Abstract
Chronic non-specific low back pain (CNLBP) affects a significant percentage of the global population, with therapeutic exercise being a key management strategy. This study evaluated the effectiveness of the clinical Pilates method in 22 patients with CNLBP. Lumbar spine range of motion (ROM) and completion times for three functional tests (prone plank, side bridge, and supine bridge) were measured before and after a six-week rehabilitation program. Motion data were collected using two inertial measurement units. Results showed statistically significant improvements in kinematic patterns, execution times, and ROM. These findings support the effectiveness of clinical Pilates in improving lumbar spine functionality and patient outcomes.
1. Introduction
Chronic non-specific low back pain (CNLBP) is a widely prevalent condition [1] that is strongly associated with disability and work absences globally [2,3]. Although the causes of CNLBP are complex and multifactorial, they are directly linked to etiological factors including social and demographic characteristics, lifestyle habits, and both physical and psychosocial influences [4].
Lumbar muscle atrophy, reduced strength and endurance, and increased fatigue are commonly observed in association with CNLBP. The stability of the core muscles, which depends on both performance and coordination, is a crucial element in assessing these patients. The supine bridge, prone bridge, and side bridge tests (left and right) are among the most frequently used methods for evaluating core muscle strength and stability [5]. While these tests provide valuable information for patient evaluation, quantitative measurements of the lumbar spine kinematics during these assessments remain limited. CNLBP patients establish a distinctive and unique lumbar motion signature by completing standardized multiplanar, lumbar-specific functional motion tasks. The motion signature is composed of the three-dimensional (3D) lumbar range of motion. In combination, these lumbar-specific motion signature datasets offer an insight into the patients’ musculoskeletal system and can be used as measures of functional health [6].
Inertial measurement units (IMUs) are reliable for capturing the kinematic data associated with movement patterns in these clinical tests [5]. These devices are increasingly integrated into routine clinical practice, with the literature supporting their reliability and validity in assessing lumbar spine kinematics [5].
According to current guidelines for managing chronic non-specific low back pain, interventions for this patient population should include a structured therapeutic exercise program [7]. Therapeutic exercise aids in restoring the functionality of these patients [8,9], as it is a targeted form of exercise that has been shown to alleviate pain and reduce disability [10]. Quantitative data are essential for evaluating the effectiveness of therapeutic exercise programs. The validated accuracy of IMU devices makes them well-suited for assessing kinematics as they capture three-dimensional movement data [5,11].
Several studies have shown that clinical Pilates reduces pain and improves functionality [12,13,14,15,16,17]. The objective of this study was to evaluate the efficacy of clinical Pilates in enhancing the functional capacity of patients with CNLBP. To achieve this, we incorporated the quantitative metrics obtained from IMUs with three clinical assessment tests: the supine bridge test (SUBT), the side bridge test (SBT), and the prone plank bridge test (PBT). This is the first time, to the extent of our knowledge, that the lumbar motion signature, a critical indicator of functional health, has been combined with functional test data to assess the efficacy of rehabilitation programs from a detailed biomechanical perspective.
2. Materials and Methods
A total of 41 individuals (14 males and 27 females) identified as having chronic low back pain were originally screened. The inclusion criteria comprised the existence of non-specific lumbar spine pain persisting for over 6 months, the absence of pathological radiological findings on MRI of the lumbar spine, negative neurodynamic tests of the lower limbs, and positive response to the written consent form. Exclusion criteria included chronic low back pain resulting from structural or abnormal spinal disorders (spondylolysis, spondylolisthesis, scoliosis, bone fractures, neurological symptoms) and pathologies such as cancer or kidney disease associated with reported low back pain originating from the spine.
Seven patients were excluded from the study due to hip pain, one due to spondylolysis, four due to radiological findings of scoliosis deformity, one due to spinal fracture in the past, one due to osteoporosis, and four due to the presence of spondyloarthropathy in the lumbar spine (Modic type II).
A total of 22 patients with non-specific low back pain participated in this study, comprising 8 men and 14 women.
