Effects of Buddhist Walking Meditation, Walking Meditation or Mindful Walking on the Health of Adults and Older Adults: A Systematic Review
Abstract
1. Introduction
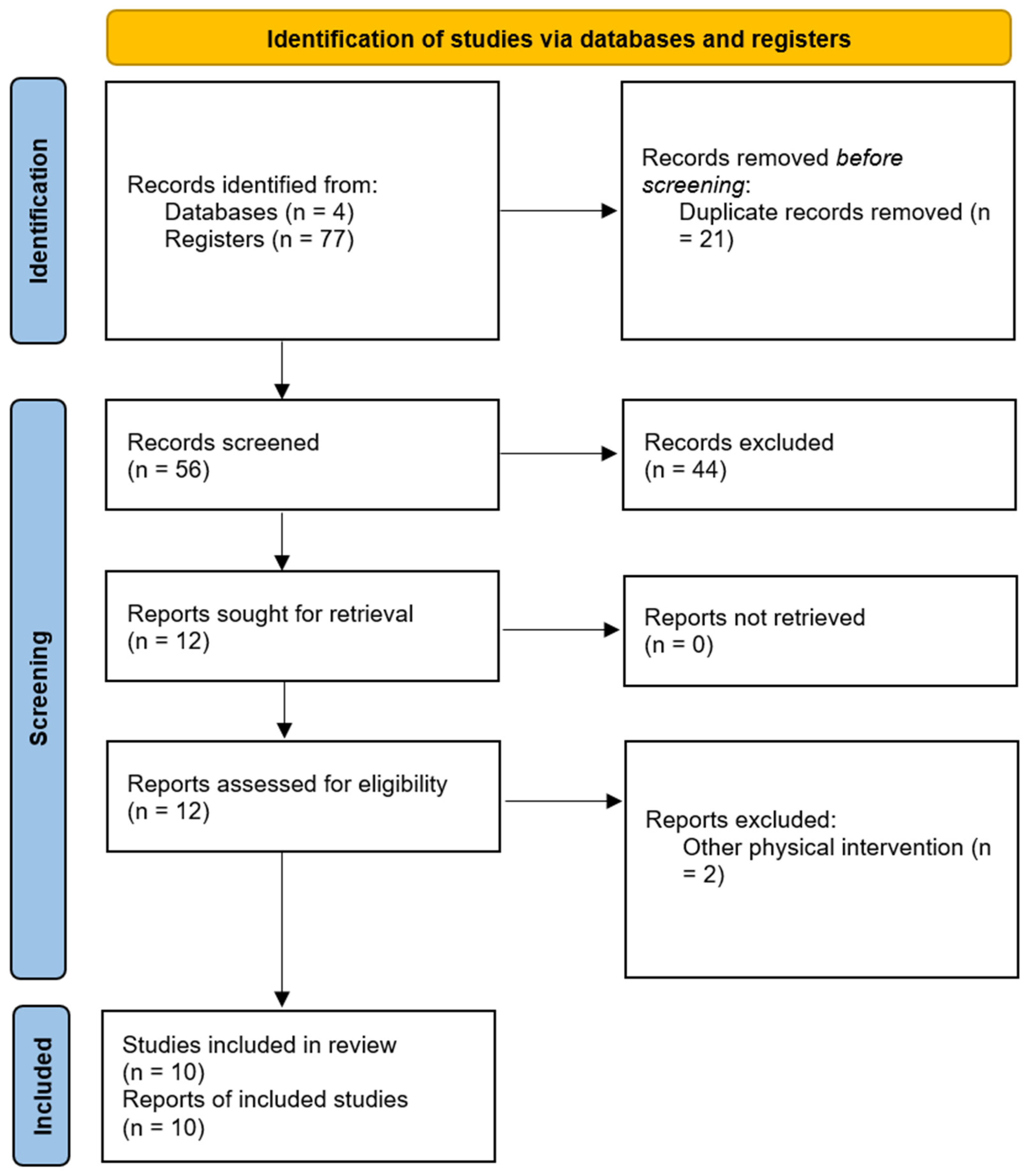
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Strategy
2.3. Selection Criteria
2.4. Selection of Studies
2.5. Data Collection
2.6. Evaluation of the Quality of the Selected Articles
3. Results
3.1. Characteristics of the Articles Included in the Review
| Author | Study Design | Groups (n) Sample Size Female (%) | Mean Age (Year) | Objective | Intervention | Duration | Data Collection Instruments | Results | Conclusions |
| Chatutain et al. [39] | RCT | 58 EG: 29 CG: 29 100% Female | 70.2 68.23 | Walking Meditation can improve ankle proprioception and balance performance among elderly women | 30 min/session–3 days/week | 8 weeks | AAE; BBS; FRT; TUG. | AAE: p = 0.001 BBS: p = 0.001 FRT: p < 0.01 TUG: p < 0.01 | Walking meditation improved ankle proprioception and balance performance. |
| Gainey et al. [40] | RCT | 23 EG (WM): 12 CG (TW): 11 83% Female | 58.0 63.0 | To investigate and compare the effects of Buddhist walking meditation and traditional walking on glycemic control and vascular function in patients with type 2 diabetes mellitus. | 30 min/session–3 days/week | 12 weeks | BMI; VO2 max; Isometric leg dynamometry; FMD; PWV; ABI; Glucose, insulin, HbA1c, lipid profile, cortisol; HOMA-IR. | FMD (TW: p < 0.05; WM: p < 0.05). Glucose: TW and WM: p < 0.05 HbA1c: WM: p < 0.05 Cortisol: WM: p < 0.05 | Walking meditation was more effective than traditional walking in reducing HbA1c (glycated hemoglobin test), blood pressure, arterial stiffness, and stress. |
| Lapanantasin et al. [41] | RCT | 32 EG (WM): 10 EG (RE): 11 CG: 11 69% Female | 19.5 19.9 19.6 | To investigate the effects of walking meditation, a mind–body practice, and compare it with resistance band exercise on ankle proprioception and balance among individuals with chronic ankle instability. | 30 min/session–3 days/week | 4 weeks | AAE; SEBT. | WM: PF5° (p = 0.007); PF10° (p = 0.040). | Increased ankle stability for the walking meditation group. |
| Prakhinkit et al. [42] | RCT | 40 EG (WM): 14 EG (TW): 13 CG (SC): 13 100% Female | 74.0 74.8 81.0 | To determine the effects of novel Buddhist-based walking meditation (BWM) and traditional walking exercise (TWE) on depression, functional fitness, and vascular reactivity. | 20 min/session–3 days/week (weeks 1–6); 30 min/session–3 days/week (weeks 7–12) | 12 weeks | Geriatric Depression Scale–Thai; HR; physical fitness (strength; flexibility; aerobic capacity); Blood analyses; FMD. | TW: BMI and blood pressure (p < 0.05). BWM: BMI, body fat, and blood pressure (p < 0.05). TW: Lowered cholesterol, triglycerides, C-reactive protein, and increased nitric oxide (p < 0.05). BWM: Lowered cholesterol, LDL cholesterol, triglycerides, C-reactive protein, and cortisol; increased nitric oxide (p < 0.05). TW: Strength, flexibility, and aerobic capacity (p < 0.05). BWM: Strength, flexibility, and aerobic capacity (p < 0.05). BWM: Improved depression levels (p < 0.05). | Buddhist walking meditation reduced depression, improved functional fitness and vascular reactivity, and appears to confer greater overall improvements than traditional walking. |
| Shi et al. [43] | RCT | 38 EG: 17 CG: 21 86.8% Female | 52.7 46.5 | To examine whether a 4-week mindful walking intervention increases physical activity and improves mental health outcomes. | 60 min/session–1 day/week | 4 weeks | Perceived Stress Scale; Mental Health Inventory-5 items; Brief Edinburgh Depression Scale; Freiburg Mindfulness Inventory; PSQI. | EG: improvement in stress (p = 0.025), improvement in depression, but not significant. | The intervention group improved in perceived stress, physical activity and depression. |
| Srisoongnern et al. [44] | RCT | 48 EG (WM): 24 CG (AE): 24 45.8% Female | 65.0 65.0 | To determine the effects of a six-week Buddhist walking meditation program on exercise capacity, quality of life, and hemodynamic response in patients with chronic heart failure. | 30–40 min/session–3 days/week | 6 weeks | Six-minute Walk test; Minnesota Living with Heart Failure Questionnaire; Hemodynamic response. | The aerobic exercise group significantly reduced their systolic pressure (p < 0.05), and the difference between groups was significant (p = 0.043). | Six weeks of walking meditation has not been shown to be effective in improving functional capacity in patients with heart failure, compared to aerobic exercise. |
| Yang et al. [45] | Preexperimental | 25 EG: 25 NO CG 84% Female | 72.4 | To establish a proof of concept for using this mindful walking program to improve short- and long-term cognition among community-dwelling older adults. | 30 min/session–2 days/week | 4 weeks | Trail Making Test; Porteus Maze Test; Stroop test; Symbol Search test; Dot Memory test; sleep test. | Significant improvement in: Trail A (p < 0.05) Trail B (p < 0.05) Maze I and II solution time (p < 0.05) Stroop test (p < 0.05). Memory and divided attention remained unchanged. | Long-term, within-person improvements in processing speed and executive function. |
| Edwards et al. [46] | RCT | 110 Walking: 22 Meditating: 22 Walking + Meditation: 22 Meditation + Walking: 22 Control: 22 73% Female | 21.5 22.6 21.2 20.7 20.9 | Examine the usefulness of a shorter walk (10 min) with meditation. | 10 min/session | 1 session | STAI-Form Y | Walk then meditation: (p < 0.05). Meditation then walk: (p < 0.05). Meditation only: (p < 0.05) CG and walking only: no significant changes. | A 10 min meditation, as well as a combination of a 10-min meditation and a 10-min brisk walk, resulted in significant reductions in state anxiety among a sample of young adults. |
