Risk Factors for Hypertension in Hospitalised Patient Mortality with Laboratory-Confirmed SARS-CoV-2: A Population-Based Study in Limpopo Province, South Africa
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting, Period and Design
2.2. Statistical Analysis
2.3. Data Collection and Validation
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Covid19.who.int. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 28 January 2022).
- Atalan, A. Is the lockdown important to prevent the COVID-19 pandemic? Effects on psychology, environment and economy-perspective. Ann. Med. Surg. 2020, 56, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Al-Samarrai, S.; Gangwar, M.; Gala, P. The Impact of the COVID-19 Pandemic on Education Financing; World Bank Group: Washington, DC, USA, 2020. [Google Scholar]
- Mahaye, N.E. The Impact of COVID-19 Pandemic on Education: Navigating Forward the Pedagogy of Blended Learning; Research Online: 2020.
- Reuters. South Africa: The Latest Coronavirus Counts, Charts and Maps. Available online: https://graphics.reuters.com/world-coronavirus-tracker-and-maps/countries-and-territories/south-africa/ (accessed on 28 January 2022).
- Tian, S.; Hu, N.; Lou, J.; Chen, K.; Kang, X.; Xiang, Z.; Chen, H.; Wang, D.; Liu, N.; Liu, D.; et al. Characteristics of COVID-19 infection in Beijing. J. Infect. 2020, 80, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Çalıca Utku, A.; Budak, G.; Karabay, O.; Güçlü, E.; Okan, H.D.; Vatan, A. Main symptoms in patients presenting in the COVID-19 period. Scott. Med. J. 2020, 65, 127–132. [Google Scholar] [CrossRef]
- Wan, S.; Xiang, Y.; Fang, W.; Zheng, Y.; Li, B.; Hu, Y.; Lang, C.; Huang, D.; Sun, Q.; Xiong, Y.; et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J. Med. Virol. 2020, 92, 797–806. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 Significantly Impacts Health Services for Noncommunicable Diseases. Available online: https://www.who.int/news/item/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases (accessed on 31 January 2022).
- Swamy, S.; Koch, C.A.; Hannah-Shmouni, F.; Schiffrin, E.L.; Klubo-Gwiezdzinska, J.; Gubbi, S. Hypertension and COVID-19: Updates from the era of vaccines and variants. J. Clin. Transl. Endocrinol. 2021, 27, 100285. [Google Scholar] [CrossRef] [PubMed]
- Hosseinzadeh, R.; Goharrizi, M.A.S.B.; Bahardoust, M.; Alvanegh, A.G.; Ataee, M.R.; Bagheri, M.; Navidiyan, E.S.; Zijoud, S.R.H.; Heiat, M. Should all patients with hypertension be worried about developing severe coronavirus disease 2019 (COVID-19)? Clin. Hypertens. 2021, 27, 3. [Google Scholar] [CrossRef]
- Tshitangano, T.G.; Setati, M.E.; Mphekgwana, P.M.; Ramalivhana, N.J.; Matlala, S.F. Epidemiological Characteristics of COVID-19 Inpatient Deaths during the First and Second Waves in Limpopo Province, South Africa. J. Respir. 2022, 2, 111–122. [Google Scholar] [CrossRef]
- Wu, J.; Li, W.; Shi, X.; Chen, Z.; Jiang, B.; Liu, J.; Wang, D.; Liu, C.; Meng, Y.; Cui, L.; et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J. Int. Med. 2020, 288, 128–138. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Qu, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. China medical treatment expert group for COVID-19 2020. Clinical Characteristics of coronavirus disease in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Jassat, W.; Cohen, C.; Masha, M.; Tempia, S.; Goldstein, S.; Kufa, T.; Murangandi, P.; Savulescu, D.; Walaza, S.; Bamet, J.-L.; et al. COVID-19 in-hospital mortality in South Africa: The intersection of communicable and non-communicable chronic diseases in a high HIV prevalence setting. medRxiv 2020. [Google Scholar] [CrossRef]
- Nicd.ac.za. Available online: https://www.nicd.ac.za/wp-content/uploads/2020/05/Clinical-management-of-suspected-or-confirmed-COVID-19-Version-4.pdf (accessed on 1 February 2022).
