Abstract
Interventional pulmonology is a rapidly growing field with increasing demand. To meet this demand, training in interventional pulmonology is expanding. What started as a single training program without a standardized curriculum has grown to 40 accredited training programs with a well-defined curriculum that is now overseen by the Accreditation Council for Graduate Medical Education. As the field develops, research is being actively performed to develop validated competency assessment tools and describe the learning curves for pulmonary procedures. As research evolves, this information can be used to better standardize training in interventional pulmonology and move the field towards a competency-based training model.
1. Introduction
Interventional pulmonology is a rapidly growing field with new procedures routinely being developed for a wide variety of conditions [1]. The field of interventional pulmonology encompasses a variety of advanced pulmonary procedures, including advanced bronchoscopic procedures for biopsy of both central and peripheral thoracic lesions, bronchoscopic modalities for relief of central airway obstruction, and procedures for the diagnosis and treatment of recurrent pleural disease. As advanced pulmonary procedures have rapidly shown their value in the diagnosis and treatment of pulmonary and pleural disease, the field of interventional pulmonology has rapidly grown, and now has its own professional association, academic journal, and training society [2,3].
The earliest North American experts in interventional pulmonology were trained in an apprenticeship model, often traveling to Europe and Japan to be trained by the physicians who originally described these procedures [4]. As demand for these advanced procedures grew, however, this training model could not produce enough North American experts to meet this demand. To meet this demand, 12-month fellowships have been developed in North America to provide adequate training in these advanced pulmonary procedures [3]. These fellowships, performed after pulmonary/critical care fellowship, provide in-depth training in both the cognitive and technical aspects of advanced pulmonary procedures.
While suggested minimum numbers of procedures to achieve procedure competency have been published, they are based on expert consensus [5,6]. The current accreditation guidelines suggest that procedural competency should be determined by program directors on the basis of the direct observation and tracking of outcomes and complications [3]. Competency-based education has become a popular paradigm in medical education, owing to its ability to account for the variable skill acquisition of different trainees [7]. Competency assessment and learning curves are currently an area of active research within interventional pulmonology, and many interventional pulmonary procedures have validated evaluation tools to help educators.
This article reviews the history of formal interventional pulmonary training and assesses both current training standards in interventional pulmonology and the current scientific literature supporting training in pulmonary procedures.
2. History of Interventional Pulmonary Training
The earliest tracheoscopy was described in 1895 by Alfred Kerstein [8], and the utility of rigid bronchoscopy for removal of foreign bodies was reported by Gustav Killian in 1897. The procedure was brought to the United States by Chevalier Jackson [9]. While originally used for foreign body removal, the rigid bronchoscope was repurposed for use in laser ablation in 1981 and tracheobronchial stenting in 1990 [8]. The use of radial endobronchial ultrasound for central and peripheral lesions was first described in 1992 [10], followed by linear endobronchial ultrasound in 2004 [11] and electromagnetic navigation in 2006 [12].
The introduction of thoracoscopy to treat pleural tuberculosis and empyema is typically credited to Hans-Christian Jacobeus, as described in his 1910 report, although some evidence suggests the procedure may have been performed as early as 1866 [13]. While originally used in the treatment of tuberculous pleural effusions, thoracoscopy was, in the 1950s–1960s, adapted for biopsy of the lung and pleura, and for pleurodesis by talc poudrage. The use of an ambulatory indwelling catheter to manage malignant pleural effusions was first described in 1986 [14], and the first commercial device for this purpose, the PleurX Catheter, was approved by the United States Food and Drug Administration in 1997 [15].
Interventional pulmonology was formally described as a distinct procedural specialty in 2002, in a joint statement by the European Respiratory Society (ERS) and the American Thoracic Society (ATS) [5]. At this time, it was recognized that advanced pulmonary procedures “require additional training and expertize beyond that required in a standard pulmonary medicine training programme”. Initial recommendations for necessary experience to gain and maintain competency in these interventional procedures were developed on the basis of expert consensus [6]. A 2005 survey showed that procedural volumes in general pulmonary/critical care fellowship were inadequate for achieving competency in most interventional procedures [16]. In addition, even for procedures such as endobronchial ultrasound, which are commonly taught in general pulmonary fellowships, providers with additional post-graduate training are more likely to perform appropriate mediastinal staging [17]. For these reasons, interventional pulmonary fellowships have formed to provide this necessary additional training.
The first dedicated interventional pulmonary program in North America was founded in 1996 [18], and by 2010, the first year interventional pulmonary participated in the match, there were 14 participating programs that all filled their positions [19]. In this same year, the Association of Interventional Pulmonology Program Directors (AIPPD) was established to help standardize and ensure the quality of interventional pulmonary training [3]. The first interventional pulmonology board examination was administered and validated in 2013 [20], and by this time there were 17 programs. Unfortunately, as the field grew, significant variability in training practices between training programs was apparent [21].
Proposed guidelines for interventional pulmonary training, which defined the scope of training and general training requirements, were published in 2010, with the goal of standardizing interventional pulmonary training [22]. Official standards for accreditation by the American Association for Bronchology and Interventional Pulmonology (AABIP) were published in 2017 [3]. For those seeking board certification in interventional pulmonology, the practice pathway, which allowed physicians to qualify to sit on boards based on procedural experience, without needing formal interventional pulmonary training, was no longer available after 2016 [23], and as of 2018 any physician seeking board eligibility is required to have graduated from a program accredited by the AABIP at the time of their graduation [24]. Interventional pulmonology became an Accreditation Council for Graduate Medical Education (ACGME) accredited subspecialty in 2023 [18]. The timeline of developments in interventional pulmonology education is summarized in Figure 1.
