Abstract
The use of ileum for ureteral reconstruction was first described in 1906. Since then, its utilization has evolved considerably. Early in the history of ileal ureters, urologists were limited by a lack of familiarity with bowel harvesting and handling. The popularization of ileal conduits for urinary diversions, however, allowed urologists to familiarize themselves with the use of ileum and paved the way for broader applications. With the emergence of laparoscopy and, later, robotic-assisted surgery, the application of ileal ureteral replacement expanded the capabilities of reconstructive urologists. This article describes the historical development of surgical techniques for ileal ureter replacement and the integration of new technologies aiding in improved outcomes, and anticipates potential future directions. In contemporary practice, robotic-assisted ileal ureteral replacement is used in cases of extensive ureteral obstruction or damage. Advantages of the robotic platform include reduced blood loss, shorter recovery time and hospital length of stay, and superior operative ergonomics. Although robotic ileal ureter replacement is a complex and challenging surgery with notable complications, studies have demonstrated the efficacy and safety of this technique in patients with an otherwise end-stage ureter. In addition, the robotic approach has provided urologists the ability to conduct complex reconstructive surgeries including bilateral ureteral replacement in conjunction with bladder augmentation or a urinary diversion. Long-term studies and continued innovation are necessary to further improve the surgical techniques, outcomes, and scope of ileal ureter reconstruction.
1. Introduction
The robotic-assisted laparoscopic intracorporeal ileal ureter replacement (RIUR) surgery is the product of decades of surgical innovation and offers a minimally invasive treatment option for patients with severe long segment ureteral stricture disease or obstruction. Conditions such as malignancy, trauma, stricture disease, or congenital anomalies can render the ureter obstructed or nonfunctional. In these cases, using a segment of ileum to reconstruct the ureteral tract can be a durable and effective solution [1,2]. Over time, advancements in surgical technology have redefined how this surgery has been performed, with the robotic-assisted laparoscopic (RAL) approach now establishing a new standard of precision and care. This article explores the evolution of the RIUR surgery, focusing on its conception and evolution, present implementation, and future directions.
Ileal ureter replacement (IUR), either open or robotic, involves substituting the nonfunctioning ureter using a segment of ileum. A portion of ileum is isolated with its blood supply intact and anastomosed proximally to the renal pelvis or proximal ureter and distally to the bladder or distal ureter, creating a new conduit for previously impaired urine to drain. Historically, the surgery was performed open until the introduction of laparoscopic surgery and as a result, the laparoscopic ileal ureter replacement (LIUR) technique [3,4]. While the laparoscopic approach improved recovery times and reduced complications, limitations such as restricted instrument maneuverability and two-dimensional visualization posed significant challenges, especially in complex reconstruction [5]. RAL surgery addresses these limitations, offering greater precision, enhanced visualization, and improved ergonomics [6,7,8]. These advancements have made RIUR surgery the preferred approach in many tertiary centers, particularly for complex cases.
Today, the RAL platform allows surgeons to perform increasingly complex reconstructive surgery that likely could not have been completed open, including bilateral ureteral replacement (BIUR) as well as ureteral reconstruction in conjunction with bladder augmentation and various urinary diversions [9,10]. While these advancements have expanded the utility of IUR, ongoing innovation is vital to address the challenges posed by such cases. Emerging technologies, including advanced imaging and integration with artificial intelligence, have the potential to improve surgical planning, execution, and outcomes.
This article examines the RIUR surgery from its origins to its current applications and cutting-edge developments. By tracing the procedure’s evolution from open to laparoscopic to robotic techniques, we aim to highlight the impact of RAL surgery on surgical outcomes and explore how ongoing innovation may further transform complex ureteral reconstruction and improve patient outcomes.
2. Foundations
2.1. Early History
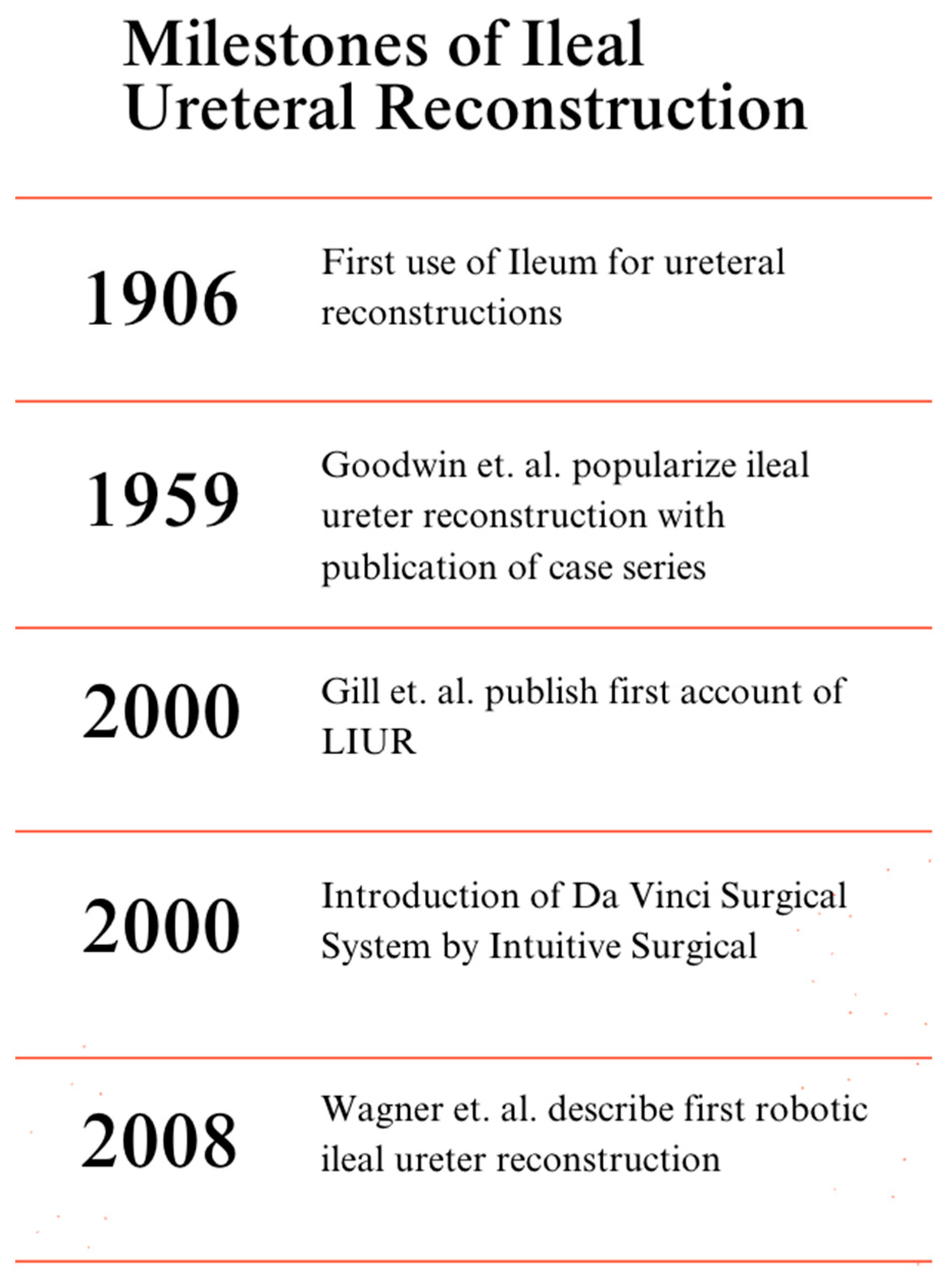
The use of ileum for ureteral replacement was first described by Shoemaker in 1906 but was popularized in the 1950s by Goodwin et al. [11,12] (Figure 1). While broad adoption of the use of ileum by urologists was limited early on, the popularization of ileal conduits for cutaneous urinary diversion provided a foundation for further applications of ileal segments in urology [12]. IUR was initially described for use in ureteral obstruction in advanced tuberculosis but its use has since grown substantially in reconstructive urology [11]. In general, IUR became a viable option for cases in which a significant portion of the native ureter was damaged or obstructed and other parts of the urinary tract could not be used for reconstruction. Early pioneers of the ileal ureter strongly advised that, when possible, techniques avoiding bowel manipulation should be employed including primary uretero-ureteral anastomosis, bridging bladder flaps, and/or transureteroureterostomy [12]. However, for patients with long defects that could not be repaired via the above approaches and were dependent on a chronic nephrostomy tube or ureteral stent, the use of ileum became a versatile tool in the belt of reconstructive urologists.
