Engaging Primary Care Professionals and People at Risk of Type 2 Diabetes in the Design of PREDIABETEXT, a Multifaceted Digital Intervention Aimed at Preventing Type 2 Diabetes: A Qualitative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participant Selection and Recruitment
- -
- Healthcare professionals: We included primary healthcare physicians and nurses working in health centers in Mallorca (Spain). We recruited participants through our network of coordinators from primary care centers. They were purposefully sampled to ensure heterogeneity in terms of gender, age, and professional background (nurse or doctor).
- -
- Primary Care users: We included adults (>18 years old) with prediabetes (HbA1c: 6–6.4%, fasting plasma glucose: 110–125 mg/dL, or both). We used purposeful sampling to ensure diversity in terms of age and gender. Participant recruitment was assisted by the previously recruited professionals.
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
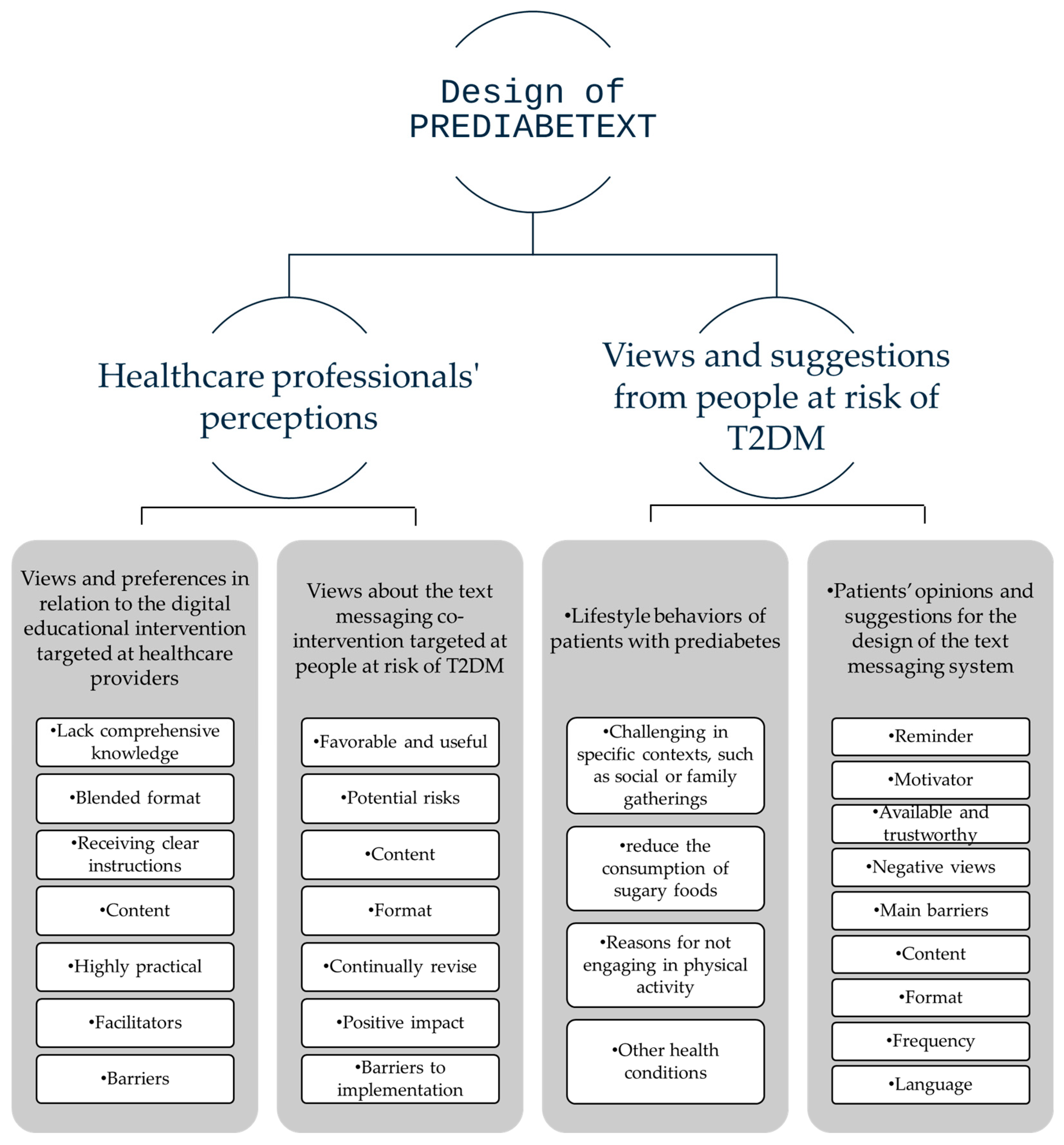
3.1. Healthcare Professionals’ Perceptions About PREDIABETEXT
3.1.1. Views and Preferences in Relation to the Digital Educational Intervention Targeted to Healthcare Providers
“I would find it quite beneficial because, in general, it’s true that we usually have more information about treating diabetes, but not so much focused on its prevention; and catching it in these early stages would be more interesting.”(Male nurse, 26 years old)
“(…) [An online format] it’s more accessible, it’s easier for professionals to get into it because they don’t have to travel; you can do it in a few hours. Often, training coincides with external commitments we have related to work, so it doesn’t allow us to attend”.(Female nurse, 42 years old)
“I think that first, we need to determine which patients we should be screening for prediabetes, and what type of intervention we should implement with them. It’s mainly about this—identifying which patients we should act upon and what we need to do for them.”(Female doctor, 51 years old)
“[we need] something very practical and feasible for us to do, let’s not complicate it with other stories that we can’t do. Clear things, an algorithm, I don’t know, what we have to do with these patients, what checks need to be done, tests, clear diet indications to offer them (…)”.(Female doctor, 50 years old)
3.1.2. Views About the Text Messaging Co-Intervention Targeted to People at Risk of T2DM
“Prediabetics come here once every six months or once a year for the test, and of course, you give them this message, but they forget, at least for six months until they return for this. So, they stick with their own criteria and what they have understood or what we have explained to them. This [the messaging intervention] is a way, I believe, to motivate them and remind them.”(Female doctor, 30 years old)
“I think when people see that they receive things from us, they think, ‘They care about me.’ That’s what we have to aim for, the empathy of saying, ‘Oh, they care.’ People love it when you care about them, don’t they? Because I also love it when people care about me.”(Female nurse, 62 years old)
“I think that graphic material, infographics, things like that, are faster, more visual, and don’t take much time.”(Male doctor, 47 years old)
