Abstract
Although research has shown that moral distress harms mental health in diverse populations, information on potential moderators of such associations is scarce. In a sample of sub-Saharan African nurses, we examined the link between moral distress and depressive symptoms. We explored for whom and when such relationships may hold with regard to gender, age, and work experience. Participants consisted of 398 nurses drawn from a tertiary healthcare institution in southeastern Nigeria. Data were collected using the Moral Distress Questionnaire (MDQ) for clinical nurses, and the Center for Epidemiological Studies Depression Scale Revised (CEDS-R). Hayes regression-based macro results for the moderation effects indicated that the association of high moral distress with increased depressive symptoms was robust for women but not significant for men. Although older age and higher years of nursing experience were associated with reduced symptoms of depression, nurses’ age and years of work experience did not moderate the relationship between moral distress and depressive symptoms. To promote mental well-being and preserve the integrity of nurses, gender-based differentials in how morals contribute depressive symptoms should be considered in policy and practice.
1. Introduction
Nurses are faced with stressful situations in dealing with the needs of patients and families [1,2,3,4,5] and they are potentially at risk for moral distress [6,7,8,9,10,11,12,13], even when compared to other healthcare workers (HCWs) [14,15,16,17,18,19,20,21,22,23]. Moral distress is the psychological disequilibrium and negative feeling experienced when a person makes a moral decision but does not follow through by performing it in overt behavior, or when one knows the right ethical decision to make but cannot make it due to institutional constraints [24]. The outbreak of the COVID-19 pandemic rekindled enormous interest in moral distress among HCWs, with these studies supporting its link to a marked sense of helplessness, sleep difficulty, and diminished quality of sleep [25,26,27,28,29,30,31]. The increased research interest is understandable because nurses’ primary emotional response in providing patient care during the pandemic was represented by moral distress [32]. Corley’s theory of moral distress upholds that when nurses cannot do what they think is right or make decisions based on ethical principles, they may experience moral distress, resulting in adverse mental health outcomes [24].
Depression is a common mental illness which should be made a priority area of interest [33]. Depressive disorders are more prevalent among nurses than in other HCWs [34], and it is most prevalent among nurses in Africa compared to their counterparts in other parts of the world [35]. Hence, research interest in depression among this critical healthcare workforce in Africa is worthwhile. Exposure to moral distress was associated with increased depressive symptoms among HCWs in Canada [36,37], Israel [38], Germany [21], Italy [39,40], Spain [41], United Kingdom [42], and the USA [43,44]. Conversely, a weak or null effect of moral distress on depression exists for nurses in Romania [45].
Recent systematic reviews and meta-analyses have noted the scarcity of research on moral distress and mental health outcomes in the African setting [6,10]. The paucity of research in the African setting does not advance the cross-cultural applications of theoretical postulations on moral distress and mental health. The role of culture in healthcare work and the cultural components of patient care encompasses healthcare professionals’ perceptions and uncertainties concerning patients, families, and populations, which may trigger moral distress [46,47]. Hence, there is a need for studies in non-western cultures on moral distress and psychopathology among nurses. Compared to their counterparts in developed Western societies, nurses who work in low- and middle-income countries have elevated levels of moral distress. Given that ethical workload, lack of resources, increased workload, and actions that are inconsistent with one’s moral values are notable moral stressors [10,48,49], the highly prevalent poor working conditions, excess workload, and inadequate resources in the sub-Saharan African health system [50,51,52] makes the continent a unique environment for research in this regard.
Psychosocial variables, especially social support, are widely recognized moderators of the association between moral distress and mental health outcomes [43,53,54], but socio-demographic factors may be critical factors in either attenuating or potentiating moral distress–wellbeing links. It is, therefore, essential to identify socio-demographic characteristics of nursing professionals that may mitigate the contributions of moral distress to depression. Recent studies have shown that depression among nurses was more severe for women [34,35,55], those who were younger in age [35], and nurses of lower rank [35]. However, in other studies, a higher service rank was linked to increased depression [34].
Similarly, some studies have found significant gender differences in moral distress, with a greater presence of moral distress in women [22,42,56,57,58], while other studies showed no gender differences [59,60,61]. Regarding age, younger nurses have higher risks for the harmful contributions of moral adversity and moral distress to poor mental health outcomes [22,60,62,63,64,65,66]. As nurses accumulate more years of work, they grow in their clinical competence and can develop coping skills to manage uncomfortable situations [15]. In other studies, both higher number of years on the job [52,67] and lower years of work [62] or temporary positions [41] were associated with higher moral distress, while null effects for age and length of service were reported among HCWs [42,58,68].
Due to the established contributions of age, gender, and work experience to both moral distress and depression, it may be informative to examine how these socio-demographic factors interact with moral distress to predict depression. Specifically, more information on the effect of gender, age, and work experience on the association of moral distress and depressive symptoms could potentially lead to carefully tailored and specific strategies to reduce moral distress, which could effectively reduce depressive symptoms and contribute to a better quality of life for nurses. Knowledge generation in this area may also be helpful in educational settings when creating a curriculum for continuing professional development, to help them deal with situations that may potentially result in moral distress and prepare nursing students to navigate ethical dilemmas. Finally, our findings will add to the nursing literature and may be relevant to practitioners in mental health care.
This is a study about moral distress in general that was conducted during the pandemic. Guided by the foregoing literature in other parts of the world, we hypothesized that: (1) nurses with high moral distress will report greater severity of depressive symptoms. (2) Being a woman, of younger age, and with fewer years of work will be associated with increased depressive symptoms. (3) Gender moderates the association between moral distress and depressive symptoms, such that there would be a higher severity of depression for morally distressed women than men. (4) Age moderates the association between moral distress and depressive symptoms, such that depressive symptoms will be more severe for younger, morally distressed nurses than older nurses. (5) Work experience moderates the association between moral distress and depressive symptoms, such that morally distressed nurses with fewer years of nursing experience will evidence a higher severity of depressive symptoms compared to those with more years of experience at work.