Figure 1.
Timeline of milestone achievements in the history of IUR [3,6,11,12,13].
2.2. Laparoscopy
Prior to the advancement of laparoscopic surgery, all ileal ureters were performed open. While laparoscopy grew in popularity and scope in all surgical fields throughout the 20th century, IUR continued to be performed exclusively in an open fashion [14]. This changed in 2000 when Gill et al. published the first account of an LIUR [3]. They utilized a 3-port approach and demonstrated that the LIUR was able to mimic established principles from open surgical techniques while being efficient and feasible [3]. While the employment of this technique boasted all of the advantages of laparoscopic surgery including less blood loss, shorter hospital stays, less scarring, lower rates of infection, among many others, it also presented additional challenges. Traditional laparoscopy severely limits the surgeon’s dexterity thus making suturing and intricate tissue manipulation challenging. Thus, laparoscopic surgical outcomes are highly correlated to a surgeon’s skill and experience level. It is then no surprise that the leap from traditional laparoscopy to RIUR took place more rapidly than the transition from open to laparoscopy.
3. Robotic Advances
3.1. History and Advantages
RIUR surgery is an advanced minimally invasive procedure that replaces or reconstructs an obstructed ureter using a segment of ileum. The robotic approach offers superior surgical precision, enhanced visualization, and greater dexterity compared to traditional open or laparoscopic methods [8,13,15]. IUR is indicated for patients with extensive ureteral damage often caused by trauma, surgical complications, radiation, or inflammatory conditions such as retroperitoneal fibrosis [16,17]. Although the procedure is complex and associated with potential complications, it can provide a viable solution for patients with an otherwise end-stage ureter where prior interventions have failed.
The history of RAL surgery began in the late 20th century, with the development of robotic systems aimed at improving surgical precision and outcomes. The Da Vinci Surgical System, introduced by Intuitive Surgical in 2000, revolutionized minimally invasive procedures by incorporating robotic arms with three-dimensional high-definition imaging, and tremor filtration [13]. Initially approved for general laparoscopic procedures, the Da Vinci system rapidly gained acceptance across multiple specialties, including urology, gynecology, and cardiothoracic surgery. The first robotic ileal ureter reconstruction was described in 2008 by Wagner and colleagues, marking a significant milestone in urologic surgery [6]. This breakthrough expanded the role of robotic systems in urology, setting the stage for innovations in minimally invasive surgical techniques.
The robotic approach provides substantial advantages over traditional surgical techniques. Robotic arms enable unparalleled precision and fine motor control, which are essential for a meticulous dissection, maintaining vasculature, and creating a water-tight anastomosis. The robot’s superior visualization with high-definition three-dimensional imaging and easy maneuverability in the pelvis allows for improved access to previously difficult to navigate anatomy and a challenging surgical field [18]. These technological advancements have shown to reduce blood loss and allow for smaller incisions, shorter recovery times, and lower morbidity when compared to open surgery. For patients, these benefits can translate into quicker recovery times and overall improved outcomes [8].
For surgeons, the robotic platform significantly enhances ergonomics and reduces physical strain during lengthy procedures. Compared to open and laparoscopic surgery, robotics allow for greater precision, improved visualization, and easier intracorporeal dissecting and suturing, which results in the successful completion of a complex reconstructive surgery [18]. Together, these advantages highlight the transformative impact of RAL surgery on the modern urologic practice.
3.2. Patient Selection
Appropriate patient selection is critical to achieving successful outcomes in robotic ileal ureter reconstruction. A patient’s prior medical and surgical history must be obtained, the extent and location of ureteral obstruction as well as baseline renal function and split renal function should be evaluated, and the suitability of ileum for reconstruction must be determined. Patients appropriate for ileal ureteral replacement are those with long-segment strictures. For strictures distal to the iliac vessels and less than 10 cm in length, our practice is to perform a ureteroneocystotomy with psoas hitch, Boari Flap or buccal mucosal grafting as needed to facilitate a tension-free anastomosis. Proximal to the iliac vessels, strictures less than 10 cm will be treated with a ureteroureterostomy or buccal graft ureteroplasty. If strictures are longer than 10 cm, we commonly employ ileal ureteral replacement.
Contraindications to ileal ureteral replacement include conditions such as inflammatory bowel disease, neurogenic bladder, short gut syndrome, and bladder outlet obstruction [19]. IUR is an important technique often considered when other surgical approaches have been unsuccessful or not feasible. Surgeons must council patients on the risk of long-term complications such as bile acid malabsorption, nephrolithiasis, and cholelithiasis, which can result from the use of intestinal segments in the urinary tract [20]. Counseling patients about the possibility of requiring ileal replacement and the associated risks ensures informed decision-making and sets appropriate expectations for recovery and long-term management. Preoperative bowel preparation is not routinely required for IUR [21,22].
