1. Introduction
Smartphone-based biosensors combine mobile computing with biological sensing to deliver real-time, low-cost diagnostics, especially valuable in low-resource settings [
1,
2]. Advances in nanomaterials, microfluidics, sensor miniaturization, and AI-enhanced mHealth apps have expanded their clinical and environmental utility [
3,
4,
5,
6,
7]. Recent reviews highlight the growing diversity of biosensor platforms, including paper-based, electrochemical, and optical sensors, and their integration with mobile interfaces for point-of-care diagnostics [
8,
9]. Despite these gains, clinical adoption lags due to performance variability, manufacturing limits, and regulatory and user-trust issues [
10].
This review shifts focus from innovation to implementation, analyzing biosensor maturity, identifying key adoption barriers, and proposing strategies for scalable, user-focused deployment. While existing reviews emphasize technological development and sensor classification, this paper uniquely synthesizes these findings to provide a roadmap for the integration of artificial intelligence and low-cost manufacturing in smartphone biosensors, with a particular emphasis on end-user adoption and commercialization pathways.
2. Methodology
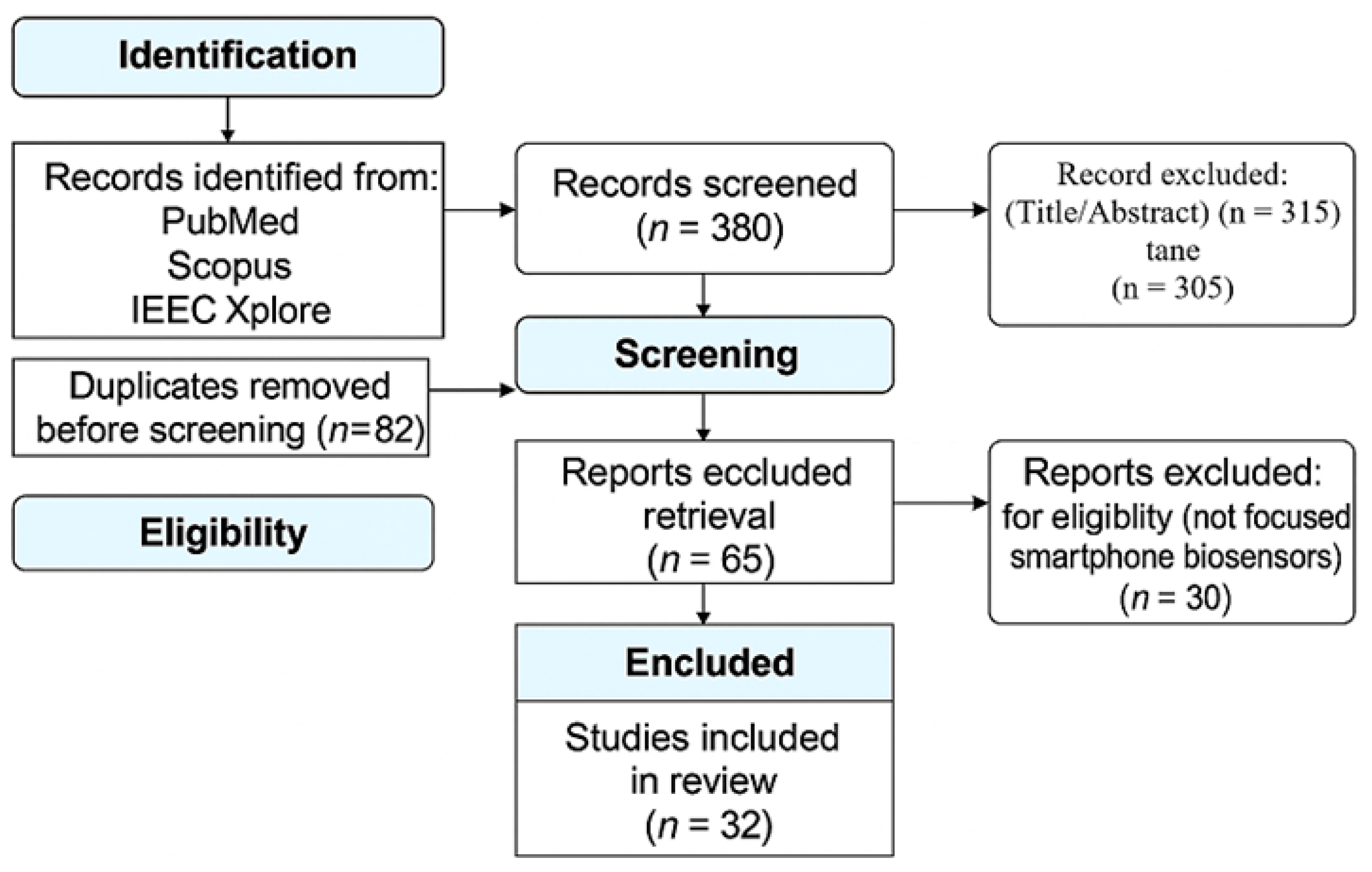
This study follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines to systematically map the landscape of smartphone-based biosensors. The objective is to identify technological trends, deployment challenges, and future opportunities in mobile diagnostics, with a focus on integration, miniaturization, and accessibility.