The lower spine’s range of motion (ROM) was measured during the course of four functional tests: the bridge test in both supine and prone postures, and the side bridge test from the right and left sides. Two MetaMotionR+ inertial measurement units (IMUs) were employed to evaluate the movement characteristics of the lumbar spine. The MetaMotionR+ is engineered for the acquisition and transmission of sensory data and carries CE certification. The raw data are recorded and transmitted at 400 Hz and 100 Hz, respectively, via Bluetooth. The raw data were captured and transferred at frequencies of 400 Hz and 100 Hz, respectively, using Bluetooth. Two clinicians acquired and examined the CSV file with the data on a local computer. The data synthesis combined information from a 3D gyroscope, a 3D magnetometer, and a 3D accelerometer to generate a stable directional position system known as quaternion or Euler angles. Furthermore, the sophisticated software seamlessly integrated the raw data from the three devices to optimize the performance of each. This approach encompassed displacement correction algorithms for each sensor, status monitoring for standardization, and the use of a Kalman filter to yield reliable and accurate direction values. The MMR+ is a scientifically validated apparatus utilized for capturing human movement data and the monitoring of movement patterns. A list of its technological features includes:
- 6-axis accelerometer BMI160 + gyroscope;
- LTR-329ALS ambient light sensor;
- 3-axis magnetometer BMM150;
- 9-axis sensor fusion by BOSCH;
- 8 MB memory;
- Rechargeable lithium-ion battery;
- Vibration motor;
- Low-power Bluetooth, CPU, power button, LED, and GPIO.
A Bluetooth unit integrated into each IMU wirelessly transmitted the data to the patient’s smartphone. The IMUs and Bluetooth units were powered by a 3.6V battery. The data collection process included six distinct phases.
2.1. Phase 1—Calibration
Accurate movement capture using an IMU needs the correct alignment between the device’s reference frame and the body’s orientation. Prior to installation and activation, the units were calibrated on a level horizontal plane to ensure that each unit maintained an identical starting position in accordance with the coordinates of the Cartesian system. Adhering to a strict calibration procedure is essential for acquiring trustworthy data. Calibration was conducted using the Metawear application installed on a smartphone (MbientLab Inc., 2758 Lantz ave San Jose, CA 95124, USA. software version 2.0.1).
2.2. Phase 2—Unit Installation
The sensors were placed to precisely identify the orientation and location of the device frame according to the natural movement axis of the lumbar spine joints. The first sensor was positioned on the L1 spinous process, and the second on the L5 spinous process. Both units were attached to the skin using non-allergenic two-sided adhesive tape.
2.3. Phase 3—Bluetooth Protocol and Data Transmission
Subsequent to each recording of the specified functional tests, the acquired data were transferred over Bluetooth to a computer for further analysis. The analysis included pre- and post-filtering of the accelerometer, gyroscope, and magnetometer’s three-dimensional data in the sensors’ local coordinate system.
2.4. Phase 4—Initial Recording Observation
Despite the accuracy of the portable devices and the use of the root mean square error (RMSE), a computer-based body model allows the clinician to verify the correctness of motion reconstruction and data acquisition. Should inaccuracies or erroneous motion records be identified, the process of calibration and measurements would need to be reiterated to guarantee the capture of representative data.
2.5. Phase 5—Data Collection for Functional Tests
Following a successful initial testing, the patients were instructed to execute the four functional bridge assessments. Each participant received detailed directions concerning the process and conducted two practice trials prior to the actual data collection.
The smartphone was kept adjacent to them during the measurement process to avert signal connection issues while capturing and transferring data from the units to the smartphone. Upon completion of the data collection, the clinical physical therapist detached the sensors from the patients and shared the data obtained from the smartphone to the computer.
2.6. Clinical Pilates Intervention Program
The intervention program consisted of exercises aimed at strengthening the transverse abdominis, rectus abdominis, upper body muscles, erector spinae, hip muscles, and glutes. Specifically, the exercises included the following:
Hundreds lvl 1, Clam lvl 1, Single leg stretch lvl 1, lvl 2, Side kick lvl 1, lvl 2, Double leg stretch lvl 1, Side lift adduction lvl 1, Scissors lvl 1, lvl 2, Dart lvl 1, Single leg circle lvl 1, Swan dive lvl 1, Shoulder bridge lvl 1, Swimming lvl 1, lvl 2, Hip twist lvl 1, lvl 2.