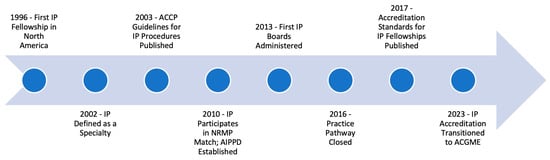
Figure 1.
Timeline of major developments in interventional pulmonology education.
3. Current State of Interventional Pulmonology Training
3.1. Interventional Pulmonary Training in North America
There are currently 40 training programs accredited by the AABIP [25], although all future accreditation has been transitioned to the ACGME. The general structure of the training program was designed to mirror ACGME general program requirements [3]. Sponsoring institutions are required to have sufficient work and call space, medical records, a library, and clinical support services to practice interventional pulmonology. Programs are required to last at least 12 months, with at least 9 months dedicated to direct clinical training. All programs must have at least two AABIP board-certified faculty, with one serving as program director. There must also be identified faculty in associated specialties, such as thoracic surgery and otolaryngology. Applicants must have graduated from a pulmonary/critical care fellowship program, which is performed after completing an internal medicine residency.
Training in interventional pulmonology involves both the cognitive aspects of care for interventional pulmonary patients and the technical aspects of advanced pulmonary procedures. The suggested core curriculum for interventional pulmonology does not only include information about the procedures themselves, and also covers the anatomy and physiology of the airway and pleura, the pathophysiology of structural airway and pleural disease, principles of thoracic imaging, basic principles of radiation therapy and chemotherapy, safety aspects of laser and radiation, business aspects of interventional pulmonology, and research methods. This knowledge is conveyed through didactics, journal clubs, and weekly case conferences. Fellows must also attend at least 44 half-day clinics dedicated to outpatient evaluation of interventional pulmonary patients.
Accredited fellowships are required to have a sufficient institutional procedure volume of all mandatory procedures; these requirements are not just for the individual fellow but are instead set to ensure that the training institution itself has sufficient experience of these procedures to ensure a safe and educational training environment. Training through use of simulation is also required. Programs seeking accreditation apply through the ACGME Accreditation Data System [26]. The application includes an online common application showing common program requirements have been met, a specialty-specific electronic document application attesting program-specific requirements have been met, and supporting documents, including an acceptance of policies and sample evaluations. The use of simulation in procedural training is also required. The AABIP and AIPPD jointly sponsor a yearly training seminar for interventional pulmonary fellows that includes cadaver simulations [27].
Board certification in interventional pulmonology is overseen by the AABIP [24]. As of 2018, only graduates of accredited fellowships are considered eligible for board certification, although a limited exemption is available in the 2023 and 2024 cycles for pre-2016 pulmonary/critical care graduates who would have been eligible under the pre-2016 practice pathway. The exam is a 120 min, 75 question, multiple choice exam that has been shown to effectively discriminate between physicians at various levels of pulmonary medicine and interventional pulmonology training [20]. For advanced bronchoscopists who do not meet the criteria for interventional pulmonology board certification, the AABIP also offers the Certificate of Added Qualification, in recognition of this additional training; the examination includes a knowledge assessment and a skills test that uses validated assessment tools. Graduates of interventional pulmonology programs are most commonly employed in interventional pulmonary positions in academic settings [28].
3.2. Interventional Pulmonary Training in Europe
Due to the nature of the European Union’s governance structure, whereby individual nations retain a greater degree of sovereignty than US states, the structure and requirements for interventional pulmonary training are less standardized than they are in the US, and training in one EU nation may not guarantee the ability to practice in another [29]. Historically, training has followed a post-graduate apprenticeship model, with focus on individual procedures rather than the specialty as a whole. This apprenticeship model is common across the world. The European Respiratory Society does sponsor a training program in endobronchial ultrasound, which consists of didactic training, simulation sessions, and supervised procedural training at the trainee’s home institution. The supervised training includes twenty procedure reports and three video procedures, with assessment and feedback provided. The training program certificate is widely recognized throughout the EU.
Among individual European nations, France and Italy stand out as offering structured fellowship training in interventional pulmonology [30]. In Italy, the University of Florence offers a structured one-year program that includes didactic sessions at the main university, along with procedural training at designated certified hospital centers. Trainees maintain a detailed training log, including all procedures performed, all training sessions attended, and final assessments of competency. The training program in France consists of a two-year program that includes four 20-h seminars, consisting of didactic sessions, practical work in laboratories, and written assessments. In the United Kingdom, interested trainees can attend one of a few 12-month fellowships where additional clinical experience is available, although the curriculum is not standardized and no graduate certificate is granted. The situation in Germany is similar, with interested trainees typically obtaining positions at centers known for interventional pulmonology practice. The British Thoracic Society and the German Society of Pulmonlogy also offer courses in basic and advanced bronchoscopy.
3.3. Post-Graduate Procedure Training
With the continued advances in interventional pulmonary medicine, practitioners need access to training in techniques that are developed, after they complete structured training. In addition, as some procedures, such as percutaneous tracheostomy and whole lung lavage, are not required procedures for training programs, an interventional pulmonologist joining a practice that performs these procedures may not have received training from a fellowship. For newer procedures, including endobronchial valve placement and robotic bronchoscopy, industry-run training programs are available. These programs include online education modules and a day of on-site training, including in-person didactics and simulation, which often use porcine lungs. If a facility does not have any physicians credentialled in the procedure, an outside physician proctor is arranged by the equipment manufacturer.