A structured search was conducted across five major databases: PubMed, Scopus, IEEE Xplore, ScienceDirect, and Google Scholar. Boolean operators were used to refine the search string: (“smartphone” OR “mobile”) AND (“biosensor” OR “wearable biosensor”) AND (“point-of-care” OR “diagnostics”) AND (“healthcare” OR “biosensor integration”). The search targeted peer-reviewed journal articles, conference papers, and patents published between January 2013 and August 2025.
After removing duplicates, titles and abstracts were screened for relevance to smartphone-enabled biosensing. Full-text articles were then assessed using predefined inclusion criteria: (1) direct relevance to biosensor integration with mobile platforms, (2) discussion of diagnostic functionality or deployment strategy, and (3) publication in English. Studies focused solely on non-mobile biosensing or lacking diagnostic context were excluded.
A total of 28 studies were included in the final synthesis. Thematic analysis was used to extract insights across five domains: sensor miniaturization, connectivity, data acquisition, diagnostic accuracy, and real-time health monitoring. Technical barriers such as calibration complexity, environmental variability, and interoperability with healthcare systems were evaluated. The findings were synthesized into a strategic roadmap emphasizing explainable AI integration and scalable, low-cost manufacturing.
A PRISMA-ScR flow diagram is included to visually represent the review process and ensure methodological transparency (
Figure 1).
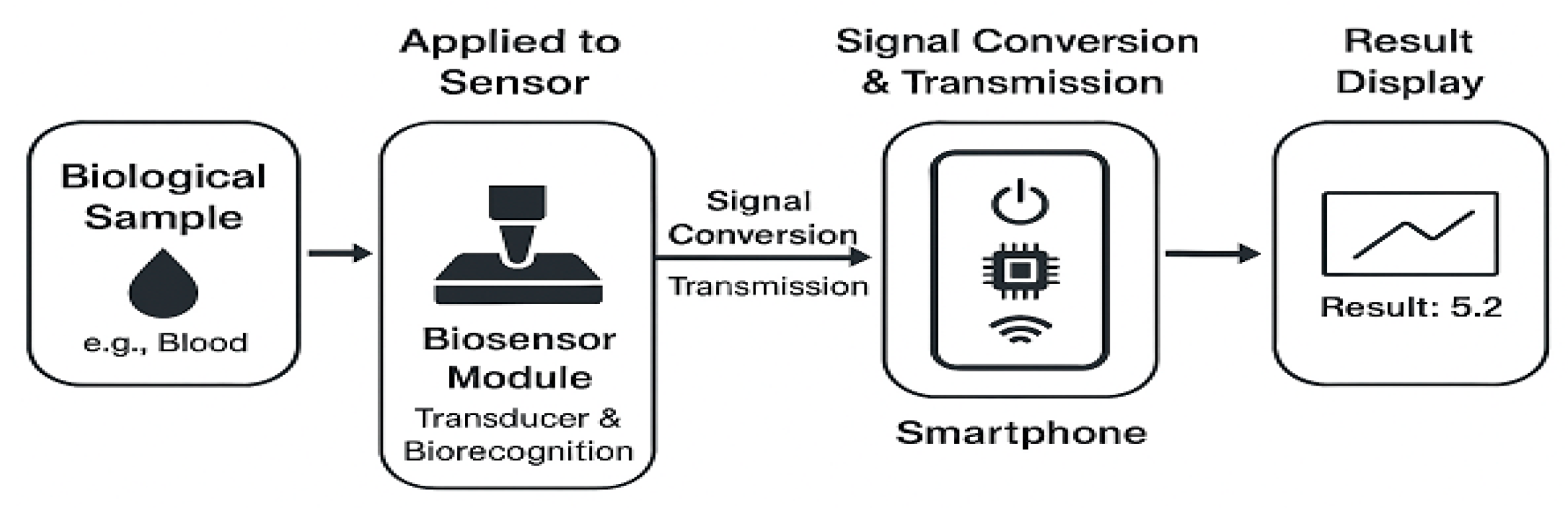
3. Fundamentals of Smartphone-Based Biosensors
Smartphone-based biosensors integrate biorecognition elements (e.g., antibodies, enzymes, and nucleic acids) with transducers to detect specific biomarkers, converting biological interactions into measurable signals (
Figure 2). Optical sensors capture colorimetric or fluorescent changes via the smartphone’s camera, while electrochemical types use external modules to measure current or voltage for high-sensitivity diagnostics [
11,
12]. The smartphone serves as the power source, processor, display, and communication hub. Signal amplification via nanomaterials and wearable designs enables real-time, remote health monitoring and supports scalable, decentralized diagnostics [
2,
10,
13].
4. Advancements and Technologies
Smartphone-based biosensors have progressed from conceptual tools to practical platforms for real-time diagnostics across healthcare, environmental, and industrial domains. Leveraging smartphone portability, processing power, and wireless connectivity, recent advancements span detection chemistry, miniaturized hardware, AI integration, and cost-effective formats.
4.1. Detection Techniques
