Impact of Perceptions of Air Pollution and Noise on Subjective Well-Being and Health
Abstract
:1. Introduction
1.1. Air Pollution and Human Well-Being
1.2. Noise and Human Well-Being
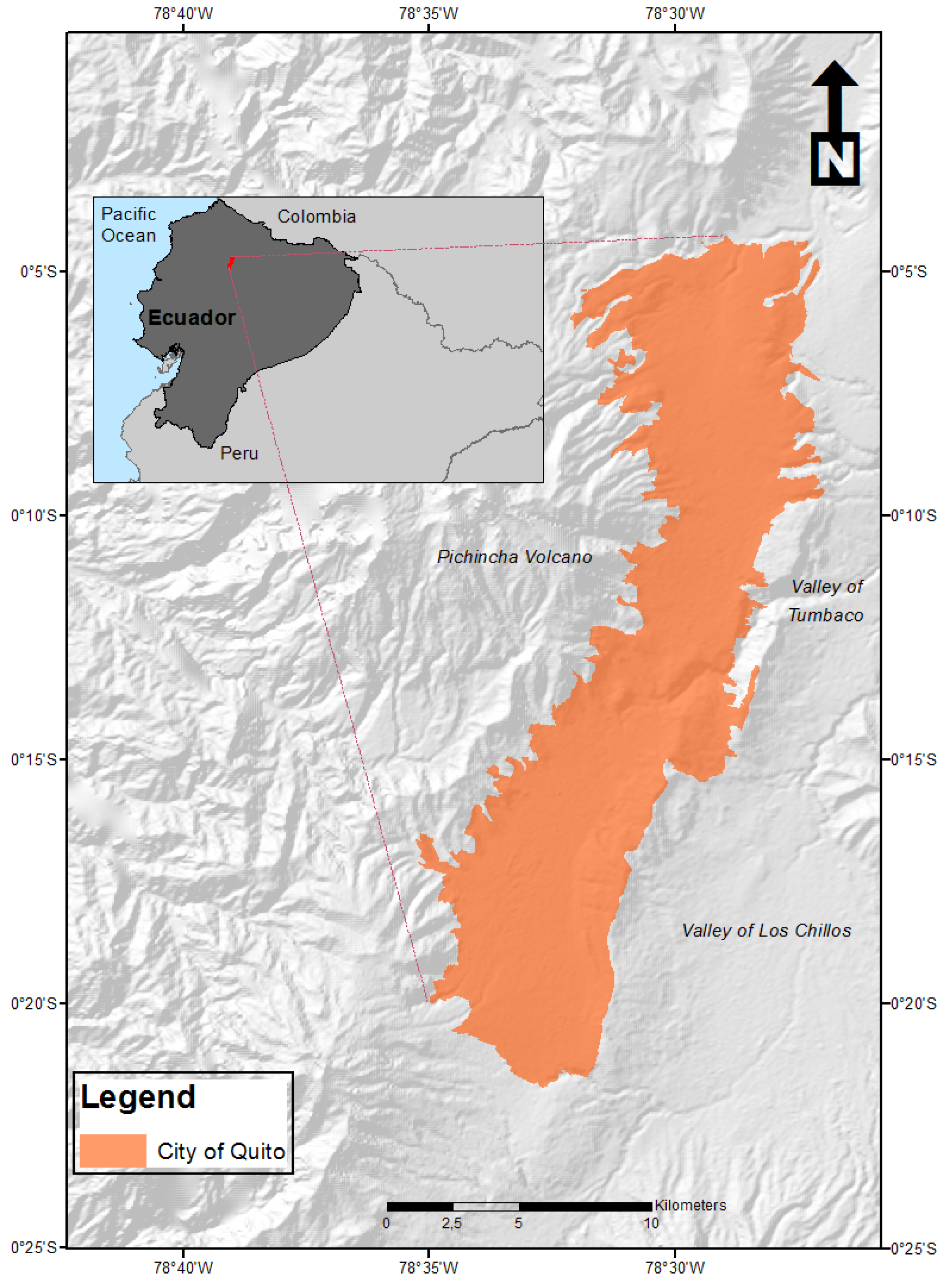
2. Materials and Methods
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Corrigan, P.W.; Watson, A.C. Understanding the Impact of Stigma on People with Mental Illness. World Psychiatry 2002, 1, 16–20. [Google Scholar] [PubMed]
- OPS. La Carga de Los Trastornos Mentales En La Región de Las Américas; Organización Panamericana de la Salud: Washington, WA, USA, 2018. [Google Scholar]
- Kassebaum, N.J.; Arora, M.; Barber, R.M.; Brown, J.; Carter, A.; Casey, D.C.; Charlson, F.J.; Coates, M.M.; Coggeshall, M.; Cornaby, L.; et al. Global, Regional, and National Disability-Adjusted Life-Years (DALYs) for 315 Diseases and Injuries and Healthy Life Expectancy (HALE), 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1603–1658. [Google Scholar] [CrossRef] [Green Version]
- Veenhoven, R. The Four Qualities of Life. J. Happiness Stud. 2000, 1, 1–39. [Google Scholar] [CrossRef]
- Vassos, E.; Pedersen, C.B.; Murray, R.M.; Collier, D.A.; Lewis, C.M. Meta-Analysis of the Association of Urbanicity with Schizophrenia. Schizophr. Bull. 2012, 38, 1118–1123. [Google Scholar] [CrossRef] [Green Version]
- Heinz, A.; Deserno, L.; Reininghaus, U. Urbanicity, Social Adversity and Psychosis. World Psychiatry 2013, 12, 187–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Landrigan, P.J. Air Pollution and Health. Lancet Public Health 2017, 2, e4–e5. [Google Scholar] [CrossRef] [Green Version]
- Galea, S.; Ahern, J.; Nandi, A.; Tracy, M.; Beard, J.; Vlahov, D. Urban Neighborhood Poverty and the Incidence of Depression in a Population-Based Cohort Study. Ann. Epidemiol. 2007, 17, 171–179. [Google Scholar] [CrossRef] [Green Version]
- Galea, S.; Freudenberg, N.; Vlahov, D. Cities and Population Health. Soc. Sci. Med. 2005, 60, 1017–1033. [Google Scholar] [CrossRef]
- Gruebner, O.; Rapp, M.A.; Adli, M.; Kluge, U.; Galea, S.; Heinz, A. Cities and Mental Health. Dtsch. Arztebl. Int. 2017, 114, 121–127. [Google Scholar] [CrossRef] [Green Version]
- Caracci, G. General Concepts of the Relationship between Urban Areas and Mental Health. Curr. Opin. Psychiatry 2008, 21, 385–390. [Google Scholar] [CrossRef]
- Marangoni, C.; Hernandez, M.; Faedda, G.L. The Role of Environmental Exposures as Risk Factors for Bipolar Disorder: A Systematic Review of Longitudinal Studies. J. Affect. Disord. 2016, 193, 165–174. [Google Scholar] [CrossRef]
