Sleep Deprivation: A Lifestyle Risk Factor for Male Infertility
Abstract
1. Introduction
2. Materials and Methods
3. Results
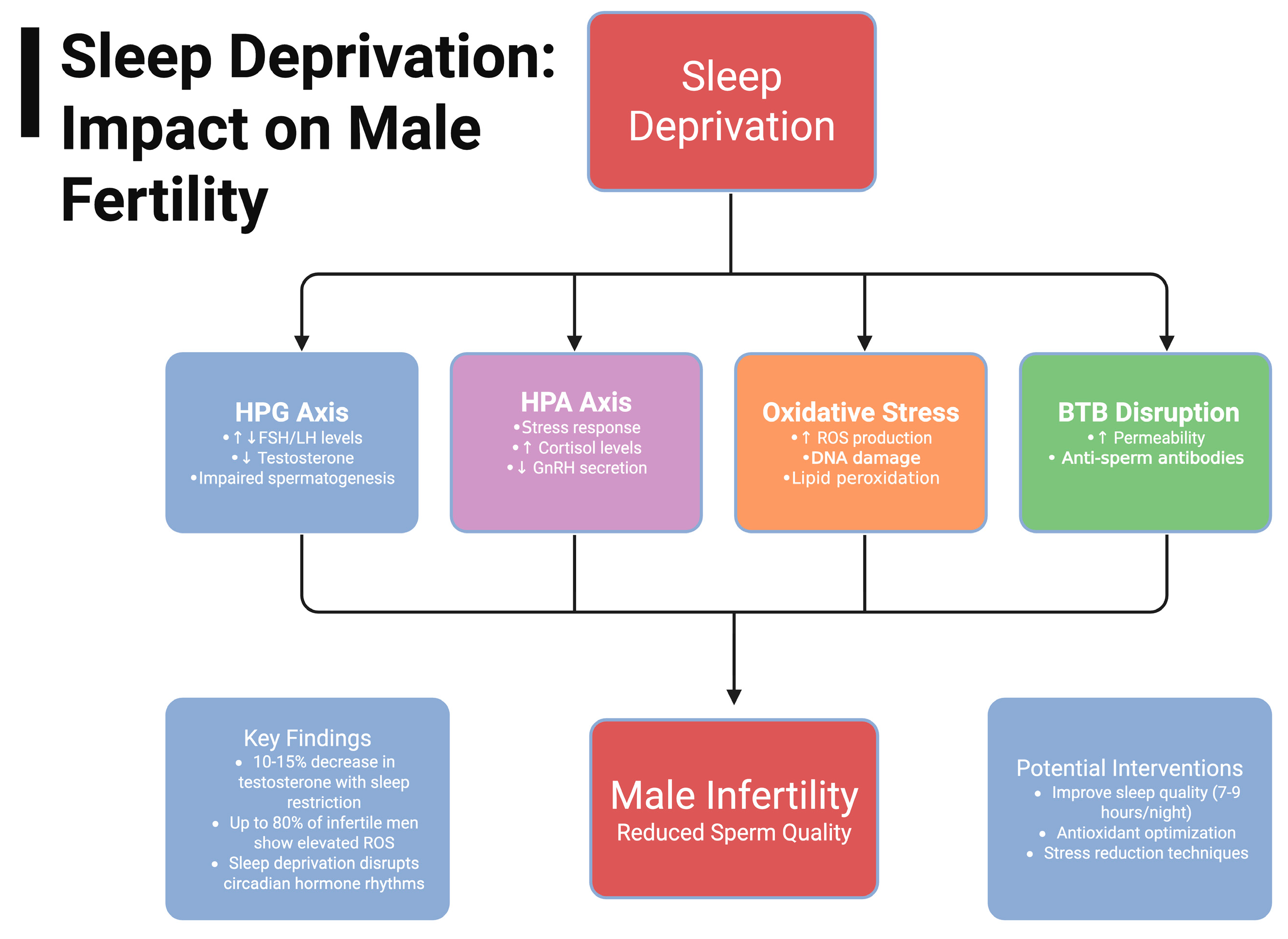
3.1. Hypothalamic–Pituitary–Gonadal Axis
3.1.1. FSH/LH
3.1.2. Testosterone
3.2. Hypothalamus–Pituitary–Adrenal Axis
Cortisol
3.3. Oxidative Stress
3.3.1. Stress and Sleep
3.3.2. Factors Affecting Oxidative Stress
3.4. Testes
3.4.1. Disruption of Blood-Testis Barrier
3.4.2. Mechanisms of BTB Disruption
3.4.3. L-Cysteine
3.4.4. Aging
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Eisenberg, M.L.; Esteves, S.C.; Lamb, D.J.; Hotaling, J.M.; Giwercman, A.; Hwang, K.; Cheng, Y.-S. Male infertility. Nat. Rev. Dis. Prim. 2023, 9, 49. [Google Scholar] [CrossRef]
- GBD 2021 Fertility and Forecasting Collaborators. Global fertility in 204 countries and territories, 1950–2021, with forecasts to 2100: A comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2057–2099. [Google Scholar] [CrossRef] [PubMed]
- Choshen-Hillel, S.; Ishqer, A.; Mahameed, F.; Reiter, J.; Gozal, D.; Gileles-Hillel, A.; Berger, I. Acute and chronic sleep deprivation in residents: Cognition and stress biomarkers. Med. Educ. 2021, 55, 174–184. [Google Scholar] [CrossRef] [PubMed]
- Gold, E.B.; Tomich, E. Occupational hazards to fertility and pregnancy outcome. Occup. Med. 1994, 9, 435–469. [Google Scholar]
- Győrffy, Z.; Dweik, D.; Girasek, E. Reproductive health and burn-out among female physicians: Nationwide, representative study from Hungary. BMC Women’s Health 2014, 14, 121. [Google Scholar] [CrossRef]
- Seliger, B. Created in BioRender. 2025. Available online: https://BioRender.com (accessed on 6 August 2025).
- Lee, D.S.; Choi, J.B.; Sohn, D.W. Impact of Sleep Deprivation on the Hypothalamic–Pituitary–Gonadal Axis and Erectile Tissue. J. Sex. Med. 2019, 16, 5–16. [Google Scholar] [CrossRef]
- Patel, P.; Shiff, B.; Kohn, T.P.; Ramasamy, R. Impaired sleep is associated with low testosterone in US adult males: Results from the National Health and Nutrition Examination Survey. World J. Urol. 2019, 37, 1449–1453. [Google Scholar] [CrossRef]
- DeMorrow, S. Role of the Hypothalamic–Pituitary–Adrenal Axis in Health and Disease. Int. J. Mol. Sci. 2018, 19, 986. [Google Scholar] [CrossRef]
- Schieber, M.; Chandel, N.S. ROS function in redox signaling and oxidative stress. Curr. Biol. 2014, 24, R453–R462. [Google Scholar] [CrossRef] [PubMed]
- Takalani, N.B.; Monageng, E.M.; Mohlala, K.; Monsees, T.K.; Henkel, R.; Opuwari, C.S. Role of oxidative stress in male infertility. Reprod. Fertil. 2023, 4, e230024. [Google Scholar] [CrossRef]