2. Materials and Methods
2.1. Participants and Procedure
Participants were 398 nurses drawn from the University of Nigeria Teaching Hospital (UNTH), Enugu, Nigeria. The UNTH is one of the oldest healthcare institutions for service, teaching, and research in Nigeria. The Hospital, which started in the early 20th century as a general medical facility, has transformed into a tertiary healthcare institution that provides inpatient and outpatient services through highly trained staff, provision of clinical materials and training as well as infrastructure for research, teaching facilities for training of students and other persons in the health delivery team, and conduct and promotion of research on all health-related matters. It has nine training schools including the School of Nursing, Midwifery, Nurse Anesthetists, Post-Basic Ophthalmic Nursing, Perioperative Nursing, and Cardiothoracic Nursing.
With a 5% margin of error, 95% confidence interval, and a depression prevalence of 48% in Nigerian nurses [19], our sample size had adequate power. Data were collected using questionnaires between November 2019 and March 2020. With the permission of the unit heads, nurses in the clinics and wards were approached by one of the authors and two research assistants to recruit potentially eligible participants for the study. After explaining the purpose of the study to them, those who agreed to participate were given the questionnaire. The nurses were instructed to sign the consent form and complete the survey without writing their name(s) on any part of the questionnaire. It took approximately 15 min to complete the survey. Response rate in the study was 80.56%, which is high.
2.2. Inclusion Criteria
To be included in the study, participants had to be be registered nurses, able to read and understand the English language, and engaged in providing direct patient care in the healthcare institution. There are two pathways to licensure as a nurse in Nigeria. One is the Basic Nursing program which requires about three years of study and training in a school of nursing. The other is a bachelor’s degree in nursing which takes five years and is obtained in a federal, state, or private university. A key aspect of both programs is the Nursing and Midwifery Council of Nigeria’s (NMCN) Professional Examination which must be passed by the student before a practice license can be given. After any of these programs, some people go for further training to specialize in an area of nursing. The nurses who work in the teaching hospitals must have such specialty training.
2.3. Ethical Considerations
Ethical clearance for the study was obtained from the hospital’s research ethics committee (Approval Number: NHREC/05/01/200BB-FWA00002458-IRB00002323). All procedures involved in this study were consistent with the ethical standards of the approving research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
2.4. Measures
Data were collected using two self-report measures, namely, the Moral Distress Questionnaire (MDQ) for clinical nurses [69] and the Center for Epidemiological Studies Depression Scale Revised (CESD-R) [70,71], including a sociodemographic questionnaire (age, gender, educational status, and years of work experience).
The 15-item MDQ for clinical nurses was used to assess moral distress. The MDQ was suitable for our study because it is theoretically grounded, culturally sensitive, generic, and applicable to nurses across work settings [69,72]. Participants were required to rate the extent of stress aroused by morally challenging work situations on a 6-point scale, ranging from not at all (1) to all the time (6). Items were marked “irrelevant” by the respondent if they had not experienced such situations (0). Although it has three dimensions related to problems caused by work relationships (α = 0.85), lack of resources (α = 0.79), and time pressure (α = 0.80), there is a higher-order unidimensional total scale (overall α = 0.79). The three factors could not be replicated in our factor analyses. Hence, we used the full scale for our study with an α of 0.83. Higher scores reflect higher moral distress.
The 20-item CESD-R was used to measure symptoms of depression, including sadness (dysphoria), loss of interest (anhedonia), appetite, sleep, concentration, worthlessness, fatigue, and suicidal ideation. The CESD-R has demonstrated good reliability, with α ranging from 0.85 to 0.90 [71], and is a helpful screening tool for assessing depressive symptoms in Nigerian samples [73,74,75,76]. We conducted a confirmatory factor analysis to identify the factor structure of the CESD-R using the current data, but failed to replicate the four factors of the CESD (depressed affect, positive affect, somatic complaints/activity inhibition, and interpersonal difficulties). Instead, a one-factor unidimensional scale had a better fit and this is in line with the previous studies in Nigeria [73,74,75,76]. In the current study, an α of 0.88 was obtained. Participants indicated how they felt or behaved in the previous weeks using a 4-point response option of not at all or less than one day (0), to nearly every day for two weeks (3). Total score ranges from 0–60, with higher scores indicating more symptoms of depression.
2.5. Data Analyses
Pearson’s correlations were conducted to establish the associations between the relevant demographic variables in the study and the significant variables. Model 1 of Hayes [77] regression-based PROCESS macro for SPSS version 28 was applied for hypotheses. Presently, PROCESS is a widely used method in tests of moderation or mediation hypotheses by numerous researchers [78,79,80,81]. Among other benefits over the traditional approaches in tests of moderation effects, the macro not only estimates the coefficients of the model using ordinary least squares linear regression (for continuous outcomes), but also produces contingent results in moderation models [82,83]. Additionally, heteroscedasticity-consistent standard errors are available for inference about path coefficients when probing interactions in moderation analysis [82]. Because we had three moderators, we conducted three multiple regression analyses. In each regression model we conducted, we entered moral distress as the predictor and depressive symptoms as the outcome, with either gender, age, or years of work experience as the moderator. The nurses indicated their actual age and number of years of work experience, and the data were computed as continuous variables. Gender and educational status were categorical variables. Moderation was confirmed when the coefficient of the interaction term (e.g., moral distress and gender) was significant. All hypotheses were tested at the p < 0.05 level.