- Bortolato, B.; Köhler, C.A.; Evangelou, E.; León-Caballero, J.; Solmi, M.; Stubbs, B.; Belbasis, L.; Pacchiarotti, I.; Kessing, L.V.; Berk, M.; et al. Systematic Assessment of Environmental Risk Factors for Bipolar Disorder: An Umbrella Review of Systematic Reviews and Meta-Analyses. Bipolar Disord. 2017, 19, 84–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srinivasan, S.; O’Fallon, L.R.; Dearry, A. Creating Healthy Communities, Healthy Homes, Healthy People: Initiating a Research Agenda on the Built Environment and Public Health. Am. J. Public Health 2003, 93, 1446–1450. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Guan, D.; Tao, S.; Wang, X.; He, K. A Review of Air Pollution Impact on Subjective Well-Being: Survey versus Visual Psychophysics. J. Clean. Prod. 2018, 184, 959–968. [Google Scholar] [CrossRef]
- Ahumada, G.; Iturra, V. If the Air Was Cleaner, Would We Be Happier? An Economic Assessment of the Effects of Air Pollution on Individual Subjective Well-Being in Chile. J. Clean. Prod. 2021, 289, 125152. [Google Scholar] [CrossRef]
- Lelieveld, J.; Klingmüller, K.; Pozzer, A.; Pöschl, U.; Fnais, M.; Daiber, A.; Münzel, T. Cardiovascular Disease Burden from Ambient Air Pollution in Europe Reassessed Using Novel Hazard Ratio Functions. Eur. Heart J. 2019, 40, 1590–1596. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Guan, D.; Yu, Y.; Westland, S.; Wang, D.; Meng, J.; Wang, X.; He, K.; Tao, S. A Psychophysical Measurement on Subjective Well-Being and Air Pollution. Nat. Commun. 2019, 10, 1–8. [Google Scholar] [CrossRef]
- Shaposhnikov, D.; Revich, B.; Bellander, T.; Bedada, G.B.; Bottai, M.; Kharkova, T.; Kvasha, E.; Lezina, E.; Lind, T.; Semutnikova, E.; et al. Mortality Related to Air Pollution with the Moscow Heat Wave and Wildfire of 2010. Epidemiology 2014, 25, 359. [Google Scholar] [CrossRef] [Green Version]
- Block, M.L.; Calderón-Garcidueñas, L. Air Pollution: Mechanisms of Neuroinflammation and CNS Disease. Trends Neurosci. 2009, 32, 506–516. [Google Scholar] [CrossRef] [Green Version]
- Mills, N.L.; Donaldson, K.; Hadoke, P.W.; Boon, N.A.; MacNee, W.; Cassee, F.R.; Sandström, T.; Blomberg, A.; Newby, D.E. Adverse Cardiovascular Effects of Air Pollution. Nat. Clin. Pract. Cardiovasc. Med. 2009, 6, 36–44. [Google Scholar] [CrossRef]
- Khan, A.; Plana-Ripoll, O.; Antonsen, S.; Brandt, J.; Geels, C.; Landecker, H.; Sullivan, P.F.; Pedersen, C.B.; Rzhetsky, A. Environmental Pollution Is Associated with Increased Risk of Psychiatric Disorders in the US and Denmark. PLoS Biol. 2019, 17, e3000353. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, I.; Zhang, S.; Kirkbride, J.B.; Osborn, D.P.J.; Hayes, J.F. Air Pollution (Particulate Matter) Exposure and Associations with Depression, Anxiety, Bipolar, Psychosis and Suicide Risk: A Systematic Review and Meta-Analysis. Environ. Health Perspect. 2020, 127, 126002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linares Gil, C. Las PM 2.5 y Su Impacto Sobre La Salud. El Caso de La Ciudad de Madrid. Ecosostenible 2007, 35, 32–37. [Google Scholar]