- Zhong, L.; Wu, Y.; Gao, J.; Zhang, J.; Xie, Q.; He, H.; Ji, J.; Liu, Z.; Wang, C.; Liu, Z. Effects of hyper-tension on the outcomes of COVID-19: A multicentre retrospective cohort study. Ann. Med. 2021, 53, 770–776. [Google Scholar] [CrossRef]
- Ruan, Q.; Yang, K.; Wang, W.; Jiang, L.; Song, J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020, 46, 846–848. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Yang, X.L.; Wang, X.G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.R.; Zhu, Y.; Li, B.; Huang, C.L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Hamming, I.; Timens, W.; Bulthuis, M.L.C.; Lely, A.T.; Navis, G.V.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004, 203, 631–637. [Google Scholar] [CrossRef]
- Xu, Y.; Chen, X.; Wang, K. Global prevalence of hypertension among people living with HIV: A systematic review and meta-analysis. J. Am. Soc. Hypertens. 2017, 11, 530–540. [Google Scholar] [CrossRef]
- Barrera, F.J.; Shekhar, S.; Wurth, R.; Pena, P.J.M.; Ponce, O.J.; Hajdenberg, M.; A Alvarez-Villalobos, N.; E Hall, J.; Schiffrin, E.L.; Eisenhofer, G.; et al. Prevalence of Diabetes and Hypertension and Their Associated Risks for Poor Outcomes in Covid-19 Patients. J. Endocr. Soc. 2020, 4, bvaa102. [Google Scholar] [CrossRef] [PubMed]