Molecular diagnostics such as Clustered Regularly Interspaced Short Palindromic Repeats/CRISPR-associated protein 12a CRISPR/Cas12a systems now enable ultra-sensitive nucleic acid detection. Recent studies on CRISPR/Cas12a-based platforms have demonstrated a limit of detection (LOD) as low as 40 femtograms (fg) per reaction for specific DNA targets, with a total assay time under 60 min, making them competitive with traditional Polymerase Chain Reaction (PCR) -based methods in both speed and sensitivity [
14]. For example, some systems have shown no cross-reactivity with non-target strains, confirming their high diagnostic precision. Similarly, Metal-Organic Framework (MOF)-enhanced fluorescence biosensors have achieved LODs in the picomolar range, representing up to a 10-fold increase in sensitivity compared to conventional fluorescent assays [
15].
4.2. System Integration and Miniaturization
Microfluidic chips automate sample handling, reducing assay complexity and reagent volume. Nanomaterials like gold nanoparticles (AuNPs) and graphene improve signal transduction and enable wearable modules that wirelessly sync with smartphones. Gold nanoparticles, when integrated into electrochemical biosensors, can boost signal amplification efficiency by up to 50%, with an inter-batch coefficient of variation (CV) below 5%, which ensures manufacturing reproducibility [
16]. Graphene-based field-effect transistor (gFET) biosensors offer label-free detection with high electrical conductivity and chemical stability. Studies have reported CV values typically under 6%, confirming their suitability for scalable, real-time diagnostics [
17].
4.3. Comparison of Biosensing Detection Methods
The following table provides a concise comparison of the key detection methods discussed, highlighting their principles, advantages, and limitations for different applications (
Table 1). This summary addresses the need for a clear visual comparison and provides a quick reference for the reader.
4.4. Multi-Mode Sensing and Data Analytics
Combining optical, electrochemical, or thermal modalities improves diagnostic robustness. Smartphones process these multimodal data streams through embedded apps, enabling cross-validation and better accuracy [
18]. AI/ML-powered mobile platforms analyze complex biosensor outputs, personalize health insights, and automate alerts without requiring expert interpretation [
21].
4.5. Cost-Effective and Self-Powered Formats
Paper-based biosensors remain key for affordable diagnostics. Emerging self-powered systems using triboelectric generators or biochemical energy harvesters operate without batteries, ideal for low-resource or emergency contexts. Bluetooth and NFC enable wireless data transfer [
14].