“I think it’s great because it surely works, and it is welcomed by patients. It could lead to a reduction in diabetes cases, which is ultimately what it’s all about (…).”(Male nurse, 26 years old)
“I think that always must be agreed with the patient: ‘Do you want us to remind you at the end of the day to see if you’ve exercised or not?’ For example, I’m thinking. Among other things, maybe it wouldn’t be necessary every day, but I believe in negotiating this aspect with the patient.”(Female nurse, 51 years old)
3.2. Views and Suggestions from People at Risk of T2DM About PREDIABETEXT
3.2.1. Lifestyle Behaviors of Patients with Prediabetes
“The diet, yeah, some weeks are tougher than others, especially on the weekends. It’s like I let loose a bit psychologically on the weekends, you know? I’m like, “On the weekend, I can have a bit of, you know, pizza, and stuff like that.”(Female, 51 years old)
“Since we’ve been dealing with this pandemic and all, because I’ve always been big on exercising: gymnastics, running, cycling, weights, you name it, always. And now, for a year and a half or two, I’ve completely stopped. I’m not doing anything.”(Male, 47 years old)
3.2.2. Participants’ Opinions and Suggestions for the Design of the Text Messaging System
“The videos are good because you can just watch them, listen, pay attention if they’re interesting, and that’s it. No need to read anymore.”(Male, 69 years old)
“Like the warning on cigarette packs, showing the potential harm with harmful images. It creates a bit more awareness.”.(Female, 48 years old)
4. Discussion
4.1. Comparison with Previous Literature
4.2. Strengths and Limitations
4.3. Implications for Practice and Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Topic Guide for the Healthcare Professional’s Semi-Structured Interviews
- What do you think about the idea of receiving a course on prediabetes? (Relevant, necessary, useful, etc.)
- What format of training would you prefer? (In-person -preferred schedule-, blended, online)
- How would you like to receive the content? (Videos, case studies, scientific articles, text documents, etc.)
- What topics do you consider important to include? (Epidemiology, diagnostic criteria, preventive measures -diet and physical activity-, pharmacology in prediabetes, behavior modification, others)
- What difficulties do you think might arise for the acceptance of this training?
- What elements could facilitate the acceptance of training on this topic?
- Overall, what do you think about the idea of sending text messages to your patients to help them manage their lifestyles to prevent diabetes?
- What impact/response do you think these messages could have on your patients? What usefulness do you see in this type of intervention?
- What content do you think would be necessary to include in these messages? (Diet, exercise, others)
- PERSONALIZATION: Based on the information in medical records, how could we personalize (age, gender, socioeconomic status, physical activity questionnaire, predimed, postal code or Medea…), based on which variables could personalization be done?
- What possible impact could implement this service on a large scale have, as part of the IBSALUT service portfolio?
