Utilisation of Group-Based Diabetes Education Programmes: Perspectives of Healthcare Practitioners
Abstract
1. Introduction
2. Research Design and Methods
2.1. Study Population
2.2. Data Collection
2.3. Ethical Implications
2.4. Data Analysis
3. Results
3.1. Theme 1. Organisation of Care
‘I have been practicing nursing for over 19 years and in the last couple of years we have had so many organisational changes such as the GP commissioning, Quality Outcome Framework changes, the Integrated Care Planning being brought in’.(Participant 6)
3.2. Targets
‘When QOF points came in, other less proactive GPs started firing off all these referrals for patients, so it overwhelmed the system’.(Participant 3)
‘There was a six month waiting list, and I think if there is a long wait, people will give up’.(Participant 6)
‘And again, you have too many people walking in, and because we are being judged and the boxes need to be ticked’.(Participant 1)
‘I think it is a memory jogger so that when they are with us and we are going through the template at their diabetic review and have you referred them to the diabetes education programme pops up, that is our trigger’.(Participant 2)
3.3. Limited Available Time
‘It really requires time, and time is one of the things we don’t have, we are constantly fighting the clock so that is the problem as I see it’.(Participant 6)
‘Yes, it’s time—we need to cover so much when you don’t know that person very well, unless you go through it fully, they will not understand’.(Participant 8)
3.4. Impact of Language Barrier
‘Language is a barrier, for example, we have a lot of people with too many dialects’.(Participant 3)
‘We have language problems so that takes a lot of the time when somebody doesn’t speak English, and I don’t speak Punjabi or anything’.(Participant 1)
3.5. Delivery of the Session
‘For working people in this area, there aren’t classes in the evening or at weekends, and at a time when they could actually get to them’.(Participant 7)
‘The session is not run at different times, and they are quite long sessions’.(Participant 4)
‘And they think oh that’s too far and I may not feel comfortable mixing with other people and may not understand what they are saying’.(Participant 2)
‘I found the elderly patients are more compliant. For example, if they live alone, it gets them out of the house to meet other people, and they may enjoy the programme’.(Participant 8)
‘Patients don’t like to travel, they like to be in their own area with their own people’.(Participant 4)
3.6. Individual Circumstances and Perceptions of Patients to Diabetes Education
‘Sometimes, it is health issues because they don’t feel well enough to attend’.(Participant 4)
‘Life is too busy for a youngster and too chaotic’.(Participant 6)
‘With the elderly sometimes, it is transport and mobility’.(Participant 8)
‘I mean they have childcare problems’.(Participant 7)
‘I forgot or I was too busy, and life gets in the way’.(Participant 1)
‘And a lot of these patients just don’t want to have diabetes, so they are very resistant to their diagnosis in the first place so anything else that they have to do on top of it, like just coming here, they are not at that point where they are willing to accept that’.(Participant 8)
‘Yes, health beliefs can be quite different, can’t they, and I think some people can put their trust in herbal things. We have a guy who has a long history of diabetes from Asia, and he is convinced that chewing this leaf his mother gave him is going to take away his diabetes, and he’s probably getting the hang of it now after about eight years’.(Participant 5)
‘A lot of my patients say to me oh my mother died of diabetes so they have a lot of wrong ideas about how diabetes can be treated, or maybe they don’t even know it can be well managed’.(Participant 1)
‘Some of my patients will say they are borderline; therefore, they don’t put enough effort’.(Participant 7)
‘And they say to us well I don’t feel ill… I haven’t got diabetes as I don’t feel ill’.(Participant 2)
‘Some may believe that God brought the disease, and the GP has nothing to do with it’.(Participant 4)
‘It’s a sort of sideline because they don’t see the importance of looking after themselves’.(Participant 2)
‘I suspect some people have a very negative experience of any sort of class and may have had a bad time at school, and so if they hear that this is a class, it might just make them turn off’.(Participant 4)
‘Generally, some patients don’t see it as part and parcel of their diabetes management’.(Participant 2)
‘Also, the issue of freedom of choice may affect their motivation to engage with the service’.(Participant 5)
‘Again, there is an issue with I have a choice, I know what I am doing; they think they know everything and don’t really think about the decisions they are making’.(Participant 7)
‘The more educated and the more affluent are quite keen, and ask you about the education, and they want to be referred to find out about diabetes and get along with life’.(Participant 8)