- Drain, P.K.; Hong, T.; Hajat, A.; Krows, M.; Govere, S.; Thulare, H.; Moosa, M.Y.S.; Bassett, I.; Celum, C. Integrating hypertension screening at the time of voluntary HIV testing among adults in South Africa. PLoS ONE 2019, 14, e0210161. [Google Scholar] [CrossRef] [PubMed]
- Mphekgwana, P.M.; Malema, N.; Monyeki, K.D.; Mothiba, T.M.; Makgahlela, M.; Kgatla, N.; Makgato, I.; Sodi, T. Hypertension Prevalence and Determinants among Black South African Adults in Semi-Urban and Rural Areas. Int. J. Environ. Res. Public Health 2020, 17, 7463. [Google Scholar] [CrossRef]
- Akalu, Y.; Belsti, Y. Hypertension and its associated factors among type 2 diabetes mellitus patients at Debre Tabor general hospital, northwest Ethiopia. Diabetes Metab. Syndr. Obes. Targets Ther. 2020, 13, 1621. [Google Scholar] [CrossRef]
- Shukuri, A.; Tewelde, T.; Shaweno, T. Prevalence of old age hypertension and associated factors among older adults in rural Ethiopia. Integr. Blood Press. Control 2019, 12, 23. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.H.; Lee, H.S. Hypertension and diabetes mellitus as risk factors for asthma in Korean adults: The Sixth Korea National Health and Nutrition Examination Survey. Int. Health 2019, 12, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Xu, J.; Yang, X. Asthma and risk of cardiovascular disease or all-cause mortality: A meta-analysis. Ann. Saudi Med. 2017, 37, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Seegert, A.B.; Rudolf, F.; Wejse, C.; Neupane, D. Tuberculosis and hypertension—A systematic review of the literature. Int. J. Infect. Dis. 2017, 56, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Seretis, A.; Cividini, S.; Markozannes, G.; Tseretopoulou, X.; Lopez, D.S.; Ntzani, E.E.; Tsilidis, K.K. Association between blood pressure and risk of cancer development: A systematic review and meta-analysis of observational studies. Sci. Rep. 2019, 9, 8565. [Google Scholar] [CrossRef]
- Leggio, M.; Lombardi, M.; Caldarone, E.; Severi, P.; D’Emidio, S.; Armeni, M.; Bravi, V.; Bendini, M.G.; Mazza, A. The relationship between obesity and hypertension: An updated comprehensive overview on vicious twins. Hypertens. Res. 2017, 40, 947–963. [Google Scholar] [CrossRef] [PubMed]
- Borrell, L.N.; Samuel, L. Body mass index categories and mortality risk in US adults: The effect of overweight and obesity on ad-vancing death. Am. J. Public Health 2014, 104, 512–519. [Google Scholar] [CrossRef] [PubMed]
| Overall | Percentage | Female | Percentage | Male | Percentage | p-Value | |
|---|---|---|---|---|---|---|---|
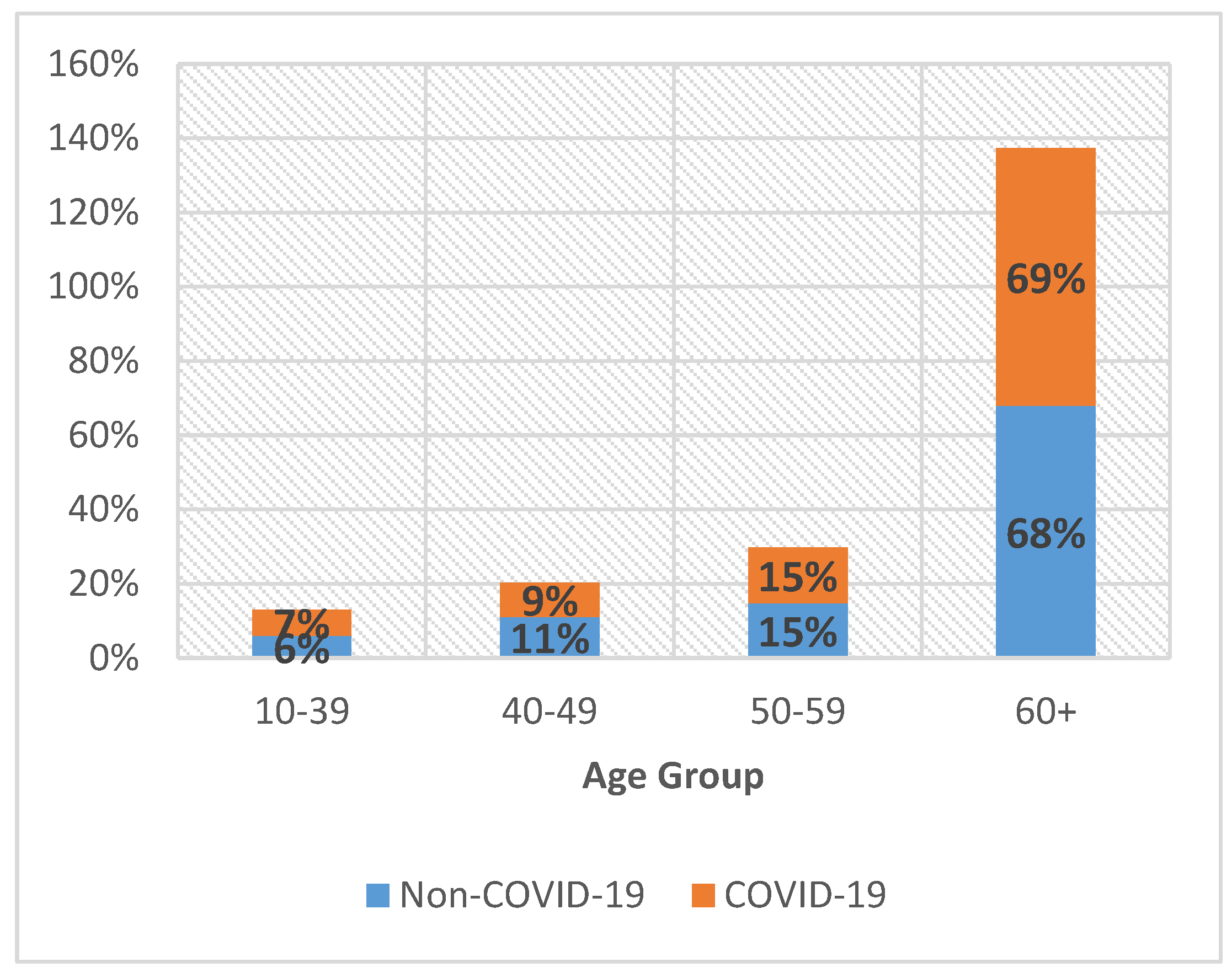
| Age | 0.986 | ||||||
| 20–29 | 10 | 1% | 6 | 1% | 4 | 2% | |
| 30–39 | 62 | 6% | 29 | 5% | 33 | 6% | |
| 40–49 | 101 | 9% | 51 | 9% | 50 | 9% | |