The intensity of the exercises was determined as follows:
Exercises at stage 1 (lvl 1) were primarily easy and performed in a single-axis direction. Following these were exercises at stage 2 (lvl 2), which were more challenging than those at stage 1 due to additional movement steps (cognitively demanding), but still performed in a single-axis direction [8].
It is important to emphasize that all exercises began at stage 1 difficulty and progressively increased to stage 2 as each individual gained good control and stabilization.
The therapeutic exercise program was conducted three times a week for a duration of 6 weeks.
3. Results
For the statistical analysis, an independent samples t-test was used with a one-tailed approach and allowance for unequal variances (heteroscedasticity) between the two samples. The study’s statistical power was calculated using G*Power 3.1.9.7 software for Windows (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany). A power analysis for two independent means was performed with a significance level of α = 0.05. The statistical power related to sample size and the observed effect size exceeded 80% for each variable (92.7% for the prone bridge test, 89.3% for the left side bridge test, and nearly maximal at 98.3% for both the supine and right-side bridge tests).
The intraclass correlation coefficient (ICC, two-way random, absolute agreement) with the corresponding 95% confidence interval was used to assess the relative reliability, providing insight into the consistency of within-session measurements across all bridge tests and clinical passive range of motion assessments (ICC > 0.90).
3.1. Supine Bridge Test (SBT)
The position achieved during the performance of the supine bridge test involved lumbar spine extension (compared with the anatomical position), with a mean extension of 11.86 and a standard deviation of 1.80 before the start, and a mean extension of 14.27 and a standard deviation of 1.33 after the completion of the therapeutic exercise program (p-value = 0.0003) (Figure 1).
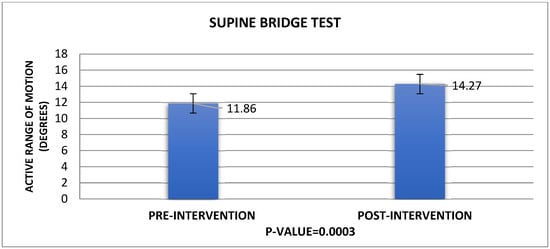
Figure 1.
Kinematic results of the supine bridge test.
3.2. Prone Bridge Test (PBT)
The position achieved during the performance of the prone bridge test involved lumbar spine extension (compared with the anatomical position), with a mean extension of 6.23 and a standard deviation of 2.36 before the start, and a mean extension of 3.95 and a standard deviation of 1.17 after the completion of the therapeutic exercise program (p-value = 0.001) (Figure 2).
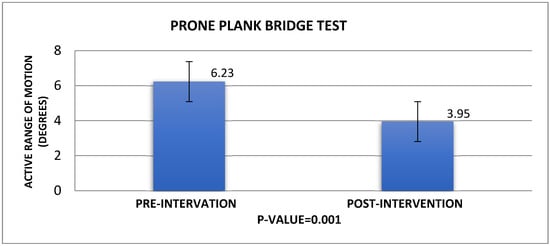
Figure 2.
Kinematic results of the prone plank bridge test.
3.3. Side Bridge Test Left (SBTL)
The position achieved during the performance of the left side bridge test involved right lateral flexion of the lumbar spine (compared with the anatomical position), with a mean value of 3.96 and a standard deviation of 1.19 before the start, and a mean value of 2.47 and a standard deviation of 1.21 after the completion of the therapeutic exercise program (p-value = 0.0004) (Figure 3).
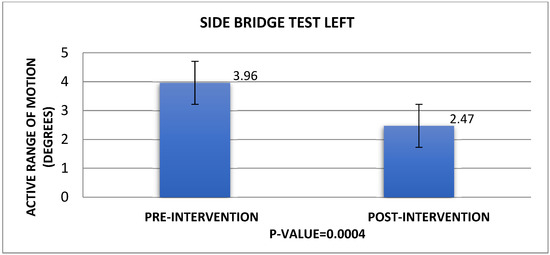
Figure 3.
Kinematic results of the side bridge test (left).
3.4. Side Bridge Test Right (SBTR)
The position achieved during the performance of the right-side bridge test involved left lateral flexion of the lumbar spine (compared with the anatomical position), with a mean value of 3.52 and a standard deviation of 0.81 before the start and a mean value of 2.27 and a standard deviation of 1.49 after the completion of the therapeutic exercise program (p-value = 0.00001) (Figure 4).