4.6. Diverse Applications
Smartphone biosensors now support the following:
Healthcare: Monitoring glucose, oxygen saturation, and cardiac markers [
22].
Public health: Supporting remote care and outbreak tracking via mHealth platforms [
21].
Environmental safety: Assessing air/water quality with mobile-readout sensors [
23].
Food safety: Detecting spoilage or contamination in real time [
24].
Industrial biotech: Monitoring fermentation and drug production processes [
20].
Wearable biosensors, embedded in skin patches or textiles, enable continuous, non-invasive monitoring and integrate with smartphones for chronic disease management and large-scale health tracking [
23,
25].
5. Challenges in Smartphone-Based Biosensors
Smartphone-based biosensors, while offering transformative potential, face a series of interrelated technical and systemic challenges that limit their transition from laboratory prototypes to widespread clinical and consumer adoption. One of the most pressing technical barriers is the integration of biosensing, signal processing, and wireless communication within compact, energy-constrained mobile platforms [
26]. These constraints often compromise device performance, particularly in resource-limited environments where power efficiency and hardware compatibility are critical. Technical challenges such as complex calibration procedures and inconsistent signal processing across different smartphone models present a significant hurdle to clinical validation. Without standardized calibration protocols, it becomes difficult to ensure reproducible and reliable results, which is an essential requirement for regulatory approval and clinical trust [
4]. This lack of consistency undermines the credibility of biosensor outputs, especially in decentralized or at-home diagnostic settings. Sensor performance variability under real-world conditions further complicates deployment. Environmental factors such as temperature fluctuations, humidity, and biological sample variability can distort readings, leading to diagnostic inaccuracies. This inconsistency erodes user confidence and poses a substantial obstacle to clinical adoption, where diagnostic certainty is paramount for both healthcare providers and patients [
4]. Another critical technical barrier lies in the integration of smartphone biosensors with existing healthcare infrastructure. The absence of unified communication standards and limited interoperability with electronic health records (EHRs) disrupts clinical workflows and impedes seamless data exchange. This fragmentation not only delays diagnosis and treatment but also restricts the long-term utility of biosensors in patient monitoring and public health surveillance [
26]. At the production level, the high cost and limited scalability of advanced sensor components continue to restrict affordability and accessibility, particularly in low-resource settings. Without cost-effective manufacturing solutions, widespread deployment remains economically unfeasible. Overcoming these challenges demands coordinated innovation across engineering, regulatory policy, and user-centered design. Addressing technical inconsistencies, improving environmental robustness, and ensuring seamless integration with healthcare systems are essential steps toward realizing scalable, accessible, and clinically reliable smartphone-based biosensing solutions.
Microfluidic Integration Challenges
Despite their promise in automating sample processing and reducing reagent volumes, microfluidic chips face significant technical barriers when integrated with smartphone platforms. One major challenge is the physical alignment of microfluidic channels with smartphone sensors, such as cameras or photo-detectors, which often requires custom-designed attachments or external modules (“dongles”) to ensure accurate optical or electrochemical readouts [
27]. These add-ons can compromise portability and user convenience. Additionally, while microfluidics streamlines internal fluid handling, the initial sample introduction remains a critical point of user error, especially in at-home settings where inconsistent pipetting or contamination can distort results. Fluid flow control at the microscale typically relies on external pumps or pressure systems, which are difficult to miniaturize without sacrificing precision. This lack of integrated flow regulation can lead to variability in reaction kinetics and compromise diagnostic accuracy. Furthermore, although microfluidic chips are compact, their fabrication often involves complex techniques such as soft lithography or photopolymerization, which are not yet scalable for low-cost, disposable production. These limitations hinder widespread deployment and underscore the need for simplified, modular designs that balance performance with manufacturability.