| Mitarnun et al. [47] | RCT | 33 EG: 17 CG: 16 57.6% Female | 61.3 61.3 | To determine the effects of walking meditation on functional performance, disease severity, and anxiety in Parkinson’s disease. | 30 min/session–3 days/week | 12 weeks | TUG; 10 m Walk Test; Five Times Sit to Stand; UPDRS; HADS-A; Adverse event registry. | EG: improved walking speed (p < 0.01); improved UPDRS (p = 0.030); UPDRS part II (p = 0.020); improved HADS-A anxiety (p < 0.05). | Walking meditation can promote high rates of exercise adherence, reduce disease severity, and reduce the percentage of participants with anxiety. |
| Phoobangkerdphol et al. [48] | RCT | 68 EG: 35 CG: 33 85.3% Female | 68.9 68.9 | To investigate the improvement in balance skills compared to walking meditation and balance training among older adults with a history of falls. | 20–30 min/session–5–7 days/week | 24 weeks | TUG; FRT; SLST; EQ-5D-5L; TGMHA-15 | Both groups improved significantly (p < 0.05), but no significant differences were found between them. | Walking meditation is comparable to balance training in improving balance in older adults with a history of falls. |
3.2. Methodological Scale PEDro
| Authors | Criteria | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total | |
| Chatutain et al. [39] | Y | Y | N | Y | N | N | Y | Y | Y | Y | Y | 7 |
| Gainey et al. [40] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Lapanantasin et al. [41] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Prakhinkit et al. [42] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Shi et al. [43] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Srisoongnern et al. [44] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Yang et al. [45] | Y | N | N | N | N | N | N | Y | Y | Y | Y | 4 |
| Edwards et al. [46] | N | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 |
| Mitarnun et al. [47] | Y | Y | N | Y | N | N | Y | Y | Y | Y | Y | 7 |
| Phoobangkerdphol et al. [48] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
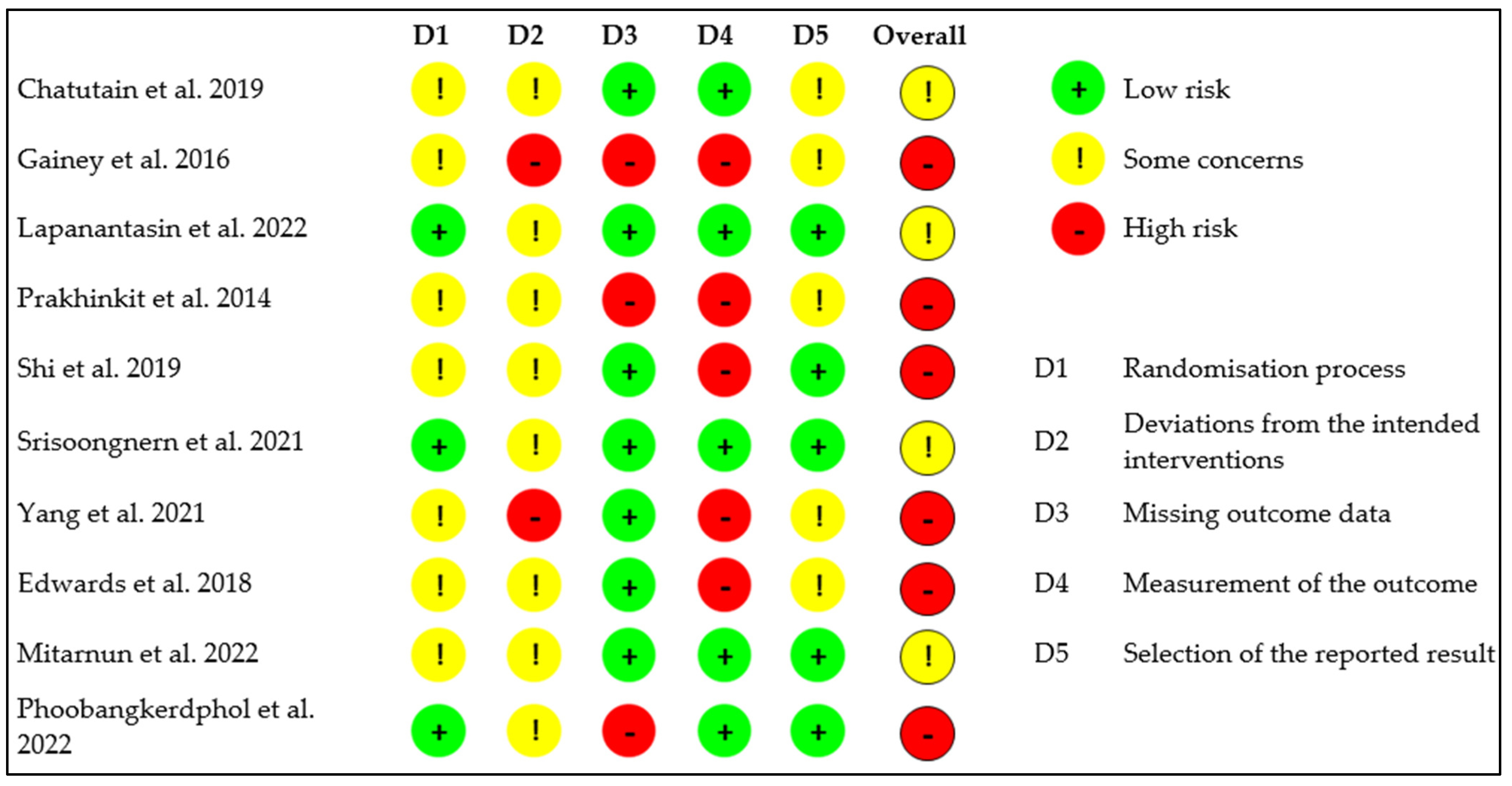
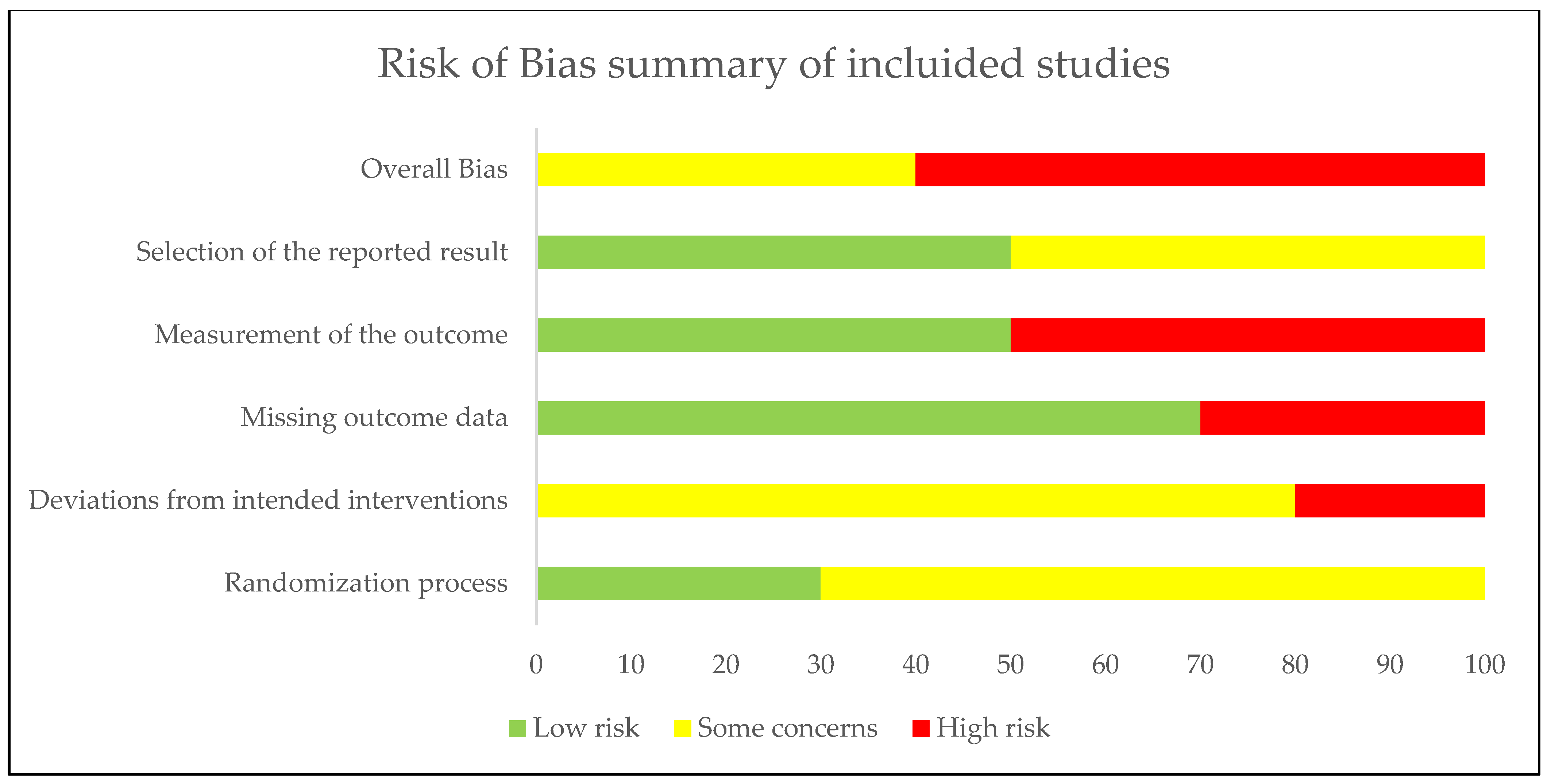
3.3. Risk of Bias
3.4. Main Results by Intervention
3.4.1. Walking Meditation
3.4.2. Buddhist Walking Meditation
3.4.3. Mindful Walking
4. Discussion
4.1. Limitations and Strengths
4.2. Future Lines of Investigation
