The Knowledge, Awareness, and Attitude Regarding COVID-19 among Trinidad and Tobago Dentists. A Cross-Sectional Survey
Abstract
:1. Introduction
2. Methods
3. Results
4. Demographic Results
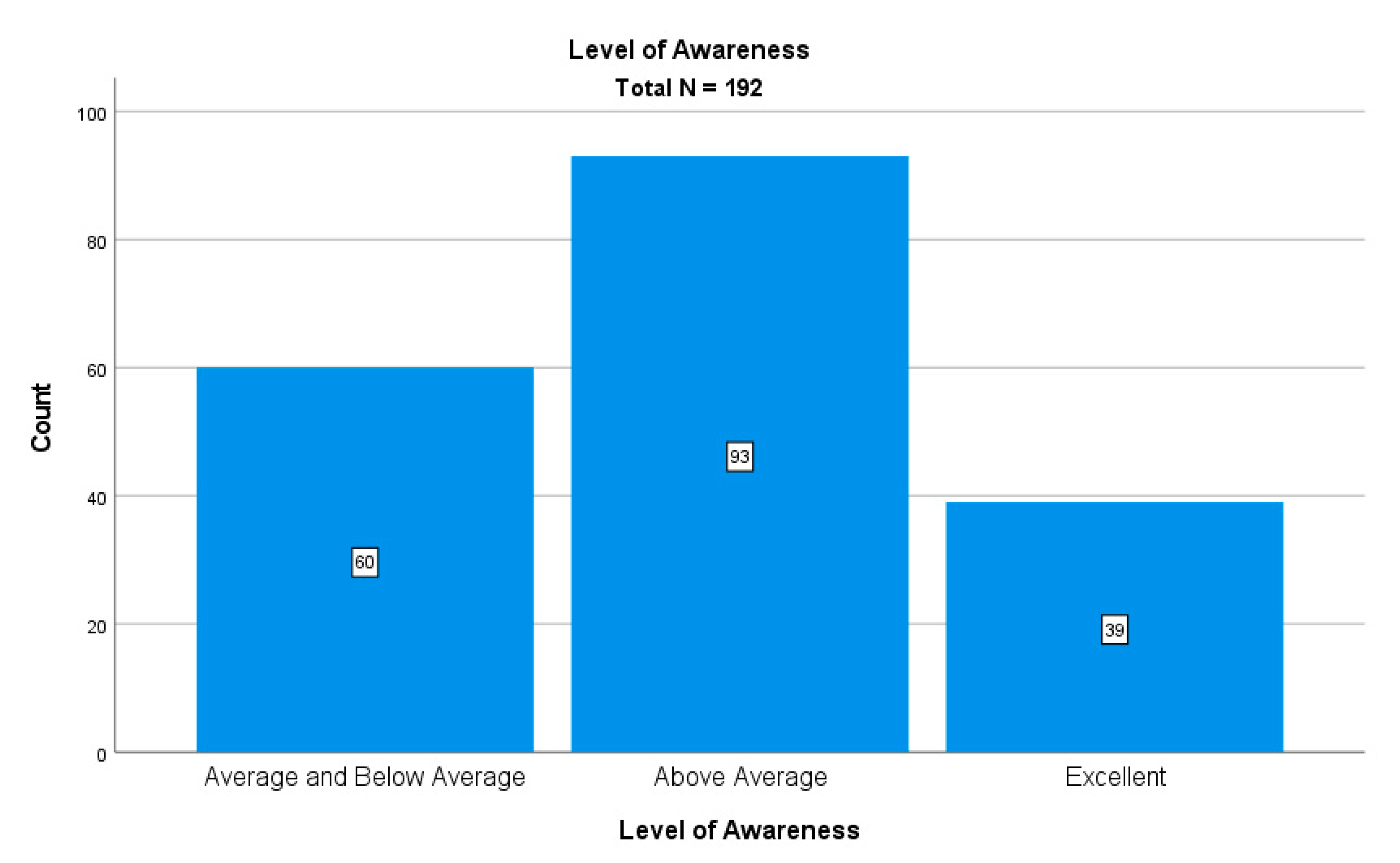
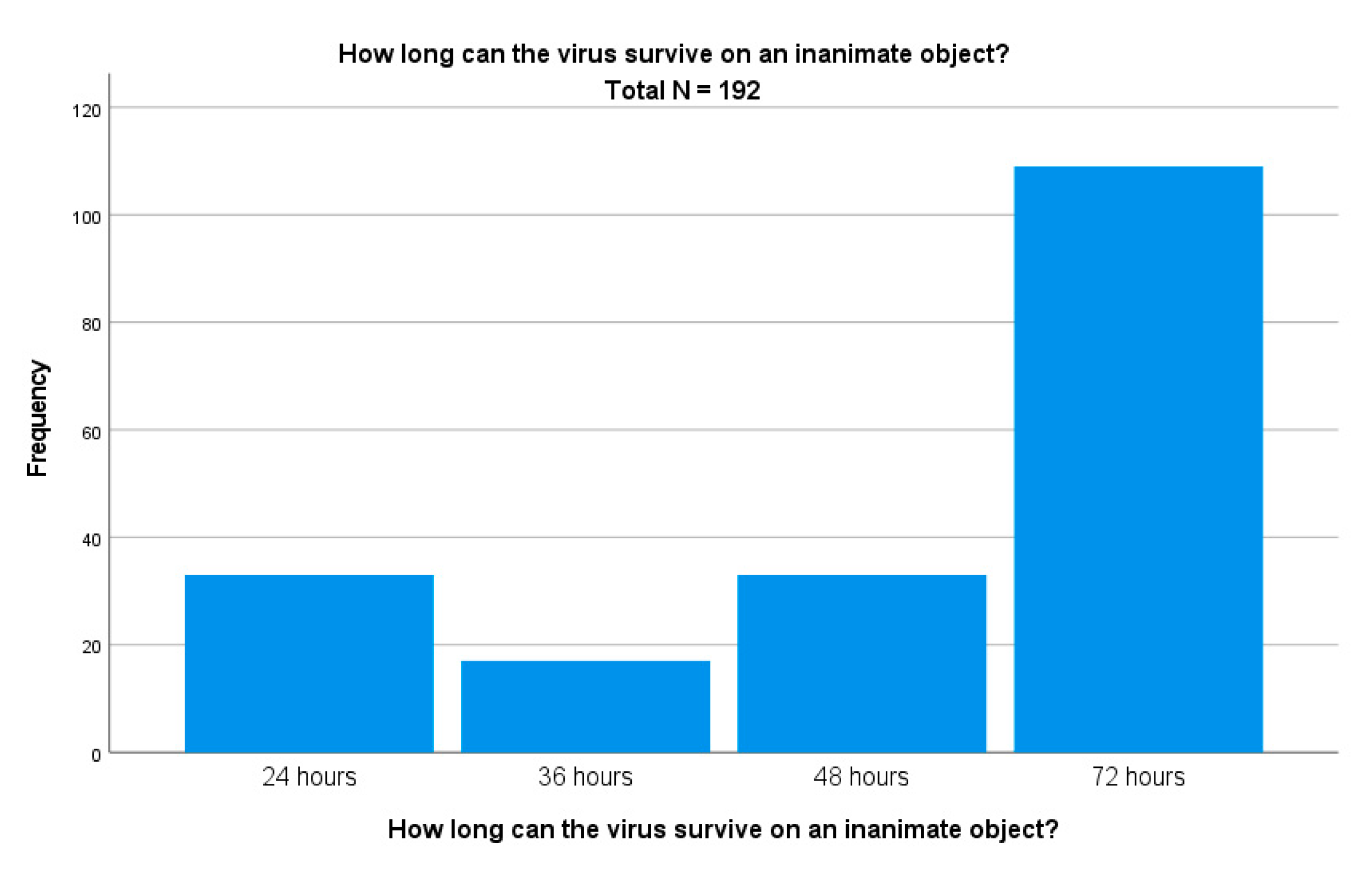
5. Knowledge, Awareness and Attitude Regarding COVID-19
6. Discussion
- Implement a pre-appointment screening process via text, telephone, or email to ensure that patients with symptoms consistent with COVID-19—or recent exposure to infected individuals—do not travel to the dental office;
- Provide and require the proper use of a face mask;
- Check patients’ temperature (<100.4 °F) with a thermometer;
- Extend time between patients, as necessary, to allow for the proper cleaning and decontamination of examination rooms;
- Have preparation strategies for the physical office and staff to prepare the environment and familiarize the staff with new policies and procedures to reduce the risk of transmission of SARS-CoV-2;
- Staff protection strategies may include recommendations for in-office clothing (emphasizing that clinical attire should only be worn in the dental practice, and not back to staff members’ homes or other community settings);
- Limit the number of patients in the waiting room simultaneously, as part of social distancing.
