Abstract
Metabolic syndrome comprises a constellation of comorbidities, including obesity, hypertension, and disorders in carbohydrate and lipid metabolism, associated with an elevated risk of cardiovascular mortality. Obesity is regarded as the principal cause of metabolic syndrome (both collectively and in relation to its components), frequently linked in previous scientific studies with a deficiency of magnesium, one of the most important cations found in the human body. Objectives: The objective of this study was to assess the prevalence of hypomagnesemia in patients with metabolic syndrome and to determine the most significant risk factor among its components for this nutritional deficiency. Methods: Retrospective medical data from 403 patients admitted to the hospital for conditions unrelated to magnesium levels from 2015 to 2019 were evaluated, encompassing serum magnesemia and specific data about components of metabolic syndrome. Data underwent statistical analysis, including linear and logistic regression, to assess the principal risk variables of hypomagnesemia. Results: Hypomagnesemia was observed in 14.89% of the patients with metabolic syndrome, exhibiting a 2.42-fold greater risk of this deficiency (95%CI: 1.40–3.40). Among the components of metabolic syndrome, hyperglycemia emerged as the most significant determinant affecting both the incidence and severity of hypomagnesemia, elevating the risk by a ratio of 2.72 (95%CI: 1.52–4.87). In the multivariate regression model, hyperglycemia was the sole factor independently influencing magnesium concentration (β = −0.145; p < 0.001). Conclusions: Patients presenting signs of metabolic syndrome are at heightened risk for hypomagnesemia. Hyperglycemia appears to be the most important variable affecting the risk of magnesium insufficiency; however, additional research is needed in this area.
Keywords:
metabolic syndrome; magnesium; hypomagnesemia; obesity; diabetes; hypertension; dyslipidemia 1. Introduction
Metabolic syndrome is a prevalent global health and societal issue characterized by an elevated risk of cardiovascular events due to the concurrent presence of obesity and other factors: hypertension, hyperglycemia, and/or dyslipidemia. Abdominal obesity is regarded as the principal cause of metabolic syndrome and its most significant component, which contributes to the development of other components as well as various health consequences like renal dysfunction, fatty liver disease and fibrosis, obstructive sleep apnea, hyperuricemia, chronic inflammation, polycystic ovary syndrome, and others [1,2,3]. A fundamental guideline for treating metabolic syndrome is lifestyle modification, encompassing increased physical activity and a balanced diet. It is well known that poor dietary habits contribute to both obesity and nutritional deficiencies [1]. This article will focus on a specific element: magnesium.
Magnesium is an essential macroelement that is important to various metabolic processes within the human body. It is involved in over 300 enzymatic reactions, including mainly those associated with protein synthesis, the regulation of muscle and nerve function, or energy production [4]. To ensure the correct functioning of the aforementioned processes, dietary intake of magnesium from food and drinks is essential—the European Food Safety Authority has established the appropriate intake of magnesium at 350 mg/day for men and 300 mg/day for women [5,6]. Magnesium deficiency has been linked to numerous health problems, including cardiovascular diseases (this association may be attributed to the effects of this cation on endothelial function, inflammation, oxidative stress, and insulin resistance, which also align with the complications of metabolic syndrome and its components) [7,8]. The relationship between hypomagnesemia and metabolic syndrome is complex, as magnesium deficiency can worsen any component of metabolic syndrome, while these conditions can also result in increased magnesium loss. However, the chronicity of metabolic syndrome components seems to be the prevailing factor in this dynamic.
Although we are aware of the importance of proper magnesium intake, the problem of hypomagnesemia sometimes seems to be underestimated or neglected in clinical practice. The aim of this study was to evaluate the prevalence of hypomagnesemia among the population of patients with metabolic syndrome and to identify the most significant risk factor among its components for this nutritional deficiency.