4.3. Practical Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Piggin, J. What is physical activity? A holistic definition for teachers, researchers and policy makers. Front. Sports Act. Living 2020, 2, 72. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. J. Am. Med. Assoc. 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Díaz Fuenzalida, C.; Mendoza Morales, A.; Rodríguez Campos, H.; Valdivia Moreno, J.; Herrera-Valenzuela, T.; Guzmán-Muñoz, E.; Magnani Branco, B.; Valdés-Badilla, P. Relationship between physical activity and quality of life in youth during the COVID-19 pandemic. Rev. Cub Med. Mil. 2021, 50, e02101557. Available online: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0138-65572021000400008 (accessed on 1 December 2024).
- Montalva-Valenzuela, F.; Castillo-Paredes, A.; Farias-Valenzuela, C.; Andrades-Ramirez, O.; Concha-Cisternas, Y.; Guzmán-Muñoz, E. Effects of exercise, physical activity, and sports on physical fitness in adults with Down syndrome: A systematic review. AIMS Public Health 2024, 11, 577–600. [Google Scholar] [CrossRef]
- Sharif, K.; Watad, A.; Bragazzi, N.L.; Lichtbroun, M.; Amital, H.; Shoenfeld, Y. Physical activity and autoimmune diseases: Get moving and manage the disease. Autoimmun. Rev. 2018, 17, 53–72. [Google Scholar] [CrossRef]
- Warburton, D.E.R.; Bredin, S.S.D. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef] [PubMed]
- An, H.Y.; Chen, W.; Wang, C.W.; Yang, H.F.; Huang, W.T.; Fan, S.Y. The Relationships between Physical Activity and Life Satisfaction and Happiness among Young, Middle-Aged, and Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 4817. [Google Scholar] [CrossRef] [PubMed]
- Galloza, J.; Castillo, B.; Micheo, W. Benefits of Exercise in the Older Population. Phys. Med. Rehab Clin. N. Am. 2017, 28, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Latorre-Román, P.Á.; Martínez, A.V.N.; García-Pinillos, F. Effect of a physical activity program on sport enjoyment, physical activity participation, physical self-concept and quality of life in children with asthma. Mot. Rev. De Educ. Física 2015, 21, 386–392. [Google Scholar] [CrossRef]
- Roe, J.; Mondschein, A.; Neale, C.; Barnes, L.; Boukhechba, M.; Lopez, S. The Urban Built Environment, Walking and Mental Health Outcomes Among Older Adults: A Pilot Study. Front. Public Health 2020, 8, 575946. [Google Scholar] [CrossRef]
- Kraus, W.E.; Powell, K.E.; Haskell, W.L.; Janz, K.F.; Campbell, W.W.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L.; et al. Physical Activity, All-Cause and Cardiovascular Mortality, and Cardiovascular Disease. Med. Sci. Sports Exerc. 2019, 51, 1270–1281. [Google Scholar] [CrossRef]
- Rivera-Torres, S.; Fahey, T.D.; Rivera, M.A. Adherence to Exercise Programs in Older Adults: Informative Report. Gerontol. Geriatr. Med. 2019, 5, 2333721418823604. [Google Scholar] [CrossRef]