3. Results
Participants comprised women (94%) and men (6%). They were aged from 19–61 years, with an average age of 36.79 years (SD = 4.28). Their educational qualifications were Basic Nursing (76.4%), Bachelor’s (22.1%), Master’s (1.0%) and Ph.D. (0.5%).
Table 1 indicated that age was positively correlated with work experience and educational status but negatively correlated to moral distress and depressive symptoms. Work experience correlated positively with educational status and negatively with moral distress and depressive symptoms.

Table 1.
Correlations of demographic variables, moral distress, and depressive symptoms.
In Table 2, moral distress was positively associated with depressive symptoms. Gender was not significantly associated with depressive symptoms. However, the interaction of gender and moral distress on depressive symptoms was significant, indicating that gender moderated the relationship between moral distress and depressive symptoms. The slope of the interaction (see Figure 1) showed that moral distress was positively linked to depressive symptoms for women (B = 0.28, p < 0.001) but not for men (B = 0.17, p = 0.517).

Table 2.
Moderating role of gender on relationship between moral distress and depressive symptoms.
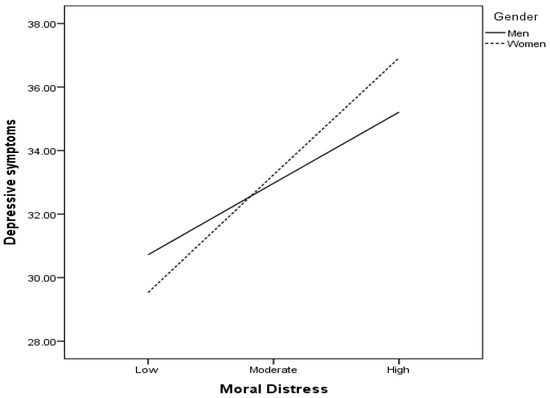
Figure 1.
Slope of moderating role of gender on relationship between moral distress and depressive symptoms.
In Table 3, age was negatively associated with depressive symptoms. The interaction of age and moral distress on depressive symptoms was insignificant, indicating that age did not moderate the relationship between moral distress and depressive symptoms.

Table 3.
Moderating role of age on relationship between moral distress and depressive symptoms.
In Table 4, work experience was negatively associated with depressive symptoms. The interaction of work experience and moral distress on depressive symptoms was insignificant, showing that work experience did not moderate the relationship between moral distress and depressive symptoms.

Table 4.
Moderating role of work experience on relationship between moral distress and depressive symptoms.
4. Discussion
We investigated whether gender moderates the relationship between moral distress and depression among nurses in sub-Saharan Africa. First, we hypothesized that nurses with high moral distress would report greater severity of depressive symptoms. The findings confirmed this hypothesis, and it agrees with previous findings showing that experience of moral distress was associated with increased depressive symptoms among HCWs [36,37,38]. On the contrary, our finding is inconsistent with the finding of a study which reported a null effect of moral distress on depression among HCWs in Romania [45]. During the COVID-19 pandemic, HCWs in sub-Saharan Africa felt a greater work burden due to inadequate resources, increased workload, poor working conditions, and compassion fatigue in the healthcare system. These factors may have contributed to increased moral distress among HCWs and increased depressive symptoms [10,83]. Some nursing assignments may have contradicted cultural or religious beliefs and created ethical dilemmas, especially in the Nigerian setting where the majority of the people are extremely religious.
A sense of helplessness and powerlessness is the root of moral discomfort and distress, which arouses the sensation of having to substantially compromise oneself or something we value because of uncontrollable external pressures [84]. During the COVID-19 pandemic, there might be challenging situations when nurses are aware of, or think they know, what is correct to do but are unable to act appropriately or stop a specific damage for a variety of reasons (such as fear, or uncontrollable external conditions). When nurses’ ideals are regularly violated, either individually or collectively, it causes moral anguish. The experiences of morally distressing events and the attendant constraints to take the right actions at the right time might result in symptoms of depression.
Healthcare institutions can help to enhance the capacity of nurses to withstand and manage the inevitable moral challenges that ignite confusion and moral distress, by supporting them to participate in professional development activities such as continuing education programs on nursing ethics [85,86]. A healthy work environment characterized by effective decision-making; effective communication; genuine teamwork; meaningful recognition; adequate staffing; and sincere leadership will help to reduce conflicts, deal with ethical dilemmas, and preserve the moral integrity of nurses. The most identified informal methods of reducing moral distress were self-care techniques (e.g., medication, physical exercise) and assistance from coworkers, family, or friends [25,27,87]. Professional or official methods of support, such as speaking with supervisors, and seeking counseling support or therapy are also worthwhile [25,38]. These internal and external resources are particularly needed in times of major stressors in the healthcare setting, such as during a pandemic. More course content for students should be designed by nursing educational institutions so that students are ready to deal with situations that are most likely to cause moral anguish in the healthcare setting. If case scenarios and role plays are employed in the classroom by lecturers teaching ethical issues in nursing, it will help to ground students in the issues they may encounter during routine practice.
Secondly, we hypothesized that being a woman, having a younger age, and having fewer years of work will be associated with increased depression. Our findings did not establish an association between gender and depressive symptoms which is inconsistent with past research [34,35,55]. Given the patriarchal culture of African societies, female nurses are more likely to face more stressors and challenging situations in which they must combine their workload with domestic duties such as housekeeping and childcare. However, the COVID-19 pandemic may have impacted both the male and female nurses in some ways that reduced the gendered pattern of depression. We also found that older nurses reported reduced severity of depression; this supports previous reports of greater severity of depression among those who were younger in age [35]. Similarly, nurses who have worked for a greater number of years reported lower severity of depressive symptoms in our study. In previous research, depression was more prevalent among nurses of lower professional rank [35]. However, the finding conflicts with previous findings that a higher service rank was associated with an increased severity of depression among HCWs [34]. Although the COVID-19 pandemic has had more serious impacts on the healthcare professions than any other pandemic in recent history, those who were older in age and work experience may have acquired more competencies and skills to manage the uncertainties of patient care. Hence, they may have more protective resources against depression. Usually, those who were older in age might also have had more years of work experience. With these increasing number of years, they may have access to both personal and workplace resources to support them in coping with, adapting to, and recovering from stressful conditions.