- Oudin, A.; Carlsen, H.; Åström, D.; Asplund, P.; Steingrimsson, S.; Szabo, Z. The Association between Daily Concentrations of Air Pollution and Visits to a Psychiatric Emergency Unit: A Case-Crossover Study. Environ. Health 2018, 17, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szyszkowicz, M.; Willey, J.B.; Grafstein, E.; Rowe, B.H.; Colman, I. Air Pollution and Emergency Department Visits for Suicide Attempts in Vancouver, Canada. Environ. Health Insights 2010, 4, EHI-S5662. [Google Scholar] [CrossRef]
- Yang, Z.; Song, Q.; Li, J.; Zhang, Y.; Yuan, X.C.; Wang, W.; Yu, Q. Air Pollution and Mental Health: The Moderator Effect of Health Behaviors. Environ. Res. Lett. 2021, 16, 044005. [Google Scholar] [CrossRef]
- Sørensen, M.; Daneshvar, B.; Hansen, M.; Dragsted, L.O.; Hertel, O.; Knudsen, L.; Loft, S. Personal PM2.5 Exposure and Markers of Oxidative Stress in Blood. Environ. Health Perspect. 2003, 111, 161–166. [Google Scholar] [CrossRef] [Green Version]
- Salim, S.; Chugh, G.; Asghar, M. Chapter One—Inflammation in Anxiety. In Advances in Protein Chemistry and Structural Biology; Donev, R., Ed.; Academic Press: Cambridge, MA, USA, 2012; Volume 88, pp. 1–25. ISBN 1876-1623. [Google Scholar]
- MohanKumar, S.M.J.; Campbell, A.; Block, M.; Veronesi, B. Particulate Matter, Oxidative Stress and Neurotoxicity. Neurotoxicology 2008, 29, 479–488. [Google Scholar] [CrossRef]
- Marazziti, D.; Cianconi, P.; Mucci, F.; Foresi, L.; Chiarantini, I.; Della Vecchia, A. Climate Change, Environment Pollution, COVID-19 Pandemic and Mental Health. Sci. Total Environ. 2021, 773, 145182. [Google Scholar] [CrossRef]
- Vert, C.; Sánchez-Benavides, G.; Martínez, D.; Gotsens, X.; Gramunt, N.; Cirach, M.; Molinuevo, J.L.; Sunyer, J.; Nieuwenhuijsen, M.J.; Crous-Bou, M.; et al. Effect of Long-Term Exposure to Air Pollution on Anxiety and Depression in Adults: A Cross-Sectional Study. Int. J. Hyg. Environ. Health 2017, 220, 1074–1080. [Google Scholar] [CrossRef]
- WHO Regional Office for Europe. Noise Guidelines for the European Region; WHO: Geneva, Switzerland, 2018; ISBN 9789289053563. [Google Scholar]
- World Health Organization. Burden of Disease from Environmental Noise: Quantification of Healthy Life Years Lost in Europe; WHO: Copenhagen, Denmark, 2011. [Google Scholar]
- Sampath, S.; Das, S.M.; Kumar, V.S. Ambient Noise Levels in Major Cities in Kerala. J. Ind. Geophys. Union 2004, 8, 293–298. [Google Scholar]
- Yuan, M.; Yin, C.; Sun, Y.; Chen, W. Examining the Associations between Urban Built Environment and Noise Pollution in High-Density High-Rise Urban Areas: A Case Study in Wuhan, China. Sustain. Cities Soc. 2019, 50, 101678. [Google Scholar] [CrossRef]
- Carozzi, F.; Roth, S. Dirty Density: Air Quality and the Density of American Cities. SSRN 2020, 13191, 1–54. [Google Scholar] [CrossRef]
- Centros Para el Control y la Prevención de Enfermedades CDC. Tipos de Pérdida Auditiva (Sordera). Available online: https://www.cdc.gov/ncbddd/spanish/hearingloss/types.html (accessed on 9 May 2022).