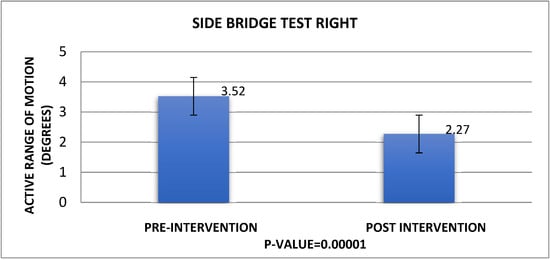
Figure 4.
Kinematic results of the side bridge test (right).
3.5. Wearable Sensors—Functional Test Duration Data
A statistically significant improvement was observed in the time that the final position was maintained in all tests (and was not abandoned due to pain or fatigue). Specifically, during the performance of the supine bridge test, patients maintained the final position for 72.3/±29.43 (mean value (s)/±standard deviation) before the intervention, while after the intervention, the recorded values increased to 162.5/±31.24 (mean value (s)/±standard deviation), p-value = 0.001.
During the performance of the prone bridge test, patients maintained the final position for 34.31/±20.51 (mean value (s)/±standard deviation) before the intervention, increasing these values after the intervention to 65.3/±25.45 (mean value (s)/±standard deviation), p-value = 0.00003.
Regarding the performance of the left side bridge test, the recorded values for the final position were 10.2/±8.49 (mean value (s)/±standard deviation) before the intervention, while after the intervention, the values improved to 27.42/±4.33 (mean value (s)/±standard deviation), p-value = 0.002.
Finally, during the performance of the right-side bridge test, the recorded values for the final position were 9.22/±7.34 (mean value (s)/±standard deviation) before the intervention and 29.19/±4.45 (mean value (s)/±standard deviation) after the intervention, respectively, p-value = 0.0001 (Table 1).

Table 1.
Time results pre- and post-intervention for each assessment test.
4. Discussion
This study explored the effectiveness of clinical Pilates intervention for individuals with chronic non-specific low back pain, focusing on improvements in lumbar spine functionality and mobility. CNLBP is among the most prevalent musculoskeletal conditions globally, significantly diminishing quality of life due to the pain and functional limitations it causes. Key factors influencing the condition’s progression include psychosocial and physical elements and the reduced endurance of core muscles [17].
In this context, clinical Pilates therapeutic exercises offer a personalized approach to reduce pain and enhance physical function [1]. Clinical Pilates has shown greater effectiveness than other treatments, such as pharmacotherapy and traditional lumbar stabilization exercises, in addressing CNLBP [18,19,20,21]. This study used inertial measurement units (IMUs) to accurately record lumbar spine movements during four functional bridge tests in various positions: supine, prone, and side bridges (right and left). IMUs provided precise data on lumbar spine mobility across three axes, contributing to a reliable assessment of movement [5,22,23,24].
The study’s results demonstrated significant enhancements in hold duration and lumbar spine mobility subsequent to the intervention.
The findings indicated increased lumbar extension, decreased flexion, and greater ability to sustain proper trunk position during the tests. These outcomes suggest improved muscular endurance and superior spinal muscle control.
Moreover, women exhibited increased susceptibility to CNLBP [25,26,27,28], while individuals with a higher BMI presented greater vulnerability to the condition [29].
The study’s limitations included a limited sample size and potential IMU errors, possibly due to skin movement (artifacts) [5,30,31,32]. Despite these limitations, the findings suggest that clinical Pilates interventions are beneficial in the management of CNLBP, highlighting the necessity for additional research to determine optimal exercise protocols and evaluate the intervention’s efficacy across various age groups [33].
5. Conclusions
Therapeutic exercise, particularly clinical Pilates, has been proven to be effective in alleviating pain and enhancing functional capacity in individuals with CNLBP, as supported by the existing literature [19,34]. This study further validates these outcomes through temporal and kinematic data collected via IMUs, which, due to their compact size, ease of use, and mobility features, provide reliable and objective assessment data for various clinical tests [5]. Following a six-week intervention, notable improvements were observed in spinal mobility and core muscle endurance. Ongoing research is essential to examine the applications of wearable sensors in chronic conditions combined with surface electromyography [35] to assess the long-term effects and specific types of therapeutic exercise.
