Patient-Reported Urinary Symptom Progression After Bacillus Calmette–Guerin Therapy for Bladder Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants and Data Collection
2.2. Statistical Analysis
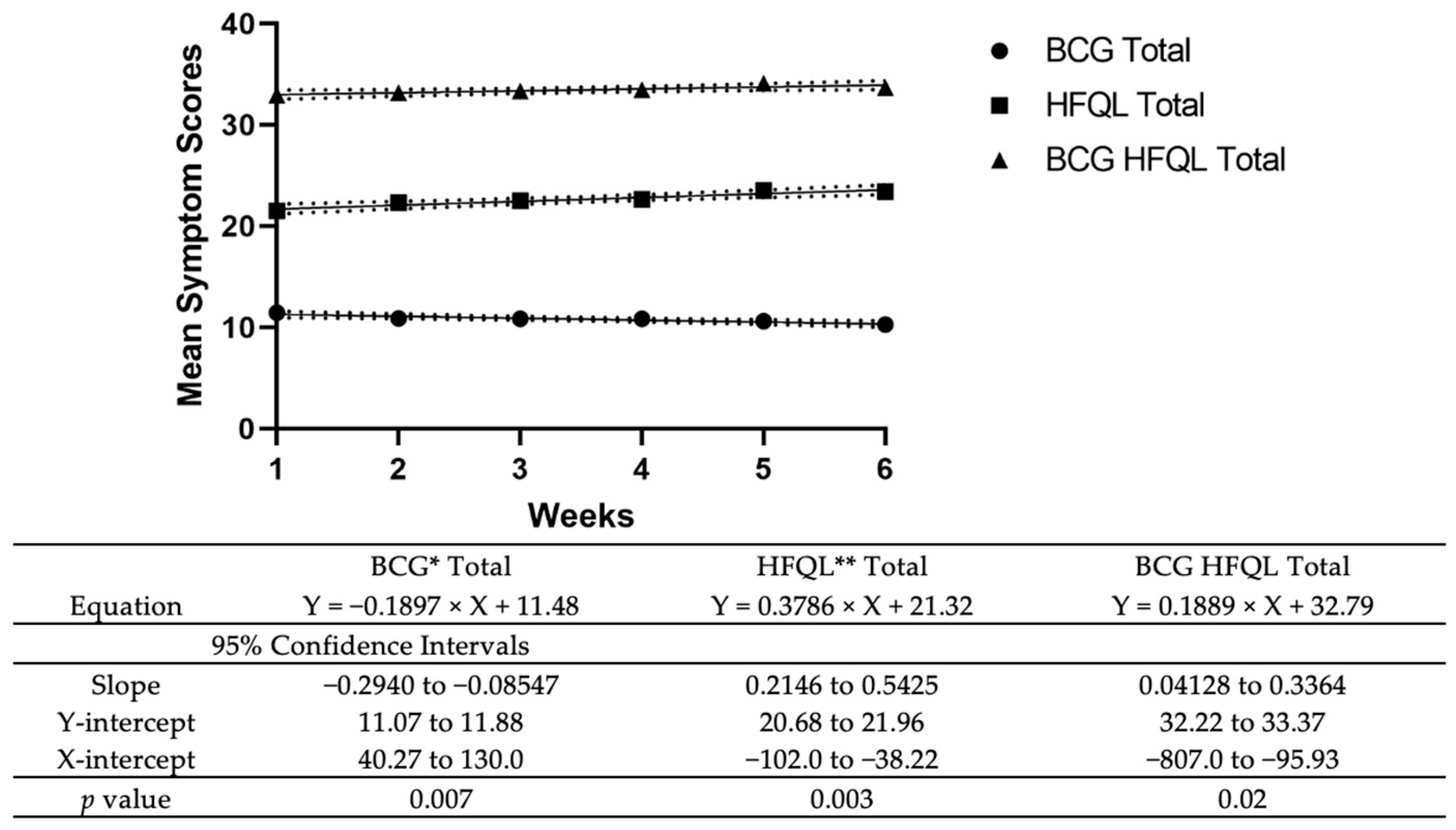
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shen, P.-L.; Lin, M.-E.; Hong, Y.-K.; He, X.-J. Bladder preservation approach versus radical cystectomy for high-grade non-muscle-invasive bladder cancer: A meta-analysis of cohort studies. World J. Surg. Oncol. 2018, 16, 197. [Google Scholar] [CrossRef]
- Han, R.F.; Pan, J.G. Can intravesical bacillus Calmette-Guérin reduce recurrence in patients with superficial bladder cancer? A meta-analysis of randomized trials. Urology 2006, 67, 1216–1223. [Google Scholar] [CrossRef]
- Shelley, M.D.; Mason, M.D.; Kynaston, H. Intravesical therapy for superficial bladder cancer: A systematic review of randomised trials and meta-analyses. Cancer Treat. Rev. 2010, 36, 195–205. [Google Scholar] [CrossRef]
- Asín, M.A.P.-J.; Fernández-Ruiz, M.; López-Medrano, F.; Lumbreras, C.; Tejido, Á.; San Juan, R.; Arrebola-Pajares, A.; Lizasoain, M.; Prieto, S.; Aguado, J.M.; et al. Bacillus Calmette-Guérin (BCG) infection following intravesical BCG administration as adjunctive therapy for bladder cancer: Incidence, risk factors, and outcome in a single-institution series and review of the literature. Medicine 2014, 93, 236–254. [Google Scholar] [CrossRef]
- Lamm, D.L.; Blumenstein, B.A.; Crissman, J.D.; Montie, J.E.; Gottesman, J.E.; Lowe, B.A.; Sarosdy, M.F.; Bohl, R.D.; Grossman, H.B.; Beck, T.M.; et al. Maintenance bacillus Calmette-Guerin immunotherapy for recurrent TA, T1 and carcinoma in situ transitional cell carcinoma of the bladder: A randomized Southwest Oncology Group Study. J. Urol. 2000, 163, 1124–1129. [Google Scholar] [CrossRef]
- Oddens, J.R.; Sylvester, R.J.; Brausi, M.A.; Kirkels, W.J.; van de Beek, C.; van Andel, G.; de Reijke, T.M.; Prescott, S.; Alfred, W.J.; Oosterlinck, W. Increasing age is not associated with toxicity leading to discontinuation of treatment in patients with urothelial non-muscle-invasive bladder cancer randomised to receive 3 years of maintenance bacille Calmette-Guérin: Results from European Organisation. BJU Int. 2016, 118, 423–428. [Google Scholar] [CrossRef]