- MedlinePlus. Tinnitus. Available online: https://medlineplus.gov/spanish/tinnitus.html (accessed on 9 May 2022).
- Gan, W.Q.; Davies, H.W.; Koehoorn, M.; Brauer, M. Association of Long-Term Exposure to Community Noise and Traffic-Related Air Pollution With Coronary Heart Disease Mortality. Am. J. Epidemiol. 2012, 175, 898–906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Münzel, T.; Sørensen, M.; Gori, T.; Schmidt, F.P.; Rao, X.; Brook, J.; Chen, L.C.; Brook, R.D.; Rajagopalan, S. Environmental Stressors and Cardio-Metabolic Disease: Part I–Epidemiologic Evidence Supporting a Role for Noise and Air Pollution and Effects of Mitigation Strategies. Eur. Heart J. 2017, 38, 550–556. [Google Scholar] [CrossRef] [Green Version]
- Cui, B.; Gai, Z.; She, X.; Wang, R.; Xi, Z. Effects of Chronic Noise on Glucose Metabolism and Gut Microbiota–Host Inflammatory Homeostasis in Rats. Sci. Rep. 2016, 6, 36693. [Google Scholar] [CrossRef]
- Halperin, D. Environmental Noise and Sleep Disturbances: A Threat to Health? Sleep Sci. 2014, 7, 209–212. [Google Scholar] [CrossRef] [Green Version]
- Langdon, F.J.; Buller, I.B. Road Traffic Noise and Disturbance to Sleep. J. Sound Vib. 1977, 50, 13–28. [Google Scholar] [CrossRef]
- Perron, S.; Plante, C.; Ragettli, M.; Kaiser, D.; Goudreau, S.; Smargiassi, A. Sleep Disturbance from Road Traffic, Railways, Airplanes and from Total Environmental Noise Levels in Montreal. Int. J. Environ. Res. Public Health 2016, 13, 809. [Google Scholar] [CrossRef] [Green Version]
- Eriksson, C.; Bodin, T.; Selander, J. Burden of Disease from Road Traffic and Railway Noise—A Quantification of Healthy Life Years Lost in Sweden. Scand. J. Work. Environ. Health 2017, 43, 519–525. [Google Scholar] [CrossRef]
- Hammersen, F.; Niemann, H.; Hoebel, J. Environmental Noise Annoyance and Mental Health in Adults: Findings from the Cross-Sectional German Health Update (GEDA) Study 2012. Int. J. Environ. Res. Public Health 2016, 13, 954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barzegar, M.; Sajjadi, F.S.; Talaei, S.A.; Hamidi, G.; Salami, M. Prenatal Exposure to Noise Stress: Anxiety, Impaired Spatial Memory, and Deteriorated Hippocampal Plasticity in Postnatal Life. Hippocampus 2015, 25, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Riojas-Rodríguez, H.; Soares Da Silva, A.; Texcalac-Sangrador, J.L.; Moreno-Banda, G.L. Air Pollution Management and Control in Latin America and the Caribbean: Implications for Climate Change. Rev. Panam. Salud Pública 2016, 40, 150–159. [Google Scholar] [PubMed]
- Páez, C. Gestión de La Contaminación Atmosférica Urbana: El Caso de Quito; FlacsoAndes: Quito, Ecuador, 2006. [Google Scholar]
- Judd, F.; Armstrong, S.; Kulkarni, J. Gender-Sensitive Mental Health Care. Australas. Psychiatry 2009, 17, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Inglehart, R. Gender, Aging, and Subjective Well-Being. Int. J. Comp. Sociol. 2002, 43, 391–408. [Google Scholar] [CrossRef]
- Diener, E.; Suh, M.E. Subjective Well-Being and Age: An International Analysis. Annu. Rev. Gerontol. Geriatr. 1998, 17, 304–324. [Google Scholar] [CrossRef]
- Golberstein, E. The Effects of Income on Mental Health: Evidence from the Social Security Notch. J. Ment. Health Policy Econ. 2015, 18, 27–37. [Google Scholar]
- Gardner, J.; Oswald, A.J. Money and Mental Wellbeing: A Longitudinal Study of Medium-Sized Lottery Wins. J. Health Econ. 2007, 26, 49–60. [Google Scholar] [CrossRef] [Green Version]