- The Mental Dental Facebook group;
- A confidential helpline;
- The Dentists’ Health Support Trust, providing specialized mental health services;
- Counselling for mental health and wellbeing support.
7. Limitations
8. Conclusions
- Awareness was consistent regarding preventative measures, routes of transmission and the incubation period for the SARS-CoV-2 virus;
- A lot of variation in responses existed in regard to the survivability of the virus and methods to prevent transmission;
- More female dentists felt anxious and fearful during the pandemic;
- Campaigns and seminars are required to educate dental professionals on COVID-19;
- Rehabilitation services and courses should be offered to allow dentists to function in their clinics in Trinidad and Tobago.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Ge, Z.Y.; Yang, L.M.; Xia, J.J.; Fu, X.H.; Zhang, Y.Z. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J. Zhejiang Univ. Sci. B 2020, 21, 361–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charan, R. T&T Confirms First Case of Coronavirus. Trinidad Express. 2020. Available online: https://trinidadexpress.com/newsextra/t-t-confirms-first-case-of-coronavirus/article_5c05b35a-6495-11ea-8bd4-1bba999d27a3.html (accessed on 19 August 2021).
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Lu, C.W.; Liu, X.F.; Jia, Z.F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet 2020, 395, e39. [Google Scholar] [CrossRef] [Green Version]
- Kampf, G.; Todt, D.; Pfaender, S.; Steinmann, E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020, 104, 246–251. [Google Scholar] [CrossRef] [Green Version]
- Chen, J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect. 2020, 22, 69–71. [Google Scholar] [CrossRef]
- Harrel, S.K.; Molinari, J. Aerosols and splatter in dentistry: A brief review of the literature and infection control implications. J. Am. Dent. Assoc. 2004, 135, 429–437. [Google Scholar] [CrossRef]
- Cleveland, J.L.; Gray, S.K.; Harte, J.A.; Robison, V.A.; Moorman, A.C.; Gooch, B.F. Transmission of blood-borne pathogens in US dental health care settings: 2016 update. J. Am. Dent. Assoc. 2016, 147, 729–738. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Wei, Q.; Alvarez, X.; Wang, H.; Du, Y.; Zhu, H.; Jiang, H.; Zhou, J.; Lam, P.; Zhang, L.; et al. Epithelial cells lining salivary gland ducts are early target cells of severe acute respiratory syndrome coronavirus infection in the upper respiratory tracts of rhesus macaques. J. Virol. 2011, 85, 4025–4030. [Google Scholar] [CrossRef] [Green Version]
- To, K.K.; Tsang, O.T.; Yip, C.C.; Chan, K.H.; Wu, T.C.; Chan, J.M.; Leung, W.S.; Chik, T.S.; Choi, C.Y.; Kandamby, D.H.; et al. Consistent Detection of 2019 Novel Coronavirus in Saliva. Clin. Infect. Dis. 2020, 71, 841–843. [Google Scholar] [CrossRef] [Green Version]
- Barabari, P.; Moharamzadeh, K. Novel Coronavirus (COVID-19) and Dentistry-A Comprehensive Review of Literature. Dent. J. 2020, 8, 53. [Google Scholar] [CrossRef]
- Setti, L.; Passarini, F.; De Gennaro, G.; Barbieri, P.; Perrone, M.G.; Borelli, M.; Palmisani, J.; Di Gilio, A.; Piscitelli, P.; Miani, A. Airborne Transmission Route of COVID-19: Why 2 Meters/6 Feet of Inter-Personal Distance Could Not Be Enough. Int. J. Environ. Res. Public Health 2020, 17, 2932. [Google Scholar] [CrossRef] [Green Version]