6. Future Prospects and Strategic Directions
Smartphone-based biosensors are set to transform point-of-care diagnostics by enabling intelligent, personalized, and real-time health monitoring. Leveraging AI, IoT, and cloud computing, next-generation platforms will deliver remote diagnostic feedback and support population-level health surveillance [
28]. Advanced nanomaterials will further improve sensitivity, specificity, and miniaturization, allowing for seamless integration with smartphones and multiplexed detection [
2]. These advances can expand healthcare access in remote, resource-constrained areas. Integration into wearables and telemedicine platforms also promotes continuous, preventive care, shifting healthcare from reactive to proactive [
29]. However, key challenges remain. Sensor standardization, validation protocols, and clinical integration pathways are critical for regulatory approval and interoperability. Privacy concerns around AI-driven, cloud-connected systems require strong encryption and cybersecurity. Additionally, affordable manufacturing through printable electronics and low-cost, biocompatible materials is vital for scalable, equitable deployment [
20,
30]. Realizing this vision will require sustained collaboration among engineers, clinicians, data scientists, manufacturers, and policymakers to create secure, accessible, and impactful diagnostic tools that advance global health equity.
Analysis of Privacy and Cybersecurity Risks
While strong encryption is a necessary foundation, the privacy risks of AI-driven, cloud-connected biosensor systems are multifaceted and require a more granular analysis. One primary risk is data leakage during transmission. Data collected by a wearable biosensor could be intercepted via an insecure Wi-Fi network or a man-in-the-middle attack if the mHealth app uses a weak or misconfigured communication protocol. Recent studies emphasize that even encrypted channels can be vulnerable if session keys are poorly managed or if transport layer security is misconfigured [
31].
A second major risk is unauthorized access to data at rest. If a user’s smartphone is compromised or the data is not properly encrypted on the device or in the cloud, it becomes vulnerable to theft. This could expose highly sensitive personal health information (PHI) to malicious actors. The World Economic Forum highlights that AI adoption in healthcare must be accompanied by robust data governance frameworks to prevent such breaches, especially as mobile health platforms scale globally [
32].
Furthermore, the use of AI for data analysis introduces unique risks. Adversaries can employ techniques like prompt injection attacks to manipulate AI models into revealing confidential user data. Additionally, re-identification attacks pose a risk; even if data is initially de-identified for training AI models, a malicious actor could cross-reference it with publicly available information to link data back to a specific individual. These vulnerabilities are increasingly relevant in biosensor ecosystems, where continuous data streams and cloud-based analytics heighten exposure [
31]. A comprehensive cybersecurity strategy must therefore go beyond simple encryption to include adversarial robustness, federated learning, and privacy-preserving AI architectures.
7. Conclusions and Recommendations
Smartphone-based biosensors hold immense promise for transforming diagnostics and enabling decentralized healthcare. However, their delayed clinical adoption is not solely due to technical limitations; it also stems from a lack of robust clinical validation. While engineering advances have improved sensor sensitivity, miniaturization, and connectivity, these innovations must be supported by rigorous, high-quality clinical studies to gain widespread trust and regulatory approval.
Multicenter randomized controlled trials are essential to demonstrate the reliability, safety, and efficacy of smartphone-integrated biosensing platforms across diverse populations and healthcare settings. Without such evidence, biosensors risk remaining in the realm of promising prototypes rather than becoming standard tools in clinical practice.
This study proposes a strategic roadmap that integrates interpretable AI for diagnostic validation and outlines scalable manufacturing pathways using advanced nanomaterials. Yet, the success of this roadmap depends on interdisciplinary collaboration not only among engineers and designers, but also among clinicians, trial coordinators, and regulatory bodies. Only through coordinated efforts and rigorous clinical evaluation can smartphone biosensors evolve into trusted, equitable tools for global health delivery.
