Transitioning to Telehealth during COVID-19: Experiences and Insights from Diabetes Prevention and Management Program Providers in Los Angeles County
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Setting
2.3. Participants
2.4. Data Collection
2.5. Qualitative Data Analysis
3. Results
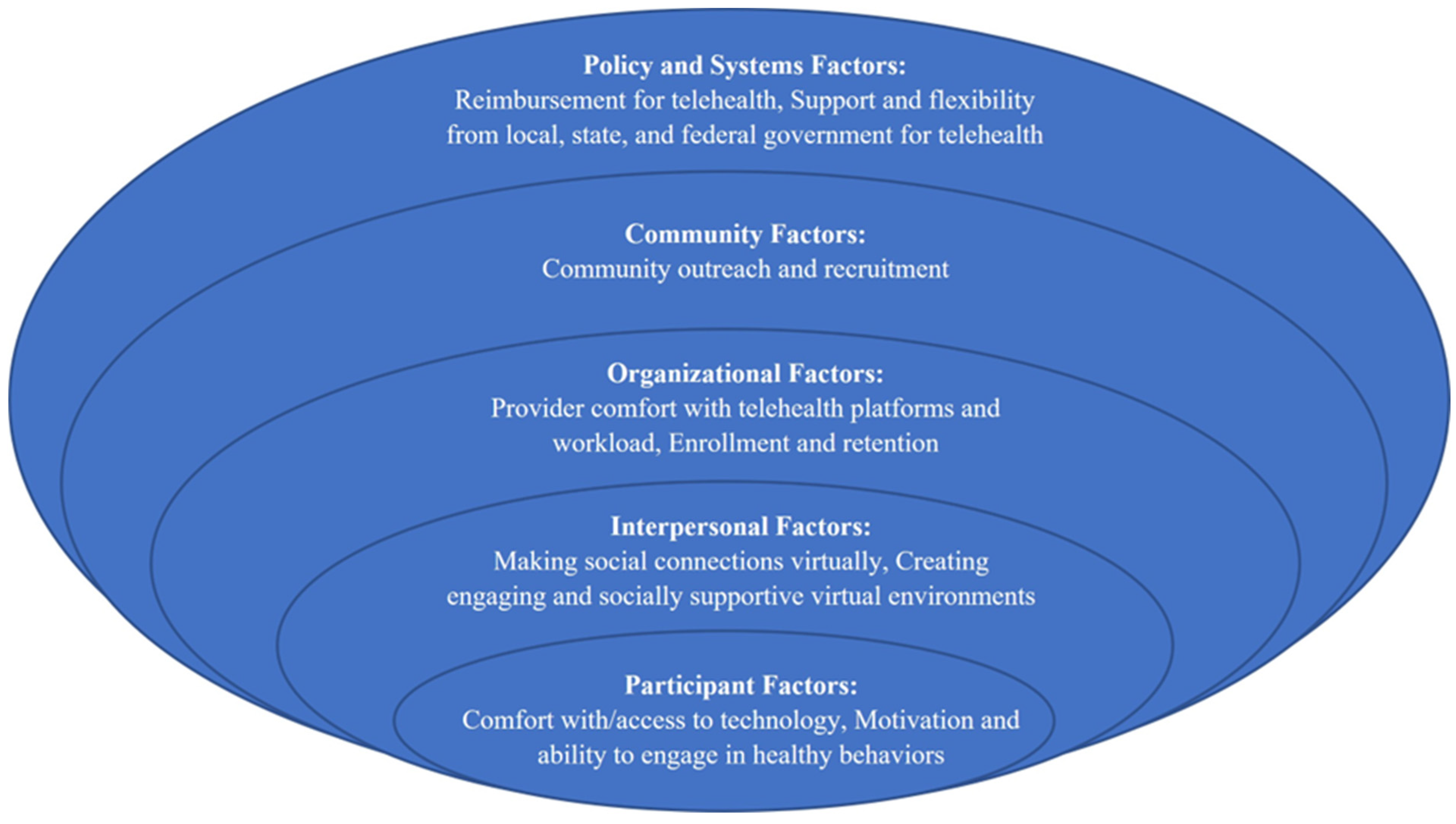
3.1. Major Themes
3.2. Individual Factors
3.2.1. Participant Comfort with and Access to Technology
“Maybe they are an 89-year-old grandmother who’s online all the time and is Queen of the internet…or maybe there’s someone that is not very familiar with technologies. We saw a big range within our communities.”