- Oddens, J.; Brausi, M.; Sylvester, R.; Bono, A.; van de Beek, C.; van Andel, G.; Gontero, P.; Hoeltl, W.; Turkeri, L.; Marreaud, S.; et al. Final results of an EORTC-GU cancers group randomized study of maintenance bacillus Calmette-Guérin in intermediate- and high-risk Ta, T1 papillary carcinoma of the urinary bladder: One-third dose versus full dose and 1 year versus 3 years of maintenance. Eur. Urol. 2013, 63, 462–472. [Google Scholar] [CrossRef]
- Witjes, J.A.; Palou, J.; Soloway, M.; Lamm, D.; Kamat, A.M.; Brausi, M.; Persad, R.; Buckley, R.; Colombel, M.; Böhle, A. Current clinical practice gaps in the treatment of intermediate- and high-risk non-muscle-invasive bladder cancer (NMIBC) with emphasis on the use of bacillus Calmette-Guérin (BCG): Results of an international individual patient data survey (IPDS). BJU Int. 2013, 112, 742–750. [Google Scholar] [CrossRef]
- Brausi, M.; Oddens, J.; Sylvester, R.; Bono, A.; van de Beek, C.; van Andel, G.; Gontero, P.; Turkeri, L.; Marreaud, S.; Collette, S.; et al. Side effects of Bacillus Calmette-Guérin (BCG) in the treatment of intermediate- and high-risk Ta, T1 papillary carcinoma of the bladder: Results of the EORTC genito-urinary cancers group randomised phase 3 study comparing one-third dose with full dose a. Eur. Urol. 2014, 65, 69–76. [Google Scholar] [CrossRef]
- Liu, Y.; Lu, J.; Huang, Y.; Ma, L. Clinical Spectrum of Complications Induced by Intravesical Immunotherapy of Bacillus Calmette-Guérin for Bladder Cancer. J. Oncol. 2019, 2019, 6230409. [Google Scholar] [CrossRef]
- Gontero, P.; Oderda, M.; Mehnert, A.; Gurioli, A.; Marson, F.; Lucca, I.; Rink, M.; Schmid, M.; Kluth, L.A.; Pappagallo, G.; et al. The impact of intravesical gemcitabine and 1/3 dose Bacillus Calmette-Guérin instillation therapy on the quality of life in patients with nonmuscle invasive bladder cancer: Results of a prospective, randomized, phase II trial. J. Urol. 2013, 190, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Yokomizo, A.; Kanimoto, Y.; Okamura, T.; Ozono, S.; Koga, H.; Iwamura, M.; Tanaka, H.; Takahashi, S.; Tsushima, T.; Kanayama, H.; et al. Randomized Controlled Study of the Efficacy, Safety and Quality of Life with Low Dose bacillus Calmette-Guérin Instillation Therapy for Nonmuscle Invasive Bladder Cancer. J. Urol. 2016, 195, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Coyne, K.S.; Thompson, C.L.; Lai, J.S.; Sexton, C.C. An overactive bladder symptom and health-related quality of life short-form: Validation of the OAB-q SF. Neurourol. Urodyn. 2015, 34, 255–263. [Google Scholar] [CrossRef]