Most importantly, we found that gender moderated the relationship between moral distress and depressive symptoms. Being male has been found to be associated with stronger moral resilience—the capacity to maintain or regain their moral integrity in the face of moral dilemma and increased distressing situations at work [54]. Although the nursing profession is dominated by women in Nigeria, the leadership of the professional association of nurses in Nigeria is often dominated by men. The male-to-female ratio is listed as 2:5 on Nursing World Nigeria, a Nigerian nursing website that features peer-reviewed clinical nursing and midwifery research. Due to the men’s involvement in those union activities and engagements with management, they often may not be involved in the daily activities of patient care. This may insulate them from depression. Hence, preventive efforts and interventions for moral distress should give more attention to female frontline nurses to reduce the likelihood of them becoming depressed.
Our study had notable strengths. It has contributed to knowledge on how moral distress may be associated with mental health, especially during the COVID-19 pandemic in the sub-Saharan African setting where there is limited research. Moreso, as a key addition to existing body of knowledge in the field, our findings go beyond direct associations by demonstrating how gender influences the link between moral distress and depression. Investigation of such gender-specific effects have been suggested in past research outside Africa [36,37]. The major limitation is that our study was based on cross-sectional data making it impossible to infer a cause-and-effect relationship from the connections discovered. We could only assess symptoms of depression and not a diagnosis of depression because our data were self-reported. We were not able to determine if the respondents exaggerated, or if social desirability bias influenced the responses. Our data were collected from one tertiary healthcare setting, which limits the generalizability of the findings.
Another notable limitation lies in the unbalanced gender distribution in the sample, and most of the participants were relatively young. However, male nurses are fewer than female nurses in the Nigerian healthcare setting. We were unable to track the proportion of surveys that were completed prior to the first case of COVID-19 in Nigeria and post-first case. If we had this information, it would have helped to offer a sense of the degree that COVID contributed to depression/moral distress.
Our results cannot account for either the impact of subsequent COVID surges or the experiences of nurses during the peak of the pandemic. Future research should examine longitudinal trajectories of moral distress and its effect on depressive symptoms in the longer term. Longitudinal data will also help to examine potential mediators of the associations between moral distress and mental health outcomes thereby elucidating possible causal effects. If possible, there should be further efforts to determine the symptom thresholds to determine the possible depression severity of nurses. Such studies should also be conducted in tertiary healthcare institutions across the regions of Nigeria. Intervention research aimed at actions designed to decrease moral distress will also be worthwhile.
5. Conclusions
Due to the limited research on moral distress and mental health among healthcare professionals in the African setting, we examined the link between moral distress and depression, as well as whether socio-demographic factors moderating the contributions of morally distressing experiences to depression in a sub-Saharan African sample of nurses. It was shown that there was a strong association between elevated moral distress and heightened depressive symptoms in women, but not in men. The association between moral distress and depressive symptoms was not moderated by the nurses’ age or years of work experience, even though older age and more years of nursing experience were linked to fewer depressive symptoms. Findings point to the survey as a modest effort to highlight the relevance of recognizing moral distress, age, gender, and work experience when designing and implementing nurses’ mental health interventions in the pandemic era.
Author Contributions
Conceptualization: M.O.N., J.C.C. and C.M.I.; methodology: M.O.N., O.H.E. and D.K.R.; data analysis and interpretation: M.O.N., J.C.C. and D.O.-O.; writing—original draft preparation: O.H.E. and O.M.O.; writing—review and editing: J.C.C., C.M.I., C.N. and A.C.-O. All authors have read and agreed to the published version of the manuscript.
Funding
No funding was received for conducting this study.
Institutional Review Board Statement
Approval was obtained from the ethics committee of the University of Nigeria Teaching Hospital (NHREC/05/01/200BB-FWA00002458-IRB00002323). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors have no competing interests to declare that are relevant to the content of this article.
