Abstract
This study proposes the adoption of the IoT technology for the home monitoring of the health status of frail patients. Such a solution is thought to be part of the forthcoming Italian COT; the latter is an organizational model which is devoted to integrate the current national healthcare network. The prevalent deployment model of IoT systems is the Cloud, which offers powerful services and unlimited storage/computing capacity on-demand; unfortunately, connecting smart devices to the Cloud poses severe issues. First of all, connected devices create large volumes of data, which will drive inevitably to performance and network congestion challenges. Secondly, there are security, bandwidth, and reliability concerns that make the Cloud-only solution not suitable for all the potential real-world applications. The Fog computing paradigm has been introduced to bridge the gap between the Cloud and IoT devices. This paper gives a twofold contribution: (a) a Cloud–Fog architecture is proposed using a three-tiers solution where the Fog computing layer constitutes the middle tier; (b) simulations have been carried out in order to compare Cloud–Fog computing as an alternative to the Cloud-only solution. The experimental results demonstrate a remarkable degradation of the latency in the first solution with respect to the second one. The measured benefit indicates that the best way to implement the COTs consists in placing inside them the fog layer mentioned above. The iFogSim open-source toolkit has been used to carry out the experiments.
1. Introduction
People aged above 65 years old amount to 702.9 million in 2019, projected to reach 1548.9 million in 2050; while people aged above 80 years old amount to 53.9 million in 2019, projected to reach 109.1 million in 2050 [1]. The increasing aging of the population all over the world determines the need for constant monitoring and assistance to those people which, in turn, causes a huge financial and human burden on health centers, families and caregivers. In Europe, “On average, 26.6% of people aged 65 or over and 39.4% aged 75 or over living at home need long-term care. The number of all people potentially in need of long-term care across the European Union […] stands at 30.8 million people and is projected […] to rise 38.1 million by 2050” [2].
In Italy, compared to almost 6 million elderly people suffering from serious and disabling chronic diseases, only 1 million are taken care of by the National Health Service (source: https://www.italialongeva.it/aree-tematiche/long-term-care/, accessed on 11 September 2022).
Principle 18 (Long-term care) of the European Pillar of Social Rights spells out as follows: “Everyone has the right to affordable long-term care services of good quality, in particular home-care and community-based services.” (Source: //ec.europa.eu/info/sites/default/files/social-summit-european-pillar-social-rights-booklet_en.pdf, accessed on 11 September 2022). In order to implement the previous ambitious goal, today most developed countries are engaged in the creation of an IT technological infrastructure devoted to increase the remote assistance service for elderly patients. In Italy, the orientation of the Ministry of Health is to strengthen the so-called Local Operational Centres (Italian name: Centrali Operative Territoriali—COT. In the remainder of this paper we use the COT acronym to refer to them). The COTs have been formally introduced in the network of the Italian health organization in May 2020 by the Law Decree n. 342 (Art.1, comma 8), just after the explosion of the COVID-19 pandemic. The purpose of the COTs is to ensure continuity, accessibility and integration of the Italian social health care service. By law 1 COT is linked to 100,000 inhabitants. Thanks to the financial support of the European Commission, the Italian Government has lunched the National Recovery and Resilience Plan (NRRP). According to such a plan, by the end of 2026 at least 600 COTs will have to be created in Italy for an expense of 280 million. For example, 101 COTs are scheduled for the Lombardy region since it has about 10 million inhabitants. The Decree Law n. 77/2022 of the Ministry of Health has set the minimum technological requirements that each COT must meet. In particular, COTs must equip themselves with adequate IT technology for the collection, management and monitoring of citizens’ health data.
Today, the IoT technology is largely considered as the best solution able to offer to the interested stakeholders a remote monitoring service which balances readiness, reliability, and cost. Collection, storage and elaboration of big data sensed by IoT wearables devices are emerging as predictive medical tools for the home monitoring of old people. The adoption of the IoT technology allows to deal with the need of gathering Patient-Generated Health Data (PGHD). The use and sharing of PGHD supplement existing clinical data, filling in gaps in information and providing a more comprehensive picture of ongoing patient health. The use and sharing of PGHD in care delivery and research can: (a) gather data about how patients are doing between medical visits; (b) provide information for use in shared decision-making about preventive and chronic care management; (c) offer potential cost savings and improvements in quality, care coordination, and patient safety. In the US, the mission of the Office of the National Coordinator for Health Information Technology (https://www.healthit.gov/topic/about-onc, accessed on 11 September 2022) is to enhance the state’s health IT infrastructure. The management of PGHD is the primary goal to be achieved.