- Sylvester, R.J.; Brausi, M.A.; Kirkels, W.J.; Hoeltl, W.; Da Silva, F.C.; Powell, P.H.; Prescott, S.; Kirkali, Z.; van de Beek, C.; Gorlia, T.; et al. Long-term efficacy results of EORTC genito-urinary group randomized phase 3 study 30911 comparing intravesical instillations of epirubicin, bacillus Calmette-Guérin, and bacillus Calmette-Guérin plus isoniazid in patients with intermediate- and high-risk. Eur. Urol. 2010, 57, 766–773. [Google Scholar] [CrossRef] [PubMed]
- Macleod, L.C.; Ngo, T.C.; Gonzalgo, M.L. Complications of intravesical bacillus calmette-guérin. Can. Urol. Assoc. J. 2014, 8, E540–E544. [Google Scholar] [CrossRef]
- Jung, A.; Nielsen, M.E.; Crandell, J.L.; Palmer, M.H.; Smith, S.K.; Bryant, A.L.; Mayer, D.K. Health-related quality of life among non-muscle-invasive bladder cancer survivors: A population-based study. BJU Int. 2020, 125, 38–48. [Google Scholar] [CrossRef]
- Feuerstein, M.A.; Jacobs, M.; Piciocchi, A.; Bochner, B.; Pusic, A.; Fayers, P.; Blazeby, J.; Efficace, F. Quality of life and symptom assessment in randomized clinical trials of bladder cancer: A systematic review. Urol. Oncol. 2015, 33, 331.e17–331.e23. [Google Scholar] [CrossRef]
- van Straten, C.G.J.I.; Caris, C.; Grimm, M.O.; Colombel, M.; Muilwijk, T.; Martínez-Piñeiro, L.; Babjuk, M.M.; Türkeri, L.N.; Palou, J.; Patel, A.; et al. Quality of Life in Patients with High-grade Non-muscle-invasive Bladder Cancer Undergoing Standard Versus Reduced Frequency of Bacillus Calmette-Guérin Instillations: The EAU-RF NIMBUS Trial. Eur. Urol. Open Sci. 2023, 56, 15–24. [Google Scholar] [CrossRef]
- Koya, M.P.; Simon, M.A.; Soloway, M.S. Complications of intravesical therapy for urothelial cancer of the bladder. J. Urol. 2006, 175, 2004–2010. [Google Scholar] [CrossRef]
- Johnson, M.H.; Nepple, K.G.; Peck, V.; Trinkaus, K.; Klim, A.; Sandhu, G.S.; Kibel, A.S. Randomized controlled trial of oxybutynin extended release versus placebo for urinary symptoms during intravesical Bacillus Calmette-Guérin treatment. J. Urol. 2013, 189, 1268–1274. [Google Scholar] [CrossRef]