For procedures where industry-sponsored training is not available, the easiest source of training is a physician in their own practice, if they are available. A physician from another specialty or a physician from another facility can also be found to provide training. Some institutions offer 1- to 3-month mini-fellowships that can be helpful for IP-trained physicians who need additional experience in a particular procedure. Professional societies, such as the American Thoracic Society and American College of Chest Physicians, also offer workshops on advanced pulmonary procedures at their national meetings.
3.4. Current Assessment of Procedure Competency
The ERS/ATS joint statement on interventional pulmonology [5] and the American College of Chest Physicians (ACCP) interventional pulmonary procedure guidelines [6] list suggested minimum procedure numbers for competency in the various procedures that comprise the field of interventional pulmonology. These procedure numbers are based on expert consensus rather than a scientific understanding of skill acquisition. A CHEST expert panel report on adult bronchoscopy training, which was published in 2015, recommends transition from a volume-based certification system to skill acquisition and knowledge-based competency assessment [31]. The AABIP program requirements do not state a set number of procedures required for competency, and certification of competency is instead delegated to program directors and is determined based on direct observation, evaluations, and the tracking of outcomes and complications [3]. While validated assessment tools do not exist for many procedures, the use of such tools is strongly recommended for procedures where they do exist. Table 1 summarizes both current AABIP procedure volume requirements and currently validated assessments and learning curves.

Table 1.
Comparison of Procedure Volumes of Various Societies’ Interventional Pulmonary Procedures.
4. Academic Studies of Skill Acquisition in Interventional Pulmonary Procedures
Procedural training is an essential part of interventional pulmonology training, whose basis lies in good training in basic pulmonary skills during the pulmonary and critical care fellowship. Although procedural volume has been a longstanding metric of procedural competency studies of skill acquisition have shown considerable variability of skill acquisition among trainees, suggesting that raw procedure numbers may be a poor surrogate for procedural competence [32,33]. In acknowledging that the heterogeneity in both trainee skill acquisition and training program experience results in significant variability in graduate procedural competency, a CHEST expert panel report (published in 2015) recommended that professional societies should move from a volume-based certification system to instead emphasize skill acquisition and undertake a knowledge-based competency assessment of trainees [31]. Such a transition requires a validated means of assessing procedural skills and an in-depth understanding of how trainees acquire procedural skills. A body of research on procedural assessment and skill acquisition is now available, which can inform the transition to such a system.
4.1. Academic Studies of Skill Acquisition in Basic Bronchoscopy
Multiple validated tools have been developed to assess competency in basic flexible bronchoscopy, including the Bronchoscopy Skills and Tasks Assessment Tool (BSTAT) [34] and the Ontario Bronchoscopy Assessment Tool (OBAT) [35]. The BSTAT is a 10-item tool that uses multiple responses from each item to test the mechanics of airway inspection, endobronchial biopsy, bronchial brushing, and bronchoalveolar lavage. The tool also includes a quiz based on standardized pictures, and all responses are dichotomous. The OBAT is a 12-item tool used to assess bronchoscopy skills, including pre-procedure planning, technical proficiency, and post-procedure management. Items are graded on a one–five scale.
In a multicenter study [32] of acquisition of basic flexible bronchoscopy skills in pulmonary fellows that used the BSTAT for assessment, a steep learning curve was observed for the first 30 procedures, with smaller but continuous improvements in skills gained between the 30th and 100th procedures. There was variation in skill acquisition between the learners at different time points (10th procedure, 20th, 40th, 60th, etc.). In bronchoscopically naive trainees, those with prior video game-playing experience had higher visual-spatial awareness and fewer airway collisions. However, the impact of video game playing, as a supplement to simulation bronchoscopic education, is still uncertain [36].
In a multicenter study [33] of pulmonary trainees, investigators created learning curves for 31 trainees, using the OBAT for assessment. They found heterogeneity in the learning process, suggesting that some learners take longer to achieve competence than other learners, which was reflected by variation in the learning curve shapes for their learners. For learners in the upper quartiles (i.e., 75th and 95th percentiles), there was a steep upward trajectory during the first 25 bronchoscopies, and performance plateaued by the 50th bronchoscopy. On the other hand, learners in the 10th and 25th percentiles had a much more gradual upslope, with more than 100 bronchoscopies needed before their OBAT scores reached the plateau phase. Fellows who received OBAT scores lower than four by their fiftieth bronchoscopy trended toward the lower performance percentiles; this may be a useful metric in identifying learners who would benefit from additional training.
The effect of simulation-based training on skill acquisition in flexible bronchoscopy has been studied on multiple occasions, as shown by a 2023 systematic review that summarizes these results [37]. Most studies have been of pretest-posttest design, but three small randomized controlled trials have also been performed. Study design has been heterogenous, in both instruction methods and outcome measures. Only two studies measured the ability to apply bronchoscopy skills to actual patients, and no studies evaluated patient-centered outcomes. Even after these limitations are acknowledged and considered, the use of simulation training did show improvements in basic skills. The studies that did show improvement in the application of skills to live patients both gradually increased the task difficulty of their simulation curriculum.
4.2. Academic Studies of Skill Acquisition in Endobronchial Ultrasound
Endobronchial ultrasound with transbronchial needle aspiration (EBUS–TBNA) is currently the standard of care for mediastinal staging of lung cancer. The EBUS–STAT is an assessment tool used to score learners’ EBUS–TBNA skills [38], which is comprised of 10 sections (100 points total), with items 1–7 evaluating technical skills and items 8–10 evaluating CT and EBUS image correlation. Items 1–7 are addressed during the bronchoscopy and include tasks such as maneuvering the scope, identifying structures (vessels, lymph nodes, etc.), obtaining adequate images, and biopsy technique. Items 8–10 are assessed on a computer by reviewing a series of CT and EBUS images. All responses are dichotomized. Scores < 60 denote novice, 60–79 denotes advanced beginner, 80–99 intermediate, and a score of 100 denotes “competent”.