3.3. Surgical Techniques
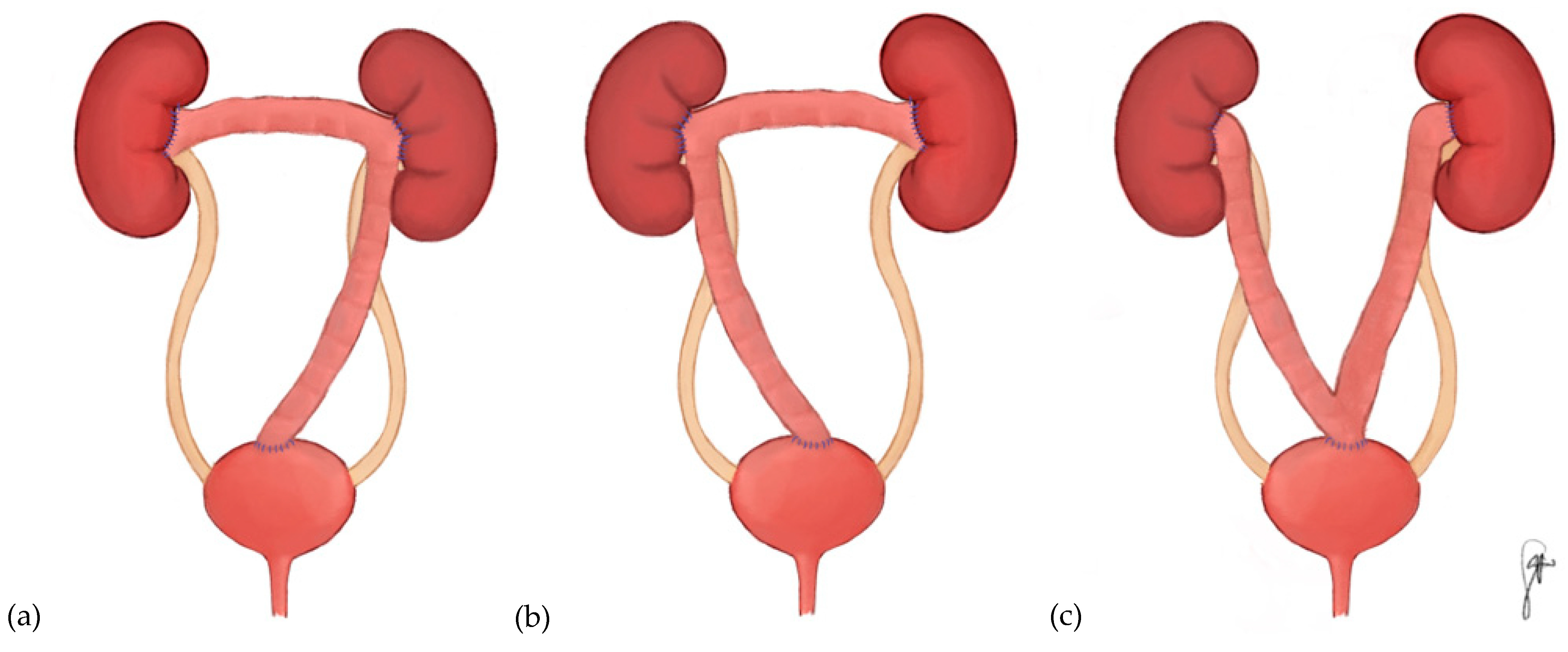
The robotic ileal ureter surgery is a meticulously orchestrated technique involving several critical steps. Initially, the colon is mobilized to access the ureter. The ureter, gonadal vein, and renal hilum are then identified, and the diseased ureteral segment is carefully excised. A 15–20 cm ileal segment is isolated for use in the reconstruction. Adequate spatulation is essential to facilitate the anastomosis on either side of the harvested bowel. Alternatively, a side-to-side anastomosis might be preferable, depending on the case. For bilateral ureteral strictures, a longer segment of ileum can be utilized, allowing for bilateral ureteral anastomoses. A “reverse 7” configuration is most often used to address both ureters with the least amount of harvested bowel [23,24,25] (Figure 2). To perform this surgery, a segment of the ileum is harvested and its proximal end is anastomosed to the left ureter or left renal pelvis, and the middle of the intestinal segment is anastomosed to the right ureter or right renal pelvis. The distal end is then connected to the bladder. A “7” configuration, wherein the right ureter or renal pelvis is anastomosed to the proximal intestinal segment is also possible, albeit less common [24]. Alternatively, each ureter can be replaced with a separate segment of ileum like that described for a unilateral ileal ureteral replacement [24,26]. Other configurations, such as a “U” or “Y” shaped approach have been described [27,28]. When performed intracorporeally, BIUR can be performed with or without re-docking the robot [29]. The ileal segment can also be prepared by an extracorporeal approach if desired [30]. While there is no absolute consensus on intracorporeal vs. extracorporeal bowel preparation, intracorporeal methods are increasingly preferred due to reduced bowel handling and smaller incisions. However, the choice depends on surgeon experience and patient anatomy [31]. An anti-refluxing iliopsoas muscle tunnel can also be used with this technique to reduce reflux into the upper urinary tract [26]. Compared with unilateral ileal ureter, a median of ~6 cm more bowel is harvested to complete BIUR [24].
Figure 2.
Configurations of bilateral ileal ureter replacement. (a) 7 bilateral ileal ureter replacement into a native bladder. (b) Reverse-7 bilateral ileal ureter replacement into a native bladder. (c) U-shaped bilateral ileal ureter replacement into native bladder. The reverse-7 configuration is the most utilized orientation, ideal for long bilateral strictures because it is conducive to the anatomical position of the ileum. The U-configuration used for bilateral disease is less common and can be used when bowel mobility is compromised. The 7 configuration is used less commonly than the reverse-7 but can be useful in select setting depending on ileal mobility.
The anastomoses to the bladder and renal pelvis should be tension-free and well-perfused, with vascularity to the harvested ileum preserved. Intravenous indocyanine green (ICG) is useful to confirm adequate perfusion to the ileum and at the level of the anastomoses. Leak testing can be performed by irrigating the bladder to ensure a water-tight closure [21]. Despite the precision afforded by robotic technology, technical challenges such as maintaining adequate blood supply to the ileal segment and achieving tension-free anastomoses remain critical to the success of the procedure [32].