| 50–59 | 172 | 15% | 90 | 15% | 82 | 15% | |
| 60+ | 774 | 69% | 412 | 70% | 362 | 68% | |
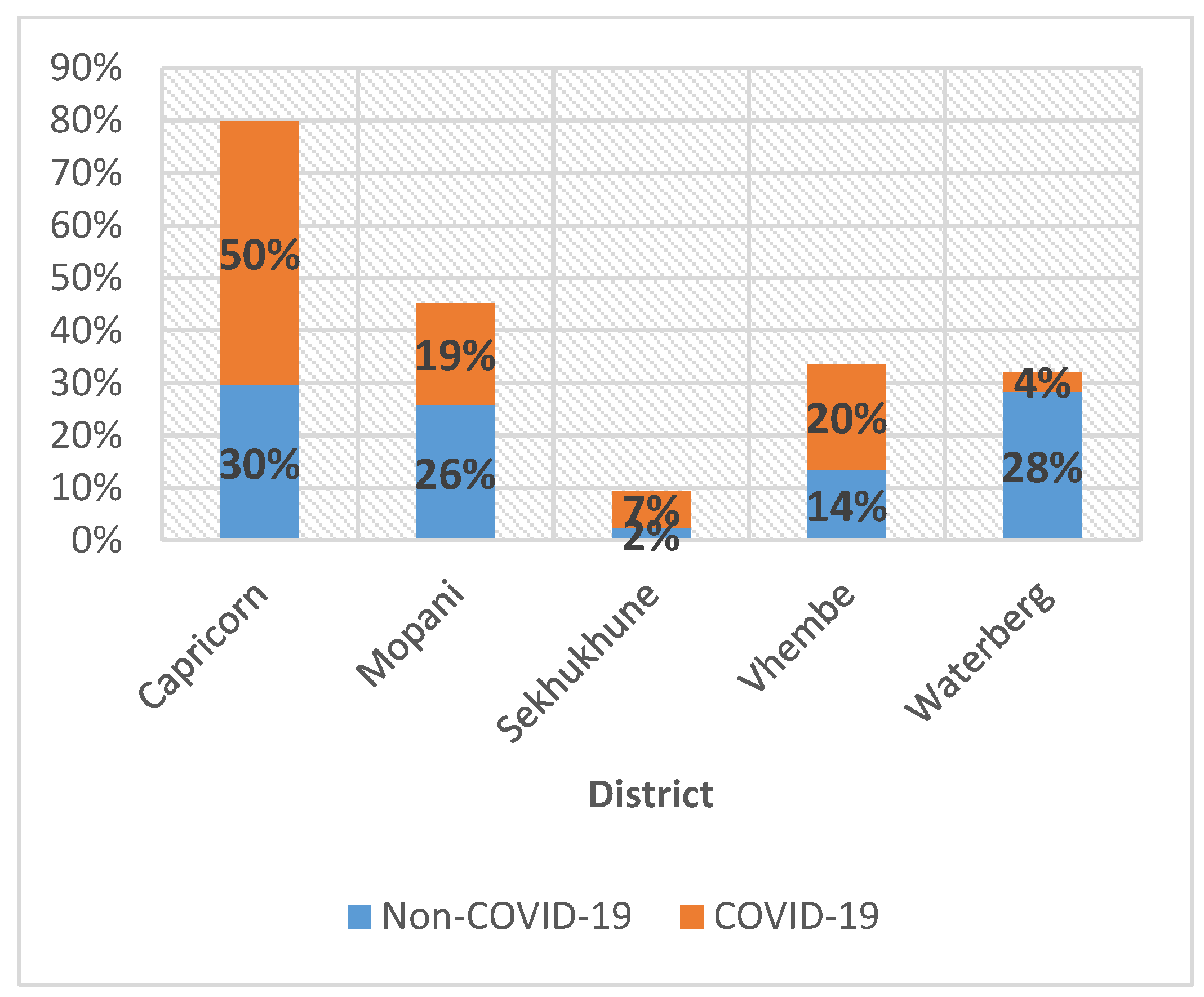
| District | <0.001 | ||||||
| Capricorn | 499 | 43% | 273 | 45% | 226 | 42% | |
| Mopani | 219 | 19% | 116 | 19% | 103 | 19% | |
| Sekhukhune | 94 | 8% | 42 | 7% | 52 | 10% | |
| Vhembe | 279 | 24% | 146 | 24% | 133 | 24% | |
| Waterberg | 57 | 5% | 27 | 4% | 30 | 6% | |
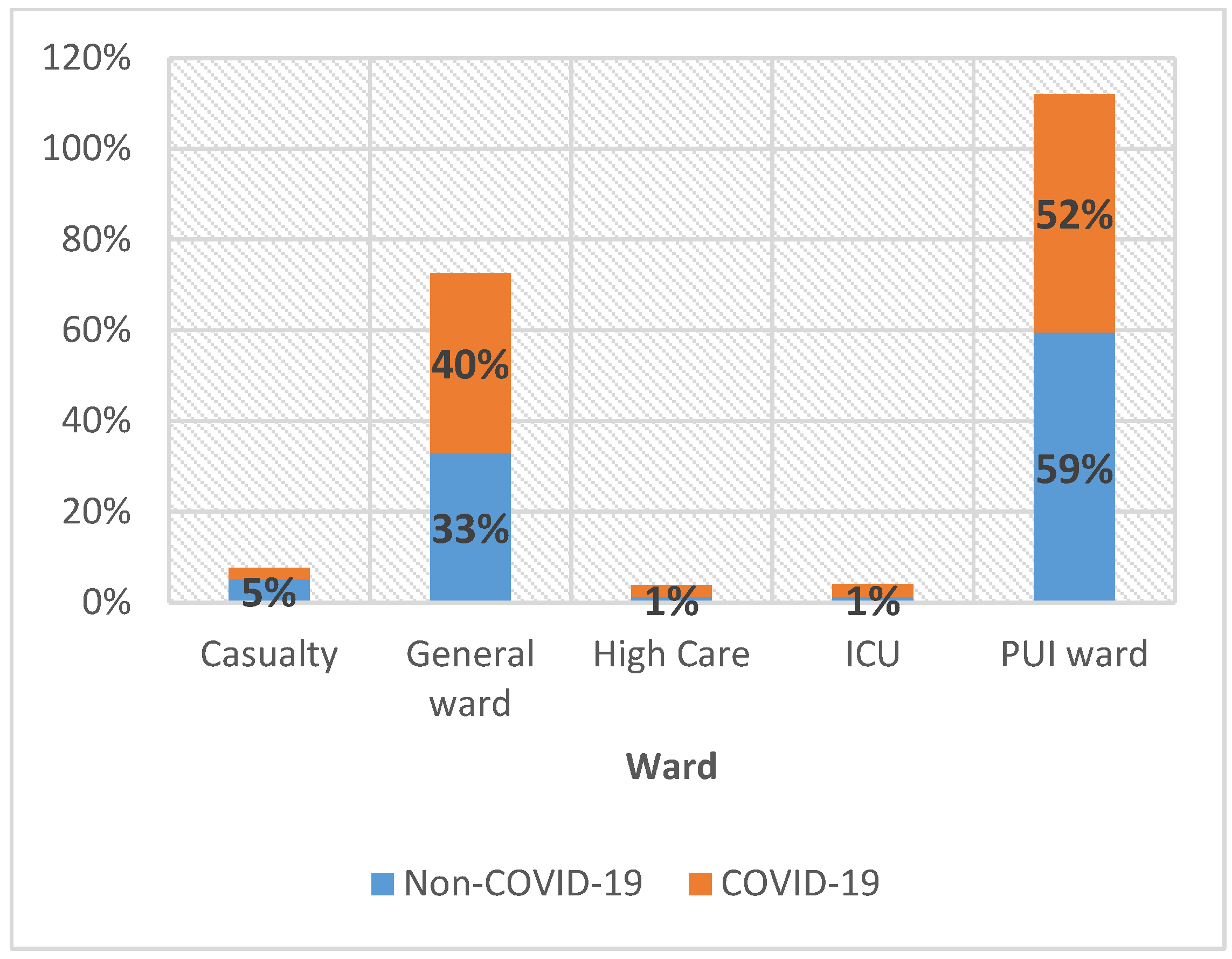
| Wards | 0.037 | ||||||
| Casualty | 27 | 2% | 10 | 2% | 17 | 3% | |
| General ward | 403 | 37% | 214 | 37% | 189 | 37% | |
| High Care | 23 | 2% | 10 | 2% | 13 | 3% | |
| ICU | 26 | 2% | 17 | 3% | 9 | 2% | |
| PUI ward | 606 | 56% | 325 | 56% | 281 | 55% | |
| Comorbid conditions | |||||||
| HIV/AIDS | 141 | 19% | 69 | 18% | 72 | 20% | 0.507 |
| TB | 37 | 5% | 12 | 3% | 25 | 8% | 0.021 |
| COPD | 18 | 3% | 9 | 3% | 9 | 3% | 0.917 |
| Hypertension | 586 | 64% | 319 | 65% | 267 | 62% | 0.344 |
| Diabetes Mellitus | 450 | 52% | 243 | 54% | 207 | 50% | 0.188 |
| Asthma | 35 | 5% | 25 | 7% | 10 | 3% | 0.016 |
| Obesity | 81 | 12% | 52 | 14% | 29 | 9% | 0.022 |
| Cancer | 23 | 4% | 11 | 3% | 12 | 4% | 0.758 |
| Chronic treatment | 493 | 67% | 275 | 70% | 218 | 63% | 0.057 |
| Respiratory distress | 919 | 88% | 483 | 88% | 436 | 89% | 0.188 |
| Mechanical ventilation | 59 | 8% | 33 | 9% | 26 | 8% | 0.692 |