In a EBUS–STAT validation study [38], Davoudi et al. included learners who had previously completed at least 100 basic flexible bronchoscopies, and stratified the learners into three groups, based on the number of EBUSs previously performed: beginner (<20 EBUS, n = 8), intermediate (20–50 EBUS, n = 8), and experienced (>50 EBUS, n = 8). In groups 1 and 2 (<50 total EBUS performed), there was a significant linear association between EBUS–STAT score and # of additional procedures performed. Once learners completed more than 50 EBUS–TBNAs, their score reached a plateau, and further procedures contributed little to their overall assessment score. Beginner and intermediate learners over-estimated their ability; however, expert learners tended to underestimate ability. Even though basic EBUS competencies assessed by EBUS–STAT plateau after the 50th procedure, learners can continue to acquire nuances of the procedure after initial benchmarks have been reached. Indeed, a separate study of ten interventional pulmonology fellows that used time per lymph node station as the primary outcome found continued improvement in performance, even after 200 procedures [39].
Although several studies have used EBUS–TBNA simulators, only two have compared simulation-based training to the traditional apprenticeship model [40]. Stather et al. [41] showed a significant improvement in total procedure time and the percent of lymph nodes correctly identified when simulation training was used; however, the outcomes were measured on a simulator rather than a living patient. Konge et al. [42] showed improved performance among simulator-trained physicians without prior EBUS experience, compared to clinically-trained physicians without prior EBUS experience. The outcomes were measured using live patients; however, the applied clinical assessment tool had not been validated prior to this study.
4.3. Academic Studies of Skill Acquisition in Navigation Bronchoscopy
Electromagnetic navigational bronchoscopy (ENB) is an advanced technology used to navigate peripheral pulmonary nodules. The Learning Electromagnetic Navigation Bronchoscopy and Percutaneous Transthoracic Needle Biopsy (LEAP) tool has been developed and validated in a study of 14 operators that used the Veran ENB platform [43]. The tool has 16 items for ENB and 17 items for ENB transthoracic biopsy that evaluate four domains: 1. Procedural planning; 2. Equipment setup and registration; 3. Navigation to target; and 4. Biopsy performance. Items are scored on a scale of 1–4 BY using the Dreyfus model of learning. As scores are averaged within a domain, the final score ranges from four to sixteen, with competency defined as a score of twelve with a minimum score of three in each domain.
In a study [44] of 26 IP fellows across 16 academic US IP fellowship programs, procedural competency in ENB was assessed by using the Veran ENB platform. Competency was defined as three consecutive procedures with an overall score > twelve and a minimum score of three in each graded domain. The fellows’ first 20 ENB cases were performed, observed and scored, and the video recorded cases were reviewed by two blinded experts. When assessing learning curves for the IP fellows, the number of procedures needed to achieve competency was variable; some fellows in the upper quartile achieved competency within two procedures, while other fellows required more than 12 procedures to gain competency. In this study, 15 ENB procedures would have been sufficient for all fellows to reach the minimum competency threshold. The fellows were followed for 20 consecutive cases and a plateau in skill was observed after they achieved minimum competency.
4.4. Academic Studies of Skill Acquisition in Rigid Bronchoscopy
Rigid bronchoscopy is one of the fundamental therapeutic modalities in interventional pulmonology. On the basis of expert opinion, the combined pulmonology societies recommend a minimum of 20 rigid bronchoscopies should be performed for initial competency [6]. A competency-based assessment tool, known as the Rigid Bronchoscopy Tool for Assessment of Skills and Competence (RIGID–TASC), was created [45], which consists of 23 items with dichotomized responses. The final score ranges from zero to 100. The 23 objectives of the assessment cover multiple aspects of the procedure, including assembling the bronchoscope, protecting the teeth, atraumatically intubating the patient, and maneuvering the bronchoscope in the airway.
In the RIGID–TASC study [45], 30 volunteers with different levels of competency in rigid bronchoscopy were recruited and stratified into three groups: novice (10 PCCM fellows, >50 flexible bronchoscopies, no rigid bronchoscopies), intermediate (mix of IP fellows and PCCM fellows, >50 flexible bronchoscopies, 5–20 rigids), and expert (>100 rigids previously performed). The participants performed rigid bronchoscopy with a 10 mm rigid bronchoscope on a mannequin and used the RIGID–TASC tool to assess the various stages of the procedure. Each operator was evaluated by two separate examiners, and the RIGID–TASC assessment tool was found to have good inter-rater reliability. There was a significant difference in scores between the three groups: mean scores were 58.1, 78.15, and 94.4 in the novice, intermediate, and expert groups, respectively. Validity was demonstrated by the test’s ability to stratify operators on the basis of the novice, intermediate, and expert skill categories.
The learning curve of rigid bronchoscopy has been assessed in a multicenter study [46] of 12 interventional pulmonology fellows. Competency was defined in this study as three consecutive procedures with a RIGID–TASC score of at least 89 and unassisted intubation and navigation of the airways. A total of 178 rigid intubations were performed. Fellows’ skill acquisition was variable, with a range of 5–24 rigid intubations required to achieve competency. The median number of procedures required to achieve competency was 15.