3.4. Advances
ICG has revolutionized the precision and safety of RIUR. This approach leverages near-infrared light to provide real-time visualization of the ureter and assess vascularity during surgery [17,33]. When ICG is administered intravenously, it enhances the surgeon’s ability to evaluate blood flow and ensure adequate perfusion at critical anastomosis sites on both the ureter and bowel [34]. This approach is particularly beneficial in complex cases, such as BIUR, where maintaining optimal blood supply is essential for successful outcomes [35]. Intraluminal instillation of ICG can aid in identification of the ureter when anatomy is difficult to comprehend and confirms ureteral patency at the resection site.
The transition to entirely intracorporeal techniques for laparoscopic ileal ureter reconstruction began in 2000, marking a major milestone in minimally invasive surgery [3]. This approach, as described by Brandao et al. involves performing the entire procedure, including bowel isolation and anastomosis, robotically [7]. The intracorporeal method reduces the need for external manipulation, minimizing trauma to surrounding tissues and reducing incision size [36]. Combined with innovations like ICG visualization, these techniques ensure a precise and efficient reconstruction, making robotics indispensable in complex urologic surgeries.
4. Horizons
4.1. Bilateral Ileal Ureter
Few studies have reported outcomes for robotic BIUR. Li et al. described creating BIUR for a subject with duplicated ureters and bilateral ureteral injuries with an operative time of 252 min and no recurrence or complications at 6 months [23]. Wang et al. evaluated 4 subjects undergoing a robotic ileal ureter with extracorporeal preparation of the ileal segment resulting in all subjects being symptom free with no reported complications at 12 months [30]. In this study, radiographic evaluation was performed demonstrating good drainage and resolution of hydronephrosis in all subjects [30]. While a majority of published reports describing robotic-assisted BIUR utilized the Da Vinci surgical platform, Fan et al. demonstrated successful performance of this technique using the KangDuo Surgical Robot 2000 [37]. In this study, operative time was 271 min and the surgery was successful [37].
Chen et al. compared RIUR vs. open IUR, with 15 of the 20 subjects having a BIUR. In this study, the robotic approach was associated with statistically significant differences in estimated blood loss, and hospital length of stay [27]. Huang et al.’s analysis of 7 subjects undergoing BIUR, one of whom had a robotic ureteral replacement, demonstrated a 100% success rate. The single robotic patient had an estimated blood loss of 100 mL, stayed in the hospital for 8 days, and had no complications [38]. Wang et al. evaluated 8 individuals requiring robotic or laparoscopic ileal ureteral replacement for ureteral polyps, 3 of whom underwent a reverse-7 procedure for BIUR, all procedures were performed successfully without open conversion with one Clavien Grade IIIb complication and two Clavien Grade I complications [39].
Launer et al.’s study of 46 subjects, 3 of whom underwent robotic ileal ureter and 10 of whom had bilateral repairs, demonstrated an overall success rate of 83% (n = 38) and a complication rate of 24% (n = 11) [40]. However, in both of these studies, neither the robotic cases nor the cases in which bilateral ureters were replaced were analyzed separately; thus, it is difficult to draw conclusions about robotic-assisted BIUR from these manuscripts [39,40].
The robotic platform allows surgeons to realize the benefits of minimally invasive surgery while addressing complex bilateral ureteral pathology. While such cases would historically have been managed in an open fashion, the surgical robot allows for precise, intracorporeal dissection, tension-free anastomosis, and bowel segment preparation. Further, the ability to complete BIUR simultaneously through a single setup eliminates the need for staged procedures and limits recovery time.
This approach is not without its technical hurdles. BIUR requires advanced surgical. Anastomotic tension, ileal blood supply, and prevention of urinary stasis are critical challenges to overcome. Standardization of techniques and long-term outcome data are still lacking which highlights the necessity of further research.
4.2. Ileal Ureter with Augmentation or Diversion
IUR can be performed in combination with bladder augmentation or with urinary diversion [41]. It can also be performed in individuals with a prior bladder augmentation or urinary diversion. While these procedures have traditionally been completed using open techniques, which remain feasible, the robotic approach has emerged as a practical alternative in select patients due to the potential to reduce morbidity. However, this evidence is emerging as few studies have described these techniques robotically to date [36,42].
Several studies have shown the feasibility of performing a RIUR in combination with a bladder augmentation. Chen et al. compared the open and robotic approaches for combined bladder augmentation with IUR. They demonstrated statistically significant improvements in estimated blood loss and hospital length of stay with the robotic approach with no difference in complication rate or other parameters evaluated [27]. Nigro et al.’s case report of an ileal ureter with bladder augmentation demonstrated maintenance of renal function at 12 months without complications, demonstrating the feasibility of a combined robotic augmentation and reverse-7 procedure [43]. Huang et al. evaluated 7 subjects who underwent a combined ileal ureter and bladder augmentation [38]. Among these 7 subjects, only one was performed robotically which demonstrated the feasibility of this technique [38].
While existing literature is lacking a comparative analysis between the open and robotic approach of a combined ileal ureteral replacement with bladder augmentation or diversion, studies evaluating the open approach can provide a point of reference for consideration of emerging robotic data. Kocot et al. examined 157 subjects who underwent ureteral replacement, 78 of whom had a prior open urinary diversion [41]. In this study, 34 of these subjects had their urinary diversion performed simultaneously with their ureteral reconstruction [41]. In 15 of these subjects, undiversion or a change in diversion was performed during the subjects’ ileal replacement surgery [41]. Subjects with combination procedures were not analyzed separately, but the overall success and complication rates reported in this study were 96% (n = 151) and 10.2% (n = 16) respectively [41]. Kim et al. analyzed cases utilizing the open technique for ileal ureteral replacement and showed that 32.2% (n = 10) of subjects underwent a bladder augmentation in combination with an ileal ureter with good success [24]. While subjects undergoing this combination procedure were not evaluated separately, the overall results demonstrate that this surgery is technically feasible [24].
Ileal ureter can also be performed in subjects who have had a previous bladder augmentation or diversion, although to our knowledge, none have specifically described performing this surgery robotically [25,41]. In a study by Soyster et al., these subjects were not analyzed separately but the overall success rate for their subjects was 89.5% [25]. While this study did not use a robotic approach, it demonstrates feasibility of this technique [25]. Studies discussing robotic ileal ureter in the setting of current or prior augmentation or diversion are warranted.