| Clinical presentations | |||||||
| Fever (self-reported) | 266 | 55% | 126 | 53% | 140 | 58% | 0.123 |
| Chills | 148 | 33% | 73 | 34% | 75 | 33% | 0.056 |
| Cough | 650 | 81% | 324 | 81% | 326 | 82% | 0.030 |
| Sore throat | 137 | 32% | 62 | 30% | 75 | 34% | 0.031 |
| Shortness of breath | 714 | 84% | 368 | 83% | 346 | 85% | 0.645 |
| Anosmia | 65 | 16% | 23 | 12% | 42 | 19% | 0.001 |
| Dysgeusia | 83 | 20% | 37 | 19% | 46 | 21% | 0.020 |
| Myalgia/body aches | 374 | 60% | 199 | 62% | 175 | 58% | 0.387 |
| Diarrhoea | 145 | 31% | 74 | 32% | 71 | 30% | 0.071 |
| Chest Pain | 55 | 8% | 29 | 8% | 26 | 8% | 0.973 |
| Loss of appetite | 65 | 9% | 34 | 9% | 31 | 9% | 0.997 |
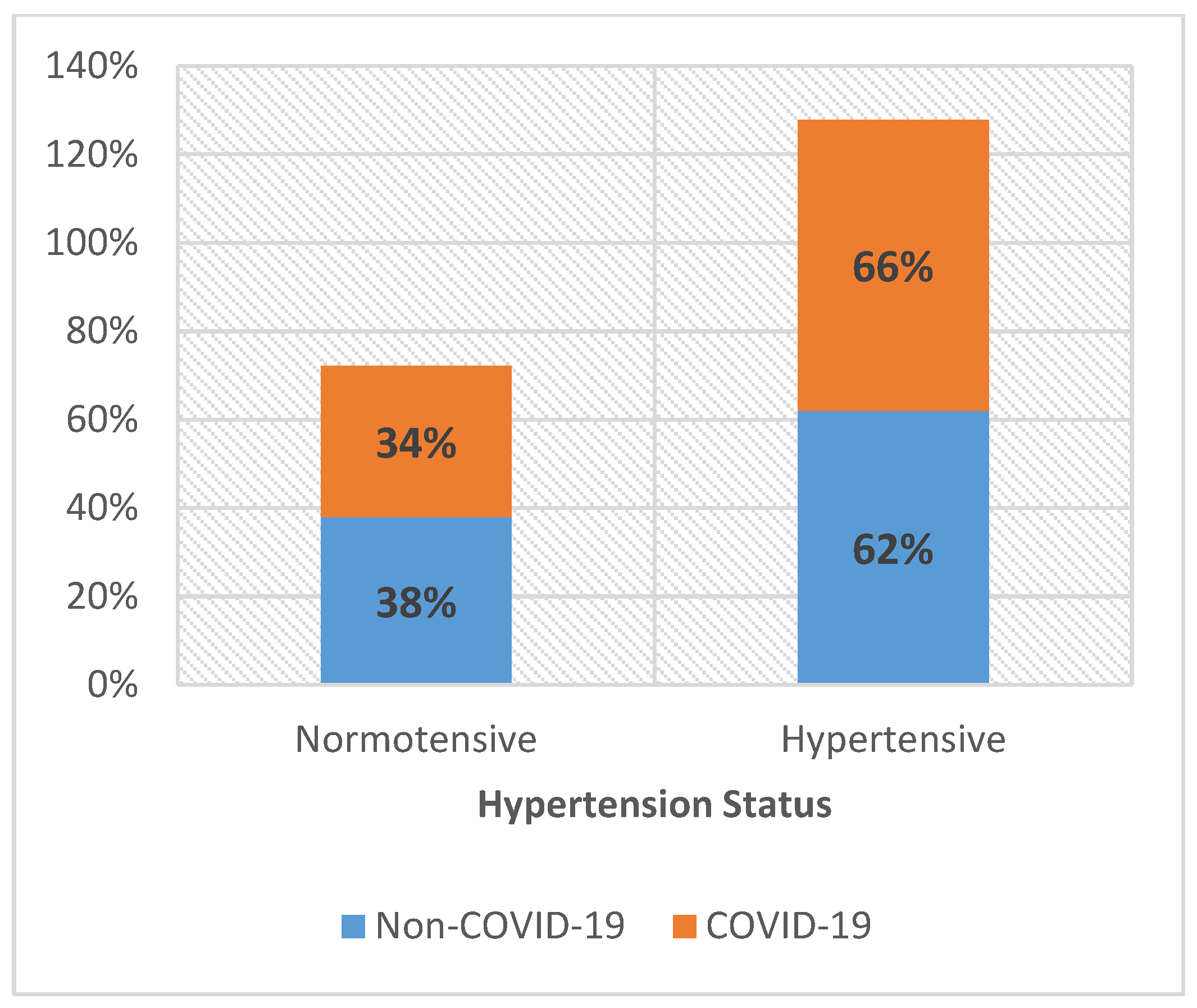
| Variables | Normotensive | Hypertensive 586 (64%) | Model 1: OR (95% CI) | Model 2: OR (95% CI) | Model 3: OR (95% CI) | p-Value |
|---|---|---|---|---|---|---|
| Comorbid conditions | ||||||
| HIV/AIDS | 40 (46.0%) | 47 (54.0%) | 0.46 (0.23; 0.91) | 0.64 (0.30; 1.34) | 0.42 (0.18; 0.99) | 0.046 |
| TB | 17 (70.8%) | 7 (29.2%) | 0.35 (0.09; 1.33) | 0.44 (0.11; 1.84) | 0.34 (0.07; 1.59) | 0.171 |
| COPD | 5 (45.5%) | 6 (54.5%) | 1.64 (0.34; 7.8) | 1.09 (0.22; 5.42) | 1.45 (0.26; 7.99) | 0.672 |
| Diabetes mellitus | 52 (16.1%) | 271 (83.9%) | 4.73 (3.09; 7.2) | 5.04 (3.22; 7.89) | 3.19 (1.81; 5.62) | <0.001 |