The prevalent deployment model of IoT systems is the Cloud which offers powerful services and unlimited storage/computing capacity on-demand; unfortunately, connecting smart devices to the Cloud poses severe issues. First of all, connected devices create large volumes of data, which will drive inevitably to network congestion and performance challenges. Secondly, there are security, bandwidth, and reliability concerns that make the Cloud-only solution not suitable for all the potential real-world applications. The Fog computing paradigm has been introduced to bridge the gap between the Cloud and IoT devices [3,4,5].
The remote monitoring of elderly patients is a category of healthcare applications that may require medical reports in near real time for handling critical scenarios especially in chronic diseases, as it is remarked, for instance, in [6]. The present contribution provides evidence, based on measurements, of the fact that the Cloud–Fog method is the architectural solution to be adopted, as an alternative to the usual Cloud-only solution, to manage those situations. So, it is the best solution in the implementation of COTs where the fog nodes have to be installed.
It has been pointed out that cloud and fog computing are on a mutually beneficial, interdependent continuum, where certain functions are more advantageous to carry out in fog nodes, while others are better suited to cloud [7]. The segmentation of what tasks go to fog and what goes to the cloud is application dependent. One of the contributions of the present empirical paper is to set the best way to make such a segmentation with regard to the reference scenario defined above.
In [8], healthcare IoT applications are broadly classified into two categories based on the number of metrics involved: applications based on a single metric (as, for instance, heart rate, blood pressure, glucose level, body temperature, and so on) and applications that use a combination of metrics. The scenario we refer to in this paper concerns elderly wearing five different smart devices each of which senses a single health parameter, so the experimental scenario comprises five applications, each based on a single metric.
Latency is the priority requirement that software applications supporting remote monitoring of elderly subjects must meet. However, today, one of the reasons that hinder widespread adoption of such systems is the high latency rate and network usage in the current cloud-only implementations. Breaking down the values of these parameters is of absolute importance. Other parameters of no less importance in healthcare applications concern the security and privacy of patient data [9], as well as the operational costs. The latter three requirements are out of the scope of the present paper.
The contributions of this paper are two-fold: (a) a Cloud–Fog architecture for an efficient healthcare system for the home monitoring of elderly is proposed using three layers with the fog as the middle tier; (b) simulations are carried out in order to evaluate the responsiveness of the proposed architecture with respect to the latency parameter, as an alternative to the cloud-only implementation of a similar healthcare system. The experimental results demonstrate a remarkable degradation of the latency in the first solution with respect to the second one. The measured benefit indicates that the best way to implement the COTs consists in placing inside them the fog layer mentioned above. The iFogSim open-source toolkit has been used to carry out the experiments.