- Ferro, M.; Tataru, O.S.; Fallara, G.; Fiori, C.; Manfredi, M.; Claps, F.; Hurle, R.; Buffi, N.M.; Lughezzani, G.; Lazzeri, M.; et al. Assessing the influence of smoking on inflammatory markers in bacillus Calmette Guérin response among bladder cancer patients: A novel machine-learning approach. Minerva Urol. Nephrol. 2024. [Google Scholar] [CrossRef] [PubMed]
- Sun, K.; Wang, D.; Wu, G.; Ma, J.; Wang, T.; Wu, J.; Wang, J. Mirabegron improves the irritative symptoms caused by BCG immunotherapy after transurethral resection of bladder tumors. Cancer Med. 2021, 10, 7534–7541. [Google Scholar] [CrossRef]
- Hannan, T.J.; Mysorekar, I.U.; Hung, C.S.; Isaacson-Schmid, M.L.; Hultgren, S.J. Early severe inflammatory responses to uropathogenic E. coli predispose to chronic and recurrent urinary tract infection. PLoS Pathog. 2010, 6, e1001042. [Google Scholar] [CrossRef]
- Grundy, L.; Caldwell, A.; Brierley, S.M. Mechanisms Underlying Overactive Bladder and Interstitial Cystitis/Painful Bladder Syndrome. Front. Neurosci. 2018, 12, 931. [Google Scholar] [CrossRef] [PubMed]
- Furuta, A.; Yamamoto, T.; Suzuki, Y.; Gotoh, M.; Egawa, S.; Yoshimura, N. Comparison of inflammatory urine markers in patients with interstitial cystitis and overactive bladder. Int. Urogynecol. J. 2018, 29, 961–966. [Google Scholar] [CrossRef]
- Zincke, H.; Utz, D.C.; Farrow, G.M. Review of Mayo Clinic experience with carcinoma in situ. Urology 1985, 26, 39–46. [Google Scholar]
| Characteristics | N (%) |
|---|---|
| Age at Diagnosis, Median (IQR) | 73 (17) |
| Sex | |
| Male | 40 (66.7) |
| Female | 20 (33.3) |
| Smoking Status | |
| Yes | 38 (63.3) |
| No | 21 (35.0) |
| Clinical Stage | |
| Ta | 25 (41.7) |
| T1 | 30 (50.0) |
| Tis | 5 (8.3) |
| Tumor Grade | |
| LG | 7 (11.7) |
| HG | 53 (88.3) |
| Tumor Focality | |
| Focal Tumor | 41 (68.3) |
| Multifocal | 19 (31.7) |
| Tumor Volume in cm3, Median (IQR) | |
| Overall | 2.7 (0.3–4.5) |
| Focal Tumor | 3.0 (0.5–4.5) |
| Multifocal Tumor | 0.5 (0.02–3.9) |
| Days From Primary TURBT and BCG Induction, Mean (Std. Dev) | 67.9 (50.1) |
| Number of Previous TURBTs, Mean (Std. Dev) | 2.1 (0.4) |
| Race | |
| Caucasian | 50 (83.3) |
| Other | 10 (16.7) |
| Preoperative Urinary Symptoms | 24 (40.0) |
| Preoperative Gross Hematuria | 44 (73.3) |
| Prior Medication Use | |