- Franklin, B.A.; Eijsvogels, T.M.H.; Pandey, A.; Quindry, J.; Toth, P.P. Physical activity, cardiorespiratory fitness, and cardiovascular health: A clinical practice statement of the American Society for Preventive Cardiology Part II: Physical activity, cardiorespiratory fitness, minimum and goal intensities for exercise training, prescriptive methods, and special patient populations. Am. J. Prev. Cardiol. 2022, 12, 100425. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Mahindru, A.; Patil, P.; Agrawal, V. Role of Physical Activity on Mental Health and Well-Being: A Review. Cureus. 2023, 15, e33475. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; West, D.; Pellegrini, C.; Wei, J.; Wilcox, S.; Neils-Strunjas, J.; Rudisil, C.; Friedman, D.; Marquez, D.; Dzwierzynski, J.; et al. Walking Interventions and Cognitive Health in Older Adults: A Systematic Review of Randomized Controlled Trials. Am. J. Health Promot. 2025, 39, 08901171251328858. [Google Scholar] [CrossRef] [PubMed]
- NIH. National Library of Medicine. National Center for Biotechnology Information. MeSH. Walking. Available online: https://www.ncbi.nlm.nih.gov/mesh/68016138 (accessed on 20 December 2024).
- Donath, L.; Faude, O.; Roth, R.; Zahner, L. Effects of stair-climbing on balance, gait, strength, resting heart rate, and submaximal endurance in healthy seniors. Scand. J. Med. Sci. Sports 2014, 24, e93–e101. [Google Scholar] [CrossRef]
- Battaglia, G.; Giustino, V.; Messina, G.; Faraone, M.; Brusa, J.; Bordonali, A.; Barbagallo, M.; Palma, A.; Dominguez, L.J. Walking in natural environments as geriatrician’s recommendation for fall prevention: Preliminary outcomes from the “passiata day” model. Sustainability 2020, 12, 2684. [Google Scholar] [CrossRef]
- Li, Q.; Otsuka, T.; Kobayashi, M.; Wakayama, Y.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Li, Y.; Hirata, K.; Shimizu, T.; et al. Acute effects of walking in forest environments on cardiovascular and metabolic parameters. Eur. J. Appl. Physiol. 2011, 111, 2845–2853. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Ma, X.; Wang, L.; Zhang, C.; Song, Q.; Gu, H.; Mao, D. Effects of Tai Chi Chuan and Brisk Walking Exercise on Balance Ability in Elderly Women: A Randomized Controlled Trial. Mot. Control 2019, 23, 100–114. [Google Scholar] [CrossRef] [PubMed]
- Gomeñuka, N.A.; Oliveira, H.B.; Silva, E.S.; Costa, R.R.; Kanitz, A.C.; Liedtke, G.V.; Schuch, F.B.; Peyré-Tartaruga, L.A. Effects of Nordic walking training on quality of life, balance and functional mobility in elderly: A randomized clinical trial. PLoS ONE 2019, 14, e0211472. [Google Scholar] [CrossRef]
- Branco, J.C.; Jansen, K.; Sobrinho, J.T.; Carrapatoso, S.; Spessato, B.; Carvalho, J.; Mota, J.; da Silva, R.A. Physical benefits and reduction of depressive symptoms among the elderly: Results from the Portuguese “National Walking Program”. Cienc. Saude Coletiva 2015, 20, 789–795. [Google Scholar] [CrossRef]
- Ogilvie, D.; Foster, C.E.; Rothnie, H.; Cavill, N.; Hamilton, V.; Fitzsimons, C.F.; Mutrie, N.; Scottish Physical Activity Research Collaboration. Interventions to promote walking: Systematic review. Br. Med. J. 2007, 334, 1204. [Google Scholar] [CrossRef]