4.3. Infrastructure, Instruction, Innovation
Utilizing a robotic platform offers the benefit of shorter hospital stays and reduced perioperative complications. Brandao et al. demonstrated minimal blood loss and rapid postoperative recovery in patients undergoing robotic ileal ureter interposition [7]. Encouragingly, longer-term follow-up data supports the durability of robotic reconstruction. Ubrig et al. reported sustained renal function and no major complications at three months postoperatively [42]. As robotic platforms continue to evolve and long term data becomes more readily available, the role of robotic-assisted surgery in complex reconstructive cases is expected to expand. Despite the advantages of use, robotic-assisted surgery faces significant barriers to widespread adoption. Access is largely limited to well-funded, urban centers, restricting availability in underserved areas [44].
The high cost of robotic systems remains a major challenge in adoption of use worldwide. Cost remains a critical limitation, with higher installation, maintenance, and hospitalization expenses than laparoscopic or open approaches [44,45]. Ng et al. demonstrated that the cost disparity between robotic-assisted and laparoscopic surgeries has persisted and continues to widen over time, further compounding current barriers to care [46]. In the United States, patients with Medicaid or no insurance have lower odds of receiving robotic surgery compared to those with private insurance, underscoring how the high cost further contributes to disparities in access in care [47]. To combat these challenges future efforts must prioritize cost-reduction strategies, broader institutional investment, and policy reforms aimed at expanding equitable access to robotic surgery across diverse patient care settings.
Robotic-assisted surgical approaches, particularly for complex urological reconstructive cases such as ileal ureter, present a steep learning curve that can hinder initial adoption (especially in resource limited settings as forementioned) [7,30,36]. Effective training programs are essential to equip surgeons with the skills at all stages of careers. Programs must be adapted in order to meet needs of residents, early career, and late career urologists seeking to adopt or further refine their techniques. Simulation-based training has become fundamental to surgical education with curricula such as SIMULATE demonstrating superior outcomes in preclinical settings through structured hands-on practice [48]. Looking ahead, virtual reality simulators and augmented reality models offer promising future directions to enhance preparedness and precision in complex procedures [49,50].
5. Efficacy and Safety
Few studies have compared open, laparoscopic, and robotic approaches to IUR surgery head-to-head. However, several studies have evaluated overall outcomes from IUR including some that we have previously mentioned (Table 1, Table 2 and Table 3). Soyster et al.’s analysis of open ureteral replacement demonstrated that, compared with unilateral, BIUR was not associated with worsening renal function [51] (Table 1). While it is unclear if this is applicable to the robotic approach, a study comparing the long-term renal function outcomes in open vs. robotic ureteral replacement is warranted. Xu et al.’s study of 44 subjects, 20 of whom had BIUR, demonstrated a success rate of 97.7%, although this group did not report the results of their BIUR surgeries separately [26]. A study by Kim et al. of 31 subjects undergoing ileal ureteral replacement, 45.1% (n = 14) of whom had bilateral ureteral strictures, demonstrated success, defined as stable creatinine, in 96.6% of subjects [24]. In this study, the complication rate was fairly high, with 28.6% (n = 4) subjects in the bilateral group experiencing a complication within 30 days and 85.7% (n = 12) of these subjects experiencing a longer-term complication [24].

Table 1.
Open ileal ureter replacement outcomes.

Table 2.
Laparoscopic ileal ureter replacement outcomes.

Table 3.
Robotic ileal ureter replacement outcomes.
Soyster et al. evaluated patients with a history of urinary tract reconstruction undergoing ileal ureteral replacement, including 4 subjects receiving BIUR, demonstrated success in 89.5% (n = 17) subjects with a 31.6% complication rate [25]. Poujade et al. analyzed 21 subjects, which included 4 BIUR, reported two Clavien Grade III or greater complications within 30 days and 14 late complications among their entire cohort [52]. Kochkin et al.’s multi-institutional study of laparoscopic ileal ureters, including 15 of 102 subjects who underwent a BIUR demonstrated high success rates and an 88% rate of clinical success with 10% experiencing complications Clavien grade II or higher [53]. (Table 2) The authors of this study noted that their described technique could be performed robotically and that further studies regarding the robotic approach are warranted [53].
Studies have shown high success rates for RIUR, with most patients regaining urinary function and experiencing symptom relief [19]. However, potential complications (to be discussed later in further detail) include bowel obstruction, urinary leaks, stricture recurrence, and metabolic abnormalities [11,55]. Yang et al. analyzed 15 patients who underwent RIUR and reported that 100% of these patients had successful operations with zero converted to open [36]. The mean length of ileum harvested was 28.3 cm and the mean length of hospitalization was 10.5 days [36]. At a median follow-up of 14 months, 100% of patients achieved subjective success and 86.7% achieved functional success [36] (Table 3). Grosso et al. looked at three patients who underwent RIUR at a single institution [54]. They reported no complications greater than Clavien-Dindo II and antegrade pyelography at one month post-operatively demonstrated full patency of the ileal ureter in all but one patient whose scan revealed a stenotic ileal-ureter anastomosis [54]. Additionally, an abstract examining quality of life (QOL) after ileal ureteral replacement demonstrated that ureteral obstruction worsened QOL and that ileal ureteral replacement significantly improved QOL at 6 and 12 months afterward.
Long-term follow-up is essential for monitoring renal function and ensuring ileal ureter patency. RIUR represents a landmark advancement in urologic surgery. By combining minimally invasive approaches with the precision of robotic surgery, this technique addresses complex ureteral pathologies while minimizing complications and recovery time. Continued innovation and research will further refine its application, making it an indispensable tool in modern urology.
The use of ileum for ureteral replacement exposes patients to a variety of potential complications resulting from the differences in physiological properties of the urinary tract and gastrointestinal tract. Anytime bowel is surgically manipulated and particularly when an anastomosis is performed, there is risk of a leak, perforation, or bowel obstruction. Removal of ileal segments also decreases the absorptive surface area of the digestive tract. Of particular importance is the terminal ileum which is largely responsible for the absorption of vitamin B12, bile salts and the fat soluble vitamins A and D [20]. If the terminal ileum is resected or damaged, excess bile acids and fats can pass into the colon and cause steatorrhea and/or diarrhea [20]. It can also disturb the colonic microbiome resulting in bacterial overgrowth and associated discomfort and diarrhea [20]. For these reasons, the terminal ileum is routinely avoided when harvesting bowel for reconstruction.