| OAB Medications | 1 (1.7) |
| BPH Medications | 16 (26.7) |
| OAB and BPH Medications | 1 (1.7) |
| Not reported | 42 (70.0) |
| History of rUTIs | 2 (3.3) |
| Mean Difference in Urinary Symptoms | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Week 2 * | Week 3 * | Week 4 * | Week 5 * | Week 6 * | ||||||
| p-Value | p-Value | p-Value | p-Value | p-Value | ||||||
| Total | −2.07 | 0.24 | −1.86 | 0.36 | −1.00 | 0.61 | −1.67 | 0.50 | 1.11 | 0.72 |
| Symptom Bother | −1.17 | 0.04 | −0.74 | 0.32 | −0.76 | 0.35 | −1.11 | 0.23 | 0.75 | 0.69 |
| Question 1 | −0.33 | 0.002 | 0.00 | 1.00 | −0.16 | 0.28 | −0.11 | 0.57 | −0.11 | 0.49 |
| Question 2 | −0.17 | 0.28 | 0.05 | 0.73 | −0.16 | 0.32 | 0.03 | 0.68 | 0.30 | 0.86 |
| Question 3 | −0.19 | 0.09 | −0.15 | 0.16 | −0.08 | 0.57 | −0.08 | 0.68 | 0.00 | 1.00 |
| Question 4 | 0.02 | 0.89 | −0.15 | 0.41 | −0.08 | 0.67 | −0.26 | 0.14 | 1.37 | 0.36 |
| Question 5 | −0.26 | 0.10 | −0.26 | 0.13 | −0.16 | 0.56 | −0.47 | 0.07 | −0.31 | 0.19 |
| Question 6 | −0.29 | 0.06 | −0.24 | 0.13 | −0.14 | 0.34 | −0.27 | 0.12 | −0.21 | 0.29 |
| HFQL ** | −0.72 | 0.53 | −1.00 | 0.47 | 0.29 | 0.83 | 0.13 | 0.93 | 1.29 | 0.48 |
| Question 1 | −0.22 | 0.15 | −0.09 | 0.56 | 0.00 | 1.00 | −0.06 | 0.75 | 0.00 | 1.00 |
| Question 2 | −0.41 | 0.02 | −0.06 | 0.54 | −0.13 | 0.25 | −0.16 | 0.28 | 0.14 | 0.40 |
| Question 3 | 0.09 | 0.65 | −0.09 | 0.65 | 0.25 | 0.21 | 0.25 | 0.22 | 0.33 | 0.16 |
| Question 4 | −0.03 | 0.81 | 0.06 | 0.76 | −0.06 | 0.74 | 0.00 | 1.00 | 0.03 | 0.87 |
| Question 5 | −0.16 | 0.20 | −0.03 | 0.84 | −0.09 | 0.54 | 0.00 | 1.00 | 0.17 | 0.33 |
| Question 6 | −0.09 | 0.65 | −0.59 | 0.02 | 0.00 | 1.00 | −0.19 | 0.48 | −0.20 | 0.30 |
| Question 7 | −0.22 | 0.23 | −0.03 | 0.89 | −0.16 | 0.43 | −0.06 | 0.73 | 0.20 | 0.30 |
| Question 8 | −0.16 | 0.28 | 0.10 | 0.66 | −0.09 | 0.50 | −0.06 | 0.71 | −0.03 | 0.84 |
| Question 9 | 0.03 | 0.83 | 0.00 | 1.00 | 0.03 | 0.79 | 0.10 | 0.50 | 0.28 | 0.13 |
| Question 10 | −0.10 | 0.18 | 0.10 | 0.57 | −0.06 | 0.33 | 0.00 | 1.00 | 0.00 | 1.00 |
| Question 11 | −0.22 | 0.26 | −0.31 | 0.05 | 0.16 | 0.43 | −0.06 | 0.75 | 0.13 | 0.49 |
| Question 12 | 0.22 | 0.05 | −0.06 | 0.54 | 0.03 | 0.81 | 0.16 | 0.32 | 0.17 | 0.20 |
| Question 13 | −0.29 | 0.18 | −0.52 | 0.02 | −0.19 | 0.36 | −0.23 | 0.32 | −0.10 | 0.69 |