- Zepke, N. Lifelong Education for Subjective Well-Being: How Do Engagement and Active Citizenship Contribute? Int. J. Lifelong Educ. 2013, 32, 639–651. [Google Scholar] [CrossRef]
- Kristoffersen, I. Great Expectations: Education and Subjective Wellbeing. J. Econ. Psychol. 2018, 66, 64–78. [Google Scholar] [CrossRef]
- Bailey, T.C.; Snyder, C.R. Satisfaction with Life and Hope: A Look at Age and Marital Status. Psychol. Rec. 2007, 57, 233–240. [Google Scholar] [CrossRef] [Green Version]
- Ma, J.; Li, C.; Kwan, M.-P.; Chai, Y. A Multilevel Analysis of Perceived Noise Pollution, Geographic Contexts and Mental Health in Beijing. Int. J. Environ. Res. Public Health 2018, 15, 1479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oiamo, T.H.; Luginaah, I.N.; Baxter, J. Cumulative Effects of Noise and Odour Annoyances on Environmental and Health Related Quality of Life. Soc. Sci. Med. 2015, 146, 191–203. [Google Scholar] [CrossRef] [PubMed]
- Wojnarowska, M.; Plichta, G.; Sagan, A.; Plichta, J.; Stobiecka, J.; Sołtysik, M. Odour Nuisance and Urban Residents’ Quality of Life: A Case Study in Kraków’s in Plaszow District. Urban Clim. 2020, 34, 100704. [Google Scholar] [CrossRef]
- Shusterman, D. The Health Significance of Environmental Odour Pollution: Revisited. J. Environ. Med. 1999, 1, 249–258. [Google Scholar] [CrossRef]
- Shroff, F.M.; Jung, D. Here’s to Sound Action on Global Hearing Health through Public Health Approaches. Int. J. Health Gov. 2020, 25, 235–244. [Google Scholar] [CrossRef]
- Secretaría de Ambiente AQI|Municipio Del Distrito Metropolitano de Quito. Available online: http://www.quitoambiente.gob.ec/index.php/indice-de-calidad-del-aire (accessed on 9 May 2022).
- Quito Cómo Vamos. Encuesta de Percepción Ciudadana de Quito; Quito Cómo Vamos: Quito, Ecuador, 2020. [Google Scholar]
- Makri, A.; Stilianakis, N.I. Vulnerability to Air Pollution Health Effects. Int. J. Hyg. Environ. Health 2008, 211, 326–336. [Google Scholar] [CrossRef]
- Cabrera-Barona, P.; Blaschke, T.; Gaona, G. Deprivation, Healthcare Accessibility and Satisfaction: Geographical Context and Scale Implications. Appl. Spat. Anal. Policy 2018, 11, 313–332. [Google Scholar] [CrossRef] [Green Version]
- Cabrera-Barona, P. Influence of Urban Multi-Criteria Deprivation and Spatial Accessibility to Healthcare on Self-Reported Health. Urban Sci. 2017, 1, 11. [Google Scholar] [CrossRef] [Green Version]
- American Psychological Association. Stress in AmericaTM Generation Z; American Psychological Association: Washington, DC, WA, USA, 2018. [Google Scholar]
- Tobias, M.I.; Cheung, J. Monitoring Health Inequalities: Life Expectancy and Small Area Deprivation in New Zealand. Popul. Health Metr. 2003, 1, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Chen, W. How Education Enhances Happiness: Comparison of Mediating Factors in Four East Asian Countries. Soc. Indic. Res. 2012, 106, 117–131. [Google Scholar] [CrossRef]
- Contreras, J. El Impacto de La Contaminación Del Aire En La Vida y En Las Percepciones de Género En La Ciudad de Quito; FLACSO Sede Ecuador: Quito, Ecuador, 2002. [Google Scholar]
- Westreich, D.; Greenland, S. The Table 2 Fallacy: Presenting and Interpreting Confounder and Modifier Coefficients. Am. J. Epidemiol. 2013, 177, 292–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Psychology Foundation of Australia Depression Anxiety Stress Scales—DASS. Available online: http://www2.psy.unsw.edu.au/groups/dass/ (accessed on 9 May 2022).