Depending on the bowel segment used, a variety of electrolyte and metabolic derangements can develop. Thus, it is important to determine a patient’s baseline renal and metabolic function so that these imbalances can be monitored and compensatory responses tracked postoperatively [20]. For the ileum in particular, the most common metabolic derangements include hypochloremia, hypokalemia, hypocalcemia, and metabolic acidosis [20]. The compensatory chronic metabolic acidosis is buffered by bone minerals which can cause significant skeletal demineralization, more common in children than adults for poorly understood reasons [56]. The risk of compromised renal function is at least theoretically exacerbated by the potential for urine reflux through the ileal ureter into the kidney. For this reason, it is recommended that in addition to lifelong creatinine screening, renal ultrasounds should be serially performed to assess for damage from urinary reflux [20]. However, metabolic abnormalities and renal functional changes as a result of ureteral replacement with bowel are uncommon. Unlike the use of bowel for urinary diversion, the ileal ureter does not serve as a reservoir for urine, reducing the amount of time that the urine is in contact with the bowel, thus resulting in less absorption of electrolytes and other metabolic products front he urine.
Another physiologic consequence of using ileum in the urinary tract is that the harvested bowel continues to perform its natural secretory functions. This introduces the potential for mucus plugging and increases the risk of stone formation in the ileal ureter [57]. However, it has been shown that the secretory capacity of the harvested bowel tends to atrophy over time which is thought to be due to decreased stimulation of the mucosa by fecal material [20]. Therefore, the risk of mucus plugging and stone formation are greatest in the acute postoperative setting and decline over time.
While these findings underscore the overall success of IUR—particularly with robotic approaches—they also highlight the importance of understanding and managing the potential complications associated with this complex reconstructive procedure.
6. Conclusions
RIUR is a versatile approach to treating an otherwise devastated and end-stage ureter. As the entire field of urology has continued its technological evolution, the techniques for performing an ileal ureter have advanced to a less invasive robotic-assisted platform. The improvements in dexterity, precision, and visualization boasted by robotic technology have been demonstrated to improve a variety of outcome measures, including blood loss, recovery time, length of hospitalization, and morbidity. These advantages enable surgeons to challenge the boundaries and perform more complex reconstructive repairs such as BIUR and ileal ureteral replacement in combination with bladder augmentation or urinary diversion. Available data demonstrate encouraging efficacy and safety, but there are still a variety of challenges associated with this approach to ureteral reconstruction including risk to long-term metabolic health, risk of infection, a steep surgical learning curve, and disparities in access to robotic surgical systems. Future work should focus efforts on considerations for patient selection, further refinement of surgical techniques, and continued expansion of the use of ileal ureteral replacement. Robotic surgery has and will continue to revolutionize the field of reconstructive urology giving surgeons more tools than ever to help care for patients.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ou, Y.C.; Hu, C.Y.; Cheng, H.L.; Yang, W.H. Long-term outcomes of total ureterectomy with ileal-ureteral substitution treatment for ureteral cancer: A single-center experience. BMC Urol. 2018, 18, 73. [Google Scholar] [CrossRef] [PubMed]
- Monn, M.F.; Roth, J.D.; Bihrle, R.; Mellon, M.J. Long term outcomes in the use of ileal ureter for radiation-induced ureteral strictures. Int. Urol. Nephrol. 2018, 50, 1375–1380. [Google Scholar] [CrossRef] [PubMed]
- Gill, I.S.; Savage, S.J.; Senagore, A.J.; Sung, G.T. Laparoscopic ileal ureter. J. Urol. 2000, 163, 1199–1202. [Google Scholar] [CrossRef] [PubMed]
- Stein, R.J.; Turna, B.; Patel, N.S.; Weight, C.J.; Nguyen, M.M.; Shah, G.; Aron, M.; Fergany, A.F.; Gill, I.S.; Desai, M.M. Laparoscopic assisted ileal ureter: Technique, outcomes and comparison to the open procedure. J. Urol. 2009, 182, 1032–1039. [Google Scholar] [CrossRef]
- Fan, S.; Han, G.; Li, Z.; Wang, X.; Li, X.; Xiong, S.; Li, D.; Zhang, J.; Meng, C.; Zhang, P.; et al. Robot-assisted laparoscopic ileal ureter replacement with extracorporeal ileal segment preparation for long ureteral strictures: A case series. BMC Surg. 2022, 22, 435. [Google Scholar] [CrossRef]
- Wagner, J.R.; Schimpf, M.O.; Cohen, J.L. Robot-assisted laparoscopic ileal ureter. JSLS 2008, 12, 306–309. [Google Scholar] [PubMed]
- Brandao, L.F.; Autorino, R.; Zargar, H.; Laydner, H.; Krishnan, J.; Samarasekera, D.; Haber, G.P.; Kaouk, J.H.; Chalikonda, S.; Stein, R.J. Robotic ileal ureter: A completely intracorporeal technique. Urology 2014, 83, 951–954. [Google Scholar] [CrossRef]
- Zhu, W.; Xiong, S.; Fang, D.; Hao, H.; Zhang, L.; Xiong, G.; Yang, K.; Zhang, P.; Zhu, H.; Cai, L.; et al. Minimally invasive ileal ureter replacement: Comparative analysis of robot-assisted laparoscopic versus conventional laparoscopic surgery. Int. J. Med. Robot. 2021, 17, e2230. [Google Scholar] [CrossRef]