2. The Adopted Architecture
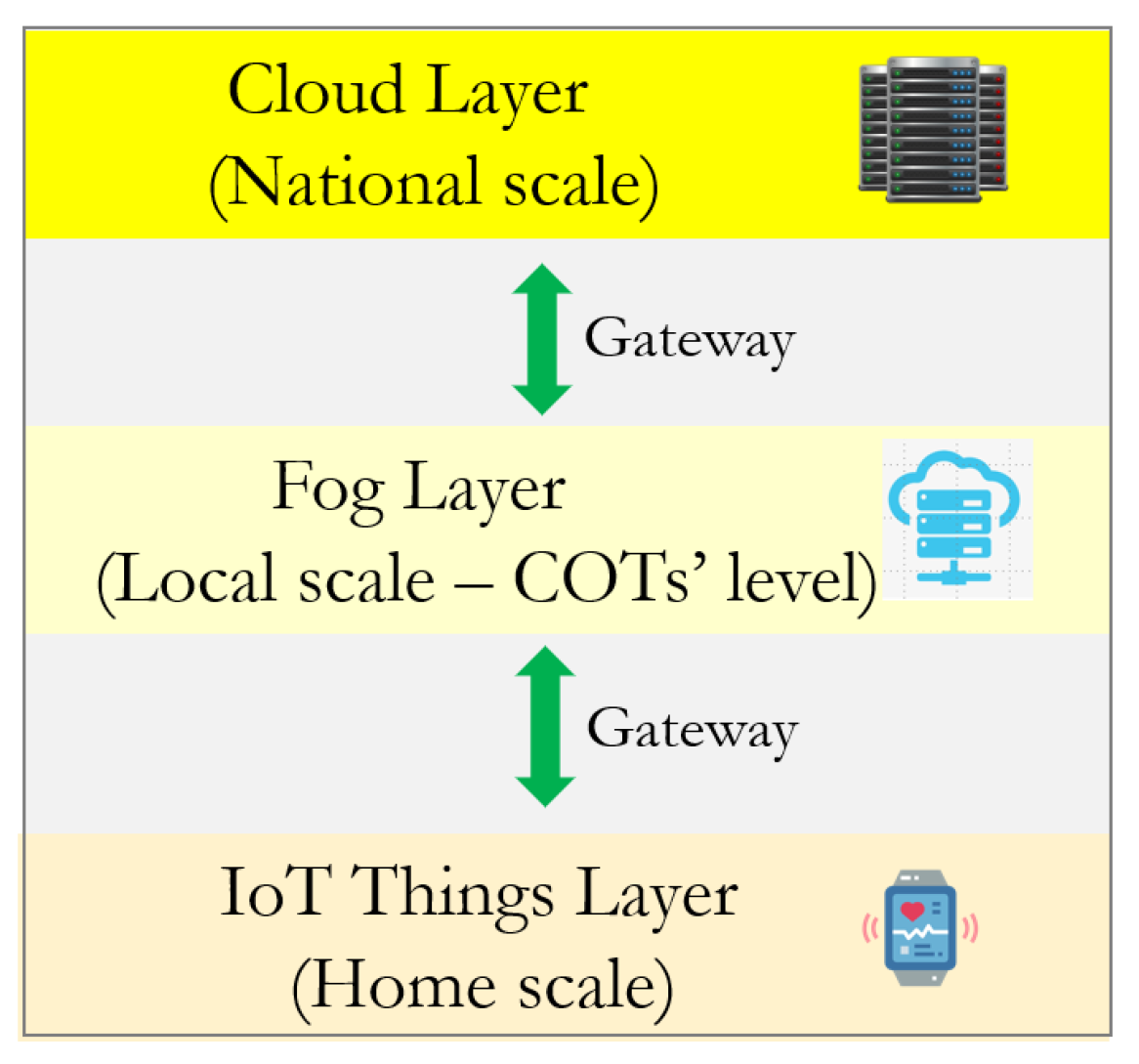
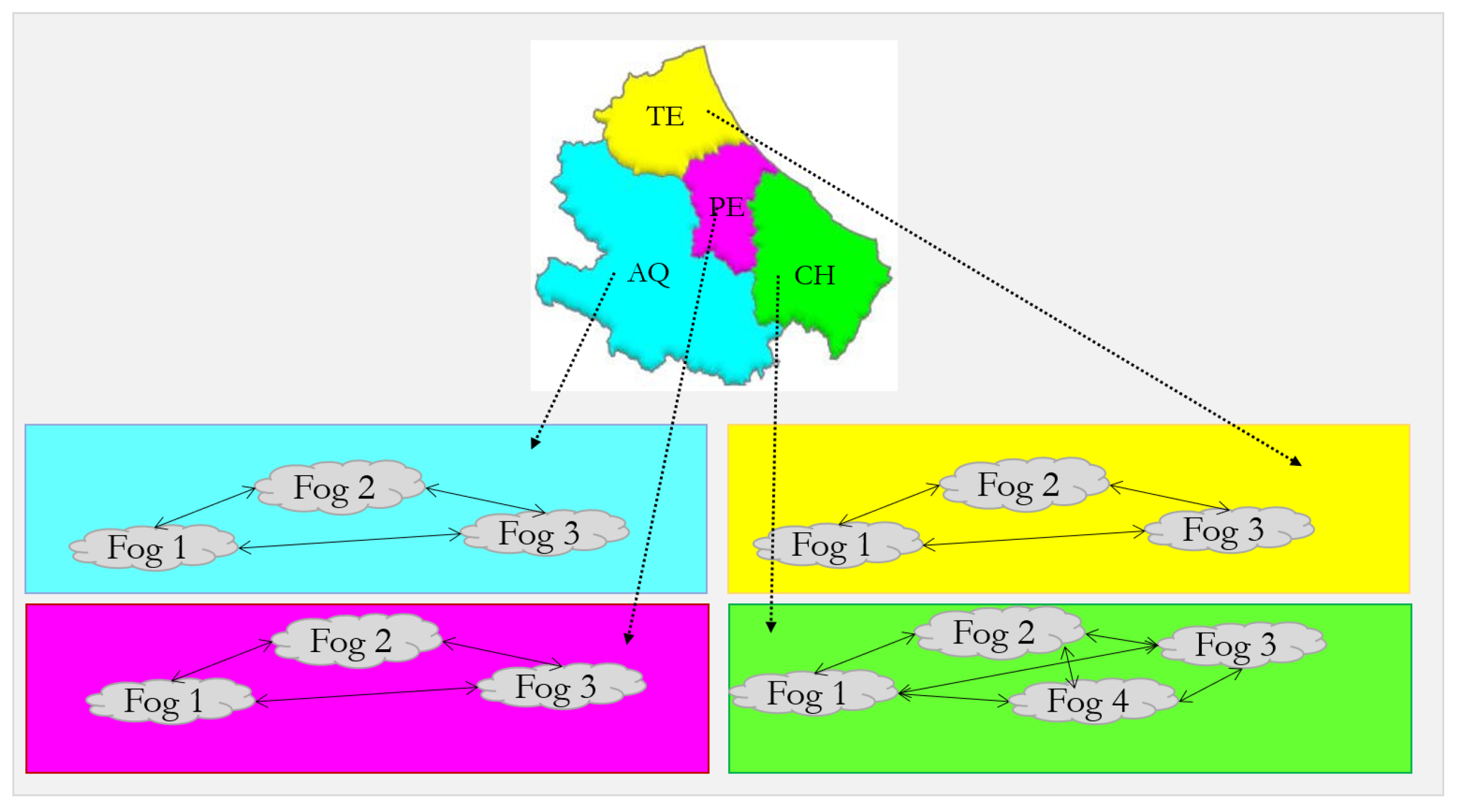
The proposed architecture consists of three layers (Figure 1). The first one contains the biomedical devices that sense the patients’ data in real-time. The second layer is composed of a variable number of fog nodes; each of which receives the data sensed by the devices of a specific remote patient and elaborate them. According to [7], each fog element may comprise fog clusters fulfilling the same functional responsibilities. In our proposal, such a layer implements all the COTs of a given Italian region. As an example, let us refer to the Abruzzo region (the region where the authors of the present paper live). Abruzzo is organized as four provinces: L’Aquila (AQ), Teramo (TE), Pescara (PE), and Chieti (CH). In those provinces live, respectively, 288 K, 300 K, 313 K, and 372 K inhabitants. According to the Law Decree 19 May 2020, n. 342, the Abruzzo will have 13 COTs. In Figure 2 each fog node corresponds to a COT. To fulfill the aimed objectives, the COTs are expected to communicate with each other for exchanging data. In the figure, the logical connections among the fog nodes are shown. Besides horizontal communications, also vertical ones are possible. In the case of COTs, both options are of practical interest.
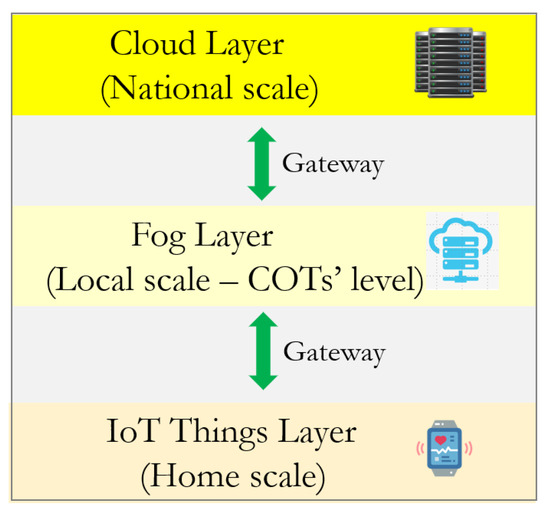
Figure 1.
The three-tier architecture of a Cloud–Fog healthcare system for monitoring home patients.
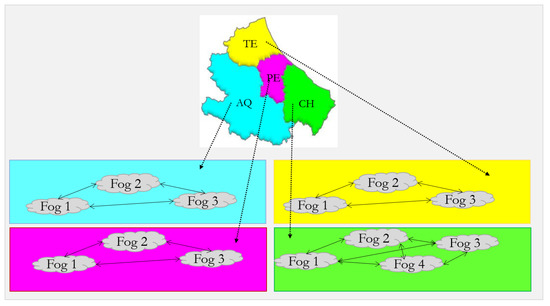
Figure 2.