| Variable | Category | Percentage |
|---|---|---|
| Sex | Female | 70.60 |
| Male | 29.40 | |
| Age | 18–24 | 43.50 |
| 25–34 | 31.60 | |
| 35–44 | 8.60 | |
| 45–54 | 7.10 | |
| >54 | 9.30 | |
| Education | Basic | 1.90 |
| High school | 15.20 | |
| Higher education | 66.50 | |
| Postgraduate studies | 16.40 | |
| Marital status | Single | 74.30 |
| Married | 21.20 | |
| Divorced | 3.70 | |
| Widow | 0.70 | |
| Income | USD 0–USD 400 | 49.40 |
| USD 401–USD 800 | 24.90 | |
| USD 801–USD 1200 | 10.40 | |
| USD 1201–USD 1600 | 5.60 | |
| USD 1601–USD 2000 | 4.80 | |
| USD 2001 or more | 4.80 |
| Variable | Category | Percentage |
|---|---|---|
| Self-perceived health | Not being healthy | 0.70 |
| Having poor health | 14.50 | |
| Being healthy | 72.20 | |
| Being very healthy | 12.60 | |
| Self-perceived happiness | Not being happy | 3.00 |
| Having low levels of happiness | 13.40 | |
| Being happy | 53.90 | |
| Being very happy | 29.70 | |
| Satisfaction with life | Not being satisfied with life | 3.30 |
| Having low satisfaction with life | 17.10 | |
| Being satisfied with life | 52.80 | |
| Being very satisfied with life | 26.80 | |
| Air pollution (visual) | Not at all polluted | 7.80 |
| Slightly polluted | 51.70 | |
| Moderately polluted | 34.20 | |
| Very polluted | 6.30 | |
| Air pollution (unpleasant odors) | Never | 9.70 |
| Rarely | 46.50 | |
| Sometimes | 36.80 | |
| Always | 7.10 | |
| Noises affecting well-being | Never | 7.10 |
| Rarely | 29.70 | |
| Sometimes | 37.90 | |
| Always | 25.30 |
| Variable | Category | Estimate | p-Value | Odds Ratio | 95% Confidence Intervals | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Air pollution (visual) | Not at all polluted | 0.32 | 0.70 | 1.38 | 0.27 | 7.13 |
| Slightly polluted | 0.43 | 0.51 | 1.53 | 0.44 | 5.39 | |
| Moderately polluted | 0.41 | 0.53 | 1.51 | 0.43 | 5.27 | |
| Very polluted | 0 | - | 1 | - | - | |
| Air pollution (unpleasant odors) | Never | 1.39 | 0.08 * | 4.00 | 0.83 | 19.42 |
| Rarely | 0.44 | 0.48 | 1.55 | 0.45 | 5.27 | |
| Sometimes | 0.52 | 0.40 | 1.68 | 0.49 | 5.67 | |
| Always | 0 | - | 1 | - | - | |
| Noises affecting well-being | Never | 0.89 | 0.19 | 2.43 | 0.64 | 9.17 |
| Rarely | 0.39 | 0.36 | 1.47 | 0.63 | 3.42 | |
| Sometimes | 0.87 | 0.02 ** | 2.38 | 1.11 | 5.09 | |
| Always | 0 | - | 1 | - | - | |
| Healthcare services quality | Not at all efficient | −2.12 | 0.01 ** | 0.12 | 0.02 | 0.59 |
| A little efficient | −2.87 | 0.00 *** | 0.06 | 0.01 | 0.22 | |
| Moderately efficient | −2.12 | 0.00 *** | 0.12 | 0.03 | 0.45 | |
| Very efficient | 0 | - | 1 | - | - | |
| Sex | Female | −0.57 | 0.10 | 0.57 | 0.29 | 1.13 |
| Male | 0 | - | 1 | - | - | |
| Age | 18–24 | 1.44 | 0.04 ** | 4.23 | 1.08 | 16.56 |
| 25–34 | 1.26 | 0.06 * | 3.52 | 0.97 | 12.75 | |
| 35–44 | 1.921 | 0.01 ** | 6.83 | 1.59 | 29.24 | |
| 45–54 | 0.30 | 0.68 | 1.36 | 0.32 | 5.69 | |
| >54 | 0 | - | 1 | - | - | |