‘They go and actually research the information themselves, they may feel that they don’t actually need an education programme’.(Participant 8)
‘A patient said he knew more… than they could teach him’.(Participant 2)
‘Some also think they can get information from friends, family, and internet. They even go to American Diabetes association website and Canadian Diabetes association website without checking or thinking that their approaches might be different from us’.(Participant 6)
3.7. Strategies to Promote Attendance
‘If the education was near to the patient and at a time they could go because a lot of the patients are working’.(Participant 1)
‘You know if the education is here, other practices in my locality would come here rather than go up to the main hospital or go to a very far community centre’.(Participant 5)
‘I’m sure they would come because they are already familiar with the GP surgery and then seeing old faces. They can see the nurse that they are used to, and they would know’.(Participant 1)
‘I think putting it at convenient times, so have evening sessions maybe a Saturday morning session’.(Participant 6)
‘They may need to do more sessions in the summer holiday’.(Participant 4)
‘I think it’ll be far better to put energy into developing programmes so that people could either do an interactive online session, or have some sort of helpline available’(Participant 5)
‘Staffing of course, if there were twice as many nurses doing the job’.(Participant 5)
‘There is also the need for staff training’.(Participant 3)
‘The big industries or companies could also help with education, instead of just sending different types of glucose meters all the time, they could help with things like translation of pamphlets to other languages because we are curtailed with finances’.(Participant 3)
‘I think something like a welcoming letter or a phone call, and they would think oh they are expecting me, and someone is going to notice if I turn up or not, obviously they are more likely to attend’.(Participant 8)
‘Non-compliance is always a problem. I see it every day, you see patients telling you that I don’t take my water tablet when I am going out for a social event and you look down at their feet, it is very oedematous’.(Participant 3)
‘I don’t feel comfortable with sanctions as there must be a better way’.
‘I don’t think any financial sanction will work; after all, the NHS is free’.(Participant 7)
‘I think there would be an outcry, a complete outcry; patients won’t even pay their fine’.(Participant 8)
4. Discussion of Findings
5. Strengths and Limitations of the Study
6. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Diabetes: Fact Sheets. 2025. Available online: https://www.who.int/health-topics/diabetes#tab=tab_1 (accessed on 20 July 2025).
- Diabetes UK. How Many People in the UK Have Diabetes? 2025. Available online: https://www.diabetes.org.uk/professionals/position-statements-reports/statistics (accessed on 2 May 2025).
- Diabetes UK. Cost of Devastating Complications Highlight Urgent Need to Transform Diabetes Care in the UK. 2024. Available online: https://www.diabetes.org.uk/about-us/news-and-views/cost-complications-highlights-urgent-need-transform-diabetes (accessed on 14 August 2025).
- Diabetes UK. 50% of People Living with Diabetes Have Missed Healthcare Appointments due to Stigma Fear. Diabetes UK. 2023. Available online: https://www.diabetes.org.uk/about-us/news-and-views/50-people-living-diabetes-have-missed-healthcare-appointments-due-stigma (accessed on 11 June 2025).
- WHO. The Ottawa Charter for Health Promotion. 1986. Available online: https://bsahely.com/2018/09/12/the-ottawa-charter-for-health-promotion-who-1986/ (accessed on 2 May 2023).
- World Health Organization. The World Health Report 2008: Primary Health Care—Now More than Ever. World Health Organization: Geneva, Switzerland, 2008. Available online: https://iris.who.int/bitstream/handle/10665/69863/WHO_IER_WHR_08.1_eng.pdf?sequence=1&isAllowed=y (accessed on 15 August 2025).
- NICE. Type 2 Diabetes in Adults: Management. NICE Guidelines (NG28). 2022. Available online: https://www.nice.org.uk/guidance/ng28 (accessed on 30 May 2023).
- American Diabetes Association. ADA and ADCES Update National Standards for Diabetes Self-Management Education and Support. 2022. Available online: https://diabetes.org/newsroom/ada-and-adces-update-national-standards-for-diabetes-self-management-education-support (accessed on 15 August 2025).
- Diabetes UK. Diabetes Education: Learning to Look After Your Diabetes. 2025. Available online: https://www.diabetes.org.uk/about-diabetes/looking-after-diabetes/education (accessed on 14 August 2025).
- Currie, C.J.; Peyrot, M.; Morgan, C.L.; Poole, C.D.; Jenkins-Jones, S.; Rubin, R.R.; Burton, C.M.; Evans, M. The impact of treatment noncompliance on mortality in people with type 2 diabetes. Diabetes Care 2012, 35, 1279–1284. [Google Scholar] [CrossRef] [PubMed]
- NHS England. Reducing Did Not Attend (DNAs) in Outpatient Services. 2023. Available online: https://www.england.nhs.uk/long-read/reducing-did-not-attends-dnas-in-outpatient-services/ (accessed on 7 June 2025).