Author Contributions
Conceptualization, N.M.T., E.F., A.T. and G.P.; Methodology, N.M.T., E.F., A.T., M.K., P.G. and G.P.; Software, N.M.T., E.F., P.G. and G.P.; Validation, N.M.T., E.F., A.T. and M.K.; Formal analysis, N.M.T., E.F. and G.P.; Investigation, N.M.T., E.F., A.T., M.K., P.G. and G.P.; Resources, N.M.T., E.F. and A.T.; Data curation, N.M.T., E.F., M.K. and P.G.; Writing—original draft preparation, N.M.T., E.F., A.T. and G.P.; Writing—review and editing, N.M.T., E.F., A.T., M.K., P.G. and G.P.; Supervision, N.M.T., E.F., A.T. and G.P.; Project administration, N.M.T., E.F. and G.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of the University of Peloponnese and approved by the Research Ethics Committee of the School of Health Sciences, University of Peloponnese (protocol code 6367 and date of approval 19 March 2024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent was obtained from the patients to publish this paper.
Data Availability Statement
The data of this research could be made available upon request.
Acknowledgments
We would like to thank our supervisor Georgios Papagiannis as well as Athanasios Triantafyllou, Maria Kyriakidou, and Panagiotis Gkrilias for their support and assistance.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef]
- Waddell, G. The Back Pain Revolution, 2nd ed; Elsevier Health Sciences: London, UK, 2004. [Google Scholar]
- Papagiannis, G.I.; Triantafyllou, A.I.; Konstantina, Y.G.; Koulouvaris, P.; Anastasiou, A.; Papadopoulos, E.C.; Papagelopoulos, P.J.; Babis, G.C. Biomechanical Factors could Affect Lumbar Disc Reherniation after Microdiscectomy. J. Orthop. Sports Med. 2019, 1, 46–50. [Google Scholar] [CrossRef]
- Manchikanti, L. Epidemiology of low back pain. Pain Physician 2000, 3, 167–192. [Google Scholar] [CrossRef] [PubMed]
- Triantafyllou, A.; Papagiannis, G.; Stasi, S.; Gkrilias, P.; Kyriakidou, M.; Kampouroglou, E.; Skouras, A.-Z.; Tsolakis, C.; Georgoudis, G.; Savvidou, O.; et al. Lumbar Kinematics Assessment of Patients with Chronic Low Back Pain in Three Bridge Tests Using Miniaturized Sensors. Bioengineering 2023, 10, 339. [Google Scholar] [CrossRef] [PubMed]
- Hani, H.; Souchereau, R.; Kachlan, A.; Harris, H.; Dufour, J.; Aurand, A.; Mageswaran, P.; Hyer, M.; Marras, W. Reliability of a Wearable Motion System for Clinical Evaluation of Dynamic Lumbar Spine Function. Adv. Complement. Altern. Med. 2022, 7, 672–683. [Google Scholar] [CrossRef] [PubMed]
- Eliks, M.; Zgorzalewicz-Stachowiak, M.; Zeńczak-Praga, K. Application of Pilates-based exercises in the treatment of chronic non-specific low back pain: State of the art. Postgrad. Med. J. 2019, 95, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Kwok, B.C.; Lim, J.X.L.; Kong, P.W. The Theoretical Framework of the Clinical Pilates Exercise Method in Managing Non-Specific Chronic Low Back Pain: A Narrative Review. Biology 2021, 10, 1096. [Google Scholar] [CrossRef]
- Valenza, M.C.; Rodríguez-Torres, J.; Cabrera-Martos, I.; Díaz-Pelegrina, A.; Aguilar-Ferrándiz, M.E.; Castellote-Caballero, Y. Results of a Pilates exercise program in patients with chronic non-specific low back pain: A randomized controlled trial. Clin. Rehabil. 2017, 31, 753–760. [Google Scholar] [CrossRef]
- Silva, M.L.D.; Miyamoto, G.C.; Franco, K.F.M.; Franco, Y.R.D.S.; Cabral, C.M.N. Different weekly frequencies of Pilates did not accelerate pain improvement in patients with chronic low back pain. Braz. J. Phys. Ther. 2020, 24, 287–292. [Google Scholar] [CrossRef]
- Glowinski, S.; Blazejewski, A.; Krzyzynski, T. Inertial Sensors and Wavelets Analysis as a Tool for Pathological Gait Identification. In Innovations in Biomedical Engineering; Advances in Intelligent Systems and Computing; Gzik, M., Tkacz, E., Paszenda, Z., Piętka, E., Eds.; Springer: Cham, Switzerland, 2017; Volume 526. [Google Scholar] [CrossRef]