2. Materials and Methods
The authors analyzed retrospective medical data from patients from their endocrinology and diabetology department who were hospitalized between 2015 and 2019. This study encompassed anonymous data from patients aged 18 to 80 years, who underwent planned hospital admissions, and evaluated all significant parameters such as waist circumference (WC), systolic and diastolic blood pressure (sBP and dBP), fasting plasma glucose (FPG), high-density lipoprotein cholesterol (HDL-C), serum triglycerides (TG), and serum magnesium (sMg). The authors excluded medical records from patients admitted to the hospital due to any acute internal medicine diseases or life-threatening conditions and from patients with diseases or conditions that could potentially alter serum magnesium levels (mainly absorption disorders, gastric or duodenal ulcers, inflammatory diseases of the stomach and intestines, chronic pancreatitis, hyperparathyroidism and state after its surgical treatment, hyperaldosteronism, adrenal insufficiency, hypothyroidism, chronic renal failure, congenital tubulopathies, neoplastic diseases, chronic alcohol abuse, and the use of substances such as proton pump inhibitors, diuretics, calcium, and magnesium). Finally, data from a total of 403 unique patients were included: 230 females (57.07%) and 173 men (42.93%).
As per the 2009 Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention, the National Heart, Lung, and Blood Institute, the American Heart Association, the World Heart Federation, the International Atherosclerosis Society, and the International Association for the Study of Obesity, the presence of each individual component of the metabolic syndrome was assessed in all patients included in the final analysis: WC ≥ 80 cm for women and ≥94 for men, FPG ≥ 100 mg/dl (or pharmacological treatment of type 2 diabetes), sBP ≥ 130 mmHg or dBP ≥ 85 mmHg (or earlier started treatment of hypertension), TG > 150 mg/dl (or earlier started treatment of hypertriglyceridemia), and HDL-C < 50 mg/dl in women and <40 mg/dl in men (or treatment of this kind for dyslipidemia) [9]. The level of sMg was verified in every analyzed patient—in accordance with the currently used analytical technique for sMg determination at the authors’ department, the normative values were established as within the range of 0.67–1.07 mmol/L.
Statistical analysis of the obtained data was conducted using STATISTICA 13.0 PL statistical software (TIBCO Software Inc., Palo Alto, CA, USA) and Microsoft Excel 2019 (Microsoft Corp, Redmond, WA, USA). The Shapiro–Wilk test was used to assess the normality of the results. Continuous variables are presented using the median and IQR (interquartile range: 25th–75th percentiles), whereas categorical variables are reported using numbers and percentages. The results were compared using the Fisher exact test or Chi-squared test (categorical variables) and the Mann–Whitney U-test or Kruskal–Wallis ANOVA test (continuous variables). The Spearman correlation coefficient was used to assess the correlation between numerical values. Linear and logistic regression analyses were employed. Evaluation of odds ratios (ORs) and relative risks (RRs) was conducted, each time also providing the 95% confidence interval (95%CI). The statistical significance level was established at 0.05.
3. Results
3.1. General Information
The study group comprised 403 patients with a median age of 64.30 years (IQR 47.99–73.73), predominantly female (n = 230; 57.07%). The median WC for females was 91 cm (IQR 84–96), while for men, it was 98 cm (IQR 91–104). The median sBP for all participants was 130 mmHg (IQR 124–136), with no significant gender differences (p = 0.639); conversely, the median dBP was 79 mmHg (IQR 74–83), revealing a significant difference between genders: females had a median of 78 mmHg (IQR 74–83), while men had a median of 80 mmHg (IQR 75–85), p = 0.015. The median FPG among all patients was 108 mg/dl (IQR 89–194), with a significant difference observed between females (101.5 mg/dl; IQR 87–168) and men (121 mg/dl; IQR 92–203), p = 0.008. The median HDL-C was 49 mg/dl (IQR 38–61) in women and 39 mg/dl (IQR 29–50) in men. The average TG levels were 114 mg/dl (IQR 84–149) and did not differ significantly by gender (p = 0.547).
The median magnesium levels in the study cohort were 0.77 mmol/L (IQR 0.69–0.85) and exhibited no statistically significant differences by gender (p = 0.433). Magnesemia did not exhibit a significant correlation with age (p = 0.086) or any other laboratory or physical examination characteristics assessed by us, with the exception of FPG (R = −0.194; p < 0.001)—full correlation data are presented in Table 1. Patients presenting hypomagnesemia constituted 14.89% of the studied cohort (n = 60), with no significant gender difference (p = 0.831), but patients with this electrolyte disorder were older (69.05 years with IQR 58.59–74.98 versus 63.90 years with IQR 45.33–73.45; p = 0.021).

Table 1.
The Spearman correlation coefficients between serum magnesemia and other analyzed parameters related to metabolic syndrome.