3.2.2. Participant Health Behaviors and Outcomes
“We saw activity in minutes plunder, and we saw those not so good eating habits go up…even though they knew staying healthy and maybe preventing diabetes would hopefully make them weather COVID better.”
3.2.3. Meeting Participants Where They Are
“People’s lives had to change. People were fearful…we would have to tell them these are some exercises you could do at home…or these are healthy recipes that you can make with the food that you would get at a food pantry or Food Bank.”
3.3. Interpersonal Factors
Social Support and Engagement
“The benefit of having an in-person workshop is the social aspect of it. People do feel more connected with each other, and they feel like they have the support of their peers. In the virtual [setting] that was a challenge…They’re just really not as connected with each other.
3.4. Organizational Factors
3.4.1. Telehealth Platforms and Technical Difficulties
“We had practice facilitation where I would have them take turns facilitating a class online and then provide feedback. So, there was a lot of training on that for my team.”
3.4.2. Provider Workload and Organizational Support
“You can provide a [telehealth] program. It’s one hour for the coach. It’s not all this travel and set up and talking time that really adds on an additional two hours for every meeting session. So, it’s much more streamlined, and that can open the possibilities for delivering the program at hours more populations can attend.”
3.4.3. Recruitment and Enrollment
“Switching to virtual allowed us to reach members that wouldn’t normally have the time to attend our in-person workshop. So, these are the working people and maybe the elderly who don’t want to drive to a site at night.”
3.4.4. Retention
3.5. Community Factors
“In a lot of these communities, the recruitment was very much this high-touch relationship-building with the community where you’re going out to health fairs, to congregate meal sites...Well, senior centers closed, the congregate meal site has become Meals on Wheels, the church is not servicing, senior housing is not letting anyone in, and the assisted living programs are on lockdown.”
3.6. Policy and Systems Factors
3.6.1. Local Government
“I think LA County Department of Public Health can continue being an advocate for health plans and vendors that provide the services and really take a role at the federal level to change some of these policies to provide more flexibility for populations covered by Medicare.”
3.6.2. State and Federal Government
3.6.3. Policy and Systems Changes Needed for National DPP
“The reimbursement needs to align, actually align with the high fixed costs of [National DPP]...It is very hard to start one of these programs and sustain it over time. You have to be incredibly efficient to be able to do that with Medi-Cal or Medicare DPP reimbursement.”
3.6.4. Policy and Systems Changes Needed for DSMES
“[DSMES providers] are afraid to bill [Medicare] because they’re afraid they’re going to do something wrong. And all they’re trying to do is take care of their patients, and they get shut down because they’re not sustainable financially.”
3.7. Beyond the Pandemic: The Future of Telehealth
“[Telehealth] provides a way in another way into the program. And with 88 million people who have prediabetes, you need as many doors as possible into this program.”
4. Discussion
4.1. Limitations
4.2. Implications for Policy and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Centers for Disease Control and Prevention. The National Diabetes Statistics Report. Available online: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf (accessed on 23 September 2021).
- Los Angeles County Department of Public Health. Key Indicators of Health by Service Planning Area. Available online: http://publichealth.lacounty.gov/ha/docs/2015LACHS/KeyIndicator/PH-KIH_2017-sec%20UPDATED.pdf (accessed on 9 December 2021).
- Centers for Disease Control and Prevention. Diabetes Report Card 2019. Available online: https://www.cdc.gov/diabetes/pdfs/library/Diabetes-Report-Card-2019-508.pdf (accessed on 6 December 2021).
- Sacks, L.J.; Pham, C.T.; Fleming, N.; Neoh, S.L.; Ekinci, E.I. Considerations for people with diabetes during the Coronavirus Disease (COVID-19) pandemic. Diabetes Res. Clin. Pract. 2020, 166, 108296. [Google Scholar] [CrossRef] [PubMed]
- Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Albright, A.L.; Gregg, E.W. Preventing type 2 diabetes in communities across the U.S.: The National Diabetes Prevention Program. Am. J. Prev. Med. 2013, 44, S346–S351. [Google Scholar] [CrossRef] [PubMed]
- United States Congress. H.R.4124–Diabetes Prevention Act of 2009. Available online: https://www.congress.gov/bill/111th-congress/house-bill/4124 (accessed on 5 August 2021).
- Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: The Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol 2015, 3, 866–875. [Google Scholar] [CrossRef]
- Chrvala, C.A.; Sherr, D.; Lipman, R.D. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ. Couns. 2016, 99, 926–943. [Google Scholar] [CrossRef]
- National Consortium of Telehealth Resource Centers. A Framework for Defining Telehealth. Available online: https://cchp.nyc3.digitaloceanspaces.com/2021/04/Telehealth-Definintion-Framework-for-TRCs_0.pdf (accessed on 26 October 2021).
- Powers, M.A.; Bardsley, J.K.; Cypress, M.; Funnell, M.M.; Harms, D.; Hess-Fischl, A.; Hooks, B.; Isaacs, D.; Mandel, E.D.; Maryniuk, M.D.; et al. Diabetes self-management education and support in adults with type 2 diabetes: A consensus report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care 2020, 43, 1636–1649. [Google Scholar] [CrossRef]
- Joiner, K.L.; Nam, S.; Whittemore, R. Lifestyle interventions based on the diabetes prevention program delivered via eHealth: A systematic review and meta-analysis. Prev. Med. 2017, 100, 194–207. [Google Scholar] [CrossRef]
- Grock, S.; Ku, J.H.; Kim, J.; Moin, T. A review of technology-assisted interventions for diabetes prevention. Curr. Diab. Rep. 2017, 17, 107. [Google Scholar] [CrossRef]
- Appuswamy, A.V.; Desimone, M.E. Managing diabetes in hard to reach populations: A review of telehealth interventions. Curr. Diab. Rep. 2020, 20, 28. [Google Scholar] [CrossRef]
- McDaniel, C.C.; Kavookjian, J.; Whitley, H.P. Telehealth delivery of motivational interviewing for diabetes management: A systematic review of randomized controlled trials. Patient Educ. Couns. 2021, 105, 805–820. [Google Scholar] [CrossRef]
- Robson, N.; Hosseinzadeh, H. Impact of telehealth care among adults living with type 2 diabetes in primary care: A systematic review and meta-analysis of randomised controlled trials. Int. J. Environ. Res. Public Health 2021, 18, 12171. [Google Scholar] [CrossRef] [PubMed]
- Los Angeles County Public Health Department. Find a Diabetes Self–Management Education and Support Program Near You. Available online: http://publichealth.lacounty.gov/phcommon/public/dsmesearch.cfm (accessed on 9 December 2021).
- Los Angeles County Public Health Department. Find a National Diabetes Prevention Program. Available online: http://publichealth.lacounty.gov/phcommon/public/nationaldpp.cfm (accessed on 9 December 2021).
- Modi, P.K.; Kaufman, S.R.; Portney, D.S.; Ryan, A.M.; Hollenbeck, B.K.; Ellimoottil, C. Telemedicine utilization by providers in accountable care organizations. Mhealth 2019, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Crossen, S.; Raymond, J.; Neinstein, A. Top 10 tips for successfully implementing a diabetes telehealth program. Diabetes Technol. Ther. 2020, 22, 920–928. [Google Scholar] [CrossRef]
- Harvey, J.B.; Valenta, S.; Simpson, K.; Lyles, M.; McElligott, J. Utilization of outpatient telehealth services in parity and nonparity states 2010–2015. Telemed J. E Health 2019, 25, 132–136. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, S.; Hanlon, P.; O’Donnell, C.A.; Garcia, S.; Glanville, J.; Mair, F.S. Understanding factors affecting patient and public engagement and recruitment to digital health interventions: A systematic review of qualitative studies. BMC Med. Inform. Decis. Mak. 2016, 16, 120. [Google Scholar] [CrossRef] [PubMed]
- Phimphasone-Brady, P.; Chiao, J.; Karamsetti, L.; Sieja, A.; Johnson, R.; Macke, L.; Lum, H.; Lee, R.; Farro, S.; Loeb, D.; et al. Clinician and staff perspectives on potential disparities introduced by the rapid implementation of telehealth services during COVID-19: A mixed-methods analysis. Transl. Behav. Med. 2021, 11, 1339–1347. [Google Scholar] [CrossRef]
- Almathami, H.K.Y.; Win, K.T.; Vlahu-Gjorgievska, E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: Systematic literature review. J. Med. Internet Res. 2020, 22, e16407. [Google Scholar] [CrossRef]
- ATLAS.ti Scientific Software Development GmbH. ATLAS.ti 22 Windows, Version 22.0.6.0. 2022.