- What barriers or difficulties do you think could arise for the implementation of this service?
- Any other comments or suggestions that you think we should take into account when designing this messaging service?
Appendix B. Topic Guide for the Patient Interviews
- What should you do to avoid having high blood sugar? (diet and physical activity should come out)
- Among these factors, which one do you find most difficult to follow?
- What things help you? What works best for you?
- Regarding recommendations about diet, what difficulties do you face in maintaining an appropriate diet to help control your condition? What helps you overcome or deal with these difficulties?
- Regarding physical exercise, what difficulties do you encounter in maintaining a level of physical activity that helps control your blood sugar? What helps you overcome or deal with these difficulties?
- In general, how do you feel about the idea of receiving text messages on your mobile phone with information that could help you manage your prediabetes?
- To what extent do you think it could be useful in your daily life as a tool to address some of the problems you mentioned earlier?
- Do you have access to a mobile phone? Do you foresee any issues in accessing the text messages we might send to your phone?
- In general, what aspects do you think we should consider when launching this service, so that it is most positively received by patients?
- Would you prefer to receive information in a format other than text messages (audio, images, or others)?
- What content do you think these messages should include?
- What are your preferences regarding:
- Language of the messages
- Frequency of the messages
- Level of personalization (e.g., patient’s name)
- Ability for patients to personalize the type of message they receive (content, frequency, language, time of day received)
- Any other ideas or suggestions?
References
- NICE. Type 2 diabetes: Prevention in people at high risk. In NICE Guideline (PH38); NICE: London, UK, 2012. [Google Scholar]
- Mata-Cases, M.; Artola, S.; Escalada, J.; Ezkurra-Loyola, P.; Ferrer-García, J.C.; Fornos, J.A.; Girbés, J.; Rica, I. Consensus on the detection and management of prediabetes. Consensus and Clinical Guidelines Working Group of the Spanish Diabetes Society. Rev. Clínica Española (Engl. Ed.) 2015, 215, 117–129. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. IDF Diabetes Atlas, 8th ed.; International Diabetes Federation: Brussels, Belgium, 2017; Available online: http://www.diabetesatlas.org (accessed on 1 December 2024).
- Soriguer, F.; Goday, A.; Bosch-Comas, A.; Bordiu, E.; Calle-Pascual, A.; Carmena, R.; Casamitjana, R.; Castano, L.; Castell, C.; Catala, M.; et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: The Di@bet.es Study. Diabetologia 2012, 55, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Tabak, A.G.; Herder, C.; Rathmann, W.; Brunner, E.J.; Kivimaki, M. Prediabetes: A high-risk state for diabetes development. Lancet 2012, 379, 2279–2290. [Google Scholar] [CrossRef] [PubMed]
- Selvin, E.; Steffes, M.W.; Zhu, H.; Matsushita, K.; Wagenknecht, L.; Pankow, J.; Coresh, J.; Brancati, F.L. Glycated Hemoglobin, Diabetes, and Cardiovascular Risk in Nondiabetic Adults. N. Engl. J. Med. 2010, 362, 800–811. [Google Scholar] [CrossRef] [PubMed]
- NICE. Guidance on the use of patienteducation models for diabetes. In NICE Technology Appraisal Guidance 60; NICE: London, UK, 2014. [Google Scholar]
- Kolb, H.; Martin, S. Environmental/lifestyle factors in the pathogenesis and prevention of type 2 diabetes. BMC Med. 2017, 15, 131. [Google Scholar] [CrossRef] [PubMed]
- Patterson, E.M.H. Provider experiences of delivering nutrition focussed lifestyle interventions for adults with metabolic syndrome and obesity: A qualitative systematic review. JBI Evid Synth. 2020, 18, 1573–1579. [Google Scholar] [PubMed]