- Wang, L.; Hussein, A.; Guru, K.; Li, Q. Robotic Ileal Ureter with Bladder Augmentation in a Modified Studer Fashion for a Long Ureteral Stricture and Small Bladder. Urol. Video J. 2022, 16, 100182. [Google Scholar] [CrossRef]
- Tanna, R.J.; Powell, J.; Mambu, L.A. Ileal Conduit. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2024. [Google Scholar]
- Armatys, S.A.; Mellon, M.J.; Beck, S.D.; Koch, M.O.; Foster, R.S.; Bihrle, R. Use of ileum as ureteral replacement in urological reconstruction. J. Urol. 2009, 181, 177–181. [Google Scholar] [CrossRef]
- Goodwin, W.E.; Winter, C.C.; Turner, R.D. Replacement of the ureter by small intestine: Clinical application and results of the ileal ureter. J. Urol. 1959, 81, 406–418. [Google Scholar] [CrossRef] [PubMed]
- Leal Ghezzi, T.; Campos Corleta, O. 30 Years of Robotic Surgery. World J. Surg. 2016, 40, 2550–2557. [Google Scholar] [CrossRef]
- Nagy, A.G.; Poulin, E.C.; Girotti, M.J.; Litwin, D.E.; Mamazza, J. History of laparoscopic surgery. Can. J. Surg. 1992, 35, 271–274. [Google Scholar]
- Catanzarite, T.; Tan-Kim, J.; Whitcomb, E.L.; Menefee, S. Ergonomics in Surgery: A Review. Female Pelvic Med. Reconstr. Surg. 2018, 24, 1–12. [Google Scholar] [CrossRef]
- Burks, F.N.; Santucci, R.A. Management of iatrogenic ureteral injury. Ther. Adv. Urol. 2014, 6, 115–124. [Google Scholar] [CrossRef]
- Fuller, T.W.; Daily, A.M.; Buckley, J.C. Robotic Ureteral Reconstruction. Urol. Clin. N. Am. 2022, 49, 495–505. [Google Scholar] [CrossRef]
- Komninos, C.; Koo, K.C.; Rha, K.H. Laparoendoscopic management of midureteral strictures. Korean J. Urol. 2014, 55, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Mattos, R.M.; Smith, J.J., 3rd. Ileal ureter. Urol. Clin. N. Am. 1997, 24, 813–825. [Google Scholar] [CrossRef] [PubMed]
- Vasdev, N.; Moon, A.; Thorpe, A.C. Metabolic complications of urinary intestinal diversion. Indian. J. Urol. 2013, 29, 310–315. [Google Scholar] [CrossRef]
- Drain, A.; Jun, M.S.; Zhao, L.C. Robotic Ureteral Reconstruction. Urol. Clin. N. Am. 2021, 48, 91–101. [Google Scholar] [CrossRef]
- Hashad, M.M.; Atta, M.; Elabbady, A.; Elfiky, S.; Khattab, A.; Kotb, A. Safety of no bowel preparation before ileal urinary diversion. BJU Int. 2012, 110 Pt C, E1109–E1113. [Google Scholar] [CrossRef]
- Li, X.; Wang, X.; Chen, S.; Li, Z.; Yang, K.; Li, X. Robot-assisted Laparoscopic Bilateral Ileal Ureter in Duplex Ureter with Strictures After Treatment Failure of Allium Stents. Urology 2022, 169, 267–268. [Google Scholar] [CrossRef]
- Kim, A.; Nam, W.; Song, S.H.; Jeong, I.G.; Hong, B. Use of the Ileum for Ureteral Stricture and Obstruction in Bilateral, Unilateral, and Single-kidney Cases. Urology 2018, 111, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Soyster, M.E.; Arnold, P.J.; Burns, R.T.; Zappia, J.L.; Roth, J.D.; Francesca Monn, M.; Bihrle, R.; Mellon, M.J. Ileal Ureter Utilization in Patients with Previous Urinary Diversions. Urology 2023, 177, 184–188. [Google Scholar] [CrossRef]
- Xu, Y.M.; Feng, C.; Kato, H.; Xie, H.; Zhang, X.R. Long-term Outcome of Ileal Ureteric Replacement with an Iliopsoas Muscle Tunnel Antirefluxing Technique for the Treatment of Long-segment Ureteric Strictures. Urology 2016, 88, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Wang, X.; Li, Z.; Li, X.; Han, G.; Tao, Z.; Li, Z.; Zhang, P.; Zhu, H.; Yang, K.; et al. Minimally invasive versus open ileal ureter with ileocystoplasty: Comparative outcomes and 5-year experience. BMC Urol. 2024, 24, 118. [Google Scholar] [CrossRef] [PubMed]
- Ramalingam, M.; Senthil, K.; Murugesan, A.; Pai, M.G. Laparoscopy assisted ‘U’ configuration bilateral ileal ureter in pelvic lipomatosis with bilateral ureteric obstruction. Urol. J. 2013, 10, 1007–1010. [Google Scholar]
- Wu, G.; Li, H.; Luo, F.; Zheng, H.; Yuegao, Y.; Xie, L.; Luo, H.; Chen, Z.; Ye, D.; Lai, C. Total intracorporeal laparoscopic ileal ureter replacement in a single position for ureteral stricture based on membrane anatomy. BMC Surg. 2024, 24, 88. [Google Scholar] [CrossRef]
- Wang, X.; Chen, S.; Li, X.; Fan, S.; Han, G.; Li, Z.; Yang, K.; Zhang, K.; Zhou, L.; Li, X. Robotic-assisted Laparoscopic Bilateral Ileal Ureter Replacement with Extracorporeal Ileal Segment Preparation for Bilateral Extensive Ureteral Strictures: The Initial Experience. Urology 2023, 176, 213–218. [Google Scholar] [CrossRef]
- Maurya, K.S.O.; Yadav, P.; Gupta, A. Robotic Ileal Ureter: Technique and outcomes. Indian. J. Urol. 2020, 36, 184–189. [Google Scholar]
- Shrivastava, N.; Bhargava, P.; Jain, P.; Choudhary, G.R.; Jena, R.; Singh, M.; Navriya, S.; Madduri, V.K.S.; Bhirud, D.P.; Sandhu, A.S. Robot-assisted ureteric reconstructive surgeries for benign diseases: Initial single-center experience with point of technique. Urol. J. 2024, 91, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Farnam, R.W.; Arms, R.G.; Klaassen, A.H.; Sorger, J.M. Intraoperative ureter visualization using a near-infrared imaging agent. J. Biomed. Opt. 2019, 24, 066004. [Google Scholar] [CrossRef] [PubMed]
- Lee, Z.; Moore, B.; Giusto, L.; Eun, D.D. Use of indocyanine green during robot-assisted ureteral reconstructions. Eur. Urol. 2015, 67, 291–298. [Google Scholar] [CrossRef]
- Asghar, A.M.; Lee, R.A.; Yang, K.K.; Metro, M.; Eun, D.D. Robot-assisted distal ureteral reconstruction for benign pathology: Current state. Investig. Clin. Urol. 2020, 61 (Suppl. S1), S23–S32. [Google Scholar] [CrossRef]