The use of simulation in rigid bronchoscopy has been studied in the setting of foreign body extraction with otolaryngology residents. Hilmi et al. [47] showed in a study of 20 otolaryngology residents that an intensive simulation-based course improved the completion time and skill assessment of foreign body extraction in a standardized porcine model. The assessment was not a standardized tool, and applicability to skills on a live patient was not assessed. Jabbour et al. [48] evaluated a simulation-based psychomotor skills curriculum by using an infant mannequin for 17 otolaryngology residents. Trainee confidence and performance (using an OSATS grading system) improved, but applicability of skills to live patients was not assessed. The use of simulation in other rigid bronchoscopy tasks has not been studied.
4.5. Academic Studies of Skill Acquisition in Medical Thoracoscopy
Medical thoracoscopy is used to visualize the pleural space and obtain tissue samples from the parietal pleural in patients with exudative effusions of unknown etiology. The local anesthetic thoracoscopy (LAT) tool has been recently developed and validated to assess competency in performing medical thoracoscopy [49]. The tool is an eight-item assessment that tests technical skill throughout the procedure, which for the purposes of the assessment is performed on a standardized model. Each item is rated on a scale of 1–5. The validation study included nine novice and eight expert operators. LAT was able to distinguish between novice and expert operators with good inter-observer consistency. The contrasting groups method was used, and the minimum passing score was set at 22. To date, a learning curve study has not been performed using this assessment tool.
The use of simulation in thoracoscopy training has been extensively studied with regard to training thoracic surgeons, with studies showing the utility of cadaver and live animal models, training boxes, and virtual reality simulators [50]. These studies however focus on thoracic surgery tasks, and none evaluate the diagnostic tasks that are necessary in medical thoracoscopy.
4.6. Academic Studies of Skill Acquisition in Other Procedures
To date, validated models have not been developed for other interventional pulmonary procedures [18].
5. Looking to the Future
The current landscape for interventional pulmonology education continues to evolve, and as demand for interventional pulmonary services continues to increase, the training methods and accreditation standards will require ongoing reassessment to ensure that a sufficient number of graduates enter the specialty to meet this demand, without compromising their competency.
5.1. Assessment of Graduate Competency
With a shift towards competency-based evaluation, a validated means of assessing competency will be needed for all procedures that are required of the interventional pulmonologist. In addition, the tools that are available now are certainly imperfect. The scoring systems that are used vary between assessments, and include dichotomized tools (BSTAT, EBUS–STAT, RIGID–TASC), individualized rating scales (OBAT, LAT), and scales based on educational theory (LEAP). This variability of methodology becomes cumbersome for evaluators; and indeed the LEAP investigators note a significant advantage in the use of a global rating scale in their instrument [43].
Currently not enough is known about how to assess competency in interventional pulmonary procedures or about how quickly trainees acquire the skills necessary for more complex procedures to fully utilize this paradigm in interventional pulmonary education. The assessment tools can be used to track trainees’ progress and establish basic competency for procedures, when such tools are available. Trends in these assessments can also be used to give trainees more focused feedback on aspects of these procedures where they show a need for improvement. For procedures where no evaluation tool exists, a case number-based evaluation, supplemented by subjective faculty assessment of competency, is the only available measure at this time. As more validated evaluation tools become available, a more structured means of assessing competency for these procedures can be used.
The 2015 chest expert panel statement [31] mentions the need to link competency assessment to meaningful clinical outcomes, such as diagnostic yield, complication rates, and patient tolerance of the procedure. An outcomes-based approach has been described in plastic surgery education and has been noted to produce positive results [51]. As trainees are required to keep detailed logs of their procedures, periodic review of outcome data with the program director would be feasible and would likely provide useful data regarding procedural competency and areas in need of improvement. As outcome-based data can be gathered retrospectively, evaluation based on such data can be particularly helpful for post-graduate feedback and improvement, as it does not require having an educator at the point of care. The main downside of this approach is that feedback is provided in hindsight, rather than at the point of care. The delay in providing feedback would result in trainees being unable to remember specifics about procedures at the time when feedback is given, which means that outcome-based feedback and assessment will most likely be best used as a complement to, rather than as a replacement for, evaluation and feedback given at the point of care.
One topic that deserves particular mention is the maintenance and refinement of existing skills after graduation from structured training. While recertification requirements can ensure that interventional pulmonologists maintain intellectual competency, there is currently not a standardized process for maintaining and improving technical competency throughout one’s career. The use of detailed procedure logging and regular review of procedure outcomes and complications would seem to be particularly helpful, particularly for practitioners who do not have a supervisor trained in interventional pulmonology. More research of skill maintenance and improvement of skills after graduation would be helpful, and the new AABIP Pulmonary Procedures Registry may be a helpful source of data for such research.
5.2. Improving Interventional Pulmonary Training
The investigation of learning curves for various procedures can further inform necessary procedure volumes for accreditation. While the requirement of adequate procedure volume helps standardize training in interventional pulmonology, excessive requirements can limit the number of training slots available at a time when the field is growing. The Multisociety Interventional Pulmonology Fellowship Accreditation Committee notes that the required procedure volumes do not necessarily seek to ensure appropriate volumes for individual fellows, but instead try to ensure appropriate faculty and staff expertise, in addition to providing a robust training experience for fellows [3]. The effect of institutional procedure volumes on trainee acquisition of skills is an area ripe for future research.
On the basis of learning curve data that are available, we conclude the required procedure volumes for endobronchial ultrasound and navigation are well-aligned with the learning curves for these procedures. Although technical competency in rigid bronchoscopy required 24 cases, well short of the 50 required for fellowship accreditation, the RIGID–TASC assessment does not account for competence in the multiple complex interventions typically performed alongside rigid bronchoscopy. In addition, a common weakness of all evaluation tools is that they do not address the ability to manage the complications of interventional procedures. Given the four percent complication rate of therapeutic bronchoscopy noted in the AQuIRE registry [52], the ability to manage procedural complications is a vital component of procedural competency. More research regarding acquisition of these more complex skills could help to further inform the program accreditation standards.
