Effectiveness of an Educational Intervention on Inhaler Technique Proficiency in Chronic Obstructive Pulmonary Disease: A Single-Center Quality Improvement Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Definition
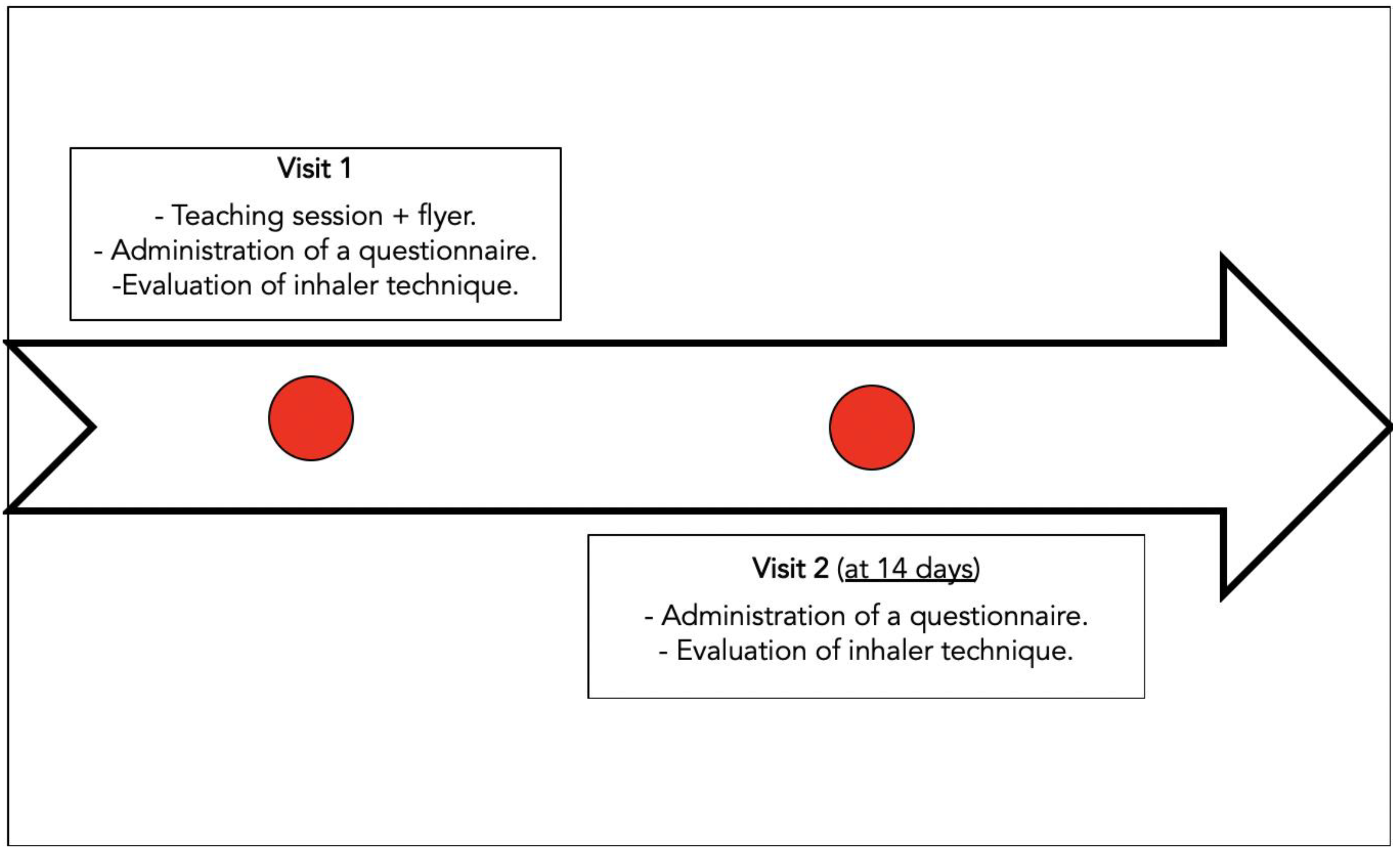
2.2. Participants and Study Design
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Blanco, I.; Diego, I.; Bueno, P.; Casas-Maldonado, F.; Miravitlles, M. Geographic distribution of COPD prevalence in the world displayed by Geographic Information System maps. Eur. Respir. J. 2019, 54, 1900610. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 16 February 2022).
