Mechanical Assessment of Glass Ionomer Cements Incorporated with Multi-Walled Carbon Nanotubes for Dental Applications
Abstract
:1. Introduction
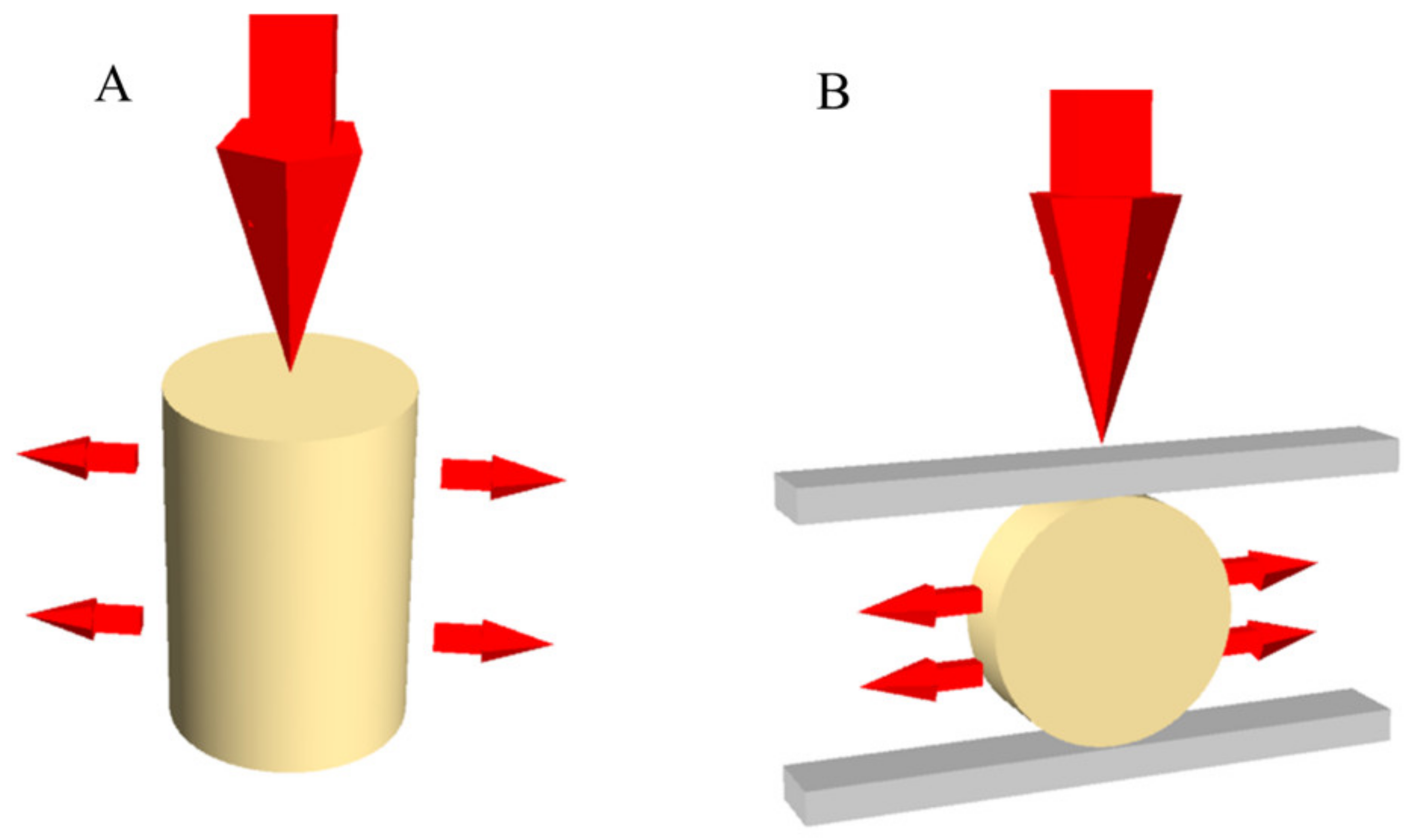
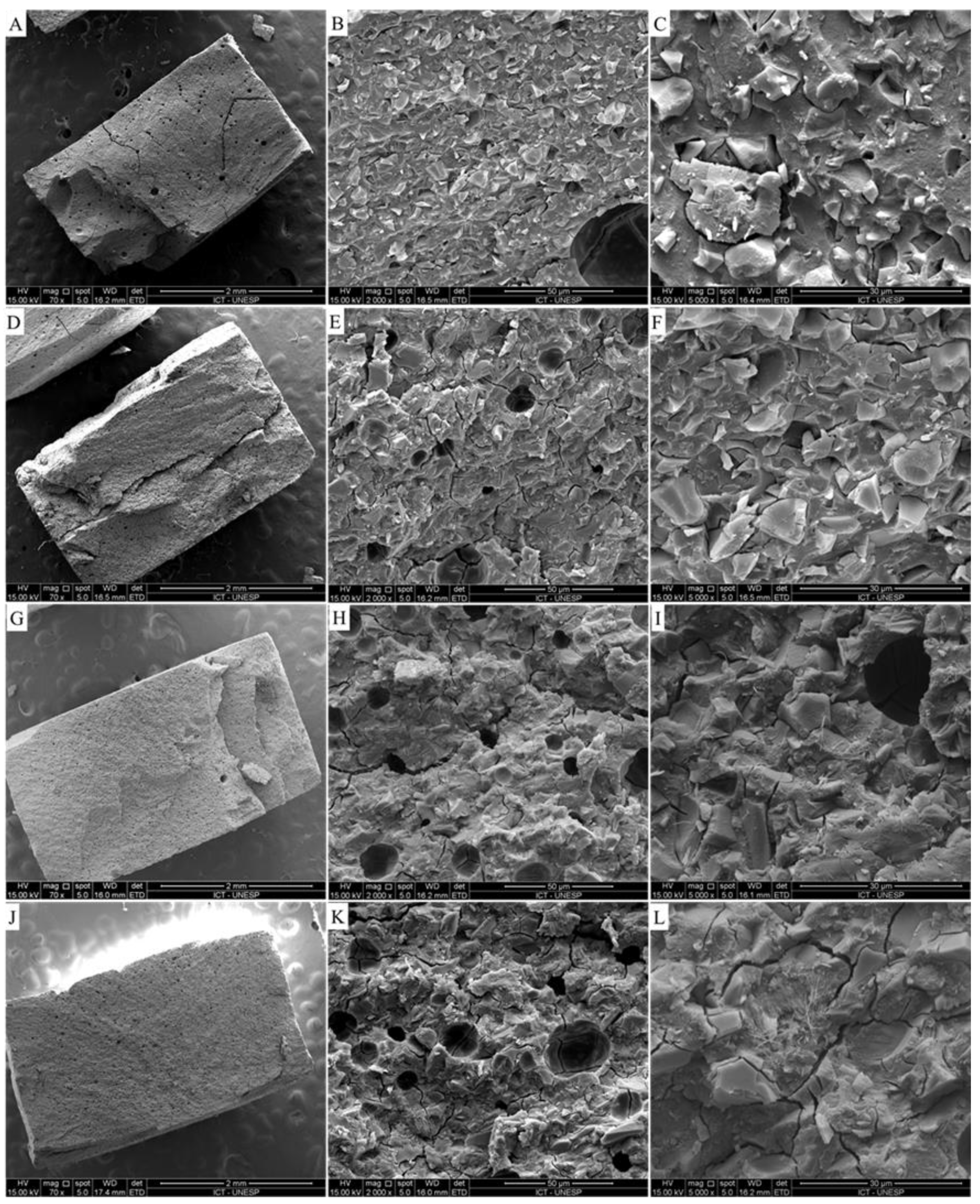
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Frencken, J.E. Atraumatic restorative treatment and minimal intervention dentistry. Br. Dent. J. 2017, 223, 183–189. [Google Scholar] [CrossRef]
- AAPD. Guideline on restorative dentistry. Pediatr. Dent. 2016, 38, 250–262. [Google Scholar]
- Da Mata, C.; McKenna, G.; Anweigi, L.; Hayes, M.; Cronin, M.; Woods, N.; O’Mahony, D.; Allen, P.F. An RCT of atraumatic restorative treatment for older adults: 5 year results. J. Dent. 2019, 83, 95–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baghdadi, Z.D.; Muhajarine, N. Effects of dental rehabilitation under general anesthesia on children’s oral-health-related quality of life: Saudi Arabian parents’ perspectives. Dent. J. 2015, 3, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Baghdadi, Z.D.; Jbara, S.; Muhajarine, N. Children’s drawing as a projective measure to understand their experiences of dental treatment under general anesthesia. Children 2020, 7, 73. [Google Scholar] [CrossRef] [PubMed]
- Moura, M.S.; Sousa, G.P.; Brito, M.H.S.F.; Silva, M.C.C.; Lima, M.D.M.; Moura, L.F.A.D.; Lima, C.C.B. Does low-cost GIC have the same survival rate as high-viscosity GIC in atraumatic restorative treatments? A RCT. Braz. Oral Res. 2020, 24, 125, Erratum in: Braz. Oral Res. 2020, 34, e125err. [Google Scholar] [CrossRef] [Green Version]
- Alves, L.M.M.; Contreras, L.P.C.; Tribst, J.P.M.; de Melo, R.M.; Borges, A.L.S. Modified technique of porcelain laminate veneer in premolars with abfraction lesions: Three-dimensional finite element analysis (FEA). J. Health Sci. 2020, 22, 120–126. [Google Scholar] [CrossRef]
- Scholtanus, J.D.; Huysmans, M.C. Clinical failure of class-II restorations of a highly viscous glass- ionomer material over a 6-year period: A retrospective study. J. Dent. 2007, 35, 156–162. [Google Scholar] [CrossRef]