References
- Etim, J.J.; Bassey, P.E.; Ndep, A.O. Work-related stress among healthcare workers in Ugep, Yakurr Local Government Area, Cross River State, Nigeria: A study of sources, effects, and coping strategies. Int. J. Public Health Pharm. Pharmacol. 2015, 1, 23–34. [Google Scholar]
- Mefoh, P.C.; Ude, E.N.; Chukwuorji, J.C. Age and burnout syndrome in nursing professionals: Moderating role of emotion-focused coping. Psychol. Health Med. 2019, 24, 101–107. [Google Scholar] [CrossRef]
- Mmule, M.M.; Mabedi, K. Perception of stress by nurses in their profession: A case of primary health care clinics. Biomed. J. Sci. Tech. Res. 2018, 2, 2137–2140. [Google Scholar]
- Ogbonnaya, C.; Ogbogu, C.J.; Ingwu, J.; Opara, H. Sources and perceived effects of work-related stress among nursing working in acute care units of University of Nigeria Teaching Hospital Enugu-Nigeria. J. Adv. Med. Med. Res. 2018, 25, 1–9. [Google Scholar]
- Sarafis, P.; Rousaki, E.; Tsounis, A.; Malliarou, M.; Lahana, L.; Bamidis, P.; Niakas, D.; Papastavrou, E. The impact of occupational stress on nurses’ caring behaviours and their health-related quality of life. BioMed Cent. Nurs. 2016, 15, 47–56. [Google Scholar]
- Alimoradi, Z.; Jafari, E.; Lin, C.Y.; Rajabi, R.; Marznaki, Z.H.; Soodmand, M.; Potenza, M.N.; Pakpour, A.H. Estimation of moral distress among nurses: A systematic review and meta-analysis. Nurs. Ethics 2023, 30, 334–357. [Google Scholar] [CrossRef]
- Emmamally, W.; Chiyangwa, O. Exploring moral distress among critical care nurses at a private hospital in Kwa-Zulu Natal, South Africa. S. Afr. J. Crit. Care 2020, 36, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Lake, E.T.; Narva, A.M.T.; Holland, S.; Smith, J.G.; Crane, E.; Fitzpatric, K.E.; Rosenbaum, R.F.; Rebecca, R.S.; Clark, J.A. Hospital nurses’ moral distress and mental health during COVID-19. J. Adv. Nurs. 2021, 78, 799–809. [Google Scholar] [CrossRef] [PubMed]
- Mewborn, E.K.; Fingerhood, M.L.; Johanson, L.; Hughes, V. Examining moral injury in clinical practice: A narrative literature review. Nurs. Ethics 2023, 30, 960–974. [Google Scholar] [CrossRef]
- Nagle, E.; Surina, S.; Griškēviča, I. Healthcare workers’ moral distress during the COVID-19 pandemic: A scoping review. Soc. Sci. 2023, 12, 371. [Google Scholar] [CrossRef]
- Nordin, A.; Engström, Å.; Fredholm, A.; Persenius, M.; Andersson, M. Measuring moral distress in Swedish intensive care: Psychometric and descriptive results. Intensive Crit. Care Nurs. 2023, 76, 103376. [Google Scholar] [CrossRef] [PubMed]
- Tavakol, N.; Molazem, Z.; Rakhshan, M.; Asemani, O.; Bagheri, S. Moral distress in psychiatric nurses in COVID-19 crisis. BMC Psychol. 2023, 11, 47. [Google Scholar] [CrossRef] [PubMed]
- Prompahakul, C.; Keim-Malpass, J.; LeBaron, V.; Yan, G.; Epstein, E.G. Moral distress among nurses: A mixed-methods study. Nurs. Ethics 2021, 28, 1165–1182. [Google Scholar] [CrossRef]
- Austin, C.L.; Saylor, R.; Finley, P.J. Moral distress in physicians and nurses: Impact on professional quality of life and turnover. Psychol. Trauma Theory Res. Pract. Policy 2017, 9, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Galiana, L.; Moreno-Mulet, C.; Carrero-Planells, A.; López-Deflory, C.; García-Pazo, P.; Nadal-Servera, M.; Sansó, N. Spanish psychometric properties of the moral distress scale-revised: A study in healthcare professionals treating COVID-19 patients. BMC Med. Ethics 2023, 24, 30. [Google Scholar] [CrossRef]
- Ibigbami, O.I.; Akinsulore, A.; Opakunle, T.; Seun-Fadipe, C.; Oginni, O.A.; Okorie, V.O.; Oloniniyi, I.; Olibamoyo, O.; Aloba, O.O.; Mapayi, B.; et al. Psychological distress, anxiety, depression, and associated factors among Nigerian healthcare workers during COVID-19 pandemic: A cross-sectional study. Int. J. Public Health 2022, 67, 1604835. [Google Scholar] [CrossRef] [PubMed]
- Johnson-Coyle, L.; Opgenorth, D.; Bellows, M.; Dhaliwal, J.; Richardson-Carr, S.; Bagshaw, S.M. Moral distress and burnout among cardiovascular surgery intensive care unit healthcare professionals: A prospective cross-sectional survey. Can. J. Crit. Care Nurs. 2016, 27, 27–36. [Google Scholar] [PubMed]
- Mehlis, K.; Bierwirth, E.; Laryionava, K.; Mumm, F.; Hiddemann, W.; Heußner, P.; Winkler, E.C. High prevalence of moral distress reported by oncologists and oncology nurses in end-of-life decision making. Psycho-Oncology 2018, 27, 2733–2739. [Google Scholar] [CrossRef]
- Olude, O.A.; Odeyemi, K.; Kanma-Okafor, O.J.; Badru, O.A.; Bashir, S.A.; Olusegun, J.O.; Atilola, O. Mental health status of doctors and nurses in a Nigerian tertiary hospital: A COVID-19 experience. S. Afr. J. Psychiatry SAJP 2022, 28, 1904. [Google Scholar] [CrossRef]
- Pergert, P.; Bartholdson, C.; Blomgren, K.; Af Sandeberg, M. Moral distress in paediatric oncology: Contributing factors and group differences. Nurs. Ethics 2019, 26, 2351–2363. [Google Scholar] [CrossRef]
- Schneider, J.N.; Hiebel, N.; Kriegsmann-Rabe, M.; Schmuck, J.; Erim, Y.; Morawa, E.; Jerg-Bretzke, L.; Beschoner, P.; Albus, C.; Hannemann, J.; et al. Moral distress in hospitals during the first wave of the COVID-19 pandemic: A web-based survey among 3293 healthcare workers within the German network university medicine. Front. Psychol. 2021, 12, 775204. [Google Scholar] [CrossRef] [PubMed]