In our cohort, the predominant element of metabolic syndrome was abdominal obesity (n = 318; 78.91%), followed by hyperglycemia (n = 230; 57.07%), elevated blood pressure (n = 216; 53.60%), and reduced HDL-C concentration (n = 209; 51.86%), with hypertriglyceridemia being the least prevalent component (n = 99; 24.57%). A statistically significant difference in the prevalence of specific components of metabolic syndrome based on gender was observed only in abdominal obesity (which was more prevalent in females—87.39% vs. 67.63%; p < 0.001) and hyperglycemia (more prevalent in men—63.58% vs. 52.17%; p = 0.022)—Figure 1 illustrates the full gender differentiation of metabolic syndrome components in our group.
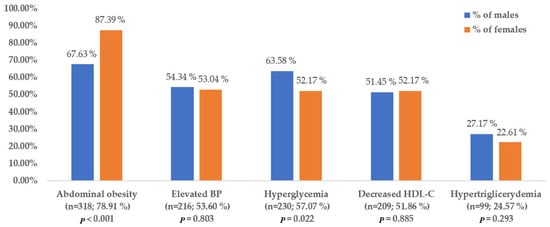
Figure 1.
Gender differentiation of metabolic syndrome components in our cohort.
The age difference was not statistically significant between groups with and without elevated blood pressure (p = 0.803) and hypertriglyceridemia (p = 0.156), but differences were observed in cases of other components: patients with abdominal obesity were older than those with normal weight (65.77 years with IQR 52.87–74.78 vs. 59.58 years with IQR 31.41–68.84; p < 0.001), as were those with hyperglycemia (65.78 years with IQR 53.92–74.83 vs. 59.98 years with IQR 42.01–71.87 in normoglycemic patients; p = 0.002) and reduced HDL-C concentration (68.64 years with IQR 57.78–76.52 vs. 59.59 years with IQR 39.32–70.68 in group with normal values of HDL-C; p < 0.001).
Patients diagnosed with metabolic syndrome, as per established guidelines, constituted 55.33% of the cohort (n = 223) and displayed no significant gender disparities when compared to patients without metabolic syndrome population (p = 0.450). Patients with metabolic syndrome were older, with a median age of 65.80 years (IQR 54.56–74.18) vs. 61.15 years (IQR 40.27–73.36); p = 0.003.
3.2. (Hypo)magnesemia and Metabolic Syndrome
As mentioned above, in our study group, hypomagnesemia was characteristic of 14.89% of patients (n = 60), and the median magnesium concentration was 0.77 mmol/L (IQR 0.69–0.85).
Hypomagnesemia was markedly more prevalent in individuals with confirmed metabolic syndrome compared to those who did not fulfill the diagnostic criteria (20.18% vs. 8.33%; p = 0.002), with the relative risk for this cohort being 2.42 (95%CI: 1.40–3.40). Data on patients who met and did not meet the individual criteria for the diagnosis of metabolic syndrome were analyzed: the components most frequently associated with hypomagnesemia, in order, were hyperglycemia (20.43%), decreased HDL-C (19.62%), elevated blood pressure (18.06%), abdominal obesity (16.67%), and hypertriglyceridemia (16.16%). Statistically significant differences were identified only for hyperglycemia and decreased HDL-C, in contrast to raised blood pressure and abdominal obesity (p-values ranging from 0.059 to 0.066). Detailed data about differences are presented in Figure 2.
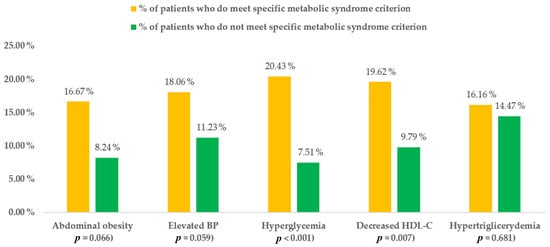
Figure 2.
Differences in the frequency of hypomagnesemia between patients who met and did not meet specific criteria for metabolic syndrome.
Based on the above data, the relative risk of hypomagnesemia was evaluated in relation to a specific component of metabolic syndrome: patients with hyperglycemia exhibited a 2.72-fold increased risk of hypomagnesemia, while those with reduced HDL-C demonstrated a 2-fold increased risk compared to patients without these conditions. Detailed information is presented in Figure 3.