- Senaratna, C.V.; Perret, J.L.; Lodge, C.J.; Lowe, A.J.; Campbell, B.E.; Matheson, M.C.; Hamilton, G.S.; Dharmage, S.C. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med. Rev. 2017, 34, 70–81. [Google Scholar] [CrossRef]
- Stanek, A.; Brożyna-Tkaczyk, K.; Myśliński, W.; Szewczyk-Golec, K. Oxidative Stress Markers among Obstructive Sleep Apnea Patients. Oxid. Med. Cell. Longev. 2021, 2021, 9681595. [Google Scholar] [CrossRef]
- Domínguez-Salazar, E.; Hurtado-Alvarado, G.; Medina-Flores, F.; Dorantes, J.; González-Flores, O.; de Oca, A.C.; Velázquez-Moctezuma, J.; Gómez-González, B. Chronic sleep loss disrupts blood–testis and blood–epididymis barriers, and reduces male fertility. J. Sleep Res. 2020, 29, e12907. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.Y.; Mruk, D.D. The blood-testis barrier and its implications for male contraception. Pharmacol. Rev. 2012, 64, 16–64. [Google Scholar] [CrossRef]
- Francavilla, F.; Santucci, R.; Barbonetti, A. Naturally-occurring antisperm antibodies in men: Interference with fertility and clinical implications. An update. Front. Biosci. J. Virtual Libr. 2007, 12, 2890–2911. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Wang, H.; Chen, Z.; Gao, H.; Gao, P.; Gao, J.; Jiang, H.; Zhang, X. Impact of chronic sleep deprivation on male reproductive health: Insights from testicular and epididymal responses in mice. Andrology 2024, 13, 968–977. [Google Scholar] [CrossRef]
- Cai, X.-F.; Zhao, J.-M.; Yang, Y.-S.; Wang, C.-Y.; Nian, M.-X.; Huang, J.-F.; Wang, B.-Y. Self-reported sleep quality and oligo/astheno/teratozoospermia among men attending an infertility clinic: A longitudinal study. Sleep Breath. 2023, 27, 1465–1471. [Google Scholar] [CrossRef] [PubMed]
- Alvarenga, T.A.; Fernandes, G.L.; Bittencourt, L.R.; Tufik, S.; Andersen, M.L. The effects of sleep deprivation and obstructive sleep apnea syndrome on male reproductive function: A multi-arm randomised trial. J. Sleep Res. 2023, 32, e13664. [Google Scholar] [CrossRef]
- Rehman, R.; Amjad, S.; Tariq, H.; Zahid, N.; Akhter, M.; Ashraf, M. Oxidative stress and male infertility: A cross sectional study. J. Pak. Med. Assoc. 2020, 70, 461–466. [Google Scholar] [CrossRef]
- Karasek, M.; Pawlikowski, M.; Nowakowska-Jankiewicz, B.; Kolodziej-Maciejewska, H.; Zieleniewski, J.; Cieslak, D.; Leidenberger, F. Circadian variations in plasma melatonin, FSH, LH, and prolactin and testosterone levels in infertile men. J. Pineal Res. 1990, 9, 149–157. [Google Scholar] [CrossRef]
- Viganò, P.; Chiaffarino, F.; Bonzi, V.; Salonia, A.; Ricci, E.; Papaleo, E.; Mauri, P.A.; Parazzini, F. Sleep disturbances and semen quality in an Italian cross sectional study. Basic Clin. Androl. 2017, 27, 16. [Google Scholar] [CrossRef] [PubMed]