- Yang, K.; Wang, X.; Xu, C.; Li, Z.; Han, G.; Fan, S.; Chen, S.; Li, X.; Zhu, H.; Zhou, L.; et al. Totally Intracorporeal Robot-assisted Unilateral or Bilateral Ileal Ureter Replacement for the Treatment of Ureteral Strictures: Technique and Outcomes from a Single Center. Eur. Urol. 2023, 84, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Fan, S.; Chen, S.; Li, X.; Li, Z.; Yang, K.; Hao, H.; Zhou, L.; Li, X. Totally Intracorporeal Robot-Assisted Bilateral Ileal Ureter Replacement for the Treat-ment of Ureteral Strictures using Kangduo Surgical Robot 2000 Plus. Int. Braz. J. Urol. 2024, 50, 781–782. [Google Scholar] [CrossRef]
- Huang, C.; Yang, K.; Gao, W.; Gu, Y.; Zhu, H.J.; Li, X. Ileal ureter replacement and ileocystoplasty for the treatment of bilateral ureteral strictures and bladder contracture: Technique and outcomes. Minerva Urol. Nephrol. 2024, 76, 97–109. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, Y.; Zhang, J.; Li, Z.; Han, G.; Zhang, L.; Li, X.; Yang, K.; Wang, B.; Zhang, P.; et al. Minimal-invasive ileal ureter replacement for the management of multiple ureteral polyps: The initial experience. Int. Urol. Nephrol. 2024, 56, 1919–1926. [Google Scholar] [CrossRef]
- Launer, B.M.; Redger, K.D.; Koslov, D.S.; Sax-Bolder, A.N.; Higuchi, T.T.; Windsperger, A.P.; Flynn, B.J. Long-term Follow Up of Ileal Ureteral Replacement for Complex Ureteral Strictures: Single Institution Study. Urology 2021, 157, 257–262. [Google Scholar] [CrossRef]
- Kocot, A.; Kalogirou, C.; Vergho, D.; Riedmiller, H. Long-term results of ileal ureteric replacement: A 25-year single-centre experience. BJU Int. 2017, 120, 273–279. [Google Scholar] [CrossRef]
- Ubrig, B.; Janusonis, J.; Paulics, L.; Boy, A.; Heiland, M.; Roosen, A. Functional Outcome of Completely Intracorporeal Robotic Ileal Ureteric Replacement. Urology 2018, 114, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Nigro, N.; Bhalla, R.; Flynn, B. Robot-Assisted Laparoscopic Reverse 7 Ileal Ureter and Bladder Augmentation: A Complex Urological Case. JU Open Plus 2024, 2, e00079. [Google Scholar] [CrossRef]
- South, C.; Megafu, O.; Moore, C.; Williams, T.; Hobson, L.; Danner, O.; Johnson, S. Robotic Surgery in Safety-Net Hospitals: Addressing Health Disparities and Improving Access to Care. Am. Surg. 2025, 91, 639–643. [Google Scholar] [CrossRef] [PubMed]
- Lawrie, L.; Gillies, K.; Duncan, E.; Davies, L.; Beard, D.; Campbell, M.K. Barriers and enablers to the effective implementation of robotic assisted surgery. PLoS ONE 2022, 17, e0273696. [Google Scholar] [CrossRef] [PubMed]
- Ng, A.P.; Sanaiha, Y.; Bakhtiyar, S.S.; Ebrahimian, S.; Branche, C.; Benharash, P. National analysis of cost disparities in robotic-assisted versus laparoscopic abdominal operations. Surgery 2023, 173, 1340–1345. [Google Scholar] [CrossRef]
- Childers, C.P.; Uppal, A.; Tillman, M.; Chang, G.J.; Tran Cao, H.S. Insurance Disparities in Access to Robotic Surgery for Colorectal Cancer. Ann. Surg. Oncol. 2023, 30, 3560–3568. [Google Scholar] [CrossRef]
- Basile, G.; Gallioli, A.; Diana, P.; Gallagher, A.; Larcher, A.; Graefen, M.; Harke, N.; Traxer, O.; Tilki, D.; Van Der Poel, H.; et al. Current Standards for Training in Robot-assisted Surgery and Endourology: A Systematic Review. Eur. Urol. 2024, 86, 130–145. [Google Scholar] [CrossRef]
- Pears, M.; Rochester, M.; Wadhwa, K.; Payne, S.R.; Konstantinidis, S.; Hanchanale, V.; Elmamoun, M.H.; Biyani, C.S.; Doherty, R. A Pilot Study Evaluating a Virtual Reality-Based Nontechnical Skills Training Application for Urology Trainees: Usability, Acceptability, and Impact. J. Surg. Educ. 2023, 80, 1836–1842. [Google Scholar] [CrossRef]
- Proietti, F.; Flammia, R.S.; Licari, L.C.; Bologna, E.; Anceschi, U.; Ferriero, M.C.; Tuderti, G.; Mastroianni, R.; Brassetti, A.; Simone, G.; et al. Simulation and Training in Robot-Assisted Urological Surgery: From Model to Patient. J. Clin. Med. 2024, 13, 1590. [Google Scholar] [CrossRef]
- Soyster, M.E.; Burns, R.T.; Slaven, J.E.; Zappia, J.L.; Arnold, P.J.; Roth, J.D.; Bihrle, R.; Francesca Monn, M.; Mellon, M.J. Long-term Renal Preservation and Complication Profile with Ileal Ureter Creation. Urology 2024, 188, 138–143. [Google Scholar] [CrossRef]
- Poujade, L.; Branchereau, J.; Rigaud, J.; Perrouin-Verbe, M.A. Ileal ureter replacement: Early morbidity and long-term results. Prog. Urol. 2021, 31, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Kochkin, A.; Kalfountzos, C.; Gallyamov, E.; Biktimirov, R.; Sanzharov, A.; Sergeev, V.; Popov, S.; Dal Moro, F.; Tokas, T.; Gözen, A.S. Laparoscopic intracorporeal ileal ureter replacement: Multi-institutional data from 102 patients. Minim. Invasive Ther. Allied Technol. 2024, 33, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Grosso, A.A.; Di Maida, F.; Mari, A.; Campi, R.; Crisci, A.; Vignolini, G.; Masieri, L.; Carini, M.; Minervini, A. Totally intracorporeal robotic ileal ureter replacement: Focus on surgical technique and outcomes. Minerva Urol. Nephrol. 2021, 73, 532–539. [Google Scholar] [CrossRef]
- Liedberg, F.; Bobjer, J. Urinary diversions for benign and oncologic indications: What did we learn about short term complications in the last 24 months? Curr. Opin. Urol. 2021, 31, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Kawakita, M.; Arai, Y.; Shigeno, C.; Terai, A.; Okada, Y.; Takeuchi, H.; Konishi, J.; Yoshida, O. Bone demineralization following urinary intestinal diversion assessed by urinary pyridinium cross-links and dual energy X-ray absorptiometry. J. Urol. 1996, 156, 355–359. [Google Scholar] [CrossRef]
- Hautmann, R.E.; Miller, K.; Steiner, U.; Wenderoth, U. The ileal neobladder: 6 years of experience with more than 200 patients. J. Urol. 1993, 150, 40–45. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).