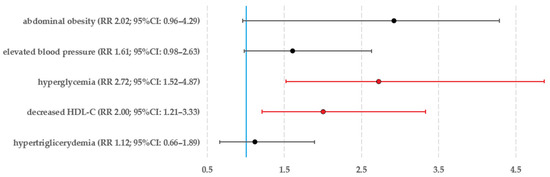
Figure 3.
The relative risk of hypomagnesemia assessed for each individual component of the metabolic syndrome (data that fulfill the criterion of statistical significance are highlighted in red).
In the univariate logistic regression model, age (OR 1.02 with 95%CI: 1.00–1.04; p = 0.016) also had a statistically significant effect on hypomagnesemia, in addition to hyperglycemia and low HDL-C concentration. Considering this, multivariate analysis was performed with age and gender taken into account, revealing hyperglycemia as the sole independent variable having a statistically significant impact on hypomagnesemia prevalence (OR 2.69, IQR 1.38–5.25; p = 0.004).
When analyzing magnesium concentrations in patients, a noticeable difference was observed between the group of patients with and without a comprehensive diagnosis of metabolic syndrome (0.77 mmol/L with IQR 0.69–0.84 in metabolic syndrome vs. 0.80 mmol/L with IQR 0.73–0.86 in the group of patients without metabolic syndrome). p = 0.015). By analyzing more precisely the specific components of metabolic syndrome, a statistically significant difference in magnesium was visible only in the comparison of normo- and hyperglycemic groups, where lower magnesium concentrations were in patients with hyperglycemia (0.76 mmol/L with IQR 0.68–0.83 vs. 0.81 mmol/L with IQR 0.75–0.87; p < 0.001). Table 2 provides a comprehensive summary of the differences in magnesium concentrations throughout every component of metabolic syndrome.

Table 2.
Differences in magnesium levels between patients with and without specific components of metabolic syndrome.
Interestingly, in the analysis of magnesium concentration relative only to the number of metabolic syndrome components (irrespective of their internal structure), the Kruskal–Wallis H test indicated a not significant difference (p = 0.058)—patients without any metabolic syndrome components (n = 33) exhibited a magnesium level of 0.81 mmol/L (IQR 0.76–0.90), those with one isolated criterion (n = 55) had a level of 0.80 mmol/L (IQR 0.74–0.85), patients with two criteria (n = 92) showed 0.79 mmol/L (IQR 0.71–0.85), with three criteria (n = 97) 0.78 mmol/L (IQR 0.73–0.86), with four criteria (n = 88) 0.76 mmol/L (IQR 0.71–0.89), and lastly, patients meeting all five criteria (n = 38) also had a level of 0.76 mmol/L (but with IQR of 0.67–0.83).
The final step of our investigation involved assessing the linear regression model on the impact of particular parameters on magnesium concentration, with comprehensive data on the univariate linear regression model provided in Table 3.

Table 3.
Results of the univariate linear regression model for the influence of various assessed factors on the magnesium concentration.
In the multivariate model, considering the patients’ gender and age, as in the univariate model, the only factor independently affecting magnesium concentration was glycemia (β = −0.145; 95%CI: (−0.242)–(−0.048); p < 0.001).
4. Discussion
Hypomagnesemia is widely recognized as a significant problem in the context of metabolic syndrome and its components—the interplay between these conditions and magnesium is complex and multifaceted, involving various physiological mechanisms and pathways.
Our study revealed that patients with metabolic syndrome exhibited a 2.42-fold increased risk of magnesium insufficiency. This corresponds to previous findings on this subject. Guerrero-Romero et al., examining the relationship between metabolic syndrome, oxidative stress, and inflammation, showed that the risk of hypomagnesemia increases 1.9× in the presence of features of metabolic syndrome (however, diagnosed according to the Adult Treatment Panel III criteria). Interestingly, this link was notably robust in West Asia and Latin America, indicating possible regional disparities in the correlation between metabolic syndrome and hypomagnesemia [10]. The meta-analysis by Dibaba et al. showed an association between an increased incidence of metabolic syndrome and a reduced magnesium intake and an increased risk of hypomagnesemia—for every 100 mg/day increment in magnesium intake, the overall risk of metabolic syndrome was lowered by 17% [11]. In a randomized double-blind placebo-controlled clinical trial conducted by Rodriguez-Moran et al., it was demonstrated that, in cases of hypomagnesemia, appropriate magnesium supplementation (30 mL of 5% magnesium chloride solution, equivalent to 382 mg of elemental magnesium) effectively improves metabolic syndrome by decreasing blood pressure, hyperglycemia, and hypertriglyceridemia [12].