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Hong, Y.R.; Lawrence, J.; Williams, D., Jr.; Mainous, I.A. Population-level interest and telehealth capacity of US hospitals in response to COVID-19: Cross-sectional analysis of google search and national hospital survey data. JMIR Public Health Surveill 2020, 6, e18961. [Google Scholar] [CrossRef]
- Fischer, S.H.; Predmore, Z.; Roth, E.; Uscher-Pines, L.; Baird, M.; Breslau, J. Use of and willingness to use video telehealth through the COVID-19 pandemic. Health Aff. 2022, 41, 1645–1651. [Google Scholar] [CrossRef] [PubMed]
- Rozga, M.; Handu, D.; Kelley, K.; Jimenez, E.Y.; Martin, H.; Schofield, M.; Steiber, A. Telehealth during the COVID-19 pandemic: A cross-sectional survey of registered dietitian nutritionists. J. Acad Nutr. Diet. 2021, 121, 2524–2535. [Google Scholar] [CrossRef] [PubMed]
- Kirley, K.; Sachdev, N. Digital health-supported lifestyle change programs to prevent type 2 diabetes. Diabetes Spectr. 2018, 31, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Odom, J.; Beauchamp, C.; Fiocchi, C.; Eicken, M.; Stancil, M.; Turner, J.; Bruch, J. Rapid innovation in diabetes care during Covid-19. ADCES Pract. 2020, 8, 28–32. [Google Scholar] [CrossRef]
- Ansari, R.M.; Harris, M.F.; Hosseinzadeh, H.; Zwar, N. Experiences of diabetes self-management: A focus group study among the middle-aged population of rural pakistan with type 2 diabetes. Diabetology 2022, 3, 17–29. [Google Scholar] [CrossRef]
- Naja, F.; Hamadeh, R. Nutrition amid the COVID-19 pandemic: A multi-level framework for action. Eur. J. Clin. Nutr. 2020, 74, 1117–1121. [Google Scholar] [CrossRef]
- Mattioli, A.V.; Sciomer, S.; Cocchi, C.; Maffei, S.; Gallina, S. Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1409–1417. [Google Scholar] [CrossRef]
- Davis, T.C.; Hoover, K.W.; Keller, S.; Replogle, W.H. Mississippi diabetes telehealth network: A collaborative approach to chronic care management. Telemed. J. E Health 2020, 26, 184–189. [Google Scholar] [CrossRef]
- Vadheim, L.M.; McPherson, C.; Kassner, D.R.; Vanderwood, K.K.; Hall, T.O.; Butcher, M.K.; Helgerson, S.D.; Harwell, T.S. Adapted diabetes prevention program lifestyle intervention can be effectively delivered through telehealth. Diabetes Educ. 2010, 36, 651–656. [Google Scholar] [CrossRef]
- Vadheim, L.M.; Patch, K.; Brokaw, S.M.; Carpenedo, D.; Butcher, M.K.; Helgerson, S.D.; Harwell, T.S. Telehealth delivery of the diabetes prevention program to rural communities. Transl. Behav. Med. 2017, 7, 286–291. [Google Scholar] [CrossRef]
- Taetzsch, A.; Gilhooly, C.H.; Bukhari, A.; Das, S.K.; Martin, E.; Hatch, A.M.; Silver, R.E.; Montain, S.J.; Roberts, S.B. Development of a videoconference-adapted version of the community diabetes prevention program, and comparison of weight loss with in-person program delivery. Mil. Med. 2019, 184, 647–652. [Google Scholar] [CrossRef]
- Tate, D.F.; Jackvony, E.H.; Wing, R.R. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: A randomized trial. JAMA Am. Med. Assoc. 2003, 289, 1833–1836. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.; DeMasi, M. The importance of teaching virtual rapport-building skills in telehealth curricula. Acad. Med. 2021, 96, 1231–1232. [Google Scholar] [CrossRef] [PubMed]
- Knotowicz, H.; Haas, A.; Coe, S.; Furuta, G.T.; Mehta, P. Opportunities for innovation and improved care using telehealth for nutritional interventions. Gastroenterology 2019, 157, 594–597. [Google Scholar] [CrossRef]
- Thomas, E.E.; Haydon, H.M.; Mehrotra, A.; Caffery, L.J.; Snoswell, C.L.; Banbury, A.; Smith, A.C. Building on the momentum: Sustaining telehealth beyond COVID-19. J. Telemed. Telecare 2022, 28, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Ariel-Donges, A.H.; Gordon, E.L.; Dixon, B.N.; Eastman, A.J.; Bauman, V.; Ross, K.M.; Perri, M.G. Rural/urban disparities in access to the National Diabetes Prevention Program. Transl. Behav. Med. 2020, 10, 1554–1558. [Google Scholar] [CrossRef] [PubMed]
- Gruß, I.; Mayhew, M.; Firemark, A.; Fitzpatrick, S.L. Participants’ perspectives on perceived usefulness of digital and in-person diabetes prevention programs: A qualitative study to inform decisions related to program participation. Obes. Sci. Pract. 2022, 8, 176–184. [Google Scholar] [CrossRef]
- The Center for Connected Health Policy. COVID-19 Telehealth Coverage Policies. Available online: https://www.cchpca.org/resources/covid-19-telehealth-coverage-policies/ (accessed on 19 October 2021).