The AABIP program requirements include requirements for simulation-based training, and the AIPPD fellows’ “boot camp” is a valuable tool for achieving such training early in the year. The optimal role of such training in shifting the learning curves for interventional procedures is an area ripe for research, as is the development of standardized models that improve cost and mitigate ethical concerns regarding the use of animal models. In particular, low-cost models for stent deployment and tissue ablation would be ideal.
6. Conclusions
The development of interventional pulmonology as a distinct subspecialty has been reflected in the growth and maturation of the specialty’s training programs. Training has evolved from a limited number of sites with lack of standardization to 40 accredited training programs with a standardized curriculum and program requirements. Concurrent with the maturation of interventional pulmonary training, validated assessment tools are being actively developed, and the learning curves of common interventional procedures are being described. Further work will include the expansion of competency-based education and evaluation models to ensure that trainees do not only graduate in adequate procedure numbers, but also with true competency in the field.
Funding
This research received no external funding.
Data Availability Statement
No new data was created for this review.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Moore, A.J.; Mercer, R.M.; Musani, A.I. Advances in Interventional Pulmonology. Clin. Chest Med. 2018, 39, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Prakash, U.B.S. The American Association for Bronchology and the Journal of Bronchology. J. Bronchol. Interv. Pulmonol. 1994, 1, 1. [Google Scholar] [CrossRef]
- Mullon, J.J.; Burkart, K.M.; Silvestri, G.; Hogarth, D.K.; Almeida, F.; Berkowitz, D.; Eapen, G.A.; Feller-Kopman, D.; Fessler, H.E.; Folch, E.; et al. Interventional Pulmonology Fellowship Accreditation Standards: Executive Summary of the Multisociety Interventional Pulmonology Fellowship Accreditation Committee. Chest 2017, 151, 1114–1121. [Google Scholar] [CrossRef] [PubMed]
- Silvestri, G.A. Looking to Our Past to Find the Way Forward for the American Association of Bronchology and Interventional Pulmonology. J. Bronchol. Interv. Pulmonol. 2010, 17, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Bolliger, C.T.; Mathur, P.N.; Beamis, J.F.; Becker, H.D.; Cavaliere, S.; Colt, H.; Diaz-Jimenez, J.P.; Dumon, J.F.; Edell, E.; Kovitz, K.L.; et al. ERS/ATS Statement on Interventional Pulmonology. European Respiratory Society/American Thoracic Society. Eur. Respir. J. 2002, 19, 356–373. [Google Scholar] [PubMed]
- Ernst, A.; Silvestri, G.A.; Johnstone, D. Interventional Pulmonary Procedures: Guidelines from the American College of Chest Physicians. Chest 2003, 123, 1693–1694. [Google Scholar] [CrossRef] [PubMed]
- Long, D.M. Competency-Based Residency Training: The Next Advance in Graduate Medical Education. Acad. Med. 2000, 75, 1178–1183. [Google Scholar] [CrossRef]
- Panchabhai, T.S.; Mehta, A.C. Historical Perspectives of Bronchoscopy. Connecting the Dots. Ann. Am. Thorac. Soc. 2015, 12, 631–641. [Google Scholar] [CrossRef]
- Jackson, C. Tracheo-Bronchoscopy, Esophagoscopy and Gastroscopy; The Laryngoscope Company: St. Louis, MO, USA, 1907. [Google Scholar]
- Hürter, T.; Hanrath, P. Endobronchial Sonography: Feasibility and Preliminary Results. Thorax 1992, 47, 565–567. [Google Scholar] [CrossRef]
- Yasufuku, K.; Chiyo, M.; Sekine, Y.; Chhajed, P.N.; Shibuya, K.; Iizasa, T.; Fujisawa, T. Real-Time Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration of Mediastinal and Hilar Lymph Nodes. Chest 2004, 126, 122–128. [Google Scholar] [CrossRef]
- Schwarz, Y.; Greif, J.; Becker, H.D.; Ernst, A.; Mehta, A. Real-Time Electromagnetic Navigation Bronchoscopy to Peripheral Lung Lesions Using Overlaid CT Images: The First Human Study. Chest 2006, 129, 988–994. [Google Scholar] [CrossRef] [PubMed]
- Loddenkemper, R.; Mathur, P.N.; Lee, P.; Noppen, M. History and Clinical Use of Thoracoscopy/Pleuroscopy in Respiratory Medicine. Breathe 2011, 8, 144–155. [Google Scholar] [CrossRef]
- Leff, R.S.; Eisenberg, B.; Baisden, C.E.; Mosley, K.R.; Messerschmidt, G.L. Drainage of Recurrent Pleural Effusion via an Implanted Port and Intrapleural Catheter. Ann. Intern. Med. 1986, 104, 208–209. [Google Scholar] [CrossRef] [PubMed]
- US Food and Drug Administration Summary of Safety and Effectiveness, Denver PLEURX Pleural Catheter Kit, Denver PLEURX Home Drainage Kit. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf/K971753.pdf (accessed on 27 December 2023).
