRef]
- Naumann, M.; Koelpin, M.; Beuer, F.; Meyer-Lueckel, H. 10-year survival evaluation for glass-fiber-supported postendodontic restoration: A prospective observational clinical study. J. Endod. 2012, 38, 432–435. [Google Scholar] [CrossRef]
- Naumann, M.; Reich, S.; Nothdurft, F.P.; Beuer, F.; Schirrmeister, J.F.; Dietrich, T. Survival of glass fiber post restorations over 5 years. Am. J. Dent. 2008, 21, 267–272. [Google Scholar]
- Martino, N.; Truong, C.; Clark, A.E.; O’Neill, E.; Hsu, S.M.; Neal, D.; Esquivel-Upshaw, J.F. Retrospective analysis of survival rates of post-and-cores in a dental school setting. J. Prosthet. Dent. 2020, 123, 434–441. [Google Scholar] [CrossRef]
- Fokkinga, W.A.; Kreulen, C.M.; Bronkhorst, E.M.; Creugers, N.H. Up to 17-year controlled clinical study on post-and-cores and covering crowns. J. Dent. 2007, 35, 778–786. [Google Scholar] [CrossRef] [PubMed]
- Naumann, M.; Rosentritt, M.; Preuss, A.; Dietrich, T. The effect of alveolar bone loss on the load capability of restored endodontically treated teeth: A comparative in vitro study. J. Dent. 2006, 34, 790–795. [Google Scholar] [CrossRef]
- Asmussen, E.; Peutzfeldt, A.; Heitmann, T. Stiffness, elastic limit, and strength of newer types of endodontic posts. J. Dent. 1999, 27, 275–278. [Google Scholar] [CrossRef]
- Kinney, J.H.; Habelitz, S.; Marshall, S.J.; Marshall, G.W. The importance of intrafibrillar mineralization of collagen on the mechanical properties of dentin. J. Dent. Res. 2003, 82, 957–961. [Google Scholar] [CrossRef] [Green Version]
- Mannocci, F.; Ferrari, M.; Watson, T.F. Intermittent loading of teeth restored using quartz fiber, carbon-quartz fiber, and zirconium dioxide ceramic root canal posts. J. Adhes. Dent. 1999, 1, 153–158. [Google Scholar] [PubMed]
- Ferrari, M.; Vichi, A.; Garcia-Godoy, F. Clinical evaluation of fiber-reinforced epoxy resin posts and cast post and cores. Am. J. Dent. 2000, 13, 15B–18B. [Google Scholar] [PubMed]
- Monticelli, F.; Goracci, C.; Ferrari, M. Micromorphology of the fiber post-resin core unit: A scanning electron microscopy evaluation. Dent. Mater. 2004, 20, 176–183. [Google Scholar] [CrossRef]
- Glazer, B. Restoration of endodontically treated teeth with carbon fibre posts—A prospective study. J. Can. Dent. Assoc. 2000, 66, 613–618. [Google Scholar]
- Lamichhane, A.; Xu, C.; Zhang, F.Q. Dental fiber-post resin base material: A review. J. Adv. Prosthodont. 2014, 6, 60–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Rijk, W.G. Removal of fiber posts from endodontically treated teeth. Am. J. Dent. 2000, 13, 19B–21B. [Google Scholar]
- Rehmann, P.; Weber, A.; Wöstmann, B.; Ferger, P. Clinical evaluation of teeth fitted with telescope crowns for retaining a partial dentur. Dtsch. Zahnärztl. Z. 2007, 62, 99–103. [Google Scholar]
- Wegner, P.K.; Freitag, S.; Kern, M. Survival rate of endodontically treated teeth with posts after prosthetic restoration. J. Endod. 2006, 32, 928–931. [Google Scholar] [CrossRef] [PubMed]
- Wostmann, B.; Balkenhol, M.; Weber, A.; Ferger, P.; Rehmann, P. Long-term analysis of telescopic crown retained removable partial dentures: Survival and need for maintenance. J. Dent. 2007, 35, 939–945. [Google Scholar] [CrossRef]
- Aquilino, S.A.; Caplan, D.J. Relationship between crown placement and the survival of endodontically treated teeth. J. Prosthet. Dent. 2002, 87, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Caplan, D.J.; Kolker, J.; Rivera, E.M.; Walton, R.E. Relationship between number of proximal contacts and survival of root canal treated teeth. Int. Endod. J. 2002, 35, 193–199. [Google Scholar] [CrossRef]