- O’Donnell, D.E.; Parker, C.M. COPD exacerbations. 3: Pathophysiology. Thorax 2006, 61, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Wedzicha, J.A.; Seemungal, T.A. COPD exacerbations: Defining their cause and prevention. Lancet 2007, 370, 786–796. [Google Scholar] [CrossRef]
- Donaldson, G.C.; Seemungal, T.A.; Bhowmik, A.; Wedzicha, J.A. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2002, 57, 847–852, Erratum in: Thorax 2008, 63, 753. [Google Scholar] [CrossRef]
- The Global Initiative for Chronic Obstructive Lung Diseases (GOLD). Global Strategy for Prevention, Diagnosis and Management of COPD: 2022 Report. Available online: https://goldcopd.org/2022-gold-reports-2/ (accessed on 8 June 2022).
- Melani, A.S.; Bonavia, M.; Cilenti, V.; Cinti, C.; Lodi, M.; Martucci, P.; Serra, M.; Scichilone, N.; Sestini, P.; Aliani, M.; et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir. Med. 2011, 105, 930–938, Erratum in: Respir. Med. 2012, 106, 757. [Google Scholar] [CrossRef] [PubMed]
- Lavorini, F.; Magnan, A.; Dubus, J.C.; Voshaar, T.; Corbetta, L.; Broeders, M.; Dekhuijzen, R.; Sanchis, J.; Viejo, J.L.; Barnes, P.; et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir. Med. 2008, 102, 593–604. [Google Scholar] [CrossRef] [PubMed]
- Molimard, M.; Raherison, C.; Lignot, S.; Balestra, A.; Lamarque, S.; Chartier, A.; Droz-Perroteau, C.; Lassalle, R.; Moore, N.; Girodet, P.O. Chronic obstructive pulmonary disease exacerbation and inhaler device handling: Real-life assessment of 2935 patients. Eur. Respir. J. 2017, 49, 1601794. [Google Scholar] [CrossRef] [PubMed]
- Navaie, M.; Dembek, C.; Cho-Reyes, S.; Yeh, K.; Celli, B.R. Device use errors with soft mist inhalers: A global systematic literature review and meta-analysis. Chron Respir. Dis. 2020, 17, 1479973119901234. [Google Scholar] [CrossRef] [PubMed]
- Vanoverschelde, A.; van der Wel, P.; Putman, B.; Lahousse, L. Determinants of poor inhaler technique and poor therapy adherence in obstructive lung diseases: A cross-sectional study in community pharmacies. BMJ Open Respir. Res. 2021, 8, e000823. [Google Scholar] [CrossRef]