Author Contributions
Conceptualization, A.P.A.; methodology, A.P.A. and T.C.M.; validation, A.P.A., T.C.M., and I.O.; formal analysis, A.P.A.; resources, T.C.M. and I.O.; writing—original draft preparation, A.P.A. and T.C.M.; writing—review and editing, A.P.A., T.C.M., and I.O.; visualization, T.C.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Çelik, H.; Caf, B.B.; Çebi, G. Smartphone-assisted biosensors in point-of-care diagnostics: Integration, applications, and future challenges. Chem. Pap. 2025. [Google Scholar] [CrossRef]
- Xing, E.; Chen, H.; Xin, X.; Cui, H.; Dou, Y.; Song, S. Recent advances in smartphone-based biosensors for various applications. Chemosensors 2025, 13, 221. [Google Scholar] [CrossRef]
- Pirzada, M.; Altintas, Z. Nanomaterials for healthcare biosensing applications. Sensors 2019, 19, 5311. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Li, X.; Zhang, Y.; Xu, Y.; Liu, Y.; Chen, H. Artificial intelligence enhanced sensors—enabling technologies for next-gen healthcare. Bioelectron Med. 2023, 6, 18. [Google Scholar] [CrossRef]
- Loima, T.; Yoon, J.Y.; Kaarj, K. Microfluidic sensors integrated with smartphones for applications in forensics, agriculture, and environmental monitoring. Micromachines 2025, 16, 835. [Google Scholar] [CrossRef]
- Wasilewski, T.; Kamysz, W.; Gębicki, J. AI-assisted detection of biomarkers by sensors and biosensors for early diagnosis and monitoring. Biosensors 2024, 14, 356. [Google Scholar] [CrossRef]
- Hyun, A.; Lee, S.; Park, J.; Kim, H. Wearable biosensors for pediatric hospitals: A scoping review. Pediatr Res. 2025, 98, 90–99. [Google Scholar] [CrossRef]
- Madrid, R.E.; Ashur Ramallo, F.; Barraza, D.E.; Chaile, R.E. Smartphone-based biosensor devices for healthcare: Technologies, trends, and adoption by end-users. Bioengineering 2022, 9, 101. [Google Scholar] [CrossRef]
- QYResearch. Global Smartphone Biosensor Market Report 2025. QYResearch Reports. 2025. Available online: https://www.qyresearch.com/reports/3851948/smartphone-based-biosensor (accessed on 16 March 2025).
- Seshadri, D.R.; Davies, E.V.; Harlow, E.R.; Hsu, J.J.; Knighton, S.C.; Walker, T.A.; Voos, J.E.; Drummond, C.K. Wearable sensors for COVID-19: A call to action to harness our digital infrastructure for remote patient monitoring and virtual assessments. Front. Digit. Health 2020, 2, 8. [Google Scholar] [CrossRef]
- Abena, T. Biosensors technological advancement and their biomedical, agricultural, environmental, and food industrial applications: A review. Int. J. Food Agric. Nat. Resour. 2023, 4, 46–57. [Google Scholar] [CrossRef]
- Lin, T.-Z.; Chen, C.-H.; Lei, Y.-P.; Huang, C.-S. Gradient Guided-Mode Resonance Biosensor with Smartphone Readout. Biosensors 2023, 13, 1006. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Yang, S.; Zheng, J.; Chai, F.; Tian, M. Smartphone-assisted portable paper-based biosensors for rapid and sensitive detection of biomarkers in urine. Microchem. J. 2024, 204, 110982. [Google Scholar] [CrossRef]
- Jia, N.; Wang, C.; Liu, X.; Huang, X.; Xiao, F.; Fu, J.; Sun, C.; Xu, Z.; Wang, G.; Zhou, J.; et al. A CRISPR-Cas12a-based platform for ultrasensitive rapid highly specific detection of Mycobacterium tuberculosis in clinical application. Front. Cell. Infect. Microbiol. 2023, 13, 1192134. [Google Scholar] [CrossRef]
- Kumar, R.; Shafique, M.S.; Martínez Chapa, S.O.; Madou, M.J. Recent advances in MOF-based materials for biosensing applications. Sensors 2025, 25, 2473. [Google Scholar] [CrossRef]
- Chiang, H.-C.; Wang, Y.; Zhang, Q.; Levon, K. Optimization of the electrodeposition of gold nanoparticles for the application of highly sensitive, label-free biosensor. Biosensors 2019, 9, 50. [Google Scholar] [CrossRef]
- Aran, K.; Goldsmith, B.; Moarefian, M. Applications of graphene field effect biosensors for biological sensing. In Trends in Biosensing Research; Springer: Berlin/Heidelberg, Germany, 2024; pp. 37–70. Available online: https://link.springer.com/chapter/10.1007/10_2024_252 (accessed on 16 March 2025).