- Centers for Medicare & Medicaid Services. President Trump Expands Telehealth Benefits for Medicare Beneficiaries During COVID-19 Outbreak. Available online: https://www.cms.gov/newsroom/press-releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-during-covid-19-outbreak (accessed on 5 October 2021).
- Anthony Jnr, B. Implications of telehealth and digital care solutions during COVID-19 pandemic: A qualitative literature review. Inform. Health Soc. Care 2021, 46, 68–83. [Google Scholar] [CrossRef]
- Hoffman, D.A. Increasing access to care: Telehealth during COVID-19. J. Law Biosc. 2020, 7, lsaa049. [Google Scholar] [CrossRef] [PubMed]
| Program Delivery before the Pandemic | Program Delivery after Start of the Pandemic | ||||||
|---|---|---|---|---|---|---|---|
| In-Person Delivery | Telehealth | Continued to Offer Primarily Telehealth | Switched to Telehealth National DPP | Stopped Offering National DPP | Switched to Telehealth DSMES | Stopped Offering DSMES | |
| National DPP ONLY | 9 | 1 * | 1 | 6 | 3 | N/A | N/A |
| DSMES ONLY | 5 | 0 | 0 | N/A | N/A | 5 | 0 |
| National DPP and DSMES | 10 | 1 * | 1 | 8 | 2 | 9 | 1 |
| Factors | Themes | Representative Quote(s) |
|---|---|---|
| Individual Participant Factors: Challenges and optimal practices influencing participants’ ability to successfully participate in telehealth National DPP and DSMES | ||
| Access to and comfort with technology | Comfort and access to technology among participants was mixed Tailored and consistent technical assistance helped many participants overcome issues with technology Despite providers’ efforts, some participants were not willing or able to engage in telehealth | “We had some groups where 50% of our group didn’t have access to a phone… And then we had other groups that made the switch very easily… [They had] access to the internet”. National DPP Expert and Provider “We created a little handout flyer with like a one pager on the steps on how to connect to the class. And we mailed it to them. We use that and we use phone calls to guide them through it”. National DPP and DSMES Provider |
| Motivation and ability to engage in healthy behaviors | Challenges collecting health data via telehealth made it difficult to determine the impact of the transition on health behaviors Participants’ motivation and ability to engage in healthy behaviors and achieve certain health outcomes was mixed Providers helped participants set individualized goals to overcome challenges and provided resources when needed | “They really didn’t want to share their weights. Also, we heard several people saying that they don’t have access to a weighing scale. So that kind of decreased the number of people reporting weights”. National DPP Provider “There was a lot of stress on participants and instead of trying to reach the DPP goal of weight loss, perhaps they would just focus on weight maintenance”. National DPP Provider |
| Interpersonal Factors: Challenges and optimal practices for facilitating relationships and engagement in a virtual environment | ||
| Creating engaging virtual environments and making social connections virtually | Establishing relationships between participants and between participants and providers was challenging in a virtual environment Modifying materials and delivery of curriculum, using the platform functions, sending group texts, and creating social media groups increased engagement and connection Hybrid approaches (in-person and telehealth) may be useful for establishing relationships and improving telehealth sessions | “They can connect to us. The language, the culture, we live in this community. And that helped us to have a very successful in-person class. But how do I make that connection virtually? It’s just not there”. National DPP and DSMES Provider “I hate to say that it’s kind of like edutainment, so the more colorful and the more interesting your materials are, the more you’ll get their attention”. National DPP Provider |
| Organizational Factors: Overcoming provider and organizational barriers to providing telehealth and maintaining enrollment and retention in the programs | ||
| Provider comfort with telehealth platforms | Comfort and familiarity with telehealth platforms and delivery was mixed among providers Training sessions for providers can be helpful for overcoming challenges with platforms and telehealth delivery Contingency plans are needed to deal with technical challenges | “Our Diabetes Prevention Program teams were not on the cutting edge of providing telehealth programming. So, there was a big learning curve for them”. National DPP Provider “Your platform might be great and awesome, but the internet might go out...I always have a dial-in conference line so everyone can get on the phone and talk”. National DPP Expert and Provider |