| Asthma | 8 (32.0%) | 17 (68.0%) | 0.99 (0.34; 2.93) | 1.13 (0.37; 3.48) | 0.59 (0.16; 2.19) | 0.437 |
| Obesity | 11 (19.3%) | 46 (80.7%) | 1.74 (0.71; 4.30) | 2.46 (0.90; 6.71) | 1.58 (0.48; 5.27) | 0.456 |
| Cancer | 5 (29.4%) | 12 (70.6%) | 3.14 (0.93; 10.52) | 3.23 (0.86; 12.07) | 4.15 (0.45; 38.24) | 0.209 |
| Gender | ||||||
| Female | 128 (32.7%) | 263 (67.3%) | Reference | Reference | ||
| Male | 114 (35.8%) | 204 (64.2%) | 0.97 (0.63; 1.49) | 0.94 (0.54; 1.63) | 0.848 | |
| Age | ||||||
| 0–29 | 3 (75.0%) | 1 (25.0%) | Reference | Reference | ||
| 30–39 | 25 (78.1%) | 7 (21.9%) | 0.50 (0.03; 8.47) | 0.84 (0.04; 18.66) | 0.913 | |
| 40–49 | 31 (51.7%) | 29 (48.3%) | 1.01 (0.07; 13.97) | 2.244 (0.13; 36.74) | 0.571 | |
| 50–59 | 48 (45.3%) | 58 (54.7%) | 2.07 (0.16; 27.42) | 3.791 (0.24; 58.25) | 0.339 | |
| 135 (26.6%) | 372 (73.4%) | 4.96 (0.39; 62.95) | 10.66 (0.73; 154.3) | 0.082 | ||
| Case severity | ||||||
| Mild | 14 (33.3%) | 28 (66.7%) | Reference | |||
| Moderate | 26 (27.1%) | 70 (72.9%) | 2.36 (0.46; 12.07) | 0.302 | ||
| Severe | 194 (35.9%) | 347 (64.1%) | 2.09 (0.45; 9.68) | 0.346 | ||
| Patient-related factors | ||||||
| On chronic treatment | 82 (22.6%) | 281 (77.4%) | 8.50 (4.71; 15.34) | <0.001 | ||