Implementation of the fog layer for the Abruzzo region.
The third layer of the architecture contains the cloud; it is connected to the fog through a Proxy Server and is responsible for storing and processing the patient data over longer time intervals.
The medical staff responsible for the remote monitoring and care of home patients may interact at the fog and cloud levels.
By removing the middle layer of the architecture of Figure 1, we obtain the usual cloud-based architecture of IoT systems. As already mentioned in Section 1, aim of this short paper is to provide numbers showing that the cloud-only solution is not suitable to implement the scenario of remote monitoring of elderly patients at the region scale.
The measurements made by the devices are collected at the fog node. The latter is also responsible for processing them according to the scheduling specified below. Periodically, or following pre-established events, the data processed at the fog node are sent to the cloud for further processing or just to make it available to stakeholders acting at the national scale.
The proposed architecture is easily scalable. In fact, in an actual scenario where N home patients have to be monitored, the cloud layer remains unaffected, while the remaining two layers changes.
3. The Experimental Set Up
The biomedical devices connected to each home patient are the following. A smartwatch that with its sensors makes the following measurements: heartbeat; blood pressure; blood oxygen level. Biometric sensors that measure: body temperature and glucose level.
The following are described: (a) the acquisition interval of the patient measurements; (b) the policy of using the measurement data charged to the fog node; (c) the policy of data forwarding to the cloud.
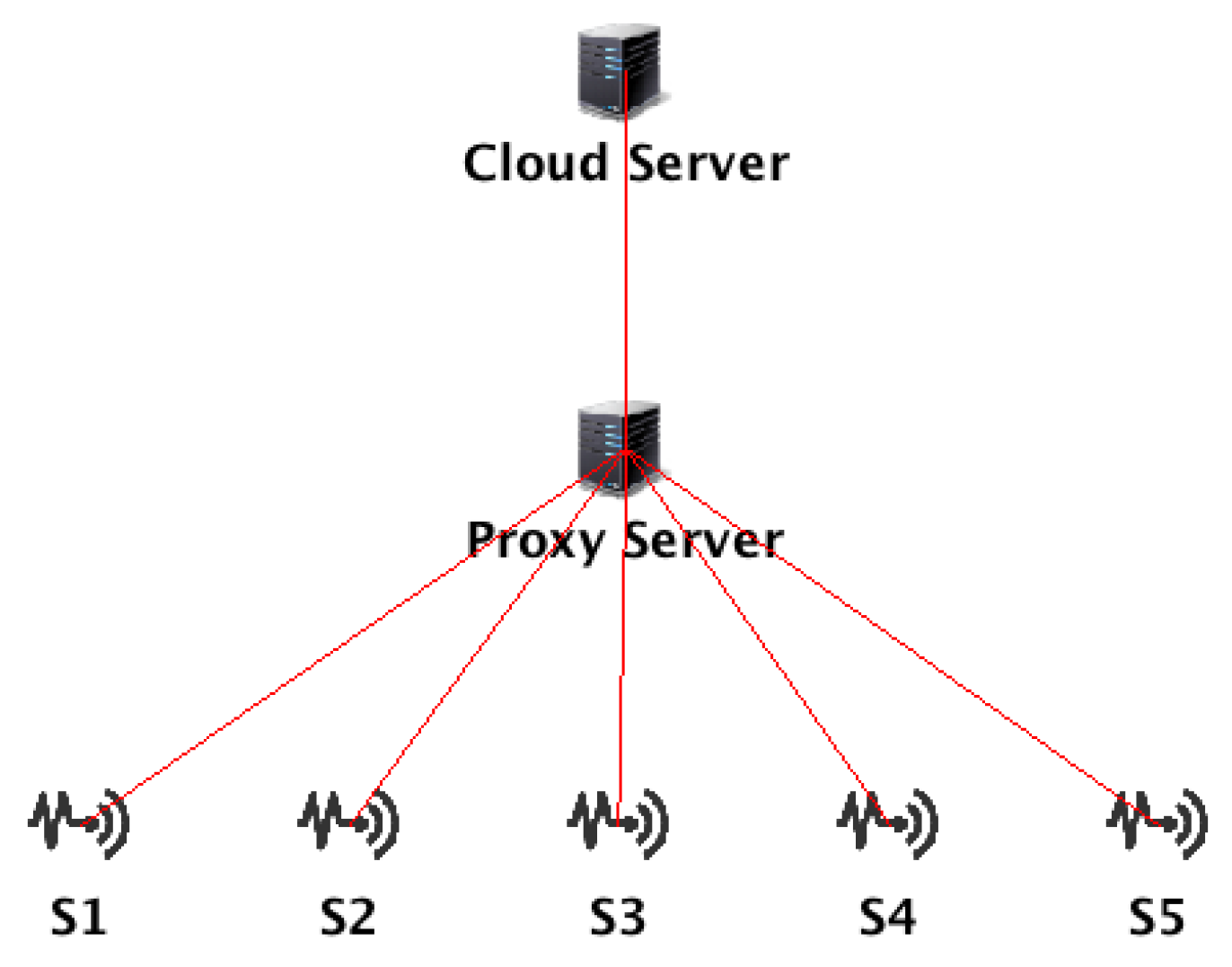
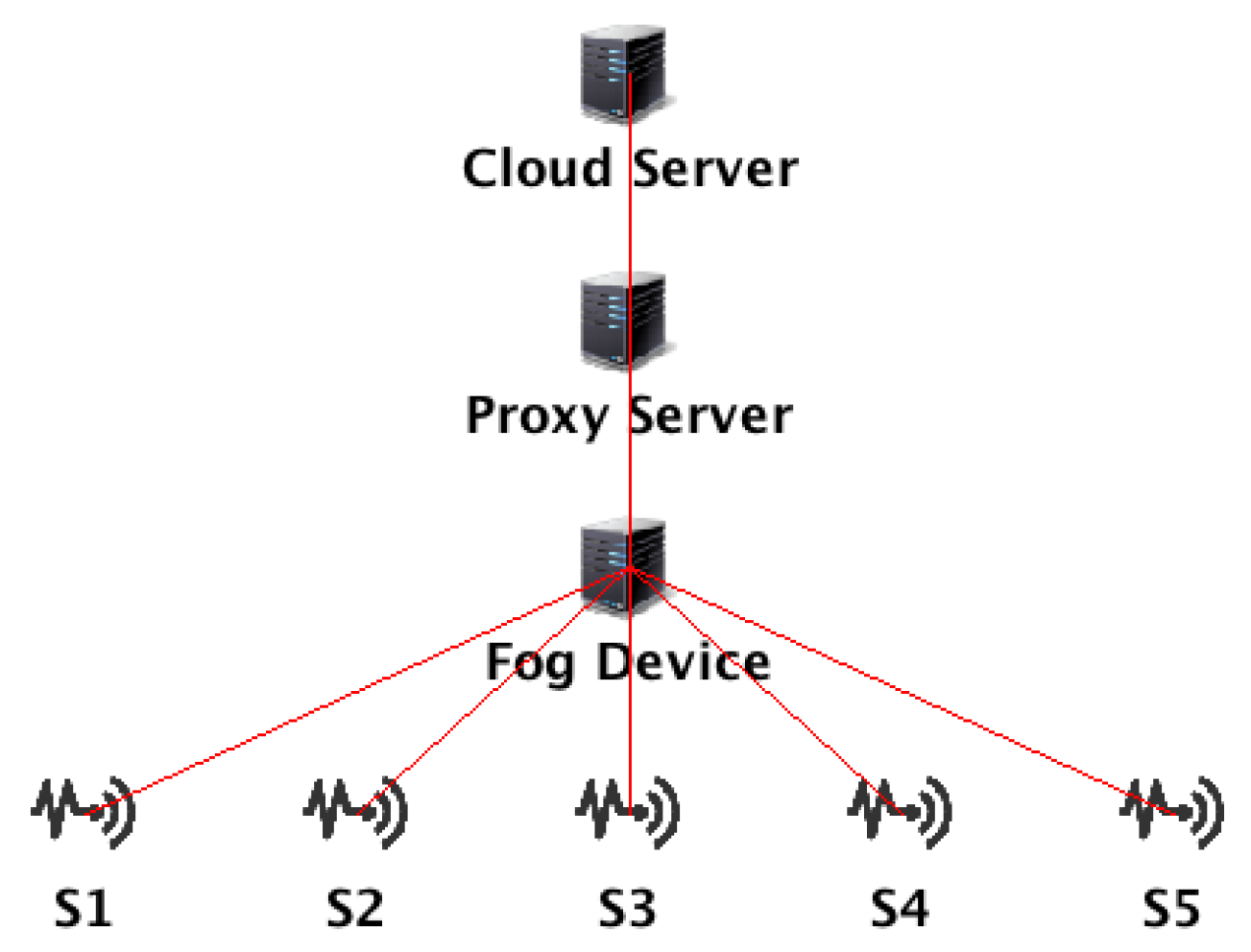
Figure 3 and Figure 4 show (for a single patient), respectively, the two IoT topologies we compared. Both scenarios adhere to the “stream-processing model”, as it is called in [10]. In fact, in both cases the five application modules (one for each sensor at the patient’s level) running on the fog node continuously process the data streams emitted from the five sensors. Hence, the information computed from the incoming streams is sent to the cloud where it is stored for large-scale and long-term analytics.