- Quanjer, P.H.; Stanojevic, S.; Cole, T.J.; Baur, X.; Hall, G.L.; Culver, B.H.; Enright, P.L.; Hankinson, J.L.; Ip, M.S.; Zheng, J.; et al. ERS Global Lung Function Initiative. Multi-ethnic reference values for spirometry for the 3-95-yr age range: The global lung function 2012 equations. Eur. Respir. J. 2012, 40, 1324–1343. [Google Scholar] [CrossRef]
- Etchells, E.; Ho, M.; Shojania, K.G. Value of small sample sizes in rapid-cycle quality improvement projects. BMJ Qual. Saf. 2016, 25, 202–206. [Google Scholar] [CrossRef]
- Sanchis, J.; Gich, I.; Pedersen, S. Aerosol Drug Management Improvement Team (ADMIT). Systematic Review of Errors in Inhaler Use: Has Patient Technique Improved Over Time? Chest 2016, 150, 394–406. [Google Scholar] [CrossRef]
- Giraud, V.; Roche, N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur. Respir. J. 2002, 19, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Roggeri, A.; Micheletto, C.; Roggeri, D.P. Inhalation errors due to device switch in patients with chronic obstructive pulmonary disease and asthma: Critical health and economic issues. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 597–602. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brocklebank, D.; Ram, F.; Wright, J.; Barry, P.; Cates, C.; Davies, L.; Douglas, G.; Muers, M.; Smith, D.; White, J. Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: A systematic review of the literature. Health Technol. Assess. 2001, 5, 1–149. [Google Scholar] [CrossRef]
- Dolovich, M.B.; Ahrens, R.C.; Hess, D.R.; Anderson, P.; Dhand, R.; Rau, J.L.; Smaldone, G.C.; Guyatt, G. Device selection and outcomes of aerosol therapy: Evidence-based guidelines: American college of chest physicians/american college of asthma, allergy, and immunology. Chest 2005, 127, 335–371. [Google Scholar] [CrossRef] [PubMed]
- Kesten, S.; Elias, M.; Cartier, A.; Chapman, K.R. Patient handling of a multidose dry powder inhalation device for albuterol. Chest 1994, 105, 1077–1081. [Google Scholar] [CrossRef]
- Axtell, S.; Haines, S.; Fairclough, J. Effectiveness of Various Methods of Teaching Proper Inhaler Technique. J. Pharm. Pract. 2017, 30, 195–201. [Google Scholar] [CrossRef]
- Dabrowska, M.; Luczak-Wozniak, K.; Miszczuk, M.; Domagala, I.; Lubanski, W.; Leszczynski, A.; Maskey-Warzechowska, M.; Rubinsztajn, R.; Hermanowicz-Salamon, J.; Krenke, R. Impact of a Single Session of Inhalation Technique Training on Inhalation Skills and the Course of Asthma and COPD. Respir. Care 2019, 64, 1250–1260. [Google Scholar] [CrossRef]