We demonstrated that, in our cohort, the sole factor independently influencing magnesium concentration was that glycemia patients with hyperglycemia had a 2.72-fold greater risk of hypomagnesemia. Ghasemi et al. demonstrated, similarly to us, that patients with metabolic syndrome are characterized by generally lower serum magnesium concentrations, but among all the components of metabolic syndrome, hyperglycemia plays the most important role [13]. In the preceding decade, Simmons et al. demonstrated that magnesium deficiency, among the disorders characteristic of metabolic syndrome, is exclusively linked to diabetes (OR 5.71–11.1), which is the primary pathological condition associated with carbohydrate metabolism [14]; however, it is important to note that different criteria for diagnosing metabolic syndrome were applicable at that time. A more recent study by Addin et al. in 2024 found that serum magnesium was inversely correlated only with higher fasting glucose among all components of metabolic syndrome (OR 0.78, 95%CI 0.71–0.88) [15]. These data correspond with the well-documented effect of persistent hyperglycemia in enhancing urine magnesium excretion [16,17]. Chronic hyperglycemia results in glucosuria when blood glucose surpasses the renal reabsorption threshold (approximately 180 mg/dl)—the presence of glucose in the renal tubule lumen functions as an osmotic agent, attracting water and elevating urine output, thereby reducing the contact duration of electrolytes, including magnesium, with the reabsorption surface and consequently increasing urinary magnesium excretion. The process of osmotic diuresis likely alters the luminal environment of the renal tubules and the electrochemical gradients essential for both paracellular and transcellular magnesium transport, hence adversely affecting optimum magnesium reabsorption in the nephron [18,19,20]—the TRPM6 channel in the apical membrane of the distal tubule is essential for the accurate regulation of transcellular magnesium reabsorption; its dysregulation, caused by reactive oxygen species in the glucotoxic pathway, results in compromised magnesium reabsorption [21,22]. Previous epidemiological studies have proven the relationship between serum magnesium level and the risk of developing heart failure, atrial fibrillation, and microvascular disease in a cohort of patients with type 2 diabetes—it is estimated that the potential protective effect of magnesium may result from such effects of its action as the reduction in oxidative stress and myocardial fibrosis and remodeling [22]. The association between hyperglycemia and hypomagnesemia may be bidirectional; that is, hyperglycemia can result in elevated urine magnesium excretion, while hypomagnesemia may adversely affect insulin sensitivity and glucose metabolism, which affirms that hyperglycemia may be a significant risk factor for serum hypomagnesemia in metabolic syndrome [10,23].
While hyperglycemia seems to significantly influence the onset of hypomagnesemia, other components of the metabolic syndrome may also contribute to or intensify it, although their status as primary and independent variables remains ambiguous according to the existing evidence. Obesity is often linked with reduced serum magnesium levels, mostly due to a diet lacking in magnesium-rich foods; however, Lecube et al. assert that hyperglycemia, particularly diabetes, rather than obesity itself, is the primary cause of hypomagnesemia in individuals with obesity [24]. It is reasonable to claim that hormonal dysfunction and chronic inflammation of adipose tissue may adversely affect magnesium levels; however, current research indicates that obesity primarily acts as a risk factor for hyperglycemia and insulin resistance, which are more direct causes of hypomagnesemia [25]. In the context of hypertension, excessive activity of the renin–angiotensin–aldosterone system, particularly with raised aldosterone levels, may adversely alter serum magnesium concentration by contributing to increased renal magnesium loss (hypermagnesuria) [26]. Aldosterone may directly influence magnesium transporters—in an animal model, it has been demonstrated that aldosterone can diminish the expression of TRPM7 protein, resulting in hypermagnesuria and subsequent hypomagnesemia [27]. Dyslipidemia is frequently linked to hypomagnesemia; nevertheless, magnesium insufficiency appears to exert a more significant influence on lipid metabolism than problems of lipid metabolism do on renal magnesium loss, because magnesium serves as a cofactor for lipoprotein lipase and lecithin-cholesterol acetyltransferase [28].