- Kassavou, A.; Turner, A.; French, D.P. Do interventions to promote walking in groups increase physical activity? A meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 18. [Google Scholar] [CrossRef]
- Williams, D.M.; Matthews, C.E.; Rutt, C.; Napolitano, M.A.; Marcus, B.H. Interventions to increase walking behavior. Med. Sci. Sports Exerc. 2008, 40, S567–S573. [Google Scholar] [CrossRef]
- Irvine, K.N.; Marselle, M.R.; Melrose, A.; Warber, S.L. Group Outdoor Health Walks Using Activity Trackers: Measurement and Implementation Insight from a Mixed Methods Feasibility Study. Int. J. Environ. Res. Public Health 2020, 17, 2515. [Google Scholar] [CrossRef]
- Quintiliani, L.M.; Dedier, J.; Amezquita, M.; Sierra-Ruiz, M.; Romero, D.; Murillo, J.; Mahar, S.; Goodman, M.; Kane, J.; Cummings, D.; et al. Community Walks: A cluster randomized controlled trial of a multilevel physical activity intervention for low income public housing residents. BMC Public Health 2023, 23, 1676. [Google Scholar] [CrossRef]
- Verma, G.; Araya, R. The effect of meditation on psychological distress among Buddhist Monks and Nuns. Int. J. Psychiatry Med. 2010, 40, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Walking Meditations. Mindfulness 2017, 8, 249–250. [Google Scholar] [CrossRef]
- Van Lutterveld, R.; van Dellen, E.; Pal, P.; Yang, H.; Stam, C.J.; Brewer, J. Meditation is associated with increased brain network integration. NeuroImage 2017, 158, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Pickut, B.; Vanneste, S.; Hirsch, M.A.; Van Hecke, W.; Kerckhofs, E.; Mariën, P.; Parizel, P.M.; Crosiers, D.; Cras, P. Mindfulness Training among Individuals with Parkinson’s Disease: Neurobehavioral Effects. Park. Dis. 2015, 2015, 816404. [Google Scholar] [CrossRef]
- Page, M.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, T.; Shamseer, L.; Tetzlaff, J.; Akl, E.; Brennan, S.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Br. Med. J. 2021, 372, n71. [Google Scholar] [CrossRef]
- Santos, C.M.D.C.; Pimenta, C.A.D.M.; Nobre, M.R.C. La estrategia PICO para la construcción de la pregunta de investigación y la búsqueda de evidencias. Rev. Lat. Am. De Enferm. 2007, 15, 508–511. [Google Scholar] [CrossRef]
- Cascaes da Silva, F.; Valdivia Arancibia, B.; da Rosa Iop, R.; Barbosa Gutierres Filho, P.; da Silva, R. Escalas y listas de evaluación de la calidad de estudios científicos. Rev. Cuba. Inf. Cienc. Salud 2013, 24, 295–312. Available online: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S2307-21132013000300007&lng=es&tlng=es (accessed on 1 December 2024).
- de Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Herbert, R.; Moseley, A.; Sherrington, C.; Maher, C. Escala PEDro-Español. Cent. Evid. Based Physiother. (CEBP) 2000, 86, 55. [Google Scholar] [CrossRef]