- Caneppele, T.M.F.; de Souza, L.G.; Spinola, M.D.S.; de Oliveira, F.E.; de Oliveira, L.D.; Carvalho, C.A.T.; Bresciani, E. Bacterial levels and amount of endotoxins in carious dentin within reversible pulpitis scenarios. Clin. Oral Investig. 2020. [Google Scholar] [CrossRef]
- Sarkar, N.K. Metal-matrix interface in reinforced glass ionomers. Dent. Mater. 1999, 15, 421–425. [Google Scholar] [CrossRef]
- Kheur, M.; Kantharia, N.; Lakha, T.; Kheur, S.; Al-Haj Husain, N.; Özcan, M. Evaluation of mechanical and adhesion properties of glass ionomer cement incorporating nano-sized hydroxyapatite particles. Odontology 2020, 108, 66–73. [Google Scholar] [CrossRef]
- Meneses, I.H.C.; Sampaio, G.A.M.; Carvalho, F.G.; Carlo, H.L.; Münchow, E.A.; Pithon, M.M.; Alves, P.M.; Lacerda-Santos, R. In vivo biocompatibility, mechanical, and antibacterial properties of cements modified with propolis in different concentrations. Eur. J. Dent. 2020, 14, 77–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, F.; Xia, Y.; Xu, L.; Gu, N. Surface modification and microstructure of single-walled carbon nanotubes for dental resin-based composites. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 86, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Borges, A.L.S.; Tribst, J.P.M.; Dal Piva, A.M.O.; Souza, A.C.O. In vitro evaluation of multi-walled carbon nanotube reinforced nanofibers composites for dental application. Int. J. Polym. Mater. 2020, 69, 1015–1022. [Google Scholar] [CrossRef]
- Popov, A.M.; Lozovik, Y.E.; Fiorito, S.; Yahia, L. Biocompatibility and applications of carbon nanotubes in medical nanorobots. Int. J. Nanomed. 2007, 2, 361–372. [Google Scholar]
- Kechagioglou, E.; Andriotis, P.; Papagerakis, S. Multiwalled carbon nanotubes for dental applications. In Odontogenesis; Humana Press: New York, NY, USA, 2019; pp. 121–128. [Google Scholar]
- Sun, L.; Yan, Z.; Duan, Y.; Zhang, J.; Liu, B. Improvement of the mechanical, tribological and antibacterial properties of glass ionomer cements by fluorinated graphene. Dent. Mater. 2018, 34, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Pani, S.C.; Aljammaz, M.T.; Alrugi, A.M.; Aljumaah, A.M.; Alkahtani, Y.M.; AlKhuraif, A. Color stability of glass ionomer cement after reinforced with two different nanoparticles. Int. J. Dent. 2020, 31, 7808535. [Google Scholar] [CrossRef]