An issue worthy of discussion is the norms for serum magnesium, which have become a subject of controversy recently among researchers and practicing physicians. In our study, we used the norm of 0.67–1.07 mmol/L, which was the standard for Poland (and, therefore, the authors’ home institution) in the period we studied, 2015–2019. In later years, however, studies have emerged indicating a compelling necessity to establish normative levels for serum magnesium. Because of the highest levels and agreement in results from different labs and locations, along with the health issues caused by low magnesium, it is suggested that normal values should be between 0.75–0.96 mmol/L or 0.85–0.96 mmol/L [29,30]. The lower cut-off point used in our study implies that we likely overlooked the diagnosis of asymptomatic hypomagnesemia more frequently; we know that overt symptoms of hypomagnesemia (muscle hyperactivity or weakness, tremors, seizures, headaches, fatigue, arrhythmias, and others) occur mainly at concentrations of <0.6 mmol/L [31]. In our forthcoming research, we will examine this element more thoroughly, seeking normative values that accurately represent the patient’s clinical status.
The present study has several limitations. Firstly, this is a retrospective study; however, we are planning a prospective study for the future to continuously verify the associations between magnesium levels and patients’ well-being and quality of life. Secondly, this study was performed on a medium–large cohort of patients, which, while satisfying the minimal sample size criterion, should be taken into account when planning the next stages of the research (as previously noted). Thirdly, the most important limitation of this study is the evaluation of hypomagnesemia through plasma magnesium concentration measurement; while this analytical method is widely utilized due to its feasibility and accessibility, it inadequately represents the actual issue of magnesium deficiency, as plasma magnesium levels do not correlate with tissue magnesium pools [32]. In the prospective study we are designing, we intend to concurrently evaluate magnesium levels in plasma, urine, and erythrocytes—the current results are, therefore, preliminary, enabling subsequent investigation. Directions for future research should also include prospective studies in humans to determine the temporal relationship and contribution of all components of the metabolic syndrome (with particular emphasis on the hyperglycemic component) to the development of hypomagnesemia.
Despite the above-mentioned study shortcomings, collectively, our findings and the existing literature highlight hyperglycemia as the predominant factor contributing to hypomagnesemia within the components of metabolic syndrome, bearing significant therapeutic implications for the management of micronutrient balance in these patients.
5. Conclusions
Among the components of metabolic syndrome, hyperglycemia shows the strongest and most significant independent association with an increased risk of hypomagnesemia. Individuals with diabetes and prediabetes need to take heightened attentiveness in maintaining enough magnesium intake and consider supplementation if a deficiency is present. Further research appears warranted to validate the pathophysiological foundation and implications of this causal link.
Author Contributions
Conceptualization, S.S. and R.J.; methodology, S.S. and R.J.; validation, S.S. and R.J.; formal analysis, S.S.; investigation, S.S.; resources, S.S.; data curation, S.S.; writing—original draft preparation, S.S.; writing—review and editing, S.S. and R.J.; visualization, S.S.; supervision, R.J.; project administration, S.S.; funding acquisition, S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Bioethics Committee of the Nicolaus Copernicus University functioning at Collegium Medicum in Bydgoszcz (approval code: 416/2024; date: 10 December 2024).
Informed Consent Statement
This study does not include the identifying information of individual participants. All data were obtained anonymously from the hospital database.