- Ng, M.-Y.; Lee, E.Y.P.; Yang, J.; Yang, F.; Li, X.; Wang, H.; Lui, M.M.-S.; Lo, C.S.-Y.; Leung, B.; Khong, P.-L.; et al. Imaging Profile of the COVID-19 Infection: Radiologic Findings and Literature Review. Radiol. Cardiothorac. Imaging 2020, 2, e200034. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.; Lau, E.H.; Wong, J.Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Khader, Y.; Al Nsour, M.; Al-Batayneh, O.B.; Saadeh, R.; Bashier, H.; Alfaqih, M.; Al-Azzam, S.; AlShurman, B.A. Dentists’ Awareness, Perception, and Attitude Regarding COVID-19 and Infection Control: Cross-Sectional Study among Jordanian Dentists. JMIR Public Health Surveill. 2020, 6, e18798. [Google Scholar] [CrossRef] [PubMed]
- Kanaparthi, A.; Dukkireddy, D.; Gopalaiah, H.; Kesary, S.; Katne, T.; Gantala, R. Awareness of COVID-19 pandemic among dental practioners of Telangana state, India: A cross sectona survey. J. Oral Biol. Craniofacial Res. 2020, 10, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Rothe, C.; Schunk, M.; Sothmann, P.; Bretzel, G.; Froeschl, G.; Wallrauch, C.; Zimmer, T.; Thiel, V.; Janke, C.; Guggemos, W.; et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N. Engl. J. Med. 2020, 382, 970–971. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolifarhood, G.; Aghaali, M.; Mozafar Saadati, H.; Taherpour, N.; Rahimi, S.; Izadi, N.; Hashemi Nazari, S.S. Epidemiological and Clinical Aspects of COVID-19; A Narrative Review. Arch. Acad. Emerg. Med. 2020, 8, e41. [Google Scholar]
- Wolf, T.G.; Zeyer, O.; Campus, G. COVID-19 in Switzerland and Liechtenstein: A Cross-Sectional Survey among Dentists’ Awareness, Protective Measures and Economic Effects. Int. J. Environ. Res. Public Health 2020, 17, 9051. [Google Scholar] [CrossRef]
- Tysiąc-Miśta, M.; Dziedzic, A. The Attitudes and Professional Approaches of Dental Practitioners during the COVID-19 Outbreak in Poland: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 4703. [Google Scholar] [CrossRef]
- Guo, H.; Zhou, Y.; Liu, X.; Tan, J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J. Dent. Sci. 2020, 15, 564–567. [Google Scholar] [CrossRef]
- Duruk, G.; Gümüşboğa, Z.Ş.; Çolak, C. Investigation of Turkish dentists clinical attitudes and behaviors towards the COVID-19 pandemic: A survey study. Braz. Oral Res. 2020, 34, e054. [Google Scholar] [CrossRef]
- Wax, R.S.; Christian, M.D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can. J. Anaesth 2020, 67, 568–576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Candeiro, G.T.; Neri, J.R.; de Carvalho, B.M.; Feijão, C.P.; Avelar, R.L.; Lemos, J.V.; Vieira-Meyer, A.P. Repercussions of COVID-19 in Brazilian Dentists’ Personal and Professional Routines: An Online Survey. J. Contemp. Dent. Pract. 2021, 22, 491–500. [Google Scholar] [CrossRef]
- Putrino, A.; Raso, M.; Magazzino, C.; Galluccio, G. Coronavirus (COVID-19) in Italy: Knowledge, management of patients and clinical experience of Italian dentists during the spread of contagion. BMC Oral Health 2020, 20, 200. [Google Scholar] [CrossRef] [PubMed]
- Škrlec, I.; Talapko, J.; Pustijanac, E.; Meštrović, T. Depression, Anxiety, Stress and Physical Activity in Health-Related University Students during COVID-19. Proceedings 2021. Available online: https://sciforum.net/manuscripts/9028/manuscript.pdf (accessed on 19 August 2021).