| Education | Basic | −0.07 | 0.95 | 0.94 | 0.09 | 9.54 |
| High school | −1.209 | 0.06 * | 0.29 | 0.09 | 1.03 | |
| Higher education | −0.82 | 0.09 * | 0.44 | 0.17 | 1.13 | |
| Postgraduate studies | 0 | - | 1 | - | - | |
| Marital status | Single | −0.80 | 0.66 | 0.45 | 0.01 | 13.51 |
| Married | −0.59 | 0.75 | 0.55 | 0.02 | 17.58 | |
| Divorced | 1.34 | 0.49 | 3.83 | 0.09 | 159.81 | |
| Widow | 0 | - | 1 | - | - | |
| Income | USD 0–USD 400 | 0.18 | 0.84 | 1.19 | 0.21 | 6.61 |
| USD 401–USD 800 | 0.37 | 0.65 | 1.44 | 0.28 | 7.49 | |
| USD 801–USD 1200 | 1.36 | 0.12 | 3.89 | 0.67 | 22.44 | |
| USD 1201–USD 1600 | −1.01 | 0.25 | 0.36 | 0.07 | 2.02 | |
| USD 1601–USD 2000 | 1.58 | 0.09 * | 4.87 | 0.74 | 31.89 | |
| USD 2001 or more | 0 | - | 1 | - | - | |
| Variable | Category | Estimate | p-Value | Odds Ratio | 95% Confidence Intervals | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Air pollution (visual) | Not at all polluted | −0.32 | 0.68 | 0.72 | 0.16 | 3.34 |
| Slightly polluted | −0.87 | 0.15 | 0.42 | 0.13 | 1.34 | |
| Moderately polluted | −0.44 | 0.46 | 0.64 | 0.20 | 2.04 | |
| Very polluted | 0 | - | 1 | - | - | |
| Air pollution (unpleasant odors) | Never | 2.12 | 0.00 *** | 8.36 | 1.89 | 36.88 |
| Rarely | 0.47 | 0.40 | 1.59 | 0.54 | 4.74 | |
| Sometimes | 1.17 | 0.03 ** | 3.23 | 1.09 | 9.57 | |
| Always | 0 | - | 1 | - | - | |
| Noises affecting well-being | Never | 1.89 | 0.00 *** | 6.62 | 1.94 | 22.56 |
| Rarely | 0.47 | 0.22 | 1.59 | 0.76 | 3.35 | |
| Sometimes | 0.49 | 0.15 | 1.63 | 0.84 | 3.16 | |
| Always | 0 | - | 1 | - | - | |
| Healthcare services quality | Not at all efficient | −2.84 | 0.00 *** | 0.06 | 0.01 | 0.32 |
| A little efficient | −2.08 | 0.01 ** | 0.12 | 0.03 | 0.58 | |
| Moderately efficient | −1.43 | 0.06 * | 0.24 | 0.05 | 1.10 | |
| Very efficient | 0 | - | 1 | - | - | |
| Sex | Female | 0.07 | 0.82 | 1.07 | 0.59 | 1.94 |
| Male | 0 | - | 1 | - | - | |
| Age | 18–24 | −0.29 | 0.66 | 0.75 | 0.21 | 2.67 |
| 25–34 | −0.78 | 0.22 | 0.46 | 0.13 | 1.56 | |
| 35–44 | 0.31 | 0.65 | 1.36 | 0.36 | 5.17 | |
| 45–54 | −0.41 | 0.59 | 0.67 | 0.16 | 2.78 | |
| >54 | 0 | - | 1 | - | - | |
| Education | Basic | 2.62 | 0.05 * | 13.77 | 1.06 | 179.29 |
| High school | 0.21 | 0.70 | 1.23 | 0.42 | 3.67 | |
| Higher education | −0.80 | 0.06 * | 0.45 | 0.19 | 1.03 | |
| Postgraduate studies | 0 | - | 1 | - | - | |
| Marital status | Single | 2.96 | 0.04 ** | 19.23 | 1.26 | 293.09 |
| Married | 3.12 | 0.03 ** | 22.68 | 1.39 | 370.72 | |
| Divorced | 3.39 | 0.03 ** | 29.85 | 1.39 | 638.41 | |
| Widow | 0 | - | 1 | - | - | |
| Income | USD 0–USD 400 | −0.89 | 0.27 | 0.41 | 0.09 | 1.91 |
| USD 401–USD 800 | −0.36 | 0.64 | 0.69 | 0.16 | 3.07 | |
| USD 801–USD 1200 | 0.82 | 0.32 | 2.26 | 0.47 | 10.95 | |
| USD 1201–USD 1600 | −0.62 | 0.45 | 0.54 | 0.11 | 2.57 | |
| USD 1601–USD 2000 | −0.15 | 0.87 | 0.86 | 0.15 | 4.82 | |
| USD 2001 or more | 0 | - | 1 | - | - | |