- Amaral, S.; Pássaro, A.C.; Casarotto, R.A. Effect of the association of continuous shortwave diathermy and Pilates-based exercises on pain, depression, and anxiety in chronic non-specific low back pain: A randomized clinical trial. Braz. J. Med. Biol. Res. 2023, 56, e12338. [Google Scholar] [CrossRef]
- Bhadauria, E.A.; Gurudut, P. Comparative effectiveness of lumbar stabilization, dynamic strengthening, and Pilates on chronic low back pain: Randomized clinical trial. J. Exerc. Rehabil. 2017, 13, 477–485. [Google Scholar] [CrossRef]
- Cruz-Díaz, D.; Romeu, M.; Velasco-González, C.; Martínez-Amat, A.; Hita-Contreras, F. The effectiveness of 12 weeks of Pilates intervention on disability, pain and kinesiophobia in patients with chronic low back pain: A randomized controlled trial. Clin. Rehabil. 2018, 32, 1249–1257. [Google Scholar] [CrossRef] [PubMed]
- Natour, J.; Cazotti Lde, A.; Ribeiro, L.H.; Baptista, A.S.; Jones, A. Pilates improves pain, function and quality of life in patients with chronic low back pain: A randomized controlled trial. Clin. Rehabil. 2015, 29, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Wajswelner, H.; Metcalf, B.; Bennell, K. Clinical pilates versus general exercise for chronic low back pain: Randomized trial. Med. Sci. Sports Exerc. 2012, 44, 1197–1205. [Google Scholar] [CrossRef] [PubMed]
- McGill, S.M.; Childs, A.; Liebenson, C. Endurance times for low back stabilization exercises: Clinical targets for testing and training from a normal database. Arch. Phys. Med. Rehabil. 1999, 80, 941–944. [Google Scholar] [CrossRef]
- Owen, P.J.; Miller, C.T.; Mundell, N.L.; Verswijveren, S.J.J.M.; Tagliaferri, S.D.; Brisby, H.; Bowe, S.J.; Belavy, D.L. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br. J. Sports Med. 2020, 54, 1279–1287. [Google Scholar] [CrossRef]
- Hayden, J.A.; Wilson, M.N.; Stewart, S.; Cartwright, J.L.; Smith, A.O.; Riley, R.D.; van Tulder, M.; Bendix, T.; Cecchi, F.; Costa, L.O.P.; et al. Exercise treatment effect modifiers in persistent low back pain: An individual participant data meta-analysis of 3514 participants from 27 randomised controlled trials. Br. J. Sports Med. 2020, 54, 1277–1278. [Google Scholar] [CrossRef]
- Fernández-Rodríguez, R.; Álvarez-Bueno, C.; Cavero-Redondo, I.; Torres-Costoso, A.; Pozuelo-Carrascosa, D.P.; Reina-Gutiérrez, S.; Pascual-Morena, C.; Martínez-Vizcaíno, V. Best Exercise Options for Reducing Pain and Disability in Adults With Chronic Low Back Pain: Pilates, Strength, Core-Based, and Mind-Body. A Network Meta-analysis. J. Orthop. Sports Phys. Ther. 2022, 52, 505–521. [Google Scholar] [CrossRef]
- Shi, J.; Hu, Z.Y.; Wen, Y.R.; Wang, Y.F.; Lin, Y.Y.; Zhao, H.Z.; Lin, Y.T.; Wang, Y.L. Optimal modes of mind-body exercise for treating chronic non-specific low back pain: Systematic review and network meta-analysis. Front. Neurosci. 2022, 16, 1046518. [Google Scholar] [CrossRef]
- Ha, T.H.; Saber-Sheikh, K.; Moore, A.P.; Jones, M.P. Measurement of lumbar spine range of movement and coupled motion using inertial sensors—A protocol validity study. Man. Ther. 2013, 1, 87–91. [Google Scholar] [CrossRef]
- Gombatto, S.P.; Collins, D.R.; Sahrmann, S.A.; Engsberg, J.R.; Van Dillen, L.R. Patterns of lumbar region movement during trunk lateral bending in 2 subgroups of people with low back pain. Phys. Ther. 2007, 87, 441–454. [Google Scholar] [CrossRef] [PubMed]
- Van Dillen, L.R.; Gombatto, S.P.; Collins, D.R.; Engsberg, J.R.; Sahrmann, S.A. Symmetry of timing of hip and lumbopelvic rotation motion in 2 different subgroups of people with low back pain. Arch. Phys. Med. Rehabil. 2007, 88, 351–360. [Google Scholar] [CrossRef]
- WHO Guideline for Non-Surgical Management of Chronic Primary Low Back Pain in Adults in Primary and Community Care Settings. World Health Organization: Geneva, Switzerland, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK599212/ (accessed on 19 April 2024).