- Park, H.J.; Byun, M.K.; Kwon, J.W.; Kim, W.K.; Nahm, D.H.; Lee, M.G.; Lee, S.P.; Lee, S.Y.; Lee, J.H.; Jeong, Y.Y.; et al. Video education versus face-to-face education on inhaler technique for patients with well-controlled or partly-controlled asthma: A phase IV, open-label, non-inferiority, multicenter, randomized, controlled trial. PLoS ONE 2018, 13, e0197358. [Google Scholar] [CrossRef]
- Normansell, R.; Kew, K.M.; Mathioudakis, A.G. Interventions to improve inhaler technique for people with asthma. Cochrane Database Syst. Rev. 2017, 3, CD012286. [Google Scholar] [CrossRef] [PubMed]
- Klijn, S.L.; Hiligsmann, M.; Evers, S.M.A.A.; Román-Rodríguez, M.; van der Molen, T.; van Boven, J.F.M. Effectiveness and success factors of educational inhaler technique interventions in asthma & COPD patients: A systematic review. NPJ Prim. Care Respir. Med. 2017, 27, 24. [Google Scholar] [CrossRef] [PubMed]
- Maricoto, T.; Monteiro, L.; Gama, J.M.R.; Correia-de-Sousa, J.; Taborda-Barata, L. Inhaler Technique Education and Exacerbation Risk in Older Adults with Asthma or Chronic Obstructive Pulmonary Disease: A Meta-Analysis. J. Am. Geriatr. Soc. 2019, 67, 57–66. [Google Scholar] [CrossRef] [PubMed]
| Questionnaire Visit 1 | n (%) |
|---|---|
| Number of patients | 30 (100.00) |
| Age | |
| ≤50 | 1 (3.33) |
| 51–60 | 5 (16.67) |
| 61–70 | 6 (20.00) |
| 71–80 | 15 (50.00) |
| 81–90 | 3 (10.00) |
| Sex | |
| Female | 19 (63.33) |
| Male | 11 (36.67) |
| Year COPD was diagnosed | |
| 2007 | 1 (3.33) |
| 2015 | 1 (3.33) |
| 2016 | 2 (6.67) |
| 2017 | 6 (20.00) |
| 2018 | 9 (30.00) |
| 2019 | 11 (36.67) |
| GOLD stage | |
| 1 | 3 (10.00) |
| 2 | 20 (66.66) |
| 3 | 7 (23.33) |
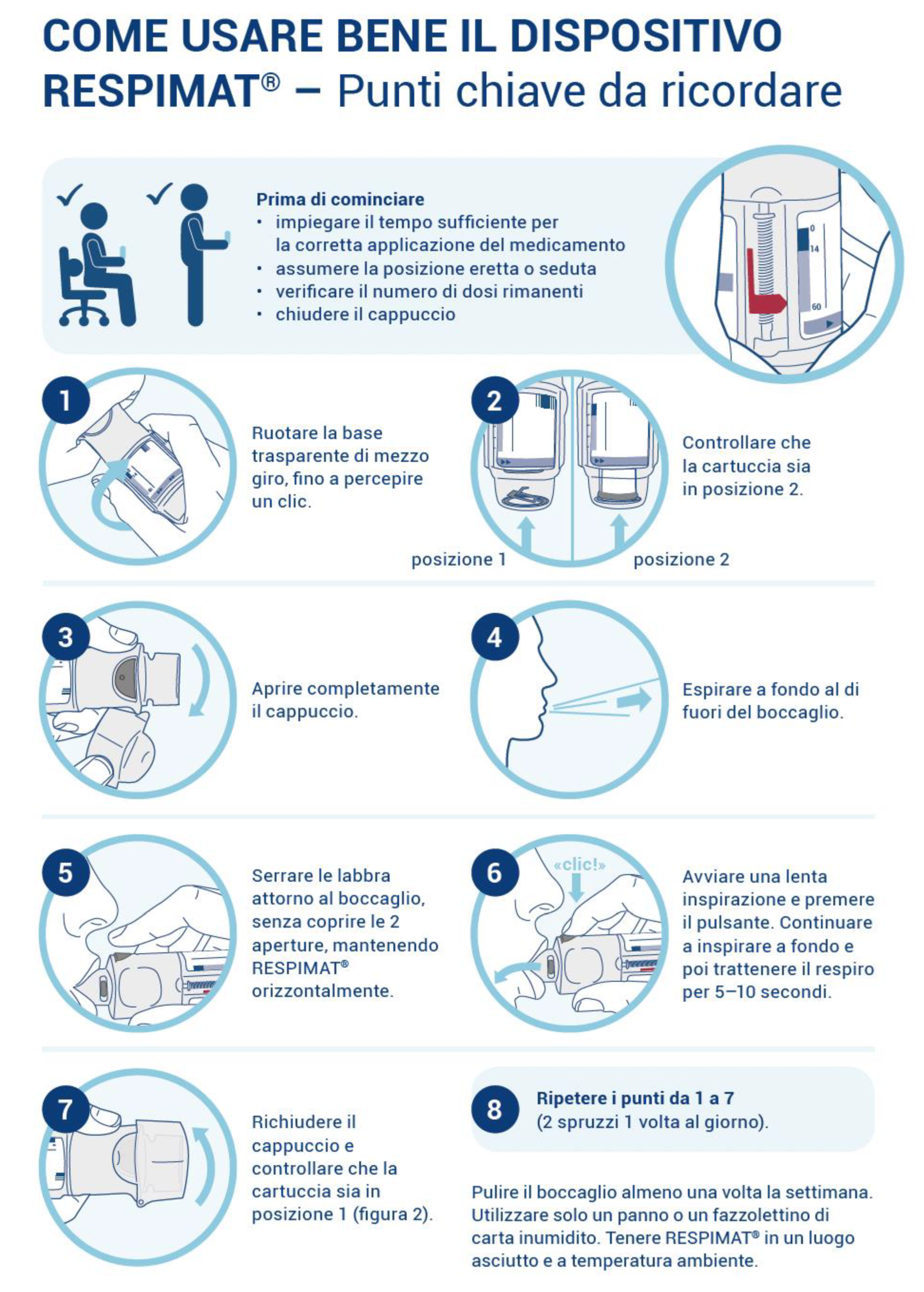
| Was the explanation with the flyer successful? | |
| Yes | 30 (100.00) |
| Did the patients ask questions? | |
| Yes | 22 (73.33) |
| No | 8 (26.37) |
| If yes: at which step | |
| 1 | 6 (27.27) |
| 2 | 11 (50) |
| 3 | 6 (27.27) |
| 4 | 6 (27.27) |
| 5 | 3 (13.63) |
| 6 | 5 (22.72) |
| 7 | 3 (13.63) |
| 8 | 2 (9.1) |
| Did the Patient follow each step in the flyer instructions? | |
| Yes | 24 (80.00) |
| No | 5 (16.67) |
| Missing | 1 (3.33) |
| If not: which step(s) should be better explained in the flyer? | |