- Du, C.-Q.; Yang, Y.-Y.; Chen, J.; Feng, L.; Lin, W.-Q. Association Between Sleep Quality and Semen Parameters and Reproductive Hormones: A Cross-Sectional Study in Zhejiang, China. Nat. Sci. Sleep 2020, 12, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Mulgund, A.; Hamada, A.; Chyatte, M.R. A unique view on male infertility around the globe. Reprod. Biol. Endocrinol. 2015, 13, 37. [Google Scholar] [CrossRef]
- Kohn, T.P.; Kohn, J.R.; Haney, N.M.; Pastuszak, A.W.; Lipshultz, L.I. The effect of sleep on men’s health. Transl. Androl. Urol. 2020, 9 (Suppl. S2), S178–S185. [Google Scholar] [CrossRef]
- Schmid, S.M.; Hallschmid, M.; Jauch-Chara, K.; Lehnert, H.; Schultes, B. Sleep timing may modulate the effect of sleep loss on testosterone. Clin. Endocrinol. 2012, 77, 749–754. [Google Scholar] [CrossRef]
- Leproult, R.; Van Cauter, E. Effect of 1 week of sleep restriction on testosterone levels in young healthy men. JAMA 2011, 305, 2173–2174. [Google Scholar] [CrossRef]
- Choi, J.H.; Lee, S.H.; Bae, J.H.; Shim, J.S.; Park, H.S.; Kim, Y.S.; Shin, C. Effect of Sleep Deprivation on the Male Reproductive System in Rats. J. Korean Med. Sci. 2016, 31, 1624–1630. [Google Scholar] [CrossRef]
- Oh, M.M.; Kim, J.W.; Jin, M.H.; Kim, J.J.; Moon, D.G. Influence of paradoxical sleep deprivation and sleep recovery on testosterone level in rats of different ages. Asian J. Androl. 2012, 14, 330–334. [Google Scholar] [CrossRef] [PubMed]
- Charlier, C.M.; Barr, M.L.; Colby, S.E.; Greene, G.W.; Olfert, M.D. Correlations of Self-Reported Androgen Deficiency in Ageing Males (ADAM) with Stress and Sleep among Young Adult Males. Healthcare 2018, 6, 121. [Google Scholar] [CrossRef]
- Joseph, D.N.; Whirledge, S. Stress and the HPA Axis: Balancing Homeostasis and Fertility. Int. J. Mol. Sci. 2017, 18, 2224. [Google Scholar] [CrossRef]
- Azmi, N.A.S.M.; Juliana, N.; Azmani, S.; Effendy, N.M.; Abu, I.F.; Teng, N.I.M.F.; Das, S. Cortisol on Circadian Rhythm and Its Effect on Cardiovascular System. Int. J. Environ. Res. Public Health 2021, 18, 676. [Google Scholar] [CrossRef]
- Nollet, M.; Wisden, W.; Franks, N.P. Sleep deprivation and stress: A reciprocal relationship. Interface Focus 2020, 10, 20190092. [Google Scholar] [CrossRef]
- Wright, K.P.; Drake, A.L.; Frey, D.J.; Fleshner, M.; Desouza, C.A.; Gronfier, C.; Czeisler, C.A. Influence of sleep deprivation and circadian misalignment on cortisol, inflammatory markers, and cytokine balance. Brain Behav. Immun. 2015, 47, 24–34. [Google Scholar] [CrossRef]
- Derenzo, J.; Macknight, B.; DiVittore, N.A.; Bonafide, C.P.; Cronin, A.J. Postoperative elevated cortisol excretion is not associated with suppression of 6-sulfatoxymelatonin excretion. Acta Anaesthesiol. Scand. 2005, 49, 52–57. [Google Scholar] [CrossRef]