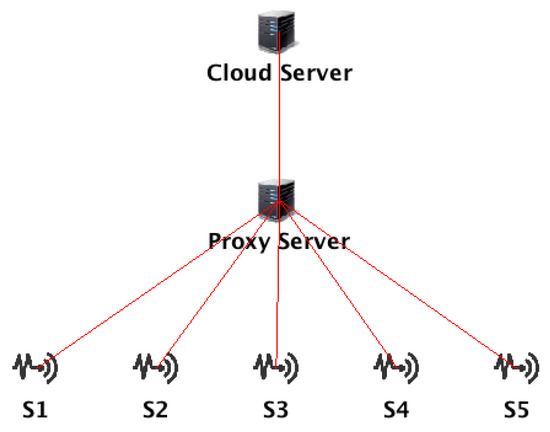
Figure 3.
The Cloud-only topology.
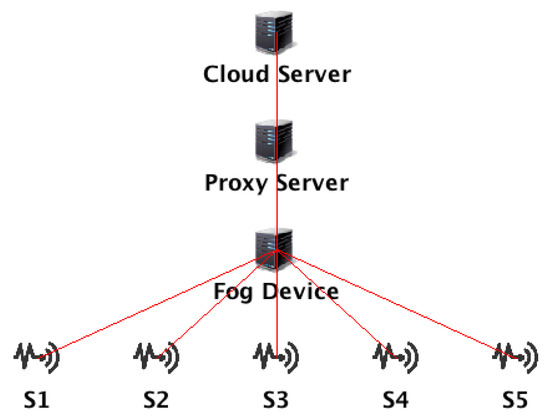
Figure 4.
The Cloud–Fog topology.
Table 1 collects the values of the parameters of the Cloud, Proxy, and Fog adopted in the experiments, for the simulations of the topologies of Figure 3 and Figure 4.

Table 1.
The values of the parameters of the Cloud, Proxy, and Fog adopted in the experiments.
The experimental settings are as follows:
- the measurements of the biometric parameters of the patient take place every 5 min;
- the values are stored in the storage of the corresponding fog node;
- if a sequence of N readings is recorded (initial hypothesis: N = 3) with values below a threshold that we will call critical, then the fog proceeds to send an alarm signal to the cloud. The cloud, in turn, will forward it to the doctor who is responsible for supervising the patient to make medical decisions appropriate to the circumstance (notice that such a part of the scenario is outside the scope of the present short paper due to the page limits);
- in the absence of such negative events, the fog proceeds to calculate the average values of the measurements every M readings (initial hypothesis: M = 12, that is, once every hour). These values are also stored in the patient’s fog node;
- if the biometric steady state of the patient persists, then the fog will send to the cloud every morning at a set time the average values of the parameters measured in the last 24 h. Those values are stored in the cloud permanently.
Ref. [11] offers a state-of-art of 27 available open-source fog simulators. According to such a study, iFogSim is the most frequently addressed fog simulator in terms of citation count. iFogSim was introduced by Gupta et al. in 2017 [10]. “iFogSim permits to evaluate different resources […] in fog environments according to their influence on energy consumption, latency, operational cost, and network congestion” [12]. Specifically, the latency is calculated using both processing latency of the fog nodes and network latency which consists of transmission and propagation delay of the data; while the network usage is computed based on the amount of data propagated across the network during the simulation time.
4. Results and Discussion
Table 2 and Table 3 collect the meaurements corresponding, in sequence, to the topology of Figure 3 and Figure 4. The measurements confirm what was expected, namely that in the case of adopting the first topology both latency and network traffic are superior to the other alternative. The reduction of the traffic sent to the network towards the cloud is a great benefit of the Cloud–Fog topology, as an uncontrolled increase in the network traffic may lead to congestion and, consequently, result in increased latency. The increase of the latency can be a serious problem in the case of patients in critical conditions, since it causes a delay in the reading of the measurements by the physician, a delay whose consequences depend directly on the health conditions of the patient.