- Mazzarino, M.; Kerr, D.; Wajswelner, H.; Morris, M.E. Pilates Method for Women’s Health: Systematic Review of Randomized Controlled Trials. Arch. Phys. Med. Rehabil. 2015, 96, 2231–2242. [Google Scholar] [CrossRef] [PubMed]
- García-Garro, P.A.; Hita-Contreras, F.; Martínez-Amat, A.; Achalandabaso-Ochoa, A.; Jiménez-García, J.D.; Cruz-Díaz, D.; Aibar-Almazán, A. Effectiveness of A Pilates Training Program on Cognitive and Functional Abilities in Postmenopausal Women. Int. J. Environ. Res. Public Health 2020, 17, 3580. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Rodríguez, R.; Alvarez-Bueno, C.; Reina-Gutiérrez, S.; Torres-Costoso, A.; Nuñez de Arenas-Arroyo, S.; Martínez-Vizcaíno, V. Effectiveness of Pilates and Yoga to improve bone density in adult women: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0251391. [Google Scholar] [CrossRef]
- Zhang, T.T.; Liu, Z.; Liu, Y.L.; Zhao, J.J.; Liu, D.W.; Tian, Q.B. Obesity as a Risk Factor for Low Back Pain: A Meta-Analysis. Clin. Spine Surg. 2018, 31, 22–27. [Google Scholar] [CrossRef]
- Xi, X.; Ling, Z.; Wang, C.; Gu, C.; Zhan, X.; Yu, H.; Lu, S.; Tsai, T.Y.; Yu, Y.; Cheng, L. Lumbar segment-dependent soft tissue artifacts of skin markers during in vivo weight-bearing forward-Backward bending. Front. Bioeng. Biotechnol. 2022, 10, 960063. [Google Scholar] [CrossRef]
- Zemp, R.; List, R.; Gülay, T.; Elsig, J.P.; Naxera, J.; Taylor, W.R.; Lorenzetti, S. Soft tissue artefacts of the human back: Comparison of the sagittal curvature of the spine measured using skin markers and an open upright MRI. PLoS ONE 2014, 9, e95426. [Google Scholar] [CrossRef]
- Fotaki, A.; Triantafyllou, A.; Papagiannis, G.; Stasi, S.; Georgios, P.; Olga, S.; Koulouvaris, P. The science of biomechanics can promote dancers’ injury prevention strategies. Phys. Ther. Rev. 2020, 26, 94–101. [Google Scholar] [CrossRef]
- Beatriz, M. Musculoskeletal spine pain in adolescents: Epidemiology of non-specific neck and low back pain and risk factors. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2020, 25, 776–780. [Google Scholar] [CrossRef]
- Miyamoto, G.C.; Lin, C.C.; Cabral, C.M.N.; van Dongen, J.M.; van Tulder, M.W. Cost-effectiveness of exercise therapy in the treatment of non-specific neck pain and low back pain: A systematic review with meta-analysis. Br. J. Sports Med. 2019, 53, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Papagiannis, G.I.; Roumpelakis, I.M.; Triantafyllou, A.I.; Makris, I.N.; Babis, G.C. Response to Letter to the Editor on “No Differences Identified in Transverse Plane Biomechanics between Medial Pivot and Rotating Platform Total Knee Implant Designs”. J. Arthroplast. 2016, 31, 2373. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).