- Cagidiaco, M.C.; Garcia-Godoy, F.; Vichi, A.; Grandini, S.; Goracci, C.; Ferrari, M. Placement of fiber prefabricated or custom made posts affects the 3-year survival of endodontically treated premolars. Am. J. Dent. 2008, 21, 179–184. [Google Scholar]
- Naumann, M.; Blankenstein, F.; Dietrich, T. Survival of glass fibre reinforced composite post restorations after 2 years-an observational clinical study. J. Dent. 2005, 33, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Schmitter, M.; Hamadi, K.; Rammelsberg, P. Survival of two post systems—Five-year results of a randomized clinical trial. Quintessence Int. 2011, 42, 843–850. [Google Scholar] [PubMed]
- Schmitter, M.; Rammelsberg, P.; Gabbert, O.; Ohlmann, B. Influence of clinical baseline findings on the survival of 2 post systems: A randomized clinical trial. Int. J. Prosthodont. 2007, 20, 173–178. [Google Scholar] [PubMed]
| FRCP | ||||
|---|---|---|---|---|
| Failure | Survival | In Total | ||
| CPC | Failure | 0 (0%) | 10 (9%) | 10 |
| Survival | 4 (4%) | 95 (87%) | 99 | |
| In total | 4 | 105 | 109 (100%) | |
| CPC | FRCP | |
|---|---|---|
| Post length < 10 mm | 64 | 61 |
| Post length ≥ 10 mm | 29 | 54 |
| Post length > Crown height | 70 | 97 |
| Post length = Crown height | 15 | 30 |
| Post length < Crown height | 2 | 3 |
| Survival | Failure | Restorable Failure | Unrestorable Failure | |||
|---|---|---|---|---|---|---|
| total | total | CPC | FRCP | CPC | FRCP | |
| Tooth type | ||||||
| Upper jaw | ||||||
| Incisors | 18 (8.2%) | 2 (0.9%) | 2 | |||
| Canines | 39 (17.9%) | 7 (3.2%) | 6 | 1 | ||
| Premolars | 36 (16.5%) | 2 (0.9%) | 1 | 1 | ||
| Molars | 14 (6.4%) | |||||
| Lower jaw | ||||||
| Incisors | 3 (1.4%) | 1 (0.4%) | 1 | |||
| Canines | 24 (11%) | |||||
| Premolars | 56 (25.7%) | 2 (0.9%) | 2 | |||
| Molars | 14 (6.4%) | |||||
| Definitive restoration | ||||||
| Crown | 77 (35.3%) | 3 (1.4%) | 3 | |||
| Fixed partial denture | 22 (10%) | |||||
| Telescopic denture | 88 (40.4%) | 10 (4.6%) | 5 | 2 | 3 | |
| Removable partial denture | 14 (6.4%) | |||||
| No prosthetic restoration | 3 (1.4%) | 1 (0.4%) | 1 | |||
| Number of proximal contacts | ||||||
| 0 | 89 (40.8%) | 9 (4.1%) | 5 | 1 | 3 | |
| 1–2 | 115 (52.7%) | 5 (2.3%) | 3 | 1 | 1 | |
| Complication | No Failure | Restorable Failure | Unrestorable Failure | |||
|---|---|---|---|---|---|---|
| CPC | FRCP | CPC | FRCP | CPC | FRCP | |
| None | 127 | 145 | ||||
| Post fracture | 2 | 6 | ||||
| Loss of retention | 15 | 1 | 1 | |||
| Apical ostitis | 3 | 1 | ||||
| Tooth mobility | 1 | |||||
| Root fracture | 7 | 2 | ||||
| Secondary caries | 1 | 2 | ||||
| Uncertain prognosis | 3 | 1 | ||||
| Pain | 4 | 2 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bunz, O.; Iwantschenko, D.; Tulka, S.; Barthel-Zimmer, C.; Piwowarczyk, A. Survival of Fiber-Reinforced Composite Resin Post-Restored vs. Cast Post-and-Core-Restored Teeth: A Retrospective Clinical Study. Oral 2021, 1, 340-349. https://doi.org/10.3390/oral1040034
Bunz O, Iwantschenko D, Tulka S, Barthel-Zimmer C, Piwowarczyk A. Survival of Fiber-Reinforced Composite Resin Post-Restored vs. Cast Post-and-Core-Restored Teeth: A Retrospective Clinical Study. Oral. 2021; 1(4):340-349. https://doi.org/10.3390/oral1040034
Chicago/Turabian StyleBunz, Oskar, Darja Iwantschenko, Sabrina Tulka, Claudia Barthel-Zimmer, and Andree Piwowarczyk. 2021. "Survival of Fiber-Reinforced Composite Resin Post-Restored vs. Cast Post-and-Core-Restored Teeth: A Retrospective Clinical Study" Oral 1, no. 4: 340-349. https://doi.org/10.3390/oral1040034
APA StyleBunz, O., Iwantschenko, D., Tulka, S., Barthel-Zimmer, C., & Piwowarczyk, A. (2021). Survival of Fiber-Reinforced Composite Resin Post-Restored vs. Cast Post-and-Core-Restored Teeth: A Retrospective Clinical Study. Oral, 1(4), 340-349. https://doi.org/10.3390/oral1040034