- Tonelli, F.M.P.; Lacerda, S.M.S.N.; Silva, M.A.; Avila, E.S.; Ladeira, L.O.; Franca, L.R.; Resende, R.R. Gene delivery to Nile tilapia spermatogonial stem cells using carboxi-functionalized multiwall carbon nanotubes. RSC Adv. 2014, 4, 37985–37987. [Google Scholar] [CrossRef]
- Chung, K.H. The properties of metal-reinforced glass ionomer materials. J. Oral Rehabil. 1993, 20, 79–87. [Google Scholar] [CrossRef]
- Fareed, M.A.; Stamboulis, A. Nanoclay addition to a conventional glass ionomer cements: Influence on physical properties. Eur. J. Dent. 2014, 8, 456–463. [Google Scholar] [CrossRef]
- Bresciani, E.; de Barata, T.J.; Fagundes, T.C.; Adachi, A.; Terrin, M.M.; Navarro, M.F. Compressive and diametral tensile strength of glass ionomer cements. J. Appl. Oral Sci. 2004, 12, 344–348. [Google Scholar] [CrossRef]
- Rohr, N.; Fischer, J. Effect of aging and curing mode on the compressive and indirect tensile strength of resin composite cements. Head Face Med. 2017, 13, 22. [Google Scholar] [CrossRef] [Green Version]
- Garoushi, S.; Vallittu, P.; Lassila, L. Hollow glass fibers in reinforcing glass ionomer cements. Dent. Mater. 2017, 33, 86–93. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.O.; de Jager, N.; Bottino, M.A.; de Kok, P.; Kleverlaan, C.J. Full-crown versus endocrown approach: A 3d-analysis of both restorations and the effect of ferrule and restoration material. J. Prosthodont. 2020, 28. [Google Scholar] [CrossRef]
- Ausiello, P.P.; Ciaramella, S.; Lanzotti, A.; Ventre, M.; Borges, A.L.; Tribst, J.P.; Dal Piva, A.; Garcia-Godoy, F. Mechanical behavior of Class I cavities restored by different material combinations under loading and polymerization shrinkage stress. A 3D-FEA study. Am. J. Dent. 2019, 32, 55–60. [Google Scholar]
- Ausiello, P.; Ciaramella, S.; De Benedictis, A.; Lanzotti, A.; Tribst, J.P.M.; Watts, D.C. The use of different adhesive filling material and mass combinations to restore class II cavities under loading and shrinkage effects: A 3D-FEA. Comput. Methods Biomech. Biomed. Eng. 2020, 22, 1–11. [Google Scholar]