- Seneviratne, C.J.; Lau, M.W.J.; Goh, B.T. The Role of Dentists in COVID-19 Is Beyond Dentistry: Voluntary Medical Engagements and Future Preparedness. Front. Med. 2020, 7, 566. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Guidance for Dental Settings. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html (accessed on 19 August 2021).
- Service, N.H. COVID-19 Guidance and Standard Operating Procedure. Available online: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/06/C0581-covid-19-urgent-dental-care-sop-update-16-june-20-.pdf (accessed on 19 August 2021).
- Ahmadi, H.; Ebrahimi, A.; Ghorbani, F. The impact of COVID-19 pandemic on dental practice in Iran: A questionnaire-based report. BMC Oral Health 2020, 20, 354. [Google Scholar] [CrossRef]
- Renzaho, A.M.; de Silva-Sanigorski, A. The importance of family functioning, mental health and social and emotional well-being on child oral health. Child. Care Health Dev. 2014, 40, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Vasiliou, A.; Shankardass, K.; Nisenbaum, R.; Quiñonez, C. Current stress and poor oral health. BMC Oral Health 2016, 16, 88. [Google Scholar] [CrossRef] [Green Version]
- Jampani, N.D.; Nutalapati, R.; Dontula, B.S.; Boyapati, R. Applications of teledentistry: A literature review and update. J. Int Soc. Prev. Community Dent. 2011, 1, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Sikka, N.; Willis, J.; Fitall, E.; Hall, K.K.; Gale, B. Telehealth and Patient Safety During the COVID-19 Response. 14 March 2020. Available online: https://psnet.ahrq.gov/perspective/telehealth-and-patient-safety-during-covid-19-response (accessed on 6 October 2020).
- Ebrahimi, A.; Ebrahimi, S.; Ashkani Esfahani, S. How COVID-19 pandemic can lead to promotion of remote medical education and democratization of education? J. Adv. Med. Educ Prof. 2020, 8, 144–145. [Google Scholar] [CrossRef] [PubMed]
- Collin, V.; Toon, M.; O’Selmo, E.; Reynolds, L.; Whitehead, P. A survey of stress, burnout and well-being in UK dentists. Br. Dent. J. 2019, 226, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Checchi, V.; Bellini, P.; Bencivenni, D.; Consolo, U. COVID-19 Dentistry-Related Aspects: A Literature Overview. Int. Dent. J. 2021, 71, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Westgarth, D. Dentistry, COVID-19 and stress: Seeking light at the end of the tunnel. BDJ Pract. 2021, 34, 10–14. [Google Scholar] [CrossRef]

| Variable | n = 192 | Percent % |
|---|---|---|
| Age (years) | ||
| 20–29 | 31 | 16.1 |
| 30–39 | 78 | 40.6 |
| 40–49 | 39 | 20.3 |
| 50–59 | 33 | 17.2 |
| 60+ | 11 | 5.7 |
| Gender | ||
| Male | 89 | 46.4 |
| Female | 103 | 53.6 |
| Where did you complete your undergraduate degree? | ||
| University of the West Indies | 165 | 85.9 |
| University located in U.K. | 15 | 7.8 |
| University located in USA | 6 | 3.1 |
| Other | 6 | 3.1 |
| Sector employed in | ||
| Private | 159 | 82.8 |
| Public | 5 | 2.6 |