- Sommerlatte, S.; Lugnier, C.; Schoffer, O.; Jahn, P.; Kraeft, A.L.; Kourti, E.; Michl, P.; Reinacher-Schick, A.; Schmitt, J.; Birkner, T.; et al. Mental burden and moral distress among oncologists and oncology nurses in Germany during the third wave of the COVID-19 pandemic: A cross-sectional survey. J. Cancer Res. Clin. Oncol. 2023, 149, 6211–6223. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Koenig, H.G.; Tong, Y.; Wen, J.; Sui, M.; Liu, H.; Zaben, F.A.; Liu, G. Moral injury in Chinese health professionals during the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy 2022, 14, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Corley, M.C. Nurse moral distress: A proposed theory and research Agenda. Nurs. Ethics 2002, 9, 636–650. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Prieto, E.; Longstaff, H.; Black, A.; Virani, A.K. COVID-19 outbreak: Understanding moral-distress experiences faced by healthcare workers in British Columbia, Canada. Int. J. Environ. Res. Public Health 2022, 19, 9701. [Google Scholar] [CrossRef] [PubMed]
- Donkers, M.A.; Gilissen, V.J.H.S.; Candel, M.J.J.M.; van Dijk, N.M.; Kling, H.; Heijnen-Panis, R.; Pragt, E.; van der Horst, I.; Pronk, S.A.; van Mook, W.N.K.A. Moral distress and ethical climate in intensive care medicine during COVID-19: A nationwide study. BMC Med. Ethics 2021, 22, 73. [Google Scholar] [CrossRef] [PubMed]
- Hegarty, S.; Lamb, D.; Stevelink, S.A.M.; Bhundia, R.; Raine, R.; Doherty, M.J.; Scott, H.R.; Marie Rafferty, A.; Williamson, V.; Dorrington, S.; et al. ‘It hurts your heart’: Frontline healthcare worker experiences of moral injury during the COVID-19 pandemic. Eur. J. Psychotraumatol. 2022, 13, 2128028. [Google Scholar] [CrossRef]
- Stephenson, P.; Warner-Stidham, A. Nurse reports of moral distress during the COVID-19 pandemic. SAGE Open Nurs. 2024, 10, 23779608231226095. [Google Scholar] [CrossRef]
- Lamiani, G.; Biscardi, D.; Meyer, E.C.; Giannini, A.; Vegni, E. Moral distress trajectories of physicians 1 year after the COVID-19 outbreak: A grounded theory study. Int. J. Environ. Res. Public Health 2021, 18, 13367. [Google Scholar] [CrossRef]
- Lemmo, D.; Vitale, R.; Girardi, C.; Salsano, R.; Auriemma, E. Moral distress events and emotional trajectories in nursing narratives during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2022, 19, 8349. [Google Scholar] [CrossRef]
- Smallwood, N.; Pascoe, A.; Karimi, L.; Willis, K. Moral distress and perceived community views are associated with mental health symptoms in frontline health workers during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 8723. [Google Scholar] [CrossRef]
- Simonovich, S.D.; Webber-Ritchey, K.J.; Spurlark, R.S.; Florczak, K.; Mueller Wiesemann, L.; Ponder, T.N.; Reid, M.; Shino, D.; Stevens, B.R.; Aquino, E.; et al. Moral distress experienced by us nurses on the frontlines during the COVID-19 pandemic: Implications for nursing policy and practice. SAGE Open Nurs. 2022, 8, 23779608221091059. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, L.L.; Long-Daniels, A.; Appah, M.; Zhai, Y.; Watson, D.M.; Walker, K.; Young-Bilbo, K.; Aboagye, A.; Tucker, C.; McCarthy, S. The association between social determinants of health and depressive disorders: A 2017 Behavioral Risk Factor Surveillance System (BRFSS) analysis. Psychiatry Int. 2023, 4, 147–159. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Rezaei, S.; Hoseinipalangi, Z.; Rafiei, S.; Dolati, Y.; Hosseinifard, H.; Asl, M.T.; Mejareh, Z.N.; Deylami, S.; Abdollahi, B.; Ardakani, M.F.; et al. The global png health workers during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. Rep. 2022, 8, 100326. [Google Scholar] [CrossRef]
- Plouffe, R.A.; Nazarov, A.; Forchuk, C.A.; Gargala, D.; Deda, E.; Le, T.; Bourret-Gheysen, J.; Jackson, B.; Soares, V.; Hosseiny, F.; et al. Impacts of morally distressing experiences on the mental health of Canadian health care workers during the COVID-19 pandemic. Eur. J. Psychotraumatol. 2021, 12, 1984667. [Google Scholar] [CrossRef] [PubMed]
- Maunder, R.G.; Heeney, N.D.; Greenberg, R.A.; Jeffs, L.P.; Wiesenfeld, L.A.; Johnstone, J.; Hunter, J.J. The relationship between moral distress, burnout, and considering leaving a hospital job during the COVID-19 pandemic: A longitudinal survey. BMC Nurs. 2023, 22, 243. [Google Scholar] [CrossRef] [PubMed]
- ForZerach, G.; Levi-Belz, Y. Moral injury and mental health outcomes among Israeli health and social care workers during the COVID-19 pandemic: A latent class analysis approach. Eur. J. Psychotraumatol. 2021, 12, 1945749. [Google Scholar] [CrossRef]
- Lamiani, G.; Setti, I.; Barlascini, L.; Vegni, E.; Argentero, P. Measuring moral distress among critical care clinicians: Validation and psychometric properties of the Italian Moral Distress Scale-Revised. Crit. Care Med. 2017, 45, 430–470. [Google Scholar] [CrossRef]