- Da Rocha, D.M.; Tribst, J.P.; Ausiello, P.; Piva, A.M.D.O.D.; Da Rocha, M.C.; Di Nicoló, R.; Borges, A.L.S. Effect of the restorative technique on load-bearing capacity, cusp deflection, and stress distribution of endodontically-treated premolars with MOD restoration. Restor. Dent. Endod. 2019, 44, e33. [Google Scholar] [CrossRef]
- Baghdadi, I.; Zaazou, A.; Tarboush, B.A.; Zakhour, M.; Özcan, M.; Salameh, Z. Physiochemical properties of a bioceramic-based root canal sealer reinforced with multi-walled carbon nanotubes, titanium carbide and boron nitride biomaterials. J. Mech. Behav. Biomed. Mater. 2020, 110, 103892. [Google Scholar] [CrossRef]
- Pratap, B.; Gupta, R.K.; Bhardwaj, B.; Nag, M. Evaluation of compressive strength and void content of resin based dental composites. Mater. Today 2020. [Google Scholar] [CrossRef]
- Sidhu, S.K.; Nicholson, J.W. A Review of Glass-Ionomer Cements for Clinical Dentistry. J. Funct. Biomater. 2016, 7, 16. [Google Scholar] [CrossRef]
- Cascos-Sanchez, R.; Molinero-Mourelle, P.; Ortega, R.; Agustin-Panadero, R.; Del Rio Highsmith, J.; Gomez-Polo, M. Comparative in vitro study of the bond strength of composite to carbon fiber versus ceramic to cobalt–chromium alloys frameworks for fixed dental prostheses. Materials 2020, 13, 3173. [Google Scholar] [CrossRef]
- Tzounis, L.; Petousis, M.; Grammatikos, S.; Vidakis, N. 3D Printed thermoelectric polyurethane/multiwalled carbon nanotube nanocomposites: A novel approach towards the fabrication of flexible and stretchable organic thermoelectrics. Materials 2020, 13, 2879. [Google Scholar] [CrossRef]
- Chieruzzi, M.; Pagano, S.; Lombardo, G.; Marinucci, L.; Kenny, J.M.; Torre, L.; Cianetti, S. Effect of nanohydroxyapatite, antibiotic, and mucosal defensive agent on the mechanical and thermal properties of glass ionomer cements for special needs patients. J. Mater. Res. 2018, 33, 638–649. [Google Scholar] [CrossRef]
- Yeo, H.W.; Loo, M.Y.; Alkhabaz, M.; Li, K.C.; Choi, J.J.E.; Barazanchi, A. Bulk-fill direct restorative materials: An in vitro assessment of their physio-mechanical properties. Oral 2021, 1, 8. [Google Scholar] [CrossRef]