- Pastis, N.J.; Nietert, P.J.; Silvestri, G.A. Variation in Training for Interventional Pulmonary Procedures Among US Pulmonary/Critical Care Fellowships: A Survey of Fellowship Directors. Chest 2005, 127, 1614–1621. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.J.; Mudambi, L.; Vial, M.R.; Hernandez, M.; Eapen, G.A. Evaluation of Appropriate Mediastinal Staging among Endobronchial Ultrasound Bronchoscopists. Ann. Am. Thorac. Soc. 2017, 14, 1162–1168. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Akulian, J.A.; Argento, A.C.; Batra, H.; Lamb, C.; Mullon, J.; Murgu, S. Interventional Pulmonary Fellowship Training: End of the Beginning. ATS Sch. 2023, 4, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Feller-Kopman, D.; Mehta, A.C. Special Announcement: Interventional Pulmonology Match. J. Bronchol. Interv. Pulmonol. 2011, 18, 377. [Google Scholar] [CrossRef]
- Lee, H.J.; Feller-Kopman, D.; Shepherd, R.W.; Almeida, F.A.; Bechara, R.; Berkowitz, D.; Chawla, M.; Folch, E.; Haas, A.; Gillespie, C.; et al. Validation of an Interventional Pulmonary Examination. Chest 2013, 143, 1667–1670. [Google Scholar] [CrossRef]
- Yarmus, L.; Feller-Kopman, D.; Imad, M.; Kim, S.; Lee, H.J. Procedural Volume and Structure of Interventional Pulmonary Fellowships: A Survey of Fellows and Fellowship Program Directors. Chest 2013, 144, 935–939. [Google Scholar] [CrossRef]
- Lamb, C.R.; Feller-Kopman, D.; Ernst, A.; Simoff, M.J.; Sterman, D.H.; Wahidi, M.M.; Kovitz, K.L. An Approach to Interventional Pulmonary Fellowship Training. Chest 2010, 137, 195–199. [Google Scholar] [CrossRef][Green Version]
- Wahidi, M.M. Interventional Pulmonology: Marching Forward Together. J. Bronchol. Interv. Pulmonol. 2016, 23, 87–88. [Google Scholar] [CrossRef] [PubMed]
- IP Board Eligibility Criteria. Available online: https://www.aabronchology.org/ip-board-eligibility-criteria-09-2022 (accessed on 11 April 2023).
- IP Fellowship Program Contact Information. Available online: https://aabip.memberclicks.net/ip-fellowship-program-contact-information (accessed on 11 April 2023).
- Accreditation Council for Graduate Medical Education Program Applications. Available online: https://www.acgme.org/programs-and-institutions/programs/program-application-information/ (accessed on 27 December 2023).
- American Association for Bronchology and Interventional Pulmonology 2023 IP Fellows Boot Camp. Available online: https://www.aabronchology.org/2023-ip-fellows-bootcamp (accessed on 28 December 2023).
- Lee, H.J.; Feller-Kopman, D.; Islam, S.; Majid, A.; Yarmus, L. Analysis of Employment Data for Interventional Pulmonary Fellowship Graduates. Ann. Am. Thorac. Soc. 2014, 12, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Corbetta, L. Training in Interventional Pulmonology: The European and US Perspective. Eur. Respir. Rev. 2021, 30, 200025. [Google Scholar] [CrossRef]
- Corbetta, L.; Arru, L.B.; Mereu, C.; Pasini, V.; Patelli, M. Competence and Training in Interventional Pulmonology. Panminerva Med. 2019, 61, 203–231. [Google Scholar] [CrossRef] [PubMed]
- Ernst, A.; Wahidi, M.M.; Read, C.A.; Buckley, J.D.; Addrizzo-Harris, D.J.; Shah, P.L.; Herth, F.J.F.; de Hoyos Parra, A.; Ornelas, J.; Yarmus, L.; et al. Adult Bronchoscopy Training: Current State and Suggestions for the Future: CHEST Expert Panel Report. Chest 2015, 148, 321–332. [Google Scholar] [CrossRef] [PubMed]
- Wahidi, M.M.; Silvestri, G.A.; Coakley, R.D.; Ferguson, J.S.; Shepherd, R.W.; Moses, L.; Conforti, J.; Que, L.G.; Anstrom, K.J.; McGuire, F.; et al. A Prospective Multicenter Study of Competency Metrics and Educational Interventions in the Learning of Bronchoscopy Among New Pulmonary Fellows. Chest 2010, 137, 1040–1049. [Google Scholar] [CrossRef]
- Voduc, N.; Adamson, R.; Kashgari, A.; Fenton, M.; Porhownick, N.; Wojnar, M.; Sharma, K.; Gillson, A.-M.; Chung, C.; McConnell, M. Development of Learning Curves for Bronchoscopy: Results of a Multicenter Study of Pulmonary Trainees. Chest 2020, 158, 2485–2492. [Google Scholar] [CrossRef]
- Davoudi, M.; Osann, K.; Colt, H.G. Validation of Two Instruments to Assess Technical Bronchoscopic Skill Using Virtual Reality Simulation. Respiration 2008, 76, 92–101. [Google Scholar] [CrossRef]
- Voduc, N.; Dudek, N.; Parker, C.M.; Sharma, K.B.; Wood, T.J. Development and Validation of a Bronchoscopy Competence Assessment Tool in a Clinical Setting. Ann. Am. Thorac. Soc. 2016, 13, 495–501. [Google Scholar] [CrossRef]