- Castro-Diehl, C.; Roux, A.V.D.; Redline, S.; Seeman, T.; Shrager, S.E.; Shea, S. Association of Sleep Duration and Quality With Alterations in the Hypothalamic-Pituitary Adrenocortical Axis: The Multi-Ethnic Study of Atherosclerosis (MESA). J. Clin. Endocrinol. Metab. 2015, 100, 3149–3158. [Google Scholar] [CrossRef]
- Shukla, K.K.; Mahdi, A.A.; Ahmad, M.K.; Jaiswar, S.P.; Shankwar, S.N.; Tiwari, S.C. Mucuna pruriens Reduces Stress and Improves the Quality of Semen in Infertile Men. Evid.-Based Complement. Altern. Med. 2010, 7, 137–144. [Google Scholar] [CrossRef]
- Agarwal, A.; Parekh, N.; Selvam, M.K.P.; Henkel, R.; Shah, R.; Homa, S.T.; Ramasamy, R.; Ko, E.; Tremellen, K.; Esteves, S.; et al. Male Oxidative Stress Infertility (MOSI): Proposed Terminology and Clinical Practice Guidelines for Management of Idiopathic Male Infertility. World J. Men’s Health 2019, 37, 296–312. [Google Scholar] [CrossRef] [PubMed]
- Barati, E.; Nikzad, H.; Karimian, M. Oxidative stress and male infertility: Current knowledge of pathophysiology and role of antioxidant therapy in disease management. Cell. Mol. Life Sci. 2020, 77, 93–113. [Google Scholar] [CrossRef]
- Lei, X.; Xu, Z.; Chen, W. Association of oxidative balance score with sleep quality: NHANES 2007–2014. J. Affect. Disord. 2023, 339, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Nargund, V.H. Effects of psychological stress on male fertility. Nat. Rev. Urol. 2015, 12, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Alahmar, A.T. Role of Oxidative Stress in Male Infertility: An Updated Review. J. Hum. Reprod. Sci. 2019, 12, 4–18. [Google Scholar] [CrossRef]
- Łakoma, K.; Kukharuk, O.; Śliż, D. The Influence of Metabolic Factors and Diet on Fertility. Nutrients 2023, 15, 1180. [Google Scholar] [CrossRef] [PubMed]
- Krzastek, S.C.; Farhi, J.; Gray, M.; Smith, R.P. Impact of environmental toxin exposure on male fertility potential. Transl. Androl. Urol. 2020, 9, 2797–2813. [Google Scholar] [CrossRef]
- Omolaoye, T.S.; Skosana, B.T.; Ferguson, L.M.; Ramsunder, Y.; Ayad, B.M.; Du Plessis, S.S. Implications of Exposure to Air Pollution on Male Reproduction: The Role of Oxidative Stress. Antioxidants 2024, 13, 64. [Google Scholar] [CrossRef] [PubMed]
- Minas, A.; Fernandes, A.C.C.; Júnior, V.L.M.; Adami, L.; Intasqui, P.; Bertolla, R.P. Influence of physical activity on male fertility. Andrologia 2022, 54, e14433. [Google Scholar] [CrossRef]
- Hamim, F.M.; Durairajanayagam, D.; Daud, S.B.; Singh, H.J.; Baker, M. Physical activity and male reproductive function. Reprod. Fertil. Dev. 2025, 37, RD24196. [Google Scholar] [CrossRef]
- Shen, Y.; You, Y.; Zhu, K.; Fang, C.; Yu, X.; Chang, D. Bibliometric and visual analysis of blood-testis barrier research. Front. Pharmacol. 2022, 13, 969257. [Google Scholar] [CrossRef]