- Ausiello, P.; Dal Piva, A.M.d.O.; Borges, A.L.S.; Lanzotti, A.; Zamparini, F.; Epifania, E.; Mendes Tribst, J.P. Effect of shrinking and no shrinking dentine and enamel replacing materials in posterior restoration: A 3D-FEA study. Appl. Sci. 2021, 11, 2215. [Google Scholar] [CrossRef]
| Material | Type | Average Particle Size (μm) | Composition |
|---|---|---|---|
| Aqua Ionofil Plus, Voco, Cuxhaven, Germany | Conventional glass ionomer cement restorative | 8 μm | Water, pure polyacrylic acid, tartaric acid, aluminofluorosilicate glass and pigments |
| Ionofil Molar, Voco, Cuxhaven, Germany | low-viscosity glass ionomer cement restorative | 5 μm | Water, pure polyacrylic acid, tartaric acid, aluminofluorosilicate glass and pigments |
| GIC | Incorporated MWCNTs | Compressive Strength (σc) | Tensile Strength (σt) |
|---|---|---|---|
| Conventional | no | 102.8 ± 11.9 * | 15.20 ± 2.2 *** |
| yes | 86.9 ± 14.6 ** | 21.20 ± 5.5 **** | |
| Low-viscosity | no | 101.9 ± 11.5 * | 19.03 ± 2.8 *** |
| yes | 77.0 ± 11.0 ** | 20.60 ± 4.8 **** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spinola, M.; Dal Piva, A.M.O.; Barbosa, P.U.; Torres, C.R.G.; Bresciani, E. Mechanical Assessment of Glass Ionomer Cements Incorporated with Multi-Walled Carbon Nanotubes for Dental Applications. Oral 2021, 1, 190-198. https://doi.org/10.3390/oral1030019
Spinola M, Dal Piva AMO, Barbosa PU, Torres CRG, Bresciani E. Mechanical Assessment of Glass Ionomer Cements Incorporated with Multi-Walled Carbon Nanotubes for Dental Applications. Oral. 2021; 1(3):190-198. https://doi.org/10.3390/oral1030019
Chicago/Turabian StyleSpinola, Manuela, Amanda Maria Oliveira Dal Piva, Patrícia Uchôas Barbosa, Carlos Rocha Gomes Torres, and Eduardo Bresciani. 2021. "Mechanical Assessment of Glass Ionomer Cements Incorporated with Multi-Walled Carbon Nanotubes for Dental Applications" Oral 1, no. 3: 190-198. https://doi.org/10.3390/oral1030019
APA StyleSpinola, M., Dal Piva, A. M. O., Barbosa, P. U., Torres, C. R. G., & Bresciani, E. (2021). Mechanical Assessment of Glass Ionomer Cements Incorporated with Multi-Walled Carbon Nanotubes for Dental Applications. Oral, 1(3), 190-198. https://doi.org/10.3390/oral1030019