- Lamiani, G.; Dordoni, P.; Arqentero, P. Value congruence and depressive symptoms among critical care clinicians: The mediating role of moral distress. Stress Health 2018, 34, 135–142. [Google Scholar] [CrossRef]
- Romero-García, M.; Delgado-Hito, P.; Gálvez-Herrer, M.; Ángel-Sesmero, J.A.; Velasco Sanz, T.R.; Benito-Aracil, L.; Heras-La Calle, G. Moral distress, emotional impact and coping in intensive care unit staff during the outbreak of COVID-19. Intensive Crit. Care Nurs. 2022, 70, 103206. [Google Scholar] [CrossRef] [PubMed]
- Colville, G.A.; Dawson, D.; Ravinthiran, S.M.; Chaudry-Daley, Z.; Perkins-Portas, L. A survey of moral distress in staff working in intensive care in UK. J. Intensive Care Soc. 2019, 20, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Guttormson, J.L.; Calkins, K.; McAndrew, N.; Fitzgerald, J.; Losurdo, H.; Loonsfoot, D. Critical care nurse burnout, moral distress, and mental health during the COVID-19 Pandemic: A United States survey. Heart Lung J. Crit. Care 2022, 55, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Sonis, J.; Pathman, D.E.; Read, S.; Gaynes, B.N. A national study of moral distress among U.S. internal medicine physicians during the COVID-19 pandemic. PLoS ONE 2022, 17, e0268375. [Google Scholar] [CrossRef] [PubMed]
- Petrișor, C.; Breazu, C.; Doroftei, M.; Mărieș, I.; Popescu, C. Association of moral distress with anxiety, depression, and an intention to leave among nurses working in intensive care units during the COVID-19 pandemic. Healthcare 2021, 9, 1377. [Google Scholar] [CrossRef] [PubMed]
- Berlinger, N.; Berlinger, A. Culture and moral distress: What’s the connection and why does it matter? AMA J. Ethics 2017, 19, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Bressler, T.; Hanna, D.R.; Smith, E. Making sense of moral distress within cultural complexity. J. Hosp. Palliat. Nurs. 2017, 19, 7–14. [Google Scholar] [CrossRef]
- Scott, M.; Wade, R.; Tucker, G.; Unsworth, J. Identifying sources of moral distress amongst critical care staff during the COVID-19 pandemic using a naturalistic inquiry. SAGE Open Nurs. 2023, 9, 23779608231167814. [Google Scholar] [CrossRef] [PubMed]
- Silverman, H.J.; Kheirbek, R.E.; Moscou-Jackson, G.; Day, J. Moral distress in nurses caring for patients with COVID-19. Nurs. Ethics 2021, 28, 1137–1164. [Google Scholar] [CrossRef]
- Abebaw, H. Predictors of Moral Distress among Nurses Working in Jimma University Medical Center, Jimma Zone, Jimma Town, South West, Ethiopia. Bachelor’s Thesis, Jimma University, Jimma, Ethiopia, 2019. Available online: https://repository.ju.edu.et/bitstream/handle/123456789/4115/PDF.pdf?sequence=1&isAllowed=n (accessed on 28 December 2023).
- Ashuntantang, G.; Miljeteig, I.; Luyckx, V.A. Bedside rationing and moral distress in nephrologists in sub- Saharan Africa. BMC Nephrol. 2022, 23, 196. [Google Scholar] [CrossRef]
- Berhie, A.Y.; Tezera, Z.B.; Azagew, A.W. Moral distress and its associated factors among nurses in Northwest Amhara regional state referral hospitals, Northwest Ethiopia. Psychol. Res. Behav. Manag. 2020, 13, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Kok, N.; Van Gurp, J.; van der Hoeven, J.G.; Fuchs, M.; Hoedemaekers, C.; Zegers, M. Complex interplay between moral distress and other risk factors of burnout in ICU professionals: Findings from a cross-sectional survey study. BMJ Qual. Saf. 2023, 32, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Spilg, E.G.; Rushton, C.H.; Phillips, J.L.; Kendzerska, T.; Saad, M.; Gifford, W.; Gautam, M.; Bhatla, R.; Edwards, J.D.; Quilty, L.; et al. The new frontline: Exploring the links between moral distress, moral resilience and mental health in healthcare workers during the COVID-19 pandemic. BMC Psychiatry 2022, 22, 19. [Google Scholar] [CrossRef]
- Cheung, T.; Yip, P.S.F. Lifestyle and depression among Hong Kong nurses. Int. J. Environ. Res. Public Health 2016, 13, 135. [Google Scholar] [CrossRef] [PubMed]
- Babamohamadi, H.; Bakuei Katrimi, S.; Paknazar, F. Moral distress and its contributing factors among emergency department nurses: A cross-sectional study in Iran. Int. Emerg. Nurs. 2021, 56, 100982. [Google Scholar] [CrossRef]
- O’Connell, C.B. Gender and the experience of moral distress in critical care nurses. Nurs. Ethics 2015, 22, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Shehadeh, J.; Almaraira, O.; Hamdan-Mansour, A. Determinants of moral distress among mental health professionals. Open Nurs. J. 2022, 16, e187443462203030. [Google Scholar] [CrossRef]
- Abdolmaleki, M.; Lakdizaji, S.; Ghahramanian, A.; Allahbakhshian, A.; Behshid, M. Relationship between autonomy and moral distress in emergency nurses. Indian J. Med. Ethics 2019, 4, 20–25. [Google Scholar] [CrossRef]
- Almutairi, A.F.; Salam, M.; Adlan, A.A.; Alturki, A.S. Prevalence of severe moral distress among healthcare providers in Saudi Arabia. Psychol. Res. Behav. Manag. 2019, 12, 107–115. [Google Scholar] [CrossRef]
- Karagozoglu, S.; Yildirim, G.; Ozden, D.; Çınar, Z. Moral distress in Turkish intensive care nurses. Nurs. Ethics 2017, 24, 209–224. [Google Scholar] [CrossRef]