- Barengo, N.C.; Diaz Valencia, P.A.; Apolina, L.M.; Estrada Cruz, N.A.; Fernández Garate, J.E.; Correa González, R.A.; Cinco Gonzalez, C.A.; Gómez Rodriguez, J.A.; González, N.C.; Arellano Flores, M.L.; et al. Mobile Health Technology in the Primary Prevention of Type 2 Diabetes: A Systematic Review. Curr. Diabetes Rep. 2022, 22, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Jeem, Y.A.; Andriani, R.N.; Nabila, R.; Emelia, D.D.; Lazuardi, L.; Koesnanto, H. The use of mobile health interventions for outcomes among middle-aged and elderly patients with prediabetes: A systematic review. Int. J. Environ. Res. Public Health 2022, 19, 13638. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Morrison, L.; Bradbury, K.; Muller, I. The Person-Based Approach to Intervention Development: Application to Digital Health-Related Behavior Change Interventions. J. Med. Internet Res. 2015, 17, e30. [Google Scholar] [CrossRef] [PubMed]
- Galmes-Panades, A.M.; Angullo, E.; Mira-Martínez, S.; Bennasar-Veny, M.; Zamanillo-Campos, R.; Gómez-Juanes, R.; Konieczna, J.; Jiménez, R.; Serrano-Ripoll, M.J.; Fiol-deRoque, M.A.; et al. Development and Evaluation of a Digital Health Intervention to Prevent Type 2 Diabetes in Primary Care: The PREDIABETEXT Study Protocol for a Randomised Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 14706. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Reflecting on reflexive thematic analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Clarke, V.; Braun, V. Successful qualitative research: A practical guide for beginners. In Successful Qualitative Research; Sage: Thousand Oaks, CA, USA, 2013; pp. 1–400. [Google Scholar]
- Odendaal, W.A.; Anstey Watkins, J.; Leon, N.; Goudge, J.; Griffiths, F.; Tomlinson, M.; Daniels, K. Health workers’ perceptions and experiences of using mHealth technologies to deliver primary healthcare services: A qualitative evidence synthesis. Cochrane Database Syst. Rev. 2020, 3, Cd011942. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.R.; Sui, Y.; Ng, C.H.; Chen, Z.X.; Goh, L.H.; Shorey, S. Patients’ and healthcare professionals’ perspectives towards technology-assisted diabetes self-management education. A qualitative systematic review. PLoS ONE 2020, 15, e0237647. [Google Scholar] [CrossRef] [PubMed]
- Walsh, D.M.; Moran, K.; Cornelissen, V.; Buys, R.; Cornelis, N.; Woods, C. Electronic Health Physical Activity Behavior Change Intervention to Self-Manage Cardiovascular Disease: Qualitative Exploration of Patient and Health Professional Requirements. J. Med. Internet Res. 2018, 20, e163. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Shi, Q.; Zeng, Y.; Li, Y. Experiences and perceptions of self-management in people with prediabetes: A qualitative meta-synthesis. J. Clin. Nurs. 2023, 32, 5886–5903. [Google Scholar] [CrossRef] [PubMed]
- Elo, S.; Kääriäinen, M.; Kanste, O.; Pölkki, T.; Utriainen, K.; Kyngäs, H. Qualitative content analysis: A focus on trustworthiness. SAGE Open 2014, 4, 2158244014522633. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serrano-Ripoll, M.J.; Zamanillo-Campos, R.; Mira Martínez, S.; Fiol-deRoque, M.A.; Malih, N.; Angullo-Martínez, E.; Ricci-Cabello, I. Engaging Primary Care Professionals and People at Risk of Type 2 Diabetes in the Design of PREDIABETEXT, a Multifaceted Digital Intervention Aimed at Preventing Type 2 Diabetes: A Qualitative Study. Diabetology 2025, 6, 1. https://doi.org/10.3390/diabetology6010001
Serrano-Ripoll MJ, Zamanillo-Campos R, Mira Martínez S, Fiol-deRoque MA, Malih N, Angullo-Martínez E, Ricci-Cabello I. Engaging Primary Care Professionals and People at Risk of Type 2 Diabetes in the Design of PREDIABETEXT, a Multifaceted Digital Intervention Aimed at Preventing Type 2 Diabetes: A Qualitative Study. Diabetology. 2025; 6(1):1. https://doi.org/10.3390/diabetology6010001
Chicago/Turabian StyleSerrano-Ripoll, Maria Jesús, Rocío Zamanillo-Campos, Sofía Mira Martínez, Maria Antònia Fiol-deRoque, Narges Malih, Escarlata Angullo-Martínez, and Ignacio Ricci-Cabello. 2025. "Engaging Primary Care Professionals and People at Risk of Type 2 Diabetes in the Design of PREDIABETEXT, a Multifaceted Digital Intervention Aimed at Preventing Type 2 Diabetes: A Qualitative Study" Diabetology 6, no. 1: 1. https://doi.org/10.3390/diabetology6010001
APA StyleSerrano-Ripoll, M. J., Zamanillo-Campos, R., Mira Martínez, S., Fiol-deRoque, M. A., Malih, N., Angullo-Martínez, E., & Ricci-Cabello, I. (2025). Engaging Primary Care Professionals and People at Risk of Type 2 Diabetes in the Design of PREDIABETEXT, a Multifaceted Digital Intervention Aimed at Preventing Type 2 Diabetes: A Qualitative Study. Diabetology, 6(1), 1. https://doi.org/10.3390/diabetology6010001