| Variable | Category | Estimate | p-Value | Odds Ratio | 95% Confidence Intervals | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Air pollution (visual) | Not at all polluted | −0.38 | 0.61 | 0.69 | 0.16 | 2.95 |
| Slightly polluted | −0.56 | 0.32 | 0.57 | 0.18 | 1.74 | |
| Moderately polluted | 0.22 | 0.69 | 1.25 | 0.41 | 3.82 | |
| Very polluted | 0 | - | 1 | - | - | |
| Air pollution (unpleasant odors) | Never | 1.70 | 0.02 ** | 5.49 | 1.34 | 22.46 |
| Rarely | 0.39 | 0.47 | 1.49 | 0.52 | 4.25 | |
| Sometimes | 1.14 | 0.04 ** | 3.13 | 1.09 | 8.97 | |
| Always | 0a | - | 1 | - | - | |
| Noises affecting well-being | Never | 1.69 | 0.00 *** | 5.46 | 1.65 | 18.07 |
| Rarely | 0.24 | 0.52 | 1.27 | 0.60 | 2.65 | |
| Sometimes | 0.16 | 0.63 | 1.17 | 0.61 | 2.23 | |
| Always | 0 | - | 1 | - | - | |
| Healthcare services quality | Not at all efficient | −1.78 | 0.02 ** | 0.17 | 0.04 | 0.74 |
| A little efficient | −1.69 | 0.01 ** | 0.18 | 0.05 | 0.66 | |
| Moderately efficient | −0.78 | 0.24 | 0.46 | 0.13 | 1.62 | |
| Very efficient | 0 | - | 1 | - | - | |
| Sex | Female | 0.04 | 0.89 | 1.04 | 0.59 | 1.85 |
| Male | 0 | - | 1 | - | - | |
| Age | 18–24 | 0.27 | 0.66 | 1.32 | 0.40 | 4.34 |
| 25–34 | −0.99 | 0.09 * | 0.37 | 0.12 | 1.16 | |
| 35–44 | 0.51 | 0.43 | 1.67 | 0.47 | 5.92 | |
| 45–54 | 0.46 | 0.51 | 1.58 | 0.41 | 6.02 | |
| >54 | 0 | - | 1 | - | - | |
| Education | Basic | 3.87 | 0.00 *** | 47.94 | 3.44 | 668.73 |
| High school | 0.20 | 0.71 | 1.22 | 0.43 | 3.45 | |
| Higher education | −0.19 | 0.64 | 0.83 | 0.38 | 1.81 | |
| Postgraduate studies | 0 | - | 1 | - | - | |
| Marital status | Single | 2.69 | 0.06 * | 14.70 | 0.92 | 233.69 |
| Married | 2.33 | 0.11 | 10.28 | 0.617 | 171.46 | |
| Divorced | 2.89 | 0.07 * | 17.93 | 0.844 | 380.84 | |
| Widow | 0 | - | 1 | - | - | |
| Income | USD 0–USD 400 | −1.19 | 0.12 | 0.30 | 0.07 | 1.28 |
| USD 401–USD 800 | −0.78 | 0.29 | 0.458 | 0.11 | 1.86 | |
| USD 801–USD 1200 | 0.77 | 0.33 | 2.16 | 0.49 | 9.43 | |
| USD 1201–USD 1600 | −0.71 | 0.37 | 0.489 | 0.110 | 2.168 | |
| USD 1601–USD 2000 | −0.24 | 0.77 | 0.79 | 0.16 | 3.95 | |
| USD 2001 or more | 0 | - | 1 | - | - | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrera, C.; Cabrera-Barona, P. Impact of Perceptions of Air Pollution and Noise on Subjective Well-Being and Health. Earth 2022, 3, 825-838. https://doi.org/10.3390/earth3030047
Herrera C, Cabrera-Barona P. Impact of Perceptions of Air Pollution and Noise on Subjective Well-Being and Health. Earth. 2022; 3(3):825-838. https://doi.org/10.3390/earth3030047
Chicago/Turabian StyleHerrera, Carolina, and Pablo Cabrera-Barona. 2022. "Impact of Perceptions of Air Pollution and Noise on Subjective Well-Being and Health" Earth 3, no. 3: 825-838. https://doi.org/10.3390/earth3030047
APA StyleHerrera, C., & Cabrera-Barona, P. (2022). Impact of Perceptions of Air Pollution and Noise on Subjective Well-Being and Health. Earth, 3(3), 825-838. https://doi.org/10.3390/earth3030047