- NHS England. NHS AI Expansion to Help Tackle Missed Appointments and Improve Waiting Times. NHS England, 14 March 2024. Available online: https://www.england.nhs.uk/2024/03/nhs-ai-expansion-to-help-tackle-missed-appointments-and-improve-waiting-times/ (accessed on 15 August 2025).
- Gadot, T.; Azuri, J. Diabetes Control in the Community, Under the Management of a Diabetes-Clinic Nurse Specialist, and the Effect of a Parallel Diabetologist Advice. J. Prim. Care Community Health 2023, 14, 21501319231162310. [Google Scholar] [CrossRef] [PubMed]
- NHS England. NHS Long Term Plan. 2019. Available online: https://www.longtermplan.nhs.uk (accessed on 12 August 2025).
- Blumenthal-Barby, J.S. That’s the doctor’s job: Overcoming patient reluctance to be involved in medical decision making. Patient Educ. Couns. 2017, 100, 14–17. [Google Scholar] [CrossRef] [PubMed]
- Horigan, G.; Davies, M.; Findlay-White, F.; Chaney, D.; Coates, V. Reasons why patients referred to diabetes education programmes choose not to attend: A systematic review. Diabet. Med. 2017, 34, 14–26. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, N.; Cardwell, C.; Hughes, C.; O’Reilly, D. Increase in the pharmacological management of type 2 diabetes with pay-for-performance in primary care in the UK. Diabet. Med. 2015, 32, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Promberger, M.; Brown, R.; Ashcroft, R.E.; Marteau, T.M. Acceptability of financial incentives to improve health outcomes in UK and US samples. J. Med. Ethics 2011, 37, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, C.; Baruffati, D.; Mackenzie, M.; Ellis, D.A.; Major, M.; O’Donnell, C.A.; Simpson, S.A.; Williamson, A.E.; Wong, G. Understanding the causes of missingness in primary care: A realist review. BMC Med. 2024, 22, 235. [Google Scholar] [CrossRef] [PubMed]
- Lawal, M.; Woodman, A.; Fanghanel, J.; Ohl, M. Barriers to attendance at diabetes education centres: Perceptions of education providers. J. Diabetes Nurs. 2017, 21, 61–66. [Google Scholar]
- Ellis, D.A.; McQueenie, R.; McConnachie, A.; Wilson, P.; Williamson, A.E. Demographic and practice factors predicting repeated non-attendance in primary care: A national retrospective cohort analysis. Lancet Public Health 2017, 2, e551–e559. [Google Scholar] [CrossRef] [PubMed]