- Mallow, C.; Shafiq, M.; Thiboutot, J.; Yu, D.H.; Batra, H.; Lunz, D.; Feller-Kopman, D.J.; Yarmus, L.B.; Lee, H.J. Impact of Video Game Cross-Training on Learning Bronchoscopy. A Pilot Randomized Controlled Trial. ATS Sch. 2020, 1, 134–144. [Google Scholar] [CrossRef]
- Gerretsen, E.C.F.; Chen, A.; Annema, J.T.; Groenier, M.; van der Heijden, E.H.F.M.; van Mook, W.N.K.A.; Smeenk, F.W.J.M. Effectiveness of Flexible Bronchoscopy Simulation-Based Training: A Systematic Review. Chest 2023, 164, 952–962. [Google Scholar] [CrossRef] [PubMed]
- Davoudi, M.; Colt, H.G.; Osann, K.E.; Lamb, C.R.; Mullon, J.J. Endobronchial Ultrasound Skills and Tasks Assessment Tool: Assessing the Validity Evidence for a Test of Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration Operator Skill. Am. J. Respir. Crit. Care Med. 2012, 186, 773–779. [Google Scholar] [CrossRef] [PubMed]
- Stather, D.R.; Chee, A.; MacEachern, P.; Dumoulin, E.; Hergott, C.A.; Gelberg, J.; Folch, E.; Majid, A.; Gonzalez, A.V.; Tremblay, A. Endobronchial Ultrasound Learning Curve in Interventional Pulmonary Fellows. Respirology 2015, 20, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Naur, T.M.H.; Nilsson, P.M.; Pietersen, P.I.; Clementsen, P.F.; Konge, L. Simulation-Based Training in Flexible Bronchoscopy and Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration (EBUS-TBNA): A Systematic Review. Respiration 2017, 93, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Stather, D.R.; Maceachern, P.; Rimmer, K.; Hergott, C.A.; Tremblay, A. Assessment and Learning Curve Evaluation of Endobronchial Ultrasound Skills Following Simulation and Clinical Training. Respirology 2011, 16, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Konge, L.; Clementsen, P.F.; Ringsted, C.; Minddal, V.; Larsen, K.R.; Annema, J.T. Simulator Training for Endobronchial Ultrasound: A Randomised Controlled Trial. Eur. Respir. J. 2015, 46, 1140–1149. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Lerner, A.D.; Coleman, B.; Semaan, R.; Mallow, C.; Arias, S.; Salwen, B.; Feller-Kopman, D.; Yarmus, L. Learning Electromagnetic Navigational Bronchoscopy and Percutaneous Transthoracic Needle Biopsy (LEAP): A Pilot Study. J. Bronchol. Interv. Pulmonol. 2019, 26, 55–61. [Google Scholar] [CrossRef]
- Lee, H.J.; Argento, A.C.; Batra, H.; Benzaquen, S.; Bramley, K.; Chambers, D.; Desai, N.; Dincer, H.E.; Ferguson, J.S.; Kalanjeri, S.; et al. A Multicenter Study Assessing Interventional Pulmonary Fellow Competency in Electromagnetic Navigation Bronchoscopy. ATS Sch. 2022, 3, 220–228. [Google Scholar] [CrossRef]
- Mahmood, K.; Wahidi, M.M.; Osann, K.E.; Coles, K.; Shofer, S.L.; Volker, E.E.; Davoudi, M. Development of a Tool to Assess Basic Competency in the Performance of Rigid Bronchoscopy. Ann. Am. Thorac. Soc. 2016, 13, 502–511. [Google Scholar] [CrossRef]
- Mahmood, K.; Wahidi, M.M.; Shepherd, R.W.; Argento, A.C.; Yarmus, L.B.; Lee, H.; Shojaee, S.; Berkowitz, D.M.; Van Nostrand, K.; Lamb, C.R.; et al. Variable Learning Curve of Basic Rigid Bronchoscopy in Trainees. Respiration 2021, 100, 530–537. [Google Scholar] [CrossRef]
- Hilmi, O.J.; White, P.S.; Mcgurty, D.W.; Oluwole, M. Bronchoscopy Training: Is Simulated Surgery Effective? Clin. Otolaryngol. Allied Sci. 2002, 27, 267–269. [Google Scholar] [CrossRef]
- Jabbour, N.; Reihsen, T.; Sweet, R.M.; Sidman, J.D. Psychomotor Skills Training in Pediatric Airway Endoscopy Simulation. Otolaryngol. Head. Neck Surg. 2011, 145, 43–50. [Google Scholar] [CrossRef]
- Nayahangan, L.J.; Svendsen, M.B.S.; Bodtger, U.; Rahman, N.; Maskell, N.; Sidhu, J.S.; Lawaetz, J.; Clementsen, P.F.; Konge, L. Assessment of Competence in Local Anaesthetic Thoracoscopy: Development and Validity Investigation of a New Assessment Tool. J. Thorac. Dis. 2021, 13, 3998–4007. [Google Scholar] [CrossRef]
- Grossi, S.; Cattoni, M.; Rotolo, N.; Imperatori, A. Video-Assisted Thoracoscopic Surgery Simulation and Training: A Comprehensive Literature Review. BMC Med. Educ. 2023, 23, 535. [Google Scholar] [CrossRef]
- Halani, S.H.; Cho, M.-J.; Garibay, M.; Nevin, J.; Zhang, A.Y. Improving Plastic Surgery Resident Education and Quality of Care with Outcomes Feedback Using the Surgery Report Card: An Initial Experience. J. Plast. Reconstruc. Aesthet. Surg. 2020, 73, 1338–1347. [Google Scholar] [CrossRef]
- Ost, D.E.; Ernst, A.; Grosu, H.B.; Lei, X.; Diaz-Mendoza, J.; Slade, M.; Gildea, T.R.; Machuzak, M.; Jimenez, C.A.; Toth, J.; et al. Complications Following Therapeutic Bronchoscopy for Malignant Central Airway Obstruction: Results of the AQuIRE Registry. Chest 2015, 148, 450–471. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).