| Subgroup Analysis | Difference in Urinary Symptoms (Week 6-Week 1) | Difference in Δ | p-Value |
|---|---|---|---|
| By Prior Medication Use | |||
| Prior Medication Use | 0.43 | 0.92 | 0.86 |
| No Prior Medication Use | 1.35 | ||
| Type of Medication Use | |||
| BPH Meds | −1.67 | 0 | 0.69 |
| OAB Meds | 13 | −14.67 | |
| BPH + OAB Meds | 0 | −1.67 | |
| By Preoperative Urinary Symptoms | |||
| Preoperative Urinary Symptoms | −0.75 | 2.64 | 0.62 |
| No Preoperative Urinary Symptoms | 1.89 | ||
| By History of rUTIs * | |||
| History of rUTIs | 3 | −2.04 | 0.79 |
| No History of rUTIs | 0.96 | ||
| By Maintenance Therapy | |||
| Maintenance Therapy | 4 | −5.33 | 0.45 |
| No Maintenance Therapy | −1.33 | ||
| By Smoking Status | |||
| Yes | 2.13 | −3.53 | 0.55 |
| No | −1.4 | ||
| By Gender | |||
| Male | 0.1 | 3.39 | 0.64 |
| Female | 3.5 | ||
| By Race | |||
| White | 0.06 | −0.06 | 0.95 |
| Other | 0 | ||
| By Preoperative Gross Hematuria | |||
| Gross Hematuria | −0.59 | 4.58 | 0.48 |
| No Gross Hematuria | 4 | ||
| By Age | |||
| <60 | 1.83 | 0.93 | 0.84 |
| ≥60 | 0.9 | ||
| By Grade | |||
| HG | −0.68 | 24.18 | 0.51 |
| LG | 23.5 | ||
| By Stage | |||
| Ta | −3.57 | 0 | 0.64 |
| T1 | 3.31 | −6.88 | |
| Tis | 0.5 | −4.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, Z.; Punyala, A.; Sze, C.; Bhojani, N.; Zorn, K.C.; Elterman, D.; Chughtai, B. Patient-Reported Urinary Symptom Progression After Bacillus Calmette–Guerin Therapy for Bladder Cancer. Uro 2025, 5, 4. https://doi.org/10.3390/uro5010004
Singh Z, Punyala A, Sze C, Bhojani N, Zorn KC, Elterman D, Chughtai B. Patient-Reported Urinary Symptom Progression After Bacillus Calmette–Guerin Therapy for Bladder Cancer. Uro. 2025; 5(1):4. https://doi.org/10.3390/uro5010004
Chicago/Turabian StyleSingh, Zorawar, Ananth Punyala, Christina Sze, Naeem Bhojani, Kevin C. Zorn, Dean Elterman, and Bilal Chughtai. 2025. "Patient-Reported Urinary Symptom Progression After Bacillus Calmette–Guerin Therapy for Bladder Cancer" Uro 5, no. 1: 4. https://doi.org/10.3390/uro5010004
APA StyleSingh, Z., Punyala, A., Sze, C., Bhojani, N., Zorn, K. C., Elterman, D., & Chughtai, B. (2025). Patient-Reported Urinary Symptom Progression After Bacillus Calmette–Guerin Therapy for Bladder Cancer. Uro, 5(1), 4. https://doi.org/10.3390/uro5010004