- The Kings Fund. Digital Triage in GP: Enhancing Access to Care or Increasing Inequalities? 2025. Available online: https://www.kingsfund.org.uk/insight-and-analysis/blogs/digital-triage-gp-access-care-inequalities (accessed on 15 August 2025).
- Rana, D.; Upton, D. Psychology for Nurses; Routledge: London, UK, 2013. [Google Scholar]
- Woodman, J.; Cross, R. Essentials of Health Promotion; Sage Publications Limited: London, UK, 2021. [Google Scholar]
- The Kings Fund. NHS Workforce in a Nutshell. Available online: https://www.kingsfund.org.uk/insight-and-analysis/data-and-charts/nhs-workforce-nutshell (accessed on 25 May 2023).
- Deakin, M. NHS workforce shortages and staff burnout are taking a toll. BMJ 2022, 377, o945. [Google Scholar] [CrossRef] [PubMed]
- Kenny, C. The 2013/14 General Medical Services contract: What we need to know for diabetes care. Diabetes Prim. Care 2013, 15, 73–76. [Google Scholar]
- McClean, S.; Bray, I.; Viggiani, N.; Bird, E.; Pilkington, P. Research Methods for Public Health; Sage: London, UK, 2020. [Google Scholar]
- Polit, D.; Beck, C. Nursing Research: Generating and Assessing Evidence for Nursing Practice, 11th ed.; Wolters Kluwer Health: London, UK, 2020. [Google Scholar]
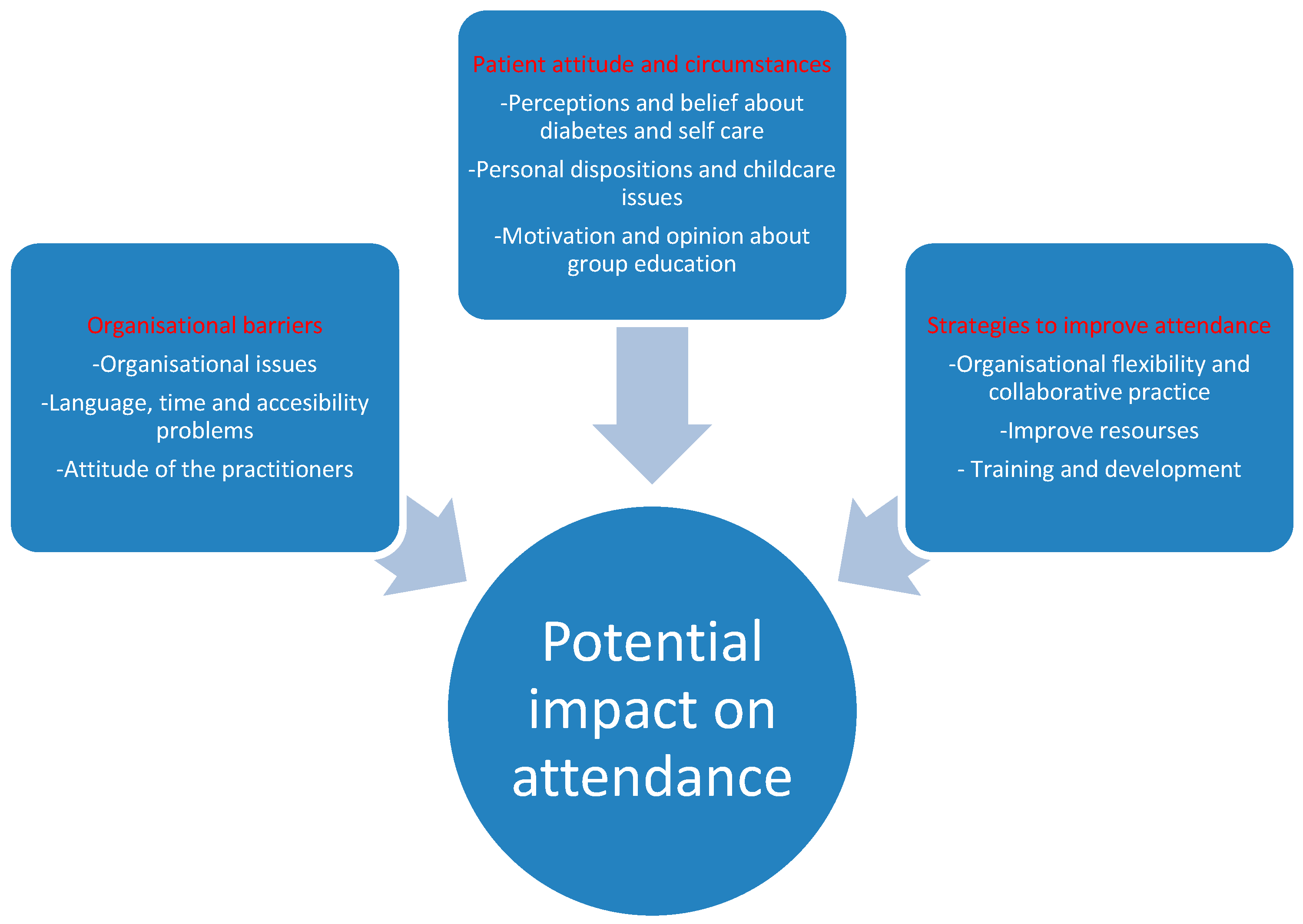
| Major Themes: | Sub Themes: |
|---|---|
| Organisation of care |
|
| Personal circumstances and attitudes of patients to diabetes education |
|
| Strategies to aid attendance |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lawal, M.O.; Woodman, A.; Lawal, F.A.; Omobayo, H.O. Utilisation of Group-Based Diabetes Education Programmes: Perspectives of Healthcare Practitioners. Diabetology 2025, 6, 136. https://doi.org/10.3390/diabetology6110136
Lawal MO, Woodman A, Lawal FA, Omobayo HO. Utilisation of Group-Based Diabetes Education Programmes: Perspectives of Healthcare Practitioners. Diabetology. 2025; 6(11):136. https://doi.org/10.3390/diabetology6110136
Chicago/Turabian StyleLawal, Muili Olugbenga, Anthony Woodman, Farouk Ayodeji Lawal, and Hameedat Olajumoke Omobayo. 2025. "Utilisation of Group-Based Diabetes Education Programmes: Perspectives of Healthcare Practitioners" Diabetology 6, no. 11: 136. https://doi.org/10.3390/diabetology6110136
APA StyleLawal, M. O., Woodman, A., Lawal, F. A., & Omobayo, H. O. (2025). Utilisation of Group-Based Diabetes Education Programmes: Perspectives of Healthcare Practitioners. Diabetology, 6(11), 136. https://doi.org/10.3390/diabetology6110136