- Margret, J.J.; Jain, S.K. The Protective Role of L-Cysteine in the Regulation of Blood–Testis Barrier Functions—A Brief Review. Genes 2024, 15, 1201. [Google Scholar] [CrossRef]
- Zhang, W.; Shi, X.; Zhang, Y.; Liu, G.; Wu, X.; Huang, H.; Jiang, H.; Zhang, X. Attenuation Effect of Recovery Sleep for Impaired Reproductive Function in Male Rats by Sleep Deprivation. World J. Men’s Health 2023, 41, 671–679. [Google Scholar] [CrossRef]
- Chen, Q.; Yang, H.; Zhou, N.; Sun, L.; Bao, H.; Tan, L.; Chen, H.; Ling, X.; Zhang, G.; Huang, L.; et al. Inverse U-shaped Association between Sleep Duration and Semen Quality: Longitudinal Observational Study (MARHCS) in Chongqing, China. Sleep 2016, 39, 79–86. [Google Scholar] [CrossRef] [PubMed]

| Study | Design | Key Findings |
|---|---|---|
| Domínguez-Salazar, E et al. [14] (2020) | Experimental Animal Model using Winstar Rats | Sleep restriction increased permeability of blood-testis and -epididymis barriers. |
| Zheng, Z et al. [17] (2024) | Experimental Animal Model using ICR Male Mice | Decreased sperm concentration and motility. Increased levels of OS in testis and epididymis. |
| Cai, X et al. [18] (2023) | Longitudinal Study with 466 males | Subjective poorer sleep quality was measured in men with OAT |
| Alvarenga, T et al. [19] (2023) | RCT, 46 candidates, aged 20–40 | OSA patients had lower ejaculated sperm count and semen volume along with higher % of sperm with abnormal morphology. |
| Rehman, R et al. [20] (2020) | Cross-sectional Case–Control study with 376 males | Increased levels of cortisol and decreased antioxidant, GPX, levels in infertile males compared to fertile. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davuluri, T.; Aslot, V.; Seliger, B.J.; Edgington, A.; Nadiminty, N.; Shah, T.; Sindhwani, P. Sleep Deprivation: A Lifestyle Risk Factor for Male Infertility. Uro 2025, 5, 17. https://doi.org/10.3390/uro5030017
Davuluri T, Aslot V, Seliger BJ, Edgington A, Nadiminty N, Shah T, Sindhwani P. Sleep Deprivation: A Lifestyle Risk Factor for Male Infertility. Uro. 2025; 5(3):17. https://doi.org/10.3390/uro5030017
Chicago/Turabian StyleDavuluri, Tarak, Vivek Aslot, Brayden J. Seliger, Andrew Edgington, Nagalakshmi Nadiminty, Tariq Shah, and Puneet Sindhwani. 2025. "Sleep Deprivation: A Lifestyle Risk Factor for Male Infertility" Uro 5, no. 3: 17. https://doi.org/10.3390/uro5030017
APA StyleDavuluri, T., Aslot, V., Seliger, B. J., Edgington, A., Nadiminty, N., Shah, T., & Sindhwani, P. (2025). Sleep Deprivation: A Lifestyle Risk Factor for Male Infertility. Uro, 5(3), 17. https://doi.org/10.3390/uro5030017