- Jørgensen, L.; Paludan-Müller, A.S.; Laursen, D.R.; Savović, J.; Boutron, I.; Sterne, J.A.; Higgins, J.P.; Hróbjartsson, A. Evaluation of the Cochrane tool for assessing risk of bias in randomized clinical trials: Overview of published comments and analysis of user practice in Cochrane and non-Cochrane reviews. Syst. Rev. 2016, 5, 80. [Google Scholar] [CrossRef] [PubMed]
- Chatutain, A.; Pattana, J.; Parinsarum, T.; Lapanantasin, S. Walking meditation promotes ankle proprioception and balance performance among elderly women. J. Bodyw. Mov. Ther. 2019, 23, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Gainey, A.; Himathongkam, T.; Tanaka, H.; Suksom, D. Effects of Buddhist walking meditation on glycemic control and vascular function in patients with type 2 diabetes. Complement. Ther. Med. 2016, 26, 92–97. [Google Scholar] [CrossRef]
- Lapanantasin, S.; Thongloy, N.; Samsee, M.; Wonghirunsombat, N.; Nuangpulsarp, N.; Ua-Areejit, C.; Phattaraphanasakul, P. Comparative effect of walking meditation and rubber-band exercise on ankle proprioception and balance performance among persons with chronic ankle instability: A randomized controlled trial. Complementary Ther. Med. 2022, 65, 102807. [Google Scholar] [CrossRef]
- Prakhinkit, S.; Suppapitiporn, S.; Tanaka, H.; Suksom, D. Effects of Buddhism walking meditation on depression, functional fitness, and endothelium-dependent vasodilation in depressed elderly. J. Altern. Complement. Med. 2014, 20, 411–416. [Google Scholar] [CrossRef]
- Shi, L.; Welsh, R.S.; Lopes, S.; Rennert, L.; Chen, L.; Jones, K.; Zhang, L.; Crenshaw, B.; Wilson, M.; Zinzow, H. A pilot study of mindful walking training on physical activity and health outcomes among adults with inadequate activity. Complementary Ther. Med. 2019, 44, 116–122. [Google Scholar] [CrossRef]
- Srisoongnern, S.; Pajareya, K.; Sriboon, R.; Thanakiatpinyo, T.; Chirakarnjanakorn, S.; Thirapatarapong, W. Effects of Buddhist walking meditation on exercise capacity and quality of life of patients with chronic heart failure: A randomized controlled trial. Heart Lung J. Crit. Care 2021, 50, 363–368. [Google Scholar] [CrossRef]
- Yang, C.H.; Hakun, J.G.; Roque, N.; Sliwinski, M.J.; Conroy, D.E. Mindful walking and cognition in older adults: A proof of concept study using in-lab and ambulatory cognitive measures. Prev. Med. Rep. 2021, 23, 101490. [Google Scholar] [CrossRef] [PubMed]
- Edwards, M.K.; Rosenbaum, S.; Loprinzi, P.D. Differential Experimental Effects of a Short Bout of Walking, Meditation, or Combination of Walking and Meditation on State Anxiety Among Young Adults. Am. J. Health Promot. 2018, 32, 949–958. [Google Scholar] [CrossRef]