| 2 | 2 (6.66) |
| 3 | 1 (3.33) |
| 4 | 1 (3.33) |
| 6 | 2 (6.66) |
| 8 | 1 (3.33) |
| Was the use of the diary explained? | |
| Yes | 29 (96.67) |
| No | 1 (3.33) |
| Questionnaire Visit 1 | n (%) |
|---|---|
| Number of patients | 30 (100.00) |
| Did the patient use the diary? | |
| Yes | 29 (96.67) |
| No | 1 (3.33) |
| Patient Evaluation of the flyer (Scale 1–6 = very bad to very good) | |
| ≤4 | 3 (10.00) |
| 5 | 6 (20.00) |
| 6 | 21 (70.00) |
| Did the patient follow each step in the flyer instructions for the Respimat®? | |
| Yes | 25 (83.33) |
| No | 4 (13.33) |
| missing | 1 (3.33) |
| If not: which step(s) should be better explained in the flyer | |
| Before | 1 (3.33) |
| 1 | 1 (3.33) |
| 2 | 1 (3.33) |
| 4 | 2 (6.66) |
| 5 | 1 (3.33) |
| 6 | 2 (6.66) |
| Has the last page (Preparation of Respimat®) been shown to the patient, and did he understand it? | |
| Yes | 29 (96.67) |
| No | 1 (3.33) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marando, M.; Tamburello, A.; Diedrich, J.P.; Valenti, A.; Gianella, P. Effectiveness of an Educational Intervention on Inhaler Technique Proficiency in Chronic Obstructive Pulmonary Disease: A Single-Center Quality Improvement Study. J. Respir. 2022, 2, 139-146. https://doi.org/10.3390/jor2030012
Marando M, Tamburello A, Diedrich JP, Valenti A, Gianella P. Effectiveness of an Educational Intervention on Inhaler Technique Proficiency in Chronic Obstructive Pulmonary Disease: A Single-Center Quality Improvement Study. Journal of Respiration. 2022; 2(3):139-146. https://doi.org/10.3390/jor2030012
Chicago/Turabian StyleMarando, Marco, Adriana Tamburello, Jens P. Diedrich, Antonio Valenti, and Pietro Gianella. 2022. "Effectiveness of an Educational Intervention on Inhaler Technique Proficiency in Chronic Obstructive Pulmonary Disease: A Single-Center Quality Improvement Study" Journal of Respiration 2, no. 3: 139-146. https://doi.org/10.3390/jor2030012
APA StyleMarando, M., Tamburello, A., Diedrich, J. P., Valenti, A., & Gianella, P. (2022). Effectiveness of an Educational Intervention on Inhaler Technique Proficiency in Chronic Obstructive Pulmonary Disease: A Single-Center Quality Improvement Study. Journal of Respiration, 2(3), 139-146. https://doi.org/10.3390/jor2030012