Data Availability Statement
The data can be made available upon reasonable request—please contact the corresponding author. The data are not publicly available due to the fact that they contain information that could compromise the privacy of research participants.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| 95%CI | 95% confidence interval |
| dBP | diastolic blood pressure |
| FPG | fasting plasma glucose |
| HDL-C | high-density lipoprotein cholesterol |
| IQR | interquartile range |
| OR | odds ratio |
| RR | relative risk |
| sBP | systolic blood pressure |
| sMg | serum magnesium |
| TG | serum triglycerides |
| WC | waist circumference |
References
- Dobrowolski, P.; Prejbisz, A.; Kuryłowicz, A.; Baska, A.; Burchardt, P.; Chlebus, K.; Dzida, G.; Jankowski, P.; Jaroszewicz, J.; Jaworski, P.; et al. Metabolic Syndrome—A New Definition and Management Guidelines. A Joint Position Paper by the Polish Society of Hypertension, Polish Society for the Treatment of Obesity, Polish Lipid Association, Polish Association for Study of Liver, Polish Society of Family Medicine, Polish Society of Lifestyle Medicine, Division of Prevention and Epidemiology Polish Cardiac Society, “Club 30” Polish Cardiac Society, and Division of Metabolic and Bariatric Surgery Society of Polish Surgeons. Arch. Med. Sci. 2022, 18, 1133–1156. [Google Scholar] [CrossRef] [PubMed]
- Suwała, S.; Junik, R. Assessment of the Liver Steatosis and Fibrosis Risk in Metabolic Syndrome and Its Individual Components, Considering the Varying Definitions Used in Clinical Practice throughout Time: A Retrospective Cross-Sectional Study. Biomedicines 2024, 12, 1739. [Google Scholar] [CrossRef] [PubMed]
- Suwała, S.; Junik, R. Body Mass Index and Waist Circumference as Predictors of Above-Average Increased Cardiovascular Risk Assessed by the SCORE2 and SCORE2-OP Calculators and the Proposition of New Optimal Cut-Off Values: Cross-Sectional Single-Center Study. J. Clin. Med. 2024, 13, 1931. [Google Scholar] [CrossRef] [PubMed]
- Šoher, L.; Banjari, I. Public Health Perspective on Magnesium. J. Appl. Health Sci. 2021, 7, 203–212. [Google Scholar] [CrossRef]
- EFSA Panel on Dietetic Products; Nutrition and Allergies (NDA). Scientific Opinion on Dietary Reference Values for Magnesium. EFSA J. 2015, 13, 4186. [Google Scholar] [CrossRef]
- Pelczyńska, M.; Moszak, M.; Bogdański, P. The Role of Magnesium in the Pathogenesis of Metabolic Disorders. Nutrients 2022, 14, 1714. [Google Scholar] [CrossRef]
- Sobhani, A.R.; Farshidi, H.; Azarkish, F.; Eslami, M.; Eftekhar, E.; Keshavarz, M.; Soltani, N. Magnesium Sulfate Improves Some Risk Factors for Atherosclerosis in Patients Suffering from One or Two Coronary Artery Diseases: A Double-Blind Clinical Trial Study. Clin. Pharmacol. 2020, 12, 159–169. [Google Scholar] [CrossRef]
- Weglicki, W.B. Hypomagnesemia and Inflammation: Clinical and Basic Aspects. Annu. Rev. Nutr. 2012, 32, 55–71. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the Metabolic Syndrome. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Rodríguez-Morán, M. Hypomagnesemia, Oxidative Stress, Inflammation, and Metabolic Syndrome. Diabetes Metab. Res. Rev. 2006, 22, 471–476. [Google Scholar] [CrossRef]
- Dibaba, D.T.; Xun, P.; Fly, A.D.; Yokota, K.; He, K. Dietary Magnesium Intake and Risk of Metabolic Syndrome: A Meta-analysis. Diabet. Med. 2014, 31, 1301–1309. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Morán, M.; Simental-Mendía, L.E.; Gamboa-Gómez, C.I.; Guerrero-Romero, F. Oral Magnesium Supplementation and Metabolic Syndrome: A Randomized Double-Blind Placebo-Controlled Clinical Trial. Adv. Chronic Kidney Dis. 2018, 25, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, A.; Zahediasl, S.; Syedmoradi, L.; Azizi, F. Low Serum Magnesium Levels in Elderly Subjects with Metabolic Syndrome. Biol. Trace Elem. Res. 2010, 136, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Simmons, D.; Joshi, S.; Shaw, J. Hypomagnesaemia Is Associated with Diabetes: Not Pre-Diabetes, Obesity or the Metabolic Syndrome. Diabetes Res. Clin. Pract. 2010, 87, 261–266. [Google Scholar] [CrossRef]