- Hamaideh, S.H. Moral distress and its correlates among mental health nurses in Jordan. Int. J. Ment. Health Nurs. 2014, 23, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, R.; Zoboli, E.L.C.P.; Vieira, M. Moral distress in nurses: A description of the risks for professionals. Texto Contexto-Enferm. 2018, 27, 2–12. [Google Scholar]
- Sriharan, A.; West, K.J.; Almost, J.M.; Hamza, A. COVID-19-related occupational burnout and moral distress among nurses: A rapid scoping review. Nurs. Leadersh. 2021, 34, 7–19. [Google Scholar] [CrossRef] [PubMed]
- Wolf, A.T.; White, K.R.; Epstein, E.G.; Enfield, K.B. Palliative care and moral distress: An institutional survey of critical care nurses. Crit. Care Nurse 2019, 39, 38–49. [Google Scholar] [CrossRef] [PubMed]
- Woods, M.; Rodgers, V.; Towers, A.; Grow, S.L. Research moral distress among New Zealand nurses: National survey. Nurs. Ethics 2015, 22, 117–130. [Google Scholar] [CrossRef]
- Abbasi, M.; Nejadsarvari, N.; Kiani, M.; Borhani, F.; Bazmi, S.; Nazari Tavaokkoli, S.; Rasouli, H. Moral distress in physicians practicing in hospitals affiliated to medical sciences universities. Iran. Red Crescent Med. J. 2014, 16, e18797. [Google Scholar] [CrossRef] [PubMed]
- Abdalgeleel, S.A.; Moneer, M.M.; Refaee, A.S.; Samir, M.M.; Khalaf, O.O.; Allam, R.M. Depression and fatigue among Egyptian health care workers: Cross-sectional survey. J. Public Health 2023. [Google Scholar] [CrossRef]
- Eizenberg, M.M.; Desivilya, H.S.; Hirschfeld, J.H. Moral distress questionnaire for the clinical nurses: Instrument development. J. Adv. Nurs. 2009, 65, 885–892. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Van Dam, N.T.; Earleywine, M. Validation of the Center for Epidemiologic Studies Depression Scale—Revised (CESD-R): Pragmatic depression assessment in the general population. Psychiatry Res. 2011, 186, 128–132. [Google Scholar] [CrossRef]
- Tian, X.; Jin, Y.; Chen, H.; Jiménez-Herrera, M.F. Instruments for detecting moral distress in clinical nurses: A systematic review. INQUIRY J. Health Care Organ. Provis. Financ. 2021, 58, 46958021996499. [Google Scholar] [CrossRef]
- Eke, O.H.; Onyenyirionwu, G.U. Psychosocial predictors of peripartum depression among Nigerian women. J. Women’s Health Dev. 2019, 2, 058–067. [Google Scholar]
- Ifeagwazi, C.M.; Chukwuorji, J.C.; Ugwu, O.A. Depressive symptoms in rural school teachers: Role of stress, gender and age. Int. J. Res. Arts Soc. Sci. 2013, 5, 485–503. [Google Scholar]
- Ifeagwazi, C.M.; Obi, N.G.; Udensi, C.E.; Chukwuorji, J.C. Influence of perceived injustice, social support and gender on depressive symptoms among orthopedic patients. Eur. J. Sci. Res. 2014, 125, 370–383. [Google Scholar]
- Kokou-Kpolou, C.K.; Iorfa, S.K.; Park, S.; Chinweuba, D.C.; Cénat, J.M.; Chukwuorji, J.C. The Center for Epidemiologic Studies Depression Scale–Revised (CESD-20-R): Factorial validity and gender invariance among Nigerian young adults. Curr. Psychol. 2022, 41, 7888–7897. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2022. [Google Scholar]
- Amazue, L.O.; Ozor, O.T.; Chukwuorji, J.C.; Ifeagwazi, C.M.; Onu, D.U.; Obi, N.G. Mental pain and suicide ideation in nursing students: The moderating role of emotion regulation. Cogn. Brain Behav. 2019, 23, 171–191. [Google Scholar] [CrossRef]
- Chukwuorji, J.C.; Uzuegbu, C.N.; Agbo, F.; Ifeagwazi, C.M.; Ebulum, G.C. Different slopes for different folks: Gender moderates the relationship between empathy and narcissism. Curr. Psychol. 2020, 39, 1808–1818. [Google Scholar] [CrossRef]
- Onyedire, N.G.; Chukwuorji, J.C.; Orjiakor, T.C.; Onu, D.U.; Aneke, C.I.; Ifeagwazi, C.M. Associations of dark triad traits and problem gambling: Moderating role of age among university students. Curr. Psychol. 2021, 40, 2083–2094. [Google Scholar] [CrossRef]
- Simha, A.; Pandey, J. Trust, ethical climate and nurses’ turnover intention. Nurs. Ethics 2021, 28, 714–722. [Google Scholar] [CrossRef]
- Igartua, J.-J.; Hayes, A.F. Mediation, moderation, and conditional process analysis: Concepts, computations, and some common confusions. Span. J. Psychol. 2021, 24, e49. [Google Scholar] [CrossRef]
- Riedel, P.L.; Kreh, A.; Kulcar, V.; Lieber, A.; Juen, B. A Scoping Review of Moral Stressors, Moral Distress and Moral Injury in Healthcare Workers during COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 1666. [Google Scholar] [CrossRef] [PubMed]
- DeMarco, M. That Powerlessness You Feel Is Called “Moral Distress”. Available online: https://www.psychologytoday.com/us/blog/soul-console/202301/that-powerlessness-you-feel-is-called-moral-distress (accessed on 24 January 2023).
- Rushton, C.H. Moral resilience: A capacity for navigating moral distress in critical care. AACN Adv. Crit. Care 2016, 27, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Rushton, C.H. Cultivating moral resilience. Am. J. Nurs. 2017, 117, S11–S15. [Google Scholar] [CrossRef] [PubMed]
- Ünal, Y.; Çakır, E.; Tekeli-Yesil, S. Determinants of the mental health condition of healthcare workers during the initial phase of the COVID-19 pandemic in Turkey. J. Public Health 2022, 30, 2847–2853. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).