Table 2.
The measurements for the Cloud-only topology (Figure 3).

Table 3.
The measurements for the Cloud–Fog topology (Figure 4).
5. Conclusions
Advanced societies aim at enhancing the quality of the services offered to the citizens. An efficient home monitoring service for frail people is a priority in those societies. Italy too pursues this goal. The present short paper has shown that the most efficient way to collect data about heartbeat, blood pressure, blood oxygen level, body temperature, and glucose level consists in adopting the IoT technology. Specifically, we proved, through experiments, that the Cloud–Fog architecture is the most efficient solution to be adopted.
Author Contributions
Conceptualization, P.D.F., G.P., R.P.; methodology, P.D.F., R.P.; data curation, R.P., D.I.; writing—original draft preparation, visualization, M.M.; supervision, G.P.; funding acquisition, G.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Gruppo Software Industriale, Italy.
Data Availability Statement
Data supporting reported results can be obtained by writing to R.P.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Stavropoulos, T.G.; Papastergiou, A.; Mpaltadoros, L.; Nikolopoulos, S.; Kompatsiaris, I. IoT Wearable Sensors and Devices in Elderly Care: A Literature Review. Sensors 2020, 20, 2826. [Google Scholar] [CrossRef] [PubMed]
- Directorate-General for Employment, Social Affairs and Inclusion (European Commission). Long-Term Care Report Trends, Challenges and Opportunities in an Ageing Society; European Union: Brussels, Belgium, 2021; Volume I. [Google Scholar] [CrossRef]
- Alli, A.A.; Alam, M.M. The fog cloud of things: A survey on concepts, architecture, standards, tools, and applications. Internet Things 2020, 9, 100177. [Google Scholar] [CrossRef]
- Ali, O.; Ishak, M.K.; Bhatti, M.K.L.; Khan, I.; Kim, K.-I. A Comprehensive Review of Internet of Things: Technology Stack, Middlewares, and Fog/Edge Computing Interface. Sensors 2022, 22, 995. [Google Scholar] [CrossRef] [PubMed]
- Firouzi, F.; Farahani, B.; Marinšek, A. The convergence and interplay of edge, fog, and cloud in the AI-driven Internet of Things (IoT). Inf. Syst. 2022, 107, 101840. [Google Scholar] [CrossRef]
- Pérez, L.J.; Salvachúa, J. An Approach to Build e-Health IoT Reactive Multi-Services Based on Technologies around Cloud Computing for Elderly Care in Smart City Homes. Appl. Sci. 2021, 11, 5172. [Google Scholar] [CrossRef]
- OpenFog: Reference Architecture for Fog Computing. 2017. Available online: https://www.iiconsortium.org/pdf/OpenFog_Reference_Architecture_2_09_17.pdf (accessed on 27 July 2022).
- Krishnamoorthy, S.; Dua, A.; Gupta, S. Role of emerging technologies in future IoT-driven Healthcare 4.0 technologies: A survey, current challenges and future directions. J. Ambient. Intell. Humaniz. Comput. 2021, 14, 361–407. [Google Scholar] [CrossRef]
- Shahid, J.; Ahmad, R.; Kiani, A.K.; Ahmad, T.; Saeed, S.; Almuhaideb, A.M. Data Protection and Privacy of the Internet of Healthcare Things (IoHTs). Appl. Sci. 2022, 12, 1927. [Google Scholar] [CrossRef]
- Gupta, H.; Vahid, D.A.; Ghosh, S.K.; Buyya, R. iFogSim: A toolkit for modeling and simulation of resource management techniques in the internet of things, edge and fog computing environments. Softw. Pract. Expir. 2017, 47, 1275–1296. [Google Scholar] [CrossRef]
- Gill, M.; Dinesh Singh, D. A comprehensive study of simulation frameworks and research directions in fog computing. Comput. Sci. Rev. 2021, 40, 100391. [Google Scholar] [CrossRef]
- Kassab, W.; Darabkh, K.A. A–Z survey of Internet of Things: Architectures, protocols, applications, recent advances, future directions and recommendations. J. Netw. Comput. Appl. 2020, 163, 102663. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).