- Shugaa Addin, N.; Niedermayer, F.; Thorand, B.; Linseisen, J.; Seissler, J.; Peters, A.; Rospleszcz, S. Association of Serum Magnesium with Metabolic Syndrome and the Role of Chronic Kidney Disease: A Population-based Cohort Study with Mendelian Randomization. Diabetes Obes. Metab. 2024, 26, 1808–1820. [Google Scholar] [CrossRef]
- Barbagallo, M.; Veronese, N.; Dominguez, L.J. Magnesium in Type 2 Diabetes Mellitus, Obesity, and Metabolic Syndrome. Nutrients 2022, 14, 714. [Google Scholar] [CrossRef]
- Oost, L.J.; van Heck, J.I.P.; Tack, C.J.; de Baaij, J.H.F. The Association between Hypomagnesemia and Poor Glycaemic Control in Type 1 Diabetes Is Limited to Insulin Resistant Individuals. Sci. Rep. 2022, 12, 6433. [Google Scholar] [CrossRef]
- Swaminathan, R. Magnesium Metabolism and Its Disorders. Clin. Biochem. Rev. 2003, 24, 47–66. [Google Scholar]
- Liamis, G. Diabetes Mellitus and Electrolyte Disorders. World J. Clin. Cases 2014, 2, 488. [Google Scholar] [CrossRef]
- Palmer, B.F.; Clegg, D.J. Kidney-Protective Effects of SGLT2 Inhibitors. Clin. J. Am. Soc. Nephrol. 2023, 18, 279–289. [Google Scholar] [CrossRef]
- Pham, P.-C.; Pham, P.A.; Pham, S.; Pham, P.T.; Pham, P.M.; Pham, P.T. Hypomagnesemia: A Clinical Perspective. Int. J. Nephrol. Renovasc Dis. 2014, 7, 219–230. [Google Scholar] [CrossRef]
- Oost, L.J.; Tack, C.J.; de Baaij, J.H.F. Hypomagnesemia and Cardiovascular Risk in Type 2 Diabetes. Endocr. Rev. 2023, 44, 357–378. [Google Scholar] [CrossRef] [PubMed]
- Severino, P.; Netti, L.; Mariani, M.V.; Maraone, A.; D’Amato, A.; Scarpati, R.; Infusino, F.; Pucci, M.; Lavalle, C.; Maestrini, V.; et al. Prevention of Cardiovascular Disease: Screening for Magnesium Deficiency. Cardiol. Res. Pract. 2019, 2019, 4874921. [Google Scholar] [CrossRef]
- Lecube, A.; Baena-Fustegueras, J.A.; Fort, J.M.; Pelegrí, D.; Hernández, C.; Simó, R. Diabetes Is the Main Factor Accounting for Hypomagnesemia in Obese Subjects. PLoS ONE 2012, 7, e30599. [Google Scholar] [CrossRef] [PubMed]
- Guerrero-Romero, F.; Bermudez-Peña, C.; Rodríguez-Morán, M. Severe Hypomagnesemia and Low-Grade Inflammation in Metabolic Syndrome. Magnes. Res. 2011, 24, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Disorders of Magnesium Metabolism. EJIFCC 1999, 11, 36–44.
- Sontia, B.; Montezano, A.C.I.; Paravicini, T.; Tabet, F.; Touyz, R.M. Downregulation of Renal TRPM7 and Increased Inflammation and Fibrosis in Aldosterone-Infused Mice. Hypertension 2008, 51, 915–921. [Google Scholar] [CrossRef]
- Sajjan, N.; Shamsuddin, M. A Study of Serum Magnesium and Dyslipidemia in Type 2 Diabetes Mellitus Patients. Int. J. Clin. Biochem. Res. 2016, 3, 36. [Google Scholar] [CrossRef]
- Micke, O.; Vormann, J.; Kraus, A.; Kisters, K. Serum Magnesium: Time for a Standardized and Evidence-Based Reference Range. Magnes. Res. 2021, 34, 84–89. [Google Scholar] [CrossRef]
- Rosanoff, A.; West, C.; Elin, R.J.; Micke, O.; Baniasadi, S.; Barbagallo, M.; Campbell, E.; Cheng, F.-C.; Costello, R.B.; Gamboa-Gomez, C.; et al. Recommendation on an Updated Standardization of Serum Magnesium Reference Ranges. Eur. J. Nutr. 2022, 61, 3697–3706. [Google Scholar] [CrossRef]
- Ehrenpreis, E.D.; Jarrouj, G.; Meader, R.; Wagner, C.; Ellis, M. A Comprehensive Review of Hypomagnesemia. Dis. A Mon. 2022, 68, 101285. [Google Scholar] [CrossRef]
- Jahnen-Dechent, W.; Ketteler, M. Magnesium Basics. Clin. Kidney J. 2012, 5, i3–i14. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).