| Provider workload | Transitioning to telehealth increased the workload of many providers initially but may ultimately save time and allow for program expansion | “You don’t have to travel. You don’t have to go anywhere. You can run it from your home office...So those two to three, or even four hours can be used for education...It can be evolved into providing more classes”. National DPP Expert and Provider |
| Enrollment and retention | Programs experienced an initial drop in enrollment and retention, but many recovered and were able to expand and reach different audiences Telehealth availability increased accessibility of programs to individuals who could not participate in-person | “Now we are able to provide a DPP in summer in Florida or even Hawaii, anywhere they want…that was a great change that we were able to adapt to be more nationwide rather than just stay in Southern California”. National DPP Expert and Provider “Our enrollment actually probably was better, because people didn’t have to drive here and try and find a parking space. And it could fit into their time without them really leaving their home”. DSMES Provider |
| Community Factors: Challenges external to organizations resulting from the COVID-19 pandemic | ||
| Community outreach and recruitment | The closure of community recruitment locations due to the pandemic made outreach and recruitment difficult for some providers Providers had to shift recruitment methods | “Recruitment was hard because we couldn’t go to places and give our nutrition workshops or hang up flyers”. National DPP Provider |
| Policy and Systems Change Factors: Policy-level barriers and support needed from government agencies for telehealth | ||
| Reimbursement for telehealth and support/flexibility from government agencies for telehealth | Changes to National DPP eligibility requirements and flexibility for maintaining DPRP recognition are needed Adequate and sustained coverage for telehealth is needed from Medicare and Medicaid | “I think once you are recognized, you should be able to go back and forth and do both [in-person and distance learning] if you want to, instead of being pegged into just one track”. National DPP Provider “Medicare has to be in-person. And I think for a lot of Medicare participants, being virtual would probably be really good for them because a lot of times they don’t have transportation, or they have to be with a caregiver”. DSMES Provider “Coverage for services virtually needs to be set in stone...Now, it’s sort of vague, and I don’t know how long it’s gonna last...With very clear policies and procedures, and coverage for virtual services, I think in my community, it will increase participation in [DSMES]”. DSMES Provider |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bullock, S.L.; Menendez, T.; Schwarte, L.; Craypo, L.; Mosst, J.T.; Green, G.; Barragan, N.C.; Kuo, T. Transitioning to Telehealth during COVID-19: Experiences and Insights from Diabetes Prevention and Management Program Providers in Los Angeles County. Diabetology 2023, 4, 46-61. https://doi.org/10.3390/diabetology4010006
Bullock SL, Menendez T, Schwarte L, Craypo L, Mosst JT, Green G, Barragan NC, Kuo T. Transitioning to Telehealth during COVID-19: Experiences and Insights from Diabetes Prevention and Management Program Providers in Los Angeles County. Diabetology. 2023; 4(1):46-61. https://doi.org/10.3390/diabetology4010006
Chicago/Turabian StyleBullock, Sally L., Telma Menendez, Liz Schwarte, Lisa Craypo, Jennifer T. Mosst, Gabrielle Green, Noel C. Barragan, and Tony Kuo. 2023. "Transitioning to Telehealth during COVID-19: Experiences and Insights from Diabetes Prevention and Management Program Providers in Los Angeles County" Diabetology 4, no. 1: 46-61. https://doi.org/10.3390/diabetology4010006
APA StyleBullock, S. L., Menendez, T., Schwarte, L., Craypo, L., Mosst, J. T., Green, G., Barragan, N. C., & Kuo, T. (2023). Transitioning to Telehealth during COVID-19: Experiences and Insights from Diabetes Prevention and Management Program Providers in Los Angeles County. Diabetology, 4(1), 46-61. https://doi.org/10.3390/diabetology4010006