| Both | 28 | 14.6 |
| How long have you been in dental practice (years)? | ||
| 1–5 | 48 | 25 |
| 6–10 | 33 | 17.2 |
| 11–20 | 56 | 29.2 |
| 20+ | 55 | 28.6 |
| In which region do you work? | ||
| North Trinidad | 46 | 18.5 |
| South Trinidad | 74 | 29.7 |
| Central Trinidad | 61 | 24.5 |
| West Trinidad | 23 | 9.2 |
| East Trinidad | 40 | 16.1 |
| Tobago | 5 | 2 |
| Did you specialize? | ||
| No (General dentist) | 155 | 80.7 |
| Yes (Specialist) | 37 | 19.3 |
| Variable | Dentist (n = 155) | Specialist (n = 37) | Total (n = 192) | p |
|---|---|---|---|---|
| Q.3. Most common symptoms of COVID-19 virus infection | ||||
| Fever | 144 (92.9%) | 31 (83.8%) | 175 (91.1%) | 0.022 |
| Dry cough | 124 (80%) | 29 (78.4%) | 153 (79.7%) | 0.439 |
| Conjunctivitis | 10 (6.5%) | 1 (2.7%) | 11 (5.7%) | 0.871 |
| Rash on skin | 6 (3.9%) | 3 (8.1%) | 9 (4.7%) | 0.157 |
| Sneezing | 32 (20.6%) | 4 (10.8%) | 36 (18.8%) | 0.878 |
| Sore throat | 88 (56.8%) | 17 (45.9%) | 105 (54.7%) | 0.341 |
| Tiredness | 107 (69%) | 21 (56.8%) | 128 (66.7%) | 0.397 |
| Q.4. What are the routes of transmission for COVID-19 infection? | ||||
| Food | 7 (4.5%) | 2 (5.4%) | 9 (4.7%) | 0.510 |
| Sexual Transmission | 10 (6.45%) | 3 (8.1%) | 13 (6.8%) | 0.404 |
| Airborne | 107 (69%) | 23 (62.1%) | 130 (67.7%) | 0.36 |
| Surface contact | 126 (81.3%) | 29 (78.4%) | 158 (82.3%) | 0.783 |
| Blood | 23 (14.8%) | 5 (13.5%) | 28 (14.6%) | 0.627 |
| Q.5 What are the preventative measures associated with COVID-19 transmission? | ||||
| Water as a disinfectant | 5 (3.22%) | 2 (5.4%) | 7 (3.6%) | 0.274 |
| Aerosols | 40 (25.8%) | 13 (35.1%) | 53 (27.6%) | 0.289 |
| Exposure to sunlight | 37 (23.9%) | 9 (24.3%) | 46 (24.0%) | 0.547 |
| Gargling saltwater | 4 (2.6%) | 2 (5.4%) | 6 (3.1%) | 0.177 |
| Alcohol consumption | 1 (0.6%) | 1 (2.7%) | 2 (1.0%) | 0.231 |
| Inhaling disinfectant | 0 | 1 (2.7%) | 1 (0.5%) | 0.120 |
| Q.6 Is your dental practice treating all cases or only emergency cases at the moment | ||||
| All cases | 151 | 35 | 186 (96.9%) | 0.11 |
| Emergency only | 4 | 2 | 6 (3.1%) | 0.846 |
| Variable | Male (n = 89) | Female (n = 103) | Total (n = 192) | p | |
|---|---|---|---|---|---|
| Q.7 Do you think the preventative measures implemented are effective? | Yes | 84 (46.7%) | 96 (53.3%) | 180 (93.8%) | 0.552 |
| No | 7 (58.3%) | 5 (41.7%) | 12 (6.3%) | ||
| Q.8 Did you suspend your practice at any time during the COVID-19 outbreak? | Yes | 52 (39.1%) | 81 (60.9%) | 133 (69.3%) | 0.020 |
| No | 37 (62.7%) | 22 (37.3%) | 59 (30.7%) | ||
| Q.9 Has the number of aerosol-generating procedures been reduced since the onset of the pandemic at your dental practice? | Yes | 37 (43%) | 49 (57%) | 86 (44.8%) | 0.404 |
| No | 52 (49.1%) | 54 (50.9%) | 106 (55.2%) | ||
| Q.10 Is there enough PPE and disinfectant supplies available? | Yes | 61 (46.6%) | 70 (53.4%) | 131 (68.2%) | 0.932 |
| No | 28 (45.9%) | 33 (54.1%) | 61 (31.8%) | ||