- Mitarnun, W.; Mitranun, W.; Mitarnun, W.; Pangwong, W. Home-Based Walking Meditation Decreases Disease Severity in Parkinson’s Disease: A Randomized Controlled Trial. J. Integr. Complement. Med. 2022, 28, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Phoobangkerdphol, C.; Limampai, P.; Dasri, S.; Kuptniratsaikul, V. Walking meditation versus balance training for improving balance abilities among older adults with history of fall: A randomized controlled trial. Clin. Rehabil. 2022, 36, 538–549. [Google Scholar] [CrossRef] [PubMed]
- Office for Health Improvement and Disparities (OHID). Physical Activity: Applying All Our Health. Available online: https://www.gov.uk/government/publications/physical-activity-applying-all-our-health/physical-activity-applying-all-our-health (accessed on 22 December 2022).
- Sallis, R.; Franklin, B.; Joy, L.; Ross, R.; Sabgir, D.; Stone, J. Strategies for promoting physical activity in clinical practice. Prog. Cardiovasc. Dis. 2015, 57, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Ungvari, Z.; Fazekas-Pongor, V.; Csiszar, A.; Kunutsor, S.K. The multifaceted benefits of walking for healthy aging: From Blue Zones to molecular mechanisms. GeroScience 2023, 45, 3211–3239. [Google Scholar] [CrossRef]
- Ma, J.; Lin, P.; Williams, J. Effectiveness of nature-based walking interventions in improving mental health in adults: A systematic review. Curr. Psychol. 2024, 43, 9521–9539. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montalva-Valenzuela, F.; Guzmán-Muñoz, E.; Ferrari, G.; Adsuar, J.C.; Escobar Ruiz, N.; Castillo-Paredes, A. Effects of Buddhist Walking Meditation, Walking Meditation or Mindful Walking on the Health of Adults and Older Adults: A Systematic Review. Psychiatry Int. 2025, 6, 122. https://doi.org/10.3390/psychiatryint6040122
Montalva-Valenzuela F, Guzmán-Muñoz E, Ferrari G, Adsuar JC, Escobar Ruiz N, Castillo-Paredes A. Effects of Buddhist Walking Meditation, Walking Meditation or Mindful Walking on the Health of Adults and Older Adults: A Systematic Review. Psychiatry International. 2025; 6(4):122. https://doi.org/10.3390/psychiatryint6040122
Chicago/Turabian StyleMontalva-Valenzuela, Felipe, Eduardo Guzmán-Muñoz, Gerson Ferrari, José Carmelo Adsuar, Natalia Escobar Ruiz, and Antonio Castillo-Paredes. 2025. "Effects of Buddhist Walking Meditation, Walking Meditation or Mindful Walking on the Health of Adults and Older Adults: A Systematic Review" Psychiatry International 6, no. 4: 122. https://doi.org/10.3390/psychiatryint6040122
APA StyleMontalva-Valenzuela, F., Guzmán-Muñoz, E., Ferrari, G., Adsuar, J. C., Escobar Ruiz, N., & Castillo-Paredes, A. (2025). Effects of Buddhist Walking Meditation, Walking Meditation or Mindful Walking on the Health of Adults and Older Adults: A Systematic Review. Psychiatry International, 6(4), 122. https://doi.org/10.3390/psychiatryint6040122