| Respiratory distress | 59 (38.3%) | 95 (61.7%) | 0.88 (0.29; 2.76) | 0.837 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mphekgwana, P.M.; Matlala, S.F.; Tshitangano, T.G.; Ramalivhana, N.J.; Sono-Setati, M.E. Risk Factors for Hypertension in Hospitalised Patient Mortality with Laboratory-Confirmed SARS-CoV-2: A Population-Based Study in Limpopo Province, South Africa. J. Respir. 2022, 2, 147-156. https://doi.org/10.3390/jor2030013
Mphekgwana PM, Matlala SF, Tshitangano TG, Ramalivhana NJ, Sono-Setati ME. Risk Factors for Hypertension in Hospitalised Patient Mortality with Laboratory-Confirmed SARS-CoV-2: A Population-Based Study in Limpopo Province, South Africa. Journal of Respiration. 2022; 2(3):147-156. https://doi.org/10.3390/jor2030013
Chicago/Turabian StyleMphekgwana, Peter M., Sogo F. Matlala, Takalani G. Tshitangano, Naledzani J. Ramalivhana, and Musa E. Sono-Setati. 2022. "Risk Factors for Hypertension in Hospitalised Patient Mortality with Laboratory-Confirmed SARS-CoV-2: A Population-Based Study in Limpopo Province, South Africa" Journal of Respiration 2, no. 3: 147-156. https://doi.org/10.3390/jor2030013
APA StyleMphekgwana, P. M., Matlala, S. F., Tshitangano, T. G., Ramalivhana, N. J., & Sono-Setati, M. E. (2022). Risk Factors for Hypertension in Hospitalised Patient Mortality with Laboratory-Confirmed SARS-CoV-2: A Population-Based Study in Limpopo Province, South Africa. Journal of Respiration, 2(3), 147-156. https://doi.org/10.3390/jor2030013