| Q.11 Select the options which describe how you felt working during the pandemic. | |||||
| Feeling fearful | Yes | 5 (20.8%) | 19 (79.2%) | 24 (12.5%) | 0.008 |
| No | 84 (50%) | 84 (50%) | 168 (87.5%) | ||
| Willing to help | Yes | 35 (39.3%) | 27 (43.5%) | 62 (32.3%) | 0.064 |
| No | 54 (60.1%) | 76 (58.5%) | 130 (67.7%) | ||
| Feeling indifferent | Yes | 15 (71.4%) | 6 (28.6%) | 21 (10.9%) | 0.015 |
| No | 74 (43.3%) | 97 (56.7%) | 171 (89.1%) | ||
| Feeling anxious | Yes | 33 (33.3%) | 66 (66.7%) | 99 (51.6%) | <0.001 |
| No | 56 (60.2%) | 37 (39.8%) | 93 (48.4%) | ||
| Feeling prepared | Yes | 53 (58.9%) | 37 (41.1%) | 90 (46.9%) | 0.001 |
| No | 36 (35.3%) | 66 (64.7%) | 102 (53.1%) | ||
| Feeling reluctant | Yes | 5 (20.8%) | 19 (79.2%) | 24 (12.5%) | 0.007 |
| No | 84 (50%) | 84 (50%) | 168 (87.5%) | ||
| Q.12 How do you feel about the protocols being implemented? | |||||
| They aid in the control of the spread of the virus | Yes | 80 (47.1%) | 90 (52.9%) | 170 (88.5%) | 0.586 |
| No | 9 (40.9%) | 13 (59.1%) | 22 (11.5%) | ||
| Not enough is being done | Yes | 13 (59.1%) | 9 (40.9%) | 22 (11.5%) | 0.654 |
| No | 76 (44.7%) | 94 (55.3%) | 170 (88.5%) | ||
| Q.13 What are you most worried about? | |||||
| Patient safety | Yes | 51 (47.2%) | 57 (52.8%) | 108 (56.2%) | 0.784 |
| No | 38 (45.2%) | 46 (54.8%) | 84 (43.8%) | ||
| Family safety | Yes | 67 (45.3%) | 81 (54.7%) | 148 (77.1%) | 0.581 |
| No | 22 (50%) | 22 (50%) | 44 (22.9%) | ||
| Personal safety | Yes | 55 (47.8%) | 60 (52.1%) | 115 (59.9%) | 0.617 |
| No | 34 (44.1%) | 43 (55.8%) | 77 (40.1%) | ||
| Employment and income | Yes | 38 (46.9%) | 43 (53.1%) | 81 (42.2%) | 0.894 |
| No | 51 (45.9%) | 60 (54.1%) | 111 (57.8%) | ||
| Nothing | Yes | 8 (100%) | 0 | 8 (4.2%) | 0.002 |
| No | 81 (44%) | 103 (56%) | 184 (95.8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoyte, T.; Kowlessar, A.; Mahabir, A.; Khemkaran, K.; Jagroo, P.; Jahoor, S. The Knowledge, Awareness, and Attitude Regarding COVID-19 among Trinidad and Tobago Dentists. A Cross-Sectional Survey. Oral 2021, 1, 250-260. https://doi.org/10.3390/oral1030024
Hoyte T, Kowlessar A, Mahabir A, Khemkaran K, Jagroo P, Jahoor S. The Knowledge, Awareness, and Attitude Regarding COVID-19 among Trinidad and Tobago Dentists. A Cross-Sectional Survey. Oral. 2021; 1(3):250-260. https://doi.org/10.3390/oral1030024
Chicago/Turabian StyleHoyte, Trudee, Anne Kowlessar, Adilah Mahabir, Kamilia Khemkaran, Priya Jagroo, and Sadiyah Jahoor. 2021. "The Knowledge, Awareness, and Attitude Regarding COVID-19 among Trinidad and Tobago Dentists. A Cross-Sectional Survey" Oral 1, no. 3: 250-260. https://doi.org/10.3390/oral1030024
APA StyleHoyte, T., Kowlessar, A., Mahabir, A., Khemkaran, K., Jagroo, P., & Jahoor, S. (2021). The Knowledge, Awareness, and Attitude Regarding COVID-19 among Trinidad and Tobago Dentists. A Cross-Sectional Survey. Oral, 1(3), 250-260. https://doi.org/10.3390/oral1030024