- Han, Q.; Wang, H.; Wang, J. Multi-mode/signal biosensors: Electrochemical integrated sensing techniques. Adv. Funct. Mater. 2024, 34, 2403122. [Google Scholar] [CrossRef]
- Shi, J.; Li, P.; Huang, Y.; Wu, Y.; Wu, J.; Huang, K.-J.; Tan, X.; Ya, Y. Smartphone-assisted self-powered dual-mode biosensor designed on binary 3D DNA walkers mediated CRISPR/Cas12a system. Chem. Eng. J. 2024, 483, 149231. [Google Scholar] [CrossRef]
- Vo, D.K.; Trinh, K.T.L. Advances in wearable biosensors for healthcare: Current trends, applications, and future perspectives. Biosensors 2024, 14, 560. [Google Scholar] [CrossRef]
- Hettiarachchi, C.; Vlieger, R.; Ge, W.; Apthorp, D.; Daskalaki, E.; Brüstle, A.; Suominen, H. Optimising personalised medical insights by introducing a scalable health informatics application for sensor data extraction, preprocessing, and analysis. Stud. Health Technol. Inform. 2024, 318, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Alhamwi, T.; Oruklu, E. Personal health monitoring with Bluetooth sensors and Android smartphones. Ill. Tech. Undergrad. Res. J. 2015, 1, 37–40. [Google Scholar] [CrossRef]
- Hofman, J.; Lazarov, B.; Stroobants, C.; Elst, E.; Smets, I.; Van Poppel, M. Portable Sensors for Dynamic Exposure Assessments in Urban Environments: State of the Science. Sensors 2024, 24, 5653. [Google Scholar] [CrossRef]
- Chakraborty, A.; Bardhan, S.; Das, S.; Ray Chowdhury, B. Development of biosensors for application in industrial biotechnology. In Metagenomics to Bioremediation: Applications, Cutting-Edge Tools, and Future Outlook; Developments in Applied Microbiology and Biotechnology; Academic Press: Oxford, UK, 2023; pp. 737–753. [Google Scholar] [CrossRef]
- Pillai, A.G.; Kewte, S. Application of Wearable Electronics Sensors for Public Health Monitoring and Disease Prevention. S. East. Eur. J. Public Health 2024, 23, 262–267. [Google Scholar] [CrossRef]
- Bui, T.H.; Thangavel, B.; Sharipov, M.; Chen, K.; Shin, J.H. Smartphone-Based Portable Bio-Chemical Sensors: Exploring Recent Advancements. Chemosensors 2023, 11, 468. [Google Scholar] [CrossRef]
- Lapins, N.; Akhtar, A.S.; Banerjee, I.; Kazemzadeh, A.; Pinto, I.F.; Russom, A. Smartphone-driven centrifugal microfluidics for diagnostics in resource-limited settings. Biomed. Microdevices 2024, 26, 43. [Google Scholar] [CrossRef]
- Manickam, P.; Mariappan, S.A.; Murugesan, S.M.; Hansda, S.; Kaushik, A.; Shinde, R.; Thipperudraswamy, S.P. Artificial Intelligence (AI) and Internet of Medical Things (IoMT) Assisted Biomedical Systems for Intelligent Healthcare. Biosensors 2022, 12, 562. [Google Scholar] [CrossRef]
- Lu, L.; Zhang, J.; Xie, Y.; Gao, F.; Xu, S.; Wu, X.; Ye, Z. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR Mhealth Uhealth 2020, 8, e18907. [Google Scholar] [CrossRef]
- Hassan, R.Y.A. Advances in Electrochemical Nano-Biosensors for Biomedical and Environmental Applications: From Current Work to Future Perspectives. Sensors 2022, 22, 7539. [Google Scholar] [CrossRef]
- Achuthan, K.; Ramanathan, S.; Srinivas, S.; Raman, R. Advancing cybersecurity and privacy with artificial intelligence: Current trends and future research directions. Front. Big Data 2024, 7, 1497535. [Google Scholar] [CrossRef]
- World Economic Forum. Artificial Intelligence and Cybersecurity: Balancing Risks and Rewards [Internet]. 2025. Available online: https://reports.weforum.org/docs/WEF_Artificial_Intelligence_and_Cybersecurity_Balancing_Risks_and_Rewards_2025.pdf (accessed on 10 March